Abstract
Background
Available evidence suggesting that the rate of re‐expansion of spontaneous pneumothorax is 1.25%/day is based on a small sample and mathematical modelling‐based estimates.
Aim
To estimate the rate of re‐expansion of spontaneous pneumothoraces by a formula derived from computed tomography volumetry studies.
Methods
This retrospective study included adult patients with spontaneous pneumothorax, identified from patient management databases, who were treated conservatively. Medical records were reviewed to confirm that no intervention such as aspiration or catheter drainage had occurred. Radiographs were reviewed independently by two researchers and measured according to the method described by Collins et al. Their formula was used to estimate pneumothorax size on each date. The rate of re‐expansion was defined as the change in size (%)/number of days between radiographs. Patients were excluded if they did not have at least two radiographs taken, at least 1 day apart. Data were analysed using cluster analysis by patient to minimise the effect of repeated measures from an individual patient.
Results
88 episodes were identified in 57 patients. 82% were men and the patients had a median age of 22 years. The average rate of re‐expansion was 2.2%/day (95% confidence interval 1.4% to 3.0%), but varied between −7.5% and 13.4%/day.
Conclusion
Spontaneous pneumothoraces treated conservatively re‐expand at an average rate of 2.2%/day.
A few studies have explored the rate of resolution of spontaneous pneumothoraces, and all have had small sample sizes. Current “best evidence” derives from the report of Kircher and Swartel,1 who used a mathematical approach based on the area (not volume) of the collapsed lung on a radiograph compared with the area of the hemithorax and serial radiographs to estimate that pneumothoraces re‐expanded at a rate of 1.25%/day when treated with bed rest. Recently, more sophisticated methods for estimating the volume of a pneumothorax have been developed using radiographic thoracic gas volume measurement2 and helical computed tomography,3 but no studies have investigated the rate of re‐expansion of pneumothoraces using these methods.
We investigated the rate of re‐expansion of spontaneous pneumothoraces in patients treated conservatively.
Methods
This was a retrospective case series and radiographic analysis conducted at the Western Hospital in Melbourne, Australia (annual emergency department census 32 000), and the Prince of Wales Hospital, Hong Kong, China (annual emergency department census 160 000). We identified adult patients (aged >16 years) with spontaneous pneumothorax, treated conservatively from emergency department patient management databases. Australian patients presenting between February 2002 and August 2004 and patients from Hong Kong presenting between August 1994 and November 2004 were included. These dates reflect the availability of searchable databases at the study centres. The relevant institutional ethics committees at both sites approved the study.
Medical records were reviewed to confirm that the pneumothorax was of the spontaneous type and that no intervention such as aspiration or catheter drainage occurred. For eligible patients, data collected included initial date of presentation, age, sex and dates of review. Erect chest radiographs were reviewed independently by two researchers and measured according to the method described by Collins et al.3 This method used computed tomography volumetry to derive a formula based on measurements of interpleural distances on a chest radiograph to estimate pneumothorax size. The formula requires measurements of the interpleural distance at the apex (A) and to the lateral wall at the mid‐point of the upper and lower halves of the collapsed lung (B and C).
This formula was used to estimate pneumothorax size on each date for which a radiograph was available, and the rate of re‐expansion was defined as the change in size (%) divided by the number of days between paired consecutive radiographs. Patients were excluded if they did not have at least two radiographs, at least 1 day apart. Where a pneumothorax had resolved and there was more than 1 day between comparison radiographs, that comparison was excluded from analysis, as the resolution date could not be accurately defined. Matched consecutive pairs of expiratory films were preferred, but matched pairs of inspiratory films were also acceptable if expiratory films were not available.
The primary outcome of interest was the rate of re‐expansion of pneumothoraces (%/day). Data were analysed using cluster analysis by patient to minimise the effect of several measurements in the same patient and of descriptive statistics. The χ2 test and logistic regression using Stata were used to compare samples by site. The reproducibility of size estimates was tested using Pearson's correlation and bias plot analysis.
During the study period, the study sites had different approaches to management. The Hong Kong site closely followed the British Thoracic Society guidelines,4 whereas the Australian site had a much more non‐interventional approach centred on the clinical condition of the patient.
Results
Eighty eight matched sets of comparison films were identified for 57 patients, representing 64 episodes of pneumothorax. Four patients had two episodes and one patient had four episodes in the study period. Patients included 47 men and 10 women, with a median age of 22 (interquartile range 19–24, range 16–43) years; 32 patients (55 comparisons) were from Australia and 25 (33 comparisons) were from Hong Kong. Initial pneumothorax size ranged from 4.7% to 91.8%, with a median of 23.8%. Of the 88 comparison films, 42 pairs were expiratory and 46 were inspiratory films. The median delay between films was 2 days.
The average rate of change per day was 2.2% (95% confidence interval (CI) 1.4% to 3.0%; range −7.5% to 13.4%). Given the differences in ethnic mix between the patient populations at the two study sites, we compared the subgroups and found that there was no significant difference in the rate of re‐expansion when controlled for age, sex and initial pneumothorax size (p = 0.91). As we used both inspiratory and expiratory film pairs, we compared film type and found that there was no significant difference between re‐expansion rate derived from inspiratory versus expiratory x ray film pairs, when controlled for initial pneumothorax size (p = 0.45).
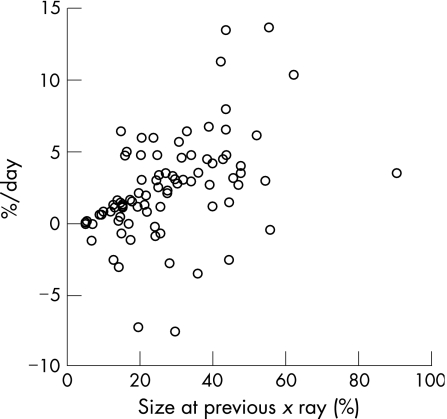
We found a significant relationship between rate of re‐expansion per day and pneumothorax size at previous radiograph (p<0.001; fig 1) The regression equation derived was
Figure 1 Relationship between the rate of re‐expansion (%/day) and pneumothorax size at initial radiograph.
With respect to reproducibility of size estimates by different observers, correlation was high.(r = 0.96, 95% CI 0.95 to 0.97). Bias plot analysis showed an average difference between observers' estimates of size by using Collins formula of 0.18%, with 95% limits of agreement of −6.7% to 8.1%.
Discussion
Major clinical guidelines for the treatment of spontaneous pneumothorax recommend intervention if the pneumothorax is >20% in size.4,5 This recommendation seems to be based on the work of Kircher and Swartel,1 who, by comparing outcomes in a non‐randomised group of 35 patients with pneumothorax treated with bed rest, intercostal catheter, or intercostal catheter and suction, concluded that if a pneumothorax was >20% in size, intervention reduced the length of hospital stay. This cut‐off is based on their estimation that pneumothoraces re‐expand at 1.25%/day. This figure was derived by comparing the area (not volume) of the remaining lung with the area of the hemithorax on a chest radiograph. Newer imaging techniques, particularly computed tomography, allow a more accurate measurement of pneumothorax volume and the derivation of more accurate ways to estimate volume from chest radiographs.3
Our study found that spontaneous pneumothoraces re‐expand at an average rate of 2.2%/day—almost double the previously accepted rate. The reasons for the discrepancy between our findings and those of Kircher et al1 are likely to be the difference in methods for calculating pneumothorax size (area v volume), the difference in sample size (35 v 57) and different treatment pathways (formal bed rest v conservative management, usually as an outpatient). If this higher rate is correct, it challenges the calculations on which the “20% rule” recommending intervention is based.
We also found considerable variability in the rate of re‐expansion. This raises some interesting questions. The rate of re‐expansion may not be linear, as has so far been tacitly assumed. It may vary with factors such as pneumothorax size and time from onset. Further research to investigate this question is warranted. It might be suggested that the wide variability in re‐expansion rate challenges the clinical relevance of our findings. On the contrary, much of medicine is like this. We believe that a knowledge of the average rate of re‐expansion and the fact that there is individual variability empowers clinicians to enter into more meaningful discussions with patients and decision making regarding therapeutic options.
That there is a relationship between initial pneumothorax size and the rate of re‐expansion is a new finding. Two physiological factors may be contributing to this. Firstly, oxygen in the pneumothorax will be reabsorbed more quickly than nitrogen, and thus there may be a faster reabsorption rate in the early period after the pneumothorax has formed. This is likely to be more pronounced in a large pneumothorax. Secondly, the transpulmonary pressure is higher when a lung collapses more. The lung may thus expand faster when a pneumothorax is large and more slowly when the transpulmonary pressure is low (ie, the pneumothorax is small).
Our study has some limitations that should be considered when interpreting our findings. It is a retrospective study, with all the well‐known limitations of retrospective data collection. Patient identification was from emergency department databases that are open to miscoding; so eligible cases may have been missed. The sample includes a relatively small number of patients from two ethnic groups. It may not be generalisable to populations of other ethnic backgrounds. With the small number of women in the study, we cannot be sure that there is no difference in re‐expansion rate on the basis of sex. There may also be patient selection bias, based on clinical condition. The method of calculation used was based on Collins et al's3 method derived using computed tomography volumetrics. The validity of this method has, to our knowledge, not been confirmed. The data refer to the overall (linear) rate of re‐expansion rather than the daily rate of re‐expansion. It is possible that the daily rate is higher when the pneumothorax is large, and this could also partially explain our findings.
Conclusion
Spontaneous pneumothoraces treated conservatively re‐expand at an average rate of 2.2%/day, with considerable variation. If these findings can be confirmed, they challenge the calculations on which the “20% rule” recommending intervention is based.
Acknowledgements
We thank the staff at the Radiology Departments of both hospitals; Professor David Hui (Respiratory Medicine, Chinese University of Hong Kong) for helpful comments on the manuscript; Miss Cecily Leung, Dr Stewart Chan and Professor Timothy Rainer (Hong Kong) for their advice and support; Mrs Megan Clooney (Australia) for assistance with case screening; and Mrs Debra Kerr and Dr Damian Jolley (Australia) for statistical assistance.
Footnotes
Funding: Departmental funds only. No external funding.
Competing interests: None.
References
- 1.Kircher L T, Swartel R L. Spontaneous pneumothorax and its treatment. JAMA 195415324–25. [DOI] [PubMed] [Google Scholar]
- 2.Rhea J T, DeLuca S A, Greene R E. Determining the size of pneumothorax in the upright patient. Radiology 1982144733–736. [DOI] [PubMed] [Google Scholar]
- 3.Collins C D, Lopez A, Mathie A.et al Quantification of pneumothorax size on chest radiographs using interpleural distances: regression analysis based on volume measurements from helical CT. Am J Roentgenol 19951651127–1130. [DOI] [PubMed] [Google Scholar]
- 4.Henry M, Arnold T, Harvey J. BTS guidelines for the management of spontaneous pneumothorax. Thorax 200358ii39–ii52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baumann M H, Strange C, Heffner J E.et al Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest 2001119590–602. [DOI] [PubMed] [Google Scholar]