Abstract
To describe trends in the utilization of surgical procedures for pelvic organ prolapse among women in Olmsted County, MN, we retrospectively identified all county residents undergoing pelvic organ prolapse repair from January 1, 1965 through December 31, 2002. From 1965 to 2002, 3,813 women had pelvic organ prolapse surgeries: 3,126 had hysterectomy combined with pelvic floor repair (PFR) procedures and 687 had PFR alone. The age-adjusted utilization of hysterectomy plus PFR and of PFR alone decreased by 62% (P<0.001) and 32% (P= 0.02), respectively. In both groups, utilization decreased in all age groups over time except in women aged 80 years and older undergoing hysterectomy plus PFR and women aged 70 years and older undergoing PFR only. The most common indication for PFR was uterovaginal prolapse. Among women in the community, the rate of utilization and age distribution of pelvic organ prolapse surgery changed substantially between 1965 and 2002.
Keywords: Hysterectomy, Pelvic floor repair, Pelvic organ prolapse, Population study, Utilization rate
Introduction
In 1997, approximately 225,000 women underwent surgery for pelvic organ prolapse in the United States. Pelvic organ prolapse is a common medical condition that represents the leading indication for hysterectomy in women aged 55 years and older in the United States [1–3]. Depending on the population studied, between 7% and 14% of all hysterectomies are performed because of pelvic organ prolapse [4–7]. An estimated 11% of all women will have a surgical intervention for this condition during their lifetime, and 30% of these women will undergo repeat operation for prolapse recurrence [8]. In addition, 42% of women undergoing a surgical intervention for stress urinary incontinence also have concomitant prolapse repair [8].
The lifetime incidence of pelvic organ prolapse is high, but the prevalence varies widely. In a Swedish study, 31% of women aged 20 to 59 years had prolapse [9]. However, half of them had a mild, clinically insignificant prolapse, and only 2% had a symptomatic prolapse. Even though severe morbidity from pelvic organ prolapse is rare [10], the condition commonly impairs a woman’s quality of life as the result of a protruding mass from the vagina, dyspareunia, low back pain, pelvic pressure, or difficulty with bladder and bowel evacuation [11, 12].
The National Hospital Discharge Survey has been used to assess the prevalence, regional distribution, demographic characteristics, morbidity, and mortality of surgery for pelvic organ prolapse in the United States [2, 3]. These surveys are derived from a multistage probability sample of nonfederal, inpatient hospital discharges. The most recent update suggested that the rate of prolapse repair procedures decreased from 2.2 per 1,000 women in 1979 to 1.5 per 1,000 in 1997. Because these studies characterized age into two categories (<50 and ≥50 years), information on the age distribution of women undergoing prolapse surgery is limited.
Although the 1997 survey separated single (e.g., vaginal hysterectomy) from combined procedures (e.g., vaginal hysterectomy and cystocele repair), temporal trends are not available at this level of detail. This information is important because most patients undergo combined procedures [2] and because hysterectomy is a putative risk factor for pelvic organ prolapse. Thus, a more clinically detailed, population-based study of prolapse surgery in the United States is imperative. The primary objective of our study was to explore secular trends in the utilization rates and types of surgical procedures performed for pelvic organ prolapse in Olmsted County, MN by using the data resources of the Rochester Epidemiology Project.
Materials and methods
Research setting
Medical care in Olmsted County, located in the southeastern part of Minnesota, is virtually self-contained within the community, thus allowing population-based epidemiologic research into the incidence and determinants of diverse diseases and therapeutic interventions [13]. Women’s surgical care is provided almost entirely by Mayo Clinic and Olmsted Medical Center. Mayo Clinic has maintained a common medical record with its two large affiliated hospitals (Rochester Methodist and Saint Marys) for 100 years. This dossier-type record thus contains both inpatient and outpatient data, and specific records are easily retrieved for review because diagnoses and surgical procedures are indexed [14]. The medical records of the other providers who serve the local population, most notably Olmsted Medical Center with its hospital, are similarly indexed by the Rochester Epidemiology Project [13]. Thus, the details of almost all the medical care provided to Olmsted County residents are available for study through this medical record linkage system. This population has been extensively studied previously for the purpose of reporting the epidemiology of surgical procedures [15–17].
Study subjects
After approval from the Institutional Review Boards of Mayo Clinic and Olmsted Medical Center, the Rochester Epidemiology Project database was used to identify all women residing in Olmsted County who underwent surgical procedures for pelvic organ prolapse between January 1, 1965, and December 31, 2002. Surgical procedures for pelvic organ prolapse were broadly divided into pelvic floor repairs (PFR) alone or PFR with hysterectomy. The procedure type and indications were identified electronically using the Berkson coding system from January 1, 1965 to December 31, 1987 (Table 1) and the International Classification of Diseases, 9th Revision, Clinical Modification procedural codes from January 1, 1988 to December 31, 2002 (Table 2). In 100 randomly selected women, the procedure type in the electronic record system was manually compared with the procedure type listed in the surgical note; these two sources agreed in 99% of cases.
Table 1.
Berkson codes for hysterectomy and pelvic floor repair, 1965–1987
| Procedure name or type | Berkson code |
|---|---|
| Hysterectomy | |
| Subtotal hysterectomy | 4694; 4695 |
| Total abdominal hysterectomy | 4680; 4690 |
| Vaginal hysterectomy | 4700; 4710 |
| Radical abdominal hysterectomy | 4720 |
| Pelvic evisceration and exenteration | 3480 |
| Oophorectomy | |
| Unilateral or bilateral | 4830 |
| Salpingo-oophorectomy | 4870 |
| Uterine suspensions | 4670 |
| Pelvic floor repairs | |
| Cystocele repair | 4990 |
| Cystocele, rectocele, urethrocele, or enterocele repair | 4710; 4990 & 4994 |
| Cystocele, rectocele, anterior and posterior colporrhaphy, and colpoperineoplasty | 4710; 4980; 4990 & 4994 |
| Vagina construction and reconstruction | 7010-4990; 7010-0122 |
| Fistula repairs | 5010 |
| Vagina suspension and fixation | 4710; 4980; 4990 & 4994 |
Table 2.
ICD-9-CM procedure codes for hysterectomy with or without pelvic floor repair, 1988–2002
| Procedure name or type | ICD-9-CM code |
|---|---|
| Total abdominal hysterectomy | 68.4 |
| Vaginal hysterectomy | 68.5 |
| Laparoscopically assisted vaginal hysterectomy | 68.51 |
| Other vaginal hysterectomy | 68.59 |
| Repair of uterine supporting structures | 69.2 |
| Other uterine suspension (hysteropexy, Manchester operation, plication of uterine ligament) | 69.22 |
| Other repair of uterus and supporting structures | 69.29 |
| Obliteration and total excision of vagina (vaginectomy) | 70.4 |
| Repair of cystocele and rectocele | 70.5 |
| Repair of cystocele (anterior colporrhaphy with urethrocele repair) | 70.51 |
| Repair of rectocele | 70.52 |
| Posterior colporrhaphy | 70.52 |
| Vaginal construction and reconstruction | 70.6 |
| Vaginal construction | 70.61 |
| Vaginal reconstruction | 70.62 |
| Other repair of vagina | 70.7 |
| Vagina suspension and fixation | 70.77 |
| Other repair of vagina (colpoperineoplasty, repair of old obstetrics laceration of vagina) | 70.79 |
| Obliteration of vaginal vault (Le Fort operation) | 70.8 |
| Other operations on vagina and cul-de-sac | 70.9 |
| Other operations of vagina | 70.91 |
| Other operations on cul-de-sac (obliteration of cul-de-sac, repair of vaginal enterocele) | 70.92 |
| Repair of vulva and perineum | 71.7 |
| Other repair of vulva and perineum | 71.79 |
| Repair of old obstetrics laceration of vulva or perineum | 71.79 |
ICD-9-CM International Classification of Diseases, 9th Revision, Clinical modification.
The procedures were then matched with their corresponding indication codes as contained in the electronic medical records of the operation and with the pathologic diagnosis. If multiple diagnoses were present, the principal indication for operation was assigned using the hierarchical system established by the Centers for Disease Control and Prevention [18]. If cancer of the reproductive tract was among the listed diagnoses, it was assigned as the primary indication. Next, if debulking of cancer of the intestinal or urinary tract was listed, debulking was assigned as the indication for the procedure. If a precancerous condition such as endometrial hyperplasia or carcinoma in situ of the cervix was listed, and no diagnosis of cancer listed, then the precancerous condition was selected as the diagnosis. If cancer or a precancerous condition was not listed, the diagnoses were then scanned for uterine leiomyoma, endometriosis, or uterine prolapse, and the first of these listed diagnoses was selected as the primary indication. A similar approach was used for menstrual disorders, menopausal disorders, and inflammatory diseases of the pelvis; the remaining records were placed in the “other” category.
Statistical analysis
To be considered an incident case, the patient must have been residing in Olmsted County at the time of the surgical procedure. Patients were excluded if they had a procedure that did not involve any type of PFR either alone or in combination with other procedures. For estimating utilization rates (incidence density), the entire population of women in Olmsted County was considered to be at risk for the procedure; the denominator and age-specific person-years were derived from decennial census data, with linear interpolation between census years [19]. The utilization rates were directly age-adjusted to the population structure of white females in the United States in 2000 because this is the population that most resembles Olmsted County (99% white in 1970, 98% in 1980, 96% in 1990, and 90% in 2000). Standard errors and 95% confidence intervals for the rates were estimated, assuming that the incidence of cases followed a Poisson distribution [19, 20].
Temporal trends in the incidence rates for hysterectomy combined with any kind of PFR, and separately for PFR alone, were assessed using Poisson regression models, incorporating age group, calendar period, and age-by-period interaction terms as predictors.
Because PFR comprises several procedures and some of these procedures were observed infrequently, several categories were collapsed. Thus, for example, “any other pelvic floor repairs” includes all other PFR except cystocele repair, cystocele and rectocele repair, vaginal reconstruction and fixation, vaginal fixation/suspension, and fistula repair.
To assess the association of calendar period, age, and “route” of procedure with types of surgical procedures for pelvic organ prolapse, a multiple logistic regression model was used to estimate the odds of a combined cystocele repair, rectocele repair, and perineoplasty versus a cystocele repair procedure only. Age, calendar period, “route” of procedure (vaginal, abdominal, PFR), age-by-period, and “route”-by-period interaction terms were incorporated as predictors. The odds ratios and 95% confidence intervals for cystocele repair, rectocele repair, and perineoplasty versus cystocele repair alone were estimated from the coefficients (and their standard errors) in the model. The reference category was the abdominal route for hysterectomy during the 1965 to 1974 calendar period.
Results
On review of the database, 10,578 women were initially identified as having undergone pelvic organ prolapse procedures during the 38-year study period. Women who had undergone hysterectomy only (n=6,150) were excluded from this study, as were 615 patients who did not authorize use of their medical records for research [21]. The remaining 3,813 women who had pelvic organ prolapse procedures were included in this analysis: 3,126 women had hysterectomy combined with a PFR procedure, and 687 women had PFR procedures only.
Temporal trends for hysterectomy combined with PFR
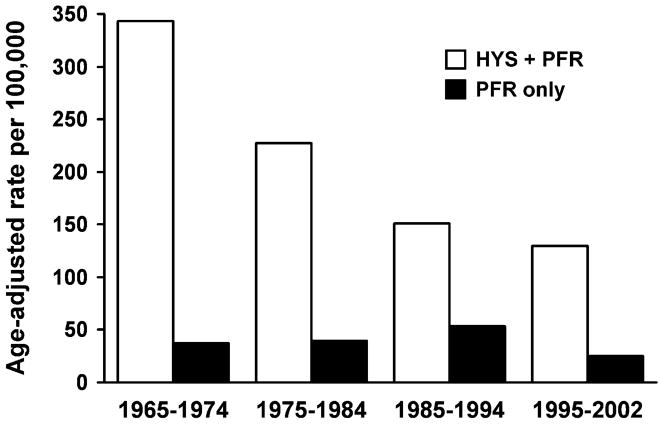
The overall age-adjusted utilization rate for hysterectomy combined with any kind of PFR decreased by 62%, from 343 per 100,000 person-years in 1965 to 1974 to 130 per 100,000 in 1995 to 2002 (P<0.001) (Fig. 1), as we reported previously [22]. Except in women aged 80 years and older, the incidence of combined hysterectomy and PFR decreased in all age groups (Table 3). The decrease was most pronounced (by 82%) among women aged 30 to 39 years. In contrast, among women aged 80 years and older, the annual incidence increased by 61%, from 87 per 100,000 person-years in 1965 to 1974 to 141 per 100,000 person-years in 1995 to 2002. The age-specific rates were significantly associated with age group (P<0.001) and calendar period (P<0.001). In addition, a significant age-by-period interaction was found (P<0.001), implying that the magnitude of temporal changes varied by age group.
Fig. 1.
Age-adjusted rate of hysterectomy (HYS) and pelvic floor repair (PFR) per 100,000 person-years among women of Olmsted County, Minnesota from 1965–2002
Table 3.
Utilization of hysterectomy with pelvic floor repair procedures in Olmsted County, MN, 1965–2002
| Rate by yeara |
|||||
|---|---|---|---|---|---|
| Age group (years) | 1965–1974 | 1975–1984 | 1985–1994 | 1995–2002 | All years |
| <30 | 10.7 | 7.5 | 9.6 | 2.4 | 7.8 |
| 30–39 | 554.2 | 227.8 | 141.9 | 97.6 | 223.0 |
| 40–49 | 946.4 | 660.4 | 337.5 | 287.2 | 495.3 |
| 50–59 | 468.8 | 374.7 | 261.5 | 198.5 | 311.4 |
| 60–69 | 357.8 | 246.7 | 240.3 | 228.3 | 264.9 |
| 70–79 | 284.3 | 273.9 | 255.2 | 271.0 | 270.0 |
| ≥80 | 87.2 | 64.8 | 84.1 | 140.5 | 97.8 |
| Age-adjusted rate (95% CI)b | 342.7 (321.7–363.7) | 227.1 (211.2–243.0) | 151.0 (139.5–162.5) | 129.6 (119.0–140.3) | 196.4 (189.4–203.3) |
CI confidence interval.
Utilization rate per 100,000 person-years.
Utilization rate directly age-adjusted to the US population in 2000.
Temporal trends for PFR alone
The overall age-adjusted utilization of PFR alone decreased by 32%, from 37 per 100,000 person-years in 1965 to 1974 to 25 per 100,000 in 1995 to 2002 (P=0.02) (Fig. 1). Except in women aged 70 to 79 years and 80 years and older, the incidence of PFR alone decreased in all age groups (Table 4). The decrease in utilization was most pronounced (by 63%) among women aged 40 to 49 years and least (by 40%) among women aged 50 to 59 years. Among older women, the annual incidence increased by 52% in those aged 70 to 79 years and by 61% in those 80 years and older. Age-specific rates were significantly associated with age group (P=0.02) and calendar period (P=0.03). As with PFR plus hysterectomy, an age-by-period interaction was seen (P<0.001), implying that the magnitude of temporal changes observed was not uniform across age groups.
Table 4.
Utilization of pelvic floor repair procedures alone in Olmsted County, MN, 1965-2002
| Rate by yeara |
|||||
|---|---|---|---|---|---|
| Age group (years) | 1965–1974 | 1975–1984 | 1985–1994 | 1995–2002 | All years |
| <30 | 10.3 | 14.6 | 66.2 | 4.3 | 24.8 |
| 30–39 | 22.5 | 19.6 | 62.1 | 12.4 | 31.8 |
| 40–49 | 38.2 | 42.5 | 15.9 | 14.2 | 24.8 |
| 50–59 | 59.3 | 56.1 | 38.9 | 35.4 | 46.0 |
| 60–69 | 120.4 | 84.4 | 45.8 | 54.8 | 74.1 |
| 70–79 | 69.8 | 116.2 | 80.2 | 106.1 | 93.8 |
| ≥80 | 29.1 | 58.3 | 42.0 | 46.8 | 45.2 |
| Age-adjusted rate (95% CI)b | 36.8 (30.1–43.5) | 40.2 (33.7–46.7) | 52.7 (46.6–58.9) | 24.7 (19.9–29.6) | 38.7 (35.7–41.7) |
CI, confidence interval.
Utilization rate per 100,000 person-years.
Utilization rate directly age-adjusted to the US population in 2000.
Procedure type, age distribution, and associated diagnosis
In terms of the number of procedures performed among different age groups, women younger than 30 years had the highest number of PFR procedures alone. When PFR was combined with hysterectomy, whether abdominal or vaginal, women aged 40 to 49 years accounted for the greatest number of procedures (Table 5). The category “Vaginal hysterectomy with any other pelvic floor repairs” is large because the Berkson code, 4710, includes vaginal hysterectomy plus PFR but does not specify the type of PFR.
Table 5.
Pelvic organ prolapse surgery type by age group in Olmsted County, MN, 1965–2002
| No. of patients (%)
|
|||||||
|---|---|---|---|---|---|---|---|
| Surgery type | <30 y (n=311) | 30–39 y (n=770) | 40–49 y (n=1,237) | 50–59 y (n=614) | 60–69 y (n=430) | 70–79 y (n=353) | ≥80 y (n=98) |
| Vaginal hysterectomy | |||||||
| With cystocele repair | 24 (7.7) | 151 (19.6) | 302 (24.4) | 130 (21.2) | 120 (27.9) | 103 (29.2) | 39 (39.8) |
| With cystocele and rectocele repair | 9 (2.9) | 111 (14.4) | 162 (13.1) | 51 (8.3) | 19 (4.4) | 13 (3.7) | 2 (2.0) |
| Vaginal construction/reconstruction | 2 (0.6) | 17 (2.2) | 42 (3.4) | 10 (1.6) | 3 (0.7) | 1 (0.3) | 0 (0) |
| Vaginal fixation/suspension | 0 (0) | 1 (0.1) | 1 (0.08) | 1 (0.2) | 0 (0) | 1 (0.3) | 0 (0) |
| Fistula repair | 0 (0) | 4 (0.5) | 2 (0.2) | 1 (0.2) | 0 (0) | 0 (0) | 0 (0) |
| With any other pelvic floor repairs | 31 (10.0) | 317 (41.2) | 511 (41.3) | 274 (44.6) | 183 (42.6) | 131 (37.1) | 22 (22.4) |
| Abdominal hysterectomy | |||||||
| With cystocele repair | 7 (2.3) | 52 (6.8) | 118 (9.5) | 43 (7.0) | 5 (1.2) | 9 (2.5) | 1 (1.0) |
| With cystocele and rectocele repair | 1 (0.3) | 20 (2.6) | 32 (2.6) | 21 (3.4) | 5 (1.2) | 2 (0.6) | 3 (3.1) |
| With vaginal construction/reconstruction | 0 (0) | 0 (0) | 5 (0.4) | 4 (0.7) | 0 (0) | 2 (0.6) | 0 (0) |
| Vaginal fixation/suspension | 0 (0) | 0 (0) | 2 (0.2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Fistula repair | 0 (0) | 1 (0.1) | 1 (0.08) | 0 (0) | 1 (0.2) | 0 (0) | 0 (0) |
| Pelvic floor repairs only | |||||||
| Cystocele repair | 78 (25.1) | 33 (4.3) | 28 (2.3) | 37 (6.0) | 49 (11.4) | 49 (13.9) | 20 (20.4) |
| Cystocele and rectocele repair | 144 (46.3) | 50 (6.5) | 25 (2.0) | 37 (6.0) | 42 (9.8) | 37 (10.5) | 9 (9.2) |
| Vaginal construction/reconstruction | 0 (0) | 0 (0) | 1 (0.08) | 3 (0.5) | 0 (0) | 1 (0.3) | 1 (1.0) |
| Vaginal fixation/suspension | 1 (0.3) | 1 (0.1) | 0 (0) | 1 (0.2) | 0 (0) | 3 (0.8) | 0 (0) |
| Fistula repair | 14 (4.5) | 12 (1.6) | 5 (0.4) | 1 (0.2) | 3 (0.7) | 1 (0.3) | 1 (1.0) |
We performed a subset analysis of 2,193 cases, comparing patients undergoing cystocele repair alone with patients undergoing multicompartment repair (cystocele, rectocele, and perineoplasty). Patients having vaginal construction/reconstruction, fistula repair, vaginal suspension, or other types of repairs were not included. On the basis of logistic regression analysis, the odds of having a combined procedure (vs cystocele repair alone) were greater for those undergoing a vaginal hysterectomy or PFR alone relative to those having an abdominal hysterectomy in the reference period (1965–1974) (Table 6). This trend continued throughout the remaining periods of study, with some variance. In general, the odds of having a multicompartment repair versus cystocele repair increased with each calendar period, regardless of the route of hysterectomy (Table 6).
Table 6.
Odds of having a multicompartment repair vs cystocele repair alone by year and type of procedure (n=2,193)
| Repair procedurea |
|||
|---|---|---|---|
| Procedure route by year | Multicompartmentb | Cystocele | OR (95% CI)c |
| 1965–1974 (n=384) | 182 (47.4) | 202 (52.6) | |
| Abdominal (n=81) | 24 (29.6) | 57 (70.4) | 1.0 (reference) |
| Vaginal (n=188) | 102 (54.3) | 86 (45.7) | 3.0 (1.7–5.3) |
| PFR (n=115) | 56 (48.7) | 59 (51.3) | 1.9 (1.0–3.5) |
| 1975–1984 (n=428) | 137 (32.0) | 291 (68.0) | |
| Abdominal (n=128) | 15 (11.7) | 113 (88.3) | 0.4 (0.1–1.2) |
| Vaginal (n=151) | 71 (47.0) | 80 (53.0) | 2.8 (1.1–7.2) |
| PFR (n=149) | 51 (34.2) | 98 (65.8) | 1.4 (0.5–4.0) |
| 1985–1994 (n=797) | 304 (38.1) | 493 (61.9) | |
| Abdominal (n=84) | 22 (26.2) | 62 (73.8) | 6.3 (2.4–16.7) |
| Vaginal (n=427) | 92 (21.6) | 335 (78.4) | 5.5 (2.3–13.2) |
| PFR (n=286) | 190 (66.4) | 96 (33.6) | 26.1 (11.2–60.8) |
| 1995–2002 (n=584) | 172 (29.4) | 412 (70.6) | |
| Abdominal (n=26) | 23 (88.5) | 3 (11.5) | 285 (58.2–1,394) |
| Vaginal (n=470) | 102 (21.7) | 368 (78.3) | 10.3 (3.8–27.8) |
| PFR (n=88) | 47 (53.4) | 41 (46.6) | 64.3 (19.7–210) |
CI confidence interval, OR odds ratio, PFR pelvic floor repair.
Values are no. of patients (%).
Combined cystocele repair, rectocele repair, and perineoplasty.
Multicompartment repair versus cystocele repair alone. Estimated from logistic regression model including age, route of procedure (abdominal, vaginal, or PFR), calendar period, and interaction terms of age by calendar period and route by calendar period.
With respect to the indications, as would be expected, the leading indications for these procedures were uterovaginal prolapse (34%) followed by leiomyoma (25%) and precancerous conditions (22%). Other indications were endometriosis, menopause, and other conditions (8%); menstrual disorders (7%); and cancer (4%).
Discussion
Similar to the National Hospital Discharge Summary database results [3], our data show that the utilization of pelvic organ prolapse surgery in the United States has decreased over time. Indeed, our findings suggest that the overall age-adjusted rates of prolapse surgery, as either hysterectomy combined with any type of PFR or PFR alone, progressively decreased by 62% and 32%, respectively, between 1965 and 2002. The overall age-adjusted annual utilization rate for PFR procedures decreased from 380 to 154 per 100,000 person-years between 1965 and 2002.
Allowing for regional variations and differences in time periods, these temporal trends are comparable to the corresponding decrease from 220 to 150 per 100,000 person-years between 1979 and 1997 reported by the National Hospital Discharge Summary [3]. A large health maintenance organization, the Kaiser Permanente system, reported an age-specific incidence of 263 per 100,000 person-years for any prolapse procedure in 1995 [8]. In contrast to those studies, the primary criterion for identifying procedures in our study was procedure code for the type of operation (i.e., hysterectomy with PFR or PFR alone) rather than the indication (i.e., prolapse). This method was used because we primarily wanted to capture surgical procedures for prolapse and minimize the inclusion of women who had procedures performed primarily for other indications (e.g., fibroids) but who also had prolapse. This distinction is important because pelvic organ prolapse is so common; in one large study, less than 10% of asymptomatic women had no (i.e., stage 0) prolapse [23].
Our data suggest that temporal trends were strongly influenced by patient age. The most pronounced decrease in hysterectomy utilization was among women younger than 40 years. In contrast to the overall trend, the utilization rate for hysterectomy combined with PFR increased among women aged 70 to 79 years between 1995 and 2002 compared with the previous period; a similar trend was observed among women aged 60 to 69 years undergoing PFR alone. The National Hospital Discharge Survey study also observed a greater decrease in the age-adjusted rate of prolapse procedures among women aged 50 years and older [3].
No direct estimates have been made of the prevalence of pelvic organ prolapse in the community. However, the proportion of vaginal hysterectomies performed for pro-lapse in Olmsted County also decreased from 33% to 16% between 1965 and 2002, as shown in our previous study [22]. Altogether, these observations suggest that the incidence of pelvic organ prolapse or the use of surgical procedures to manage prolapse (or both) has decreased over time, particularly among younger women.
Several factors may account for changes in the rates of prolapse surgeries, such as changes in practice patterns due to health care reform, increased patient education, and new minimally invasive options for treatment of benign gynecologic conditions [18]. Hysterectomy is a risk factor for pelvic organ prolapse [8]. Indeed, the cumulative risk of surgically treated prolapse after hysterectomy increases linearly over time to 5% at 15 years [24]. Moreover, case-control and population-based cohort studies suggest that the risk of a subsequent PFR after hysterectomy is higher when hysterectomy is performed for genital prolapse [25, 26]. Because hysterectomy is a potential risk factor for pelvic organ prolapse [24], it is conceivable that the observed decrease in hysterectomy utilization rates [7, 22] may also be contributing to the overall decrease in procedures for pelvic organ prolapse.
In contrast, the increased utilization of PFR among elderly women in the most recent time period may be a result of an increased prevalence of prolapse or may be because elderly women with pelvic prolapse are now more likely to undergo surgical repair.
Since the 1985–1994 period, surgeons have increasingly favored multicompartment repair (cystocele repair and/or rectocele repair and/or perineoplasty) over cystocele repair alone, which reinforces previous observations that women with pelvic organ prolapse often have multiple anatomic defects [27]. Therefore, they often undergo multiple procedures during the same operation [2]. It is unclear whether these temporal trends reflect an increased prevalence of multicompartment defects or an increasing appreciation among urogynecologists that pelvic organ prolapse is a multicompartment disorder.
More than 80% of women in our study had a PFR procedure in conjunction with hysterectomy. However, 75% of all PFR procedures in women younger than 30 years did not include hysterectomy. For women aged between 30 and 60 years, most PFR procedures included hysterectomy. Thereafter, the proportion of women who had PFR alone increased, reaching 32% for women aged 80 years and older. It is likely that this bimodal distribution of isolated PFR procedures is composed of younger women who have not had a hysterectomy and older women who have had a hysterectomy previously. Also of interest, between 1985 and 1994, there was a pronounced blip (i.e., an increase) in the age-adjusted utilization of PFRs alone among women aged younger than 40 years.
These data have substantial implications for public health. It has been suggested that approximately one-third of women with pelvic organ prolapse will require surgery [28] and many will require more than one procedure in their lifetime. Although the overall rates have decreased up to 2002, this trend may abate given increased utilization of these procedures in the elderly and the aging of the US population. Conversely, because pelvic surgery for benign conditions may increase the risk for pelvic surgery in the future [8], the decreasing utilization of PFR in younger women may in turn decrease the need for pelvic surgery among older women. Advances in medical therapies for comorbid conditions, as well as surgical techniques and anesthetic options, may allow a more aggressive approach than in previous decades. Evolving data suggest that older patients tolerate surgical intervention for those conditions well, with low associated complication rates [29].
Because our data were obtained from an existing database, the accuracy of procedure coding is a possible limitation. However, the procedure type in the electronic record system agreed with the procedure type listed in the actual surgical note assessed manually in 99% of cases. Other pertinent clinical information (such as gravidity and parity, associated medical conditions, and possible procedure-related complications) was not collected, limiting our ability to collate the possible surgical and medical complications associated with prolapse surgeries. Furthermore, the overall rate and numbers of procedures reflect primary surgery in some women and repeat surgery in others because it is not possible to completely distinguish them in this database. The rate of nonsurgical treatment for prolapse in the community is still unknown because some women with pelvic organ prolapse are relatively asymptomatic and therefore have not sought care, whereas other symptomatic women also may not have sought care or may have declined suggested therapies. Finally, given the lack of significant racial diversity in our community, our findings may not be applicable to more racially diverse settings.
In summary, the utilization and age distribution of pelvic organ prolapse surgery has changed substantially in the past several decades. Although less surgery is being performed overall, those having surgical intervention are more likely to undergo multicompartment repair, and older women are more likely to have surgery than in the past. Our study and changing population demographics suggest that surgical and nonsurgical management of prolapse may increase in the near future. Luber et al. [28] project that over the next 30 years, growth in the demand for services to care for female pelvic floor disorders will increase at twice the rate of growth of the same population. This projection has broad-reaching implications. Future research should investigate improved ways of addressing our questions epidemiologically while providing outcome-based observations of our surgical techniques. In addition, budgetary projections for necessary allocated funding of research in female pelvic floor disorders as well as a needs assessment evaluation of physician training and administrative programs to care for these women must be addressed.
Acknowledgments
This study was supported in part by research grants HD 41129, AR 30582, and AG 04875 from the National Institutes of Health, U.S. Public Health Service. Editing, proofreading, and reference verification were provided by the Section of Scientific Publications, Mayo Clinic.
Abbreviation
- PFR
pelvic floor repair
Footnotes
Portions of this manuscript were originally published in Babalola et al. [22]. Used with permission.
Conflicts of interest None.
References
- 1.MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000;107:1460–1470. doi: 10.1111/j.1471-0528.2000.tb11669.x. [DOI] [PubMed] [Google Scholar]
- 2.Brown JS, Waetjen LE, Subak LL, Thom DH, Van den Eeden S, Vittinghoff E. Pelvic organ prolapse surgery in the United States, 1997. Am J Obstet Gynecol. 2002;186:712–716. doi: 10.1067/mob.2002.121897. [DOI] [PubMed] [Google Scholar]
- 3.Boyles SH, Weber AM, Meyn L. Procedures for pelvic organ prolapse in the United States, 1979–1997. Am J Obstet Gynecol. 2003;188:108–115. doi: 10.1067/mob.2003.101. [DOI] [PubMed] [Google Scholar]
- 4.Allard P, Rochette L. The descriptive epidemiology of hysterectomy, Province of Quebec, 1981–1988. Ann Epidemiol. 1991;1:541–549. doi: 10.1016/1047-2797(91)90026-9. [DOI] [PubMed] [Google Scholar]
- 5.Weber AM, Lee JC. Use of alternative techniques of hysterectomy in Ohio, 1988–1994. N Engl J Med. 1996;335:483–489. doi: 10.1056/NEJM199608153350706. Erratum in: N Engl J Med 335:1406. [DOI] [PubMed] [Google Scholar]
- 6.Weaver F, Hynes D, Goldberg JM, Khuri S, Daley J, Henderson W. Hysterectomy in Veterans Affairs Medical Centers. Obstet Gynecol. 2001;97:880–884. doi: 10.1016/s0029-7844(01)01350-3. [DOI] [PubMed] [Google Scholar]
- 7.Farquhar CM, Steiner CA. Hysterectomy rates in the United States 1990–1997. Obstet Gynecol. 2002;99:229–234. doi: 10.1016/s0029-7844(01)01723-9. [DOI] [PubMed] [Google Scholar]
- 8.Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–506. doi: 10.1016/S0029-7844(97)00058-6. [DOI] [PubMed] [Google Scholar]
- 9.Samuelsson EC, Victor FT, Tibblin G, Svardsudd KF. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol. 1999;180:299–305. doi: 10.1016/s0002-9378(99)70203-6. [DOI] [PubMed] [Google Scholar]
- 10.Gemer O, Bergman M, Segal S. Prevalence of hydronephrosis in patients with genital prolapse. Eur J Obstet Gynecol Reprod Biol. 1999;86:11–13. doi: 10.1016/s0301-2115(99)00052-4. [DOI] [PubMed] [Google Scholar]
- 11.Lukman Y. Utero-vaginal prolapse: a rural disability of the young. East Afr Med J. 1995;72:2–9. [PubMed] [Google Scholar]
- 12.Gungor T, Ekin M, Dogan M, Mungan T, Ozcan U, Gokmen O. Influence of anterior colporrhaphy with colpoperineoplasty operations for stress incontinence and/or genital descent on sexual life. J Pak Med Assoc. 1997;47:248–250. [PubMed] [Google Scholar]
- 13.Melton LJ., III History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 14.Kurland LT, Molgaard CA. The patient record in epidemiology. Sci Am. 1981;245:54–63. doi: 10.1038/scientificamerican1081-54. [DOI] [PubMed] [Google Scholar]
- 15.Gabriel SE, O’Fallon WM, Beard CM, Kurland LT, Woods JE, Melton LJ., III Trends in the utilization of silicone breast implants, 1964–1991, and methodology for a population-based study of outcomes. J Clin Epidemiol. 1995;48:527–537. doi: 10.1016/0895-4356(94)00209-9. [DOI] [PubMed] [Google Scholar]
- 16.Melton LJ, III, Alothman KI, Achenbach SJ, O’Fallon WM, Zincke H. Decline in bilateral orchiectomy for prostate cancer in Olmsted county, Minnesota, 1956–2000. Mayo Clin Proc. 2001;76:1199–1203. doi: 10.4065/76.12.1199. [DOI] [PubMed] [Google Scholar]
- 17.Ghosh K, Melton LJ, III, Suman VJ, Grant CS, Sterioff S, Brandt KR, et al. Breast biopsy utilization: a population-based study. Arch Intern Med. 2005;165:1593–1598. doi: 10.1001/archinte.165.14.1593. [DOI] [PubMed] [Google Scholar]
- 18.Lepine LA, Hillis SD, Marchbanks PA, Koonin LM, Morrow B, Kieke BA, et al. Hysterectomy surveillance: United States, 1980–1993. Morb Mortal Wkly Rep CDC Surveill Summ. 1997;46:1–15. [PubMed] [Google Scholar]
- 19.Bergstralh EJ, Offord KP, Chu CP, Beard CM, O’Fallon WM, Melton LJ., III . Calculating incidence: prevalence and mortalities for Olmsted County, Minnesota: an update. Rochester, Minnesota: Mayo Clinic Department of Health Sciences Research, Section of Biostatistics; 1992. Technical report No.: 49. [Google Scholar]
- 20.Beyer WH. CRC handbook of tables for probability and statistics. Chemical Rubber Company; Cleveland, Ohio: 1966. [Google Scholar]
- 21.Melton LJ., III The threat to medical-records research. N Engl J Med. 1997;337:1466–1470. doi: 10.1056/NEJM199711133372012. [DOI] [PubMed] [Google Scholar]
- 22.Babalola EO, Bharucha AE, Schleck CD, Gebhart JB, Zinsmeister AR, Melton LJ., III Decreasing utilization of hysterectomy: a population-based study in Olmsted County, Minnesota, 1965–2002. Am J Obstet Gynecol. 2007;196:214.e1–214.e7. doi: 10.1016/j.ajog.2006.10.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Swift SE. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol. 2000;183:277–285. doi: 10.1067/mob.2000.107583. [DOI] [PubMed] [Google Scholar]
- 24.Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. Br J Obstet Gynaecol. 1997;104:579–585. doi: 10.1111/j.1471-0528.1997.tb11536.x. [DOI] [PubMed] [Google Scholar]
- 25.Dällenbach P, Kaelin-Gambirasio I, Dubuisson JB, Boulvain M. Risk factors for pelvic organ prolapse repair after hysterectomy. Obstet Gynecol. 2007;110:625–632. doi: 10.1097/01.AOG.0000278567.37925.4e. [DOI] [PubMed] [Google Scholar]
- 26.Blandon RE, Bharucha AE, Melton LJ, 3rd, Schleck CD, Babalola EO, Zinsmeister AR, et al. Incidence of pelvic floor repair after hysterectomy: a population-based cohort study. Am J Obstet Gynecol. 2007;197:664.e1–e7. doi: 10.1016/j.ajog.2007.08.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the Women’s Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186:1160–1166. doi: 10.1067/mob.2002.123819. [DOI] [PubMed] [Google Scholar]
- 28.Luber KM, Boero S, Choe JY. The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol. 2001;184:1496–1501. doi: 10.1067/mob.2001.114868. [DOI] [PubMed] [Google Scholar]
- 29.Stepp KJ, Barber MD, Yoo EH, Whiteside JL, Paraiso MF, Walters MD. Incidence of perioperative complications of urogynecologic surgery in elderly women. Am J Obstet Gynecol. 2005;192:1630–1636. doi: 10.1016/j.ajog.2004.11.026. [DOI] [PubMed] [Google Scholar]