Abstract
Physical therapists commonly treat people with diabetes for a wide variety of diabetes-associated impairments, including those from diabetes-related vascular disease. Diabetes is associated with both microvascular and macrovascular diseases affecting several organs, including muscle, skin, heart, brain, and kidneys. A common etiology links the different types of diabetes-associated vascular disease. Common risk factors for vascular disease in people with diabetes, specifically type 2 diabetes, include hyperglycemia, insulin resistance, dyslipidemia, hypertension, tobacco use, and obesity. Mechanisms for vascular disease in diabetes include the pathologic effects of advanced glycation end product accumulation, impaired vasodilatory response attributable to nitric oxide inhibition, smooth muscle cell dysfunction, overproduction of endothelial growth factors, chronic inflammation, hemodynamic dysregulation, impaired fibrinolytic ability, and enhanced platelet aggregation. It is becoming increasingly important for physical therapists to be aware of diabetes-related vascular complications as more patients present with insulin resistance and diabetes. The opportunities for effective physical therapy interventions (such as exercise) are significant.
Diabetes mellitus (DM) is a global health issue affecting children, adolescents, and adults. According to the World Health Organization, approximately 180 million people worldwide currently have type 2 DM (formerly called adult-onset diabetes); over 95% of people with diabetes have this form. The number of people with type 2 DM is estimated to double by 2030.1 In the year 2000, death from diabetes-associated complications accounted for approximately 6% of worldwide mortality.2 Additionally, the economic burden of diabetes in the United States in 2002 was estimated to be $132 billion.3
Diabetes is a disease that is strongly associated with both microvascular and macrovascular complications, including retinopathy, nephropathy, and neuropathy (microvascular) and ischemic heart disease, peripheral vascular disease, and cerebrovascular disease (macrovascular), resulting in organ and tissue damage in approximately one third to one half of people with diabetes.4 Because of the progressive nature of the disease, physical therapists will increasingly encounter patients with prediabetes (ie, impaired glucose tolerance or insulin resistance), early type 2 DM without or with only a few vascular complications, and more advanced disease with several vascular complications. For additional information describing the epidemiology of these problems in people with DM, see the perspective article by Deshpande et al5 in this issue.
Diabetes-associated vascular alterations include anatomic, structural, and functional changes leading to multiorgan dysfunction.6 As physical therapists increasingly become first-line providers of treatment for musculoskeletal and movement disorders in people with diabetes, it will be important for clinicians to be keenly aware of the underlying vascular deficits in conditions such as diabetic neuropathy, retinopathy, nephropathy, and cardiovascular and peripheral vascular diseases in their treatment programs, even if these conditions are not the reasons for referral. Additionally, physical therapists will play an important role in the care of people with diabetes because numerous interventions provided by physical therapists (such as therapeutic exercise) can assist in alleviating symptoms, slow the metabolic progression to overt type 2 DM, and reduce morbidity and mortality associated with these complications.7–10
Diabetic microvascular (involving small vessels, such as capillaries) and macrovascular (involving large vessels, such as arteries and veins) complications have similar etiologic characteristics. Chronic hyperglycemia plays a major role in the initiation of diabetic vascular complications through many metabolic and structural derangements, including the production of advanced glycation end products (AGE), abnormal activation of signaling cascades (such as protein kinase C [PKC]), elevated production of reactive oxygen species (ROS, oxygen-containing molecules that can interact with other biomolecules and result in damage), and abnormal stimulation of hemodynamic regulation systems (such as the renin-angiotensin system [RAS]).
The objectives of this article are to briefly describe the epidemiology of, the comorbidities and risk factors associated with, the pathogenesis of, and the physical therapy management associated with microvascular and macrovascular complications of diabetes. In a significant portion of the article, the term “diabetes” includes both type 1 DM and type 2 DM, which have much the same vascular pathology and etiology.
Microvascular Complications of Diabetes
Diabetic Retinopathy
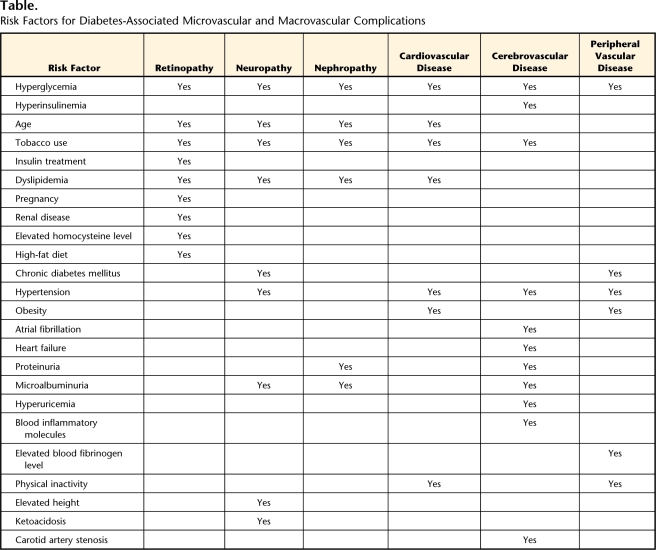
Diabetic retinopathy (DR) is a microvascular complication that can affect the peripheral retina, the macula, or both and is a leading cause of visual disability and blindness in people with diabetes.1 The severity of DR ranges from nonproliferative and preproliferative to more severely proliferative DR, in which the abnormal growth of new vessels occurs.11 Total or partial vision loss can occur through a vitreous hemorrhage or retinal detachment, and central vision loss can occur through retinal vessel leakage and subsequent macular edema.12 The prevalence of DR increases with prolonged duration of diabetes.13 In studies including people with both type 1 diabetes and type 2 diabetes, after 30 years of diabetes, most patients had some form of DR, and over half had proliferative DR; people with type 1 diabetes and taking insulin had the highest prevalence of DR, and people with type 2 diabetes diagnosed after age 30 had the lowest prevalence of DR.14–16 Diabetic retinopathy also recently was seen in approximately 10% of people with insulin resistance (prediabetes) and was associated with the presence of hypertension and a higher body mass index.17 Other studies of DR showed associations with younger age of onset, tobacco use, insulin treatment, abnormal blood lipid (ie, total cholesterol, low-density lipoprotein [LDL], and triglyceride) levels, pregnancy, renal disease, elevated homocysteine levels,18 and a diet high in fat (Table).19–21
Table.
Risk Factors for Diabetes-Associated Microvascular and Macrovascular Complications
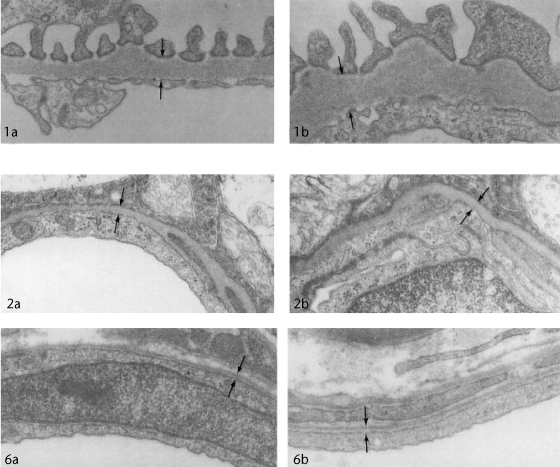
The earliest histological marker of DR is the loss of pericytes.22 Pericytes are elongated contractile cells that wrap around endothelial cells of small vessels23 and assist in providing maintenance of capillary tone (ie, dilatation and constriction),24 capillary growth, and protection against ROS damage.25 Therefore, the loss of pericytes with DR would interfere with capillary constriction (producing chronically dilated vessels), new capillary generation, and processes that protect vessels against continuous exposure to noxious molecules (ie, normal homeostasis). Other microvascular changes that occur with DR include capillary basement membrane thickening (Fig. 1),26 increased permeability of endothelial cells, and formation of microaneurysms (ie, weakening of vessel walls that results in the projection of a balloonlike sac) (Fig. 2).27
Figure 1.
Representative transmission electron micrographs of capillary basement membranes (opposing arrows) in tissues from 300- to 350-day-old normal mice (a) and age- and sex-matched transgenic diabetic mice (b). Capillary basement membranes are shown in renal glomerulus (1a, 1b), retina (2a, 2b), and peripheral nerve (6a, 6b). All micrographs: ×28,500. Reprinted with permission of Wiley-Liss Inc, a subsidiary of John Wiley & Sons Inc, from: Carlson EC, Audette JL, Veitenheimer NJ, et al. Ultrastructural morphometry of capillary basement membrane thickness in normal and transgenic diabetic mice. Anat Rec A Discov Mol Cell Evol Biol. 2003;271:332–341.
Figure 2.
Microaneurysms in diabetic retinopathy. From the Slice of Life collection, curated by Suzanne Stensaas, University of Utah.
The most significant factor in the development and progression of DR in people with diabetes appears to be poor glycemic (blood sugar) control.28,29 Under hyperglycemic conditions, which are frequently seen in people with diabetes, impairment of retinal blood flow, increased inflammatory cell adhesion to retinal blood vessels, and capillary blockage can result in hypoxia and damage to the retina.30
Diabetic Neuropathy
Approximately one half of people with diabetes have some form of peripheral neuropathy (PN), either polydiabetic or monodiabetic neuropathy.31 People with diabetes also frequently have autonomic neuropathy, including cardiovascular autonomic dysfunction, which is manifested as abnormal heart rate (HR) and vascular control.32 Physical therapists commonly encounter diabetes- associated PN in the evaluation and treatment of balance and movement disorders because these disorders frequently affect lower-extremity sensation and can cause lower-extremity pain in people with diabetes. Loss of lower-extremity sensation coupled with impaired peripheral vascular function can contribute to lower-extremity (commonly foot) ulceration.33 Like those for DR, the risk factors for PN include poor glycemic control (ie, elevated glycation hemoglobin levels and impaired glucose tolerance34), age, duration of diabetes, tobacco use, dyslipidemia, and hypertension (especially diastolic) (Table).35 Other independent risk factors for PN include increased height, presence of cardiovascular disease (CVD), presence of severe ketoacidosis (ie, elevated by-products of fat metabolism in the blood), and presence of microalbuminuria (ie, presence of albumin in urine, indicating early renal dysfunction) (Table).36 Unlike that of DR, the pathogenesis of PN appears to be related to both vascular and nonvascular metabolic mechanisms, but this theory is controversial.37–39 For additional information related to the effects of peripheral neuropathy on skin and muscle, see related articles by Mueller et al,40 LeMaster et al,41 and Hilton et al42 in this issue.
Characteristic traits of PN include axonal thickening with progression to axonal loss,43 basement membrane thickening, pericyte loss,44,45 loss of microfilaments (ie, cytoskeletal filaments comprising actin and myosin), and decreased capillary blood flow to C fibers,46 leading to decreased nerve perfusion and endoneurial hypoxia44,45 (Fig. 1). Neuronal microvasculature is impaired in the presence of hyperglycemia,47 and this impairment is mediated through the abnormal initiation of signaling cascades,48,49 potentially leading to the demyelination associated with diabetic PN.50 Both nonvascular and vascular mechanisms of PN appear to be primarily related to the metabolic aspects (ie, hyperglycemia) of diabetes.
Diabetes-related cardiac autonomic neuropathy is frequently underdiagnosed and can include clinical abnormalities such as resting tachycardia, exercise intolerance, resting HR variability, slow HR recovery after exercise, orthostasis, “silent” myocardial infarction, and increased risk of mortality.51,52 The prevalence of diabetes-related cardiac autonomic neuropathy is unclear and has been reported to range from 1% to 90%, depending on the outcome variable.32 Risk factors for diabetes-associated cardiac neuropathy include age, obesity, smoking, poor glycemic control, and hypertension (Table).53
Cardiac autonomic dysfunction in people with diabetes has been associated with diabetic cardiomyopathy, a topic beyond the scope of this article. In brief, people with diabetic cardiomyopathy have diastolic filling and relaxation abnormalities frequently later accompanied by systolic dysfunction and heart failure. It is unclear whether cardiac autonomic dysfunction directly mediates diabetic cardiomyopathy, because many of the same risk factors and mechanisms contribute to the development of both conditions.51
Diabetic Nephropathy
Diabetic nephropathy (DN) is a serious and progressive complication of both type 1 DM and type 2 DM. The first manifestation of DN is typically microalbuminuria, which progresses to overt albuminuria (ie, increased albumin levels in the urine, indicating more severe renal dysfunction) and eventually to renal failure54 and is the leading cause of end-stage renal disease (ESRD).55 Approximately one fourth of people with type 2 diabetes have microalbuminuria or a more advanced stage of DN that worsens at a rate of 2% to 3% per year.56 Other characteristic features of DN include thickening of glomerular basement membranes (Fig. 1) and glomerular hyperfiltration, leading to mesangial (central part of the renal glomerulus) extracellular matrix expansion and further increases in urinary albumin excretion57 and progressing to glomerular and tubular sclerosis and renal failure.58,59 Like those for DR and PN, the risk factors for DN include hyperglycemia, duration of diabetes, age of onset, tobacco use, dyslipidemia, hypertension,60,61 and obesity (Table).62
Macrovascular Complications of Diabetes
Cardiovascular disease (CVD) is the leading cause (∼70%) of death in people with type 2 diabetes.63,64 People with diabetes have a 4-fold-greater risk for having a CVD event than people without diabetes after controlling for traditional risk factors for CVD, such as age, obesity, tobacco use, dyslipidemia, and hypertension.65,66 These CVD risk factors are common in diabetes, but data suggest that diabetes is an independent risk factor for CVD. People with diabetes also have a 5-fold-greater risk for a first myocardial infarction (MI) and a 2-fold-greater risk for a recurrent MI than people who previously had an MI but do not have diabetes. These data suggest that the risk for an MI in people who have diabetes but who have not had an MI is similar to that in people without diabetes but with a previous MI.67 Further, people with diabetes have a poorer long-term prognosis after an MI, including an increased risk for congestive heart failure and death.68 Even people with insulin resistance (ie, the blunted response of tissues [such as muscle, fat, and liver] to insulin that frequently precedes type 2 DM) have an increased risk for CVD.69 Traditionally, diabetes and CVD were limited primarily to Westernized populations. However, recent evidence suggests that these conditions are rapidly emerging in resource-limited regions of the world,70 and estimates indicate that 80% of people with diabetes worldwide will die from CVD.71
People with diabetes (particularly type 2 DM) frequently have many traditional risk factors for CVD, including central obesity, dyslipidemia (ie, elevated serum triglyceride, LDL, and free fatty acid levels and low high-density lipoprotein levels), and hypertension.72 The combination of central adiposity, dyslipidemia, hyperglycemia, and hypertension in the general population is termed “metabolic syndrome.”73 These factors, along with the independent risk factor of diabetes, can act both independently and cumulatively over time to significantly increase risk for CVD. The combination of hyperglycemia, insulin resistance, dyslipidemia, hypertension, and chronic inflammation can injure the vascular endothelium, leading to macrovasculopathy and CVD in people with type 2 DM.74
Cerebrovascular Disease
Stroke is the third leading cause of death in the United States, after CVD and cancer,75 and is an event very familiar to physical therapists. Diabetes is an independent risk factor across all ages76 for stroke; the risk in people with diabetes is up to 2- to 4-fold greater, more so in white people and women.75,77–79 Diabetes is also a risk factor for sudden and eventual death from stroke,80,81 and people who have diabetes and who have a stroke have more severe neurological deficits and disability,82–84 a poorer long-term prognosis,85 and a higher incidence of stroke recurrence than people without diabetes.86
As in CVD, the presence of diabetes adversely affects the cerebrovascular circulation by increasing the risk of intracranial and extracranial (eg, carotid artery) atherosclerosis.87,88 People with diabetes have an increased incidence of traditional risk factors for stroke, including hypertension, dyslipidemia, heart failure, and atrial fibrillation.89 However, after these factors are controlled for, diabetes remains a strong predictor for stroke, suggesting that the presence of diabetes carries an independent risk for stroke apart from the increased presence of traditional risk factors (Table).80
As in other diabetes-related complications, hyperglycemia appears to be a significant factor in stroke. Hyperglycemia is a significant predictor of fatal and nonfatal stroke90 and death from stroke.91 Hyperinsulinemia (ie, elevated blood insulin levels) also appears to be a risk factor for stroke,92,93 although this relationship is still unclear.94 The presence of DR, proteinuria, microalbuminuria, and hyperuricemia (ie, elevated blood uric acid levels) are other diabetes-related factors associated with an increased risk for stroke (Table).91,95,96 Finally, elevated blood levels of chronic inflammatory markers are associated with an increased risk for stroke in people with diabetes.97
Peripheral Artery Disease
Currently in the United States, more than 3.5 million people (African-American > white > Hispanic people) with diabetes have peripheral artery disease (PAD).98 Peripheral artery disease is characterized by occlusion of the lower-extremity arteries,99 which can cause intermittent claudication and pain, especially upon exercise and activity,100 and which can result in functional impairments101 and disability.102 Physical therapists frequently encounter people with diabetes-related PAD because of these functional impairments and because of common events of more severe PAD: foot ulceration and lower-extremity amputation.103 Because people with diabetes are 15 times more likely to have lower-extremity amputation than people without diabetes,104 physical therapists frequently treat people with diabetes-related amputations. As the incidence of diabetes increases, physical therapists will more frequently see, treat, and prescribe exercise for these people. An elevated awareness of PAD is needed among physical therapists because death in people with diabetes and PN is frequently attributed to CVD.105 Moreover, lower-extremity amputation is more common in people with diabetes and PAD than in people without diabetes but with PAD106; these data suggest that physical therapists should carefully assess lower-extremity blood flow (ie, peripheral pulses) and skin integrity for all patients with diabetes, especially those with known PAD.
Peripheral artery disease, like the aforementioned vascular diseases, is related to the duration and severity of diabetes.106,107 Hyperglycemia, specifically, glycation hemoglobin, has been shown to be an independent risk factor for PAD.108 In addition to diabetes, other risk factors for PAD include hypertension, tobacco use, obesity (ie, waist-to-hip ratio), elevated serum fibrinogen levels, dyslipidemia, a history of CVD, and physical inactivity (Table).109,110
Common Mechanisms for Microvascular and Macrovascular Diseases in Diabetes
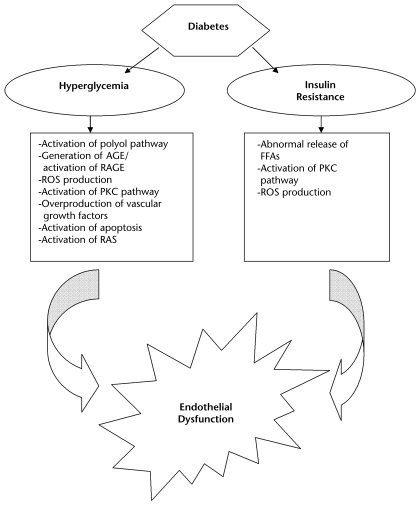
One common pathogenic mechanism for microvascular disease is rooted in chemical reactions between by-products of sugars and proteins that occur over the course of days to weeks and eventually produce irreversible cross-linked protein derivatives called AGE.111 These derivatives can exhibit a wide range of effects on surrounding tissues, including modification (eg, thickening) of collagen112 and endothelium.113 Specifically, in DR, AGE can induce growth inhibition and programmed cell death (ie, apoptosis) of retinal pericytes,114 induce overproduction of endothelial growth factors (including vascular endothelial growth factor, insulin-like growth factor 1, basic fibroblast growth factor, and hepatocyte growth factor),115,116 increase pathologic angiogenesis (neovascularization),117 and increase vascular inflammation118; all of these actions lead to an increased risk for microthrombosis formation, capillary blockage, and retinal ischemia.119 Neovascularization, vitreous hemorrhage, and increased levels of vascular endothelial growth factor can further lead to retinal fibrosis and detachment and loss of vision.12 In addition, AGE can bind to immunoglobulin protein receptors for AGE and produce a cascade of signaling events that lead to endothelial cell dysfunction120 (Fig. 3).
Figure 3.
Potential mechanisms for diabetes-associated endothelial dysfunction. AGE=advanced glycation end products, RAGE=receptors for AGE, ROS=reactive oxygen species, PKC=protein kinase C, RAS=renin-angiotensin system, FFA=free fatty acid.
Advanced glycation end products also play a role in DN through AGE-mediated programmed cell death of mesangial cells and altered extracellular matrix proteins that appear to contribute to both glomerular hyperfiltration116 and sclerosis.121 The formation of AGE also may stimulate the oversecretion of growth factors such as insulin-like growth factor 1 and transforming growth factor β and further contribute to glomerular fibrosis,122 leading to a decrease in available glomerular surface area for filtration.123
Other mechanisms involved in microvascular disease include the PKC pathway (a family of multifunctional enzymes involved in signal transduction and gene expression of growth factors and inflammatory signals124 that may increase vascular permeability) and the polyol pathway (the enzymes aldose reductase and sorbitol dehydrogenase, which catalyze reactions that can lead to sorbitol accumulation-associated osmotic and oxidative stress damage to the endothelium125) (Fig. 3). Peripheral nerve damage in DN, including neuronal degeneration and impairment of regeneration of thinly myelinated fibers, is also mediated by AGE accumulation, the activation of the polyol and PKC pathways, and the deleterious effects of ROS.126,127
Additionally, the RAS128 plays a role in microvascular disease because it can alter glomerular hemodynamics and mediate sclerosis in DN. Other enzymatic pathways are involved in the development and progression of microvascular disease but are not discussed here. For an in-depth discussion of these pathways, see more detailed reviews.129,130
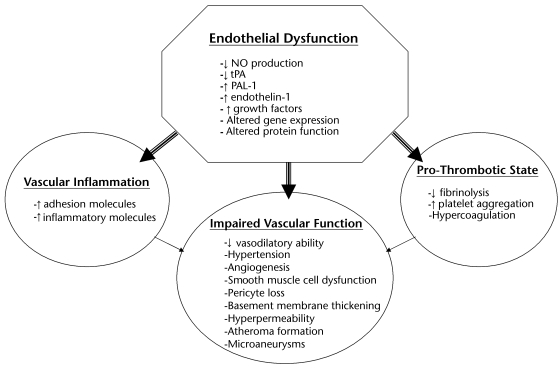
The pathogenesis of macrovascular disease in diabetes is multifactorial; however, the common recipient of injury is the vascular endothelium (Fig. 4). Diabetes initially impairs the ability of the vascular endothelium to vasodilate through inhibition of the nitric oxide (NO, a gas molecule that maintains arteriolar vasodilatation) pathway.131 The presence of hyperglycemia inhibits the enzyme responsible for the production of NO (ie, endothelial nitric oxide synthase [eNOS]) and increases the production of ROS, leading to further inhibition of eNOS.132,133 The vascular endothelium also loses its ability to produce NO-activated tissue plasminogen activator, a fibrinolytic (anti-clotting) protein that inhibits the ability of inflammatory cells to “stick” to the endothelial surface.134 Insulin resistance also can contribute to a decrease in NO production and the subsequent impaired vasodilatory response. In addition, insulin resistance can lead to an increase in the release of free fatty acids from adipose tissue135 and stimulate the PKC pathway, which can directly and indirectly inhibit eNOS activity through increased ROS generation.136 The production of AGE (from hyperglycemia) also inhibits NO production, further impairing the vasodilatory response in diabetes.137 In addition to the reduction in the vasodilatory response in diabetes, an overproduction of vasoconstrictor substances occurs; these substances include endothelin 1, which has direct vasoconstrictive effects on the endothelium as well as indirect fluid volume effects, including the stimulation of water and salt retention and the activation of the RAS.138
Figure 4.
Potential mechanisms for diabetes-associated vascular abnormalities. NO=nitric oxide, tPA-1=tissue plasminogen activator-1, PAI-1=plasminogen activator inhibitor-1.
Another factor involved in the development and progression of macrovascular disease in diabetes is impaired platelet function, which may lead to increased risks for thrombus formation, atherosclerosis progression, and plaque rupture.134 Hyperglycemia-stimulated PKC pathway effects on NO and ROS generation and diabetes-associated impaired fibrinolytic capacity may contribute to this increased coagulative state.139,140 Another diabetes-related mechanism for macrovascular disease is a hyperinflammatory state. Inflammatory cells (eg, monocytes and T lymphocytes) enter damaged endothelial cells and migrate into the deeper layers (intima media) of vessels, ingesting oxidized LDL and forming foam cells.141 Foam cells are the central component of atherosclerotic fatty streaks, an early marker of macrovascular disease (Fig. 2). The levels of adhesion molecules (ie, proteins that recruit inflammatory cells) are also elevated in people with diabetes, thereby facilitating the process of foam cell formation.142 Finally, diabetes is associated with smooth muscle cell dysfunction.74 Although the precise mechanism for smooth muscle cell dysfunction in diabetes is unclear, it may be associated with similar mechanisms for endothelial cell dysfunction, including activation of the PKC pathway, AGE deposition, and AGE receptor activation as well as overproduction of growth factors.136 In the development of atherosclerosis, activated smooth muscle cells in the medial layer of arteries migrate to the atherosclerotic fatty streaks in the intimal layer and produce an extensive extracellular matrix, solidifying the streaks and reciprocally reducing the protective strengthening function in the medial layer, making the atherosclerotic plaque unstable and prone to rupture.143 These hyperglycemia-stimulated events act in conjunction over time to produce atheroma and eventual atherosclerosis.72
Many of the mechanisms for CVD appear to affect the cerebrovasculature in a similar manner, but this theory is under debate.144 However, a unique effect of diabetes on neurons and glial cells occurs during ischemia (such as during a transient ischemic attack or stroke). This relationship has been demonstrated through the relationship between hyperglycemia and increased intracellular acidosis.145 Neuronal intracellular acidosis occurs during an ischemic event as a result of elevated anaerobic metabolism, which leads to neuron and glial cell damage.145,146 Acidosis may induce intracellular damage through ROS generation, intracellular signaling disruption, and activation of DNA-splitting enzymes.146 Hyperglycemia also is associated with increased levels of excitatory amino acids (eg, glutamate), which may induce neuronal cell death through the activation of glutamate receptors, the influx of excess calcium, and mitochondrial (cell energy powerhouse) injury.146,147 This process may lead to a poorer outcome of stroke in people with diabetes.
Role of Physical Therapists in Diabetes-Related Microvascular and Macrovascular Diseases
Diabetes-related comorbidities are conditions that physical therapists will encounter during the evaluation and treatment of movement and functional disorders in people with diabetes. Besides improving movement and function, in general, physical therapists may improve the quality of life for people with diabetes and macrovascular and microvascular diseases through the use of interventions that address pain, poor endurance, obesity, and increased risk for microvascular and macrovascular diseases. Specifically, the prescription and monitoring of an individualized exercise program are essential in a management program, regardless of the severity of diabetes. Exercise therapy may greatly benefit many patients with diabetes by reducing hyperglycemia, insulin resistance, dyslipidemia, and hypertension; these reductions may translate into an improved vascular disease risk profile in children, adolescents, and adults with diabetes.148–150 Exercise also may aid in weight loss, specifically, loss of trunk fat, and also may improve glycemic and lipemic control in people with diabetes.151 Additionally, exercise may improve physical function152 and quality of life in people with diabetes.153 Caution should be observed in patients who have proliferative DR, microalbuminuria, and cardiac autonomic dysfunction and who are starting aerobic exercise programs, because exercise, particularly resistance exercise, increases retinal blood pressure, reduces kidney blood flow, and stresses autonomic control of HR and contractility.154 For additional information related to the metabolic effects of exercise in people with DM, see related articles by Turcotte and Fisher155 and Gulve156 in this issue.
A frequent progression of DN, ESRD, is a significant cause of functional impairments and disability157 in people with diabetes and an area in which physical therapists may play an increasing role in the treatment of these consequences, because exercise training appears to improve functional and work capacities and increase independence in these people.158,159 People with ESRD frequently have a low hematocrit and muscle atrophy,160 which may contribute to their reduced exercise capacity and disability.161 An impaired glomerular filtration rate has been associated with low exercise capacity162 and low activity levels.163 Exercise training has been shown to improve markers of DN, specifically decreasing microalbuminuria.164
Peripheral artery disease is another condition that physical therapists frequently encounter in patients with diabetes. The clinical evaluation of PAD in people with diabetes commonly involves palpating for peripheral arterial pulses, but this technique has been shown to have poor accuracy for the determination of PAD.165 The ankle brachial index (ABI), a sensitive and specific test for determining PAD,166 is performed by measuring systolic blood pressure in the upper (brachial artery) and lower (dorsalis pedis and posterior tibialis arteries) extremities with a hand-held Doppler probe and dividing the higher ankle systolic pressure by the higher brachial artery pressure.167 An ABI of less than 0.90 is predictive of PAD, and an ABI of less than 0.50 is associated with impaired physical function (such as walking distance).166 Although a Doppler probe is not commonly used in the physical therapy setting, clinics that frequently treat people with diabetes-associated PAD may benefit from using this relatively inexpensive tool because it may provide diagnostic and treatment monitoring criteria. Other clinical testing in patients with diabetes-associated PAD may include treadmill testing168 or the 6-minute walk test169 to determine walking capacity and time to claudication and pain, if present. Supervised exercise training in people with PAD has been shown to be highly beneficial in terms of walking distance and time, time to claudication and pain, and quality of life170,171; is more effective than pharmacologic therapy172; and is considered to be first-line therapy in the treatment of PAD.168 Accordingly, physical therapists are becoming first-line treatment providers for patients with diabetes-related PAD and should be strong advocates of exercise treatment for these patients.
The clinical evaluation and treatment of DN, a common condition in the physical therapy setting, require more specificity. The evaluation of diabetic PN in the clinical setting involves a variety of tests, which may include the measurement of peripheral (typically of the lower extremity, such as the foot) light touch and vibration sense as well as nerve biopsy.173 The clinical evaluation of vibration sense, a test frequently used in the physical therapy setting, is the strongest predictor of foot insensitivity ulceration.174 Electrophysiologic nerve conduction testing, occasionally performed in physical therapy clinics but more often performed in physicians’ offices, is considered to be the gold standard for measuring nerve function.175 Nerve biopsy is not considered part of routine clinical testing in DN; however, skin biopsy testing is becoming more frequent in clinics. Skin biopsy testing is minimally invasive and may provide important information, such as nerve density and small-fiber neuropathy,176 and it may be useful in predicting the progression of the disease.177 A newly developed noninvasive technique for assessing the presence of DN is corneal confocal microscopy, with which the density and length of the corneal nerve have been shown to be strongly associated with lower-extremity nerve density and which is gaining in popularity.37 These clinical measurements also may be used to assess the efficacy of specific interventions, including medications, exercise, and weight loss.
Clinical tests to evaluate diabetes-associated cardiac autonomic neuropathy include measurement of resting HR, exercise testing, measurement of blood pressure in response to postural changes (such as moving from a supine position to a standing position), autonomic reflex testing, measurement of 24-hour HR variability, spontaneous baroreflex sensitivity testing, and cardiac radionuclide imaging.51 Several of these tests, including HR and blood pressure responses to exercise and postural changes, can be performed in the physical therapy setting. A resting HR of ≥100 beats per minute is considered to be tachycardia in adults. Orthostatic hypotension is defined as a decrease of greater than 30 mm Hg in systolic blood pressure and a decrease greater than 10 mm Hg in diastolic blood pressure in response to a change from a supine position to a standing position.178 Patients with diabetes-associated cardiac autonomic neuropathy have a blunted HR response to exercise (ie, they do not attain the age-predicted maximal HR) and a slow HR recovery after peak exercise52; the latter is predictive of CVD and all-cause mortality.52 Physical therapists, therefore, may have to rely more on the patient's perceived exertion than on HR responses for exercise prescription.179
Conclusion
Diabetes is associated with both microvascular and macrovascular diseases affecting numerous organs, including skeletal muscle, skin, heart, brain, and kidneys. Common pathogenic mechanisms link the different types of diabetes-associated vascular disease (such as CVD and PAD). Common risk factors for vascular disease in diabetes include hyperglycemia, insulin resistance, dyslipidemia, hypertension, tobacco use, and obesity.
Mechanisms for microvascular disease in diabetes include the pathologic effects of AGE accumulation, overproduction of endothelial growth factors, and abnormal stimulation of the PKC and polyol pathways and the RAS. Mechanisms for macrovascular disease in diabetes include the pathologic effects of AGE accumulation, impaired vasodilatory response attributable to NO inhibition, smooth muscle cell dysfunction, overproduction of endothelial growth factors, chronic inflammation, hemodynamic dysregulation, impaired fibrinolytic ability, and enhanced platelet aggregation (clotting). It is becoming increasingly important for physical therapists to be aware of diabetes-related vascular complications as more patients present with insulin resistance and type 2 DM. The opportunities for effective physical therapy interventions (such as exercise) are significant.
This work was supported by National Institutes of Health grant K0K074343A.
References
- 1.World Health Organization. Diabetes facts. Available at: http://www.who.int/mediacentre/factsheets/fs312/en/index.html. Accessed December 13, 2007.
- 2.World Health Organization. Diabetes action now booklet: a life-threatening condition. Available at: www.who.int/diabetes/BOOKLET_HTML/en/index3.html. Accessed December 13, 2007.
- 3.Hogan P, Dall T, Nikolov P. Economic costs of diabetes in the US in 2002. Diabetes Care. 2003;26:917–932. [DOI] [PubMed] [Google Scholar]
- 4.UK Prospective Diabetes Study (UKPDS). VIII. Study design, progress and performance. Diabetologia. 1991;34:877–890. [PubMed] [Google Scholar]
- 5.Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys Ther. 2008;88:1254–1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rahman S, Rahman T, Ismail AA, Rashid AR. Diabetes-associated macrovasculopathy: pathophysiology and pathogenesis. Diabetes Obes Metab. 2007;9:767–780. [DOI] [PubMed] [Google Scholar]
- 7.Davey Smith G, Bracha Y, Svendsen KH, et al. Incidence of type 2 diabetes in the Randomized Multiple Risk Factor Intervention Trial. Ann Intern Med. 2005;142:313–322. [DOI] [PubMed] [Google Scholar]
- 8.Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–1350. [DOI] [PubMed] [Google Scholar]
- 9.Eriksson J, Franssila-Kallunki A, Ekstrand A, et al. Early metabolic defects in persons at increased risk for non-insulin-dependent diabetes mellitus. N Engl J Med. 1989;321:337–343. [DOI] [PubMed] [Google Scholar]
- 10.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harding S. Extracts from “concise clinical evidence”: diabetic retinopathy. BMJ. 2003;326:1023–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheetz MJ, King GL. Molecular understanding of hyperglycemia's adverse effects for diabetic complications. JAMA. 2002;288:2579–2588. [DOI] [PubMed] [Google Scholar]
- 13.Orchard TJ, Dorman JS, Maser RE, et al. Prevalence of complications in IDDM by sex and duration. Pittsburgh Epidemiology of Diabetes Complications Study II. Diabetes. 1990;39:1116–1124. [DOI] [PubMed] [Google Scholar]
- 14.Kempen JH, O'Colmain BJ, Leske MC, et al. The prevalence of diabetic retinopathy among adults in the United States. Arch Ophthalmol. 2004;122:552–563. [DOI] [PubMed] [Google Scholar]
- 15.Klein R, Klein BE, Moss SE, et al. The Wisconsin epidemiologic study of diabetic retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol. 1984;102:520–526. [DOI] [PubMed] [Google Scholar]
- 16.Klein R, Klein BE, Moss SE, et al. The Wisconsin epidemiologic study of diabetic retinopathy. III. Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Arch Ophthalmol. 1984;102:527–532. [DOI] [PubMed] [Google Scholar]
- 17.Tyrberg M, Melander A, Lövestam-Adrian M, Lindblad U. Retinopathy in subjects with impaired fasting glucose: the NANSY-Eye baseline report. Diabetes Obes Metab. 2007. Jul 21. [Epub ahead of print] [DOI] [PubMed]
- 18.Brazionis L, Rowley K Sr, Itsiopoulos C, et al. Homocysteine and diabetic retinopathy. Diabetes Care. 2008;31:50–56. [DOI] [PubMed] [Google Scholar]
- 19.Romero P, Salvat M, Fernandez J, et al. Renal and retinal microangiopathy after 15 years of follow-up study in a sample of type 1 diabetes mellitus patients. Journal of Diabetes Complications. 2007;21:93–100. [DOI] [PubMed] [Google Scholar]
- 20.Cundiff DK, Nigg CR. Diet and diabetic retinopathy: insights from the Diabetes Control and Complications Trial (DCCT). MedGenMed. 2005;7:3. [PMC free article] [PubMed] [Google Scholar]
- 21.Cusick M, Chew EY, Chan CC, et al. Histopathology and regression of retinal hard exudates in diabetic retinopathy after reduction of elevated serum lipid levels. Ophthalmology. 2003;110:2126–2133. [DOI] [PubMed] [Google Scholar]
- 22.Wilkinson-Berka JL. Diabetes and retinal vascular disorders: role of the renin-angiotensin system. Expert Rev Mol Med. 2004;6:1–18. [DOI] [PubMed] [Google Scholar]
- 23.Yamagishi S, Imaizumi T. Pericyte biology and diseases. Int J Tissue React. 2005;27:125–135. [PubMed] [Google Scholar]
- 24.Rajala U, Pajunpaa H, Koskela P, Keinanen-Kiukaanniemi S. High cardiovascular disease mortality in subjects with visual impairment caused by diabetic retinopathy. Diabetes Care. 2000;23:957–961. [DOI] [PubMed] [Google Scholar]
- 25.Yamagishi S, Kobayashi K, Yamamoto H. Vascular pericytes not only regulate growth, but also preserve prostacyclin-producing ability and protect against lipid peroxide-induced injury of co-cultured endothelial cells. Biochem Biophys Res Commun. 1993;190:418–425. [DOI] [PubMed] [Google Scholar]
- 26.Carlson EC, Audette JL, Veitenheimer NJ, et al. Ultrastructural morphometry of capillary basement membrane thickness in normal and transgenic diabetic mice. Anat Rec A Discov Mol Cell Evol Biol. 2003;271:332–341. [DOI] [PubMed] [Google Scholar]
- 27.Hammes HP. Pericytes and the pathogenesis of diabetic retinopathy. Horm Metab Res. 2005;37(suppl 1):39–43. [DOI] [PubMed] [Google Scholar]
- 28.Henricsson M, Nilsson A, Janzon L, Groop L. The effect of glycaemic control and the introduction of insulin therapy on retinopathy in non-insulin-dependent diabetes mellitus. Diabet Med. 1997;14:123–131. [DOI] [PubMed] [Google Scholar]
- 29.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 30.Kohner EM, Patel V, Rassam SM. Role of blood flow and impaired autoregulation in the pathogenesis of diabetic retinopathy. Diabetes. 1995;44:603–607. [DOI] [PubMed] [Google Scholar]
- 31.Dyck PJ, Kratz KM, Karnes JL, et al. The prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: the Rochester Diabetic Neuropathy Study. Neurology. 1993;43:817–824. [DOI] [PubMed] [Google Scholar]
- 32.Vinik AI, Maser RE, Mitchell BD, Freeman R. Diabetic autonomic neuropathy. Diabetes Care. 2003;26:1553–1579. [DOI] [PubMed] [Google Scholar]
- 33.Boulton AJ. Foot problems in patients with diabetes mellitus. In: Pickup J, Williams G, ed. Textbook of Diabetes. London, United Kingdom: Blackwell Science; 1997:1–58.
- 34.Sumner CJ, Sheth S, Griffin JW, et al. The spectrum of neuropathy in diabetes and impaired glucose tolerance. Neurology. 2003;60:108–111. [DOI] [PubMed] [Google Scholar]
- 35.Dyck PJ, Davies JL, Wilson DM, et al. Risk factors for severity of diabetic polyneuropathy: intensive longitudinal assessment of the Rochester Diabetic Neuropathy Study cohort. Diabetes Care. 1999;22:1479–1486. [DOI] [PubMed] [Google Scholar]
- 36.Tesfaye S, Stevens LK, Stephenson JM, et al. Prevalence of diabetic peripheral neuropathy and its relation to glycaemic control and potential risk factors: the EURODIAB IDDM Complications Study. Diabetologia. 1996;39:1377–1384. [DOI] [PubMed] [Google Scholar]
- 37.Thrainsdottir S, Malik RA, Dahlin LB, et al. Endoneurial capillary abnormalities presage deterioration of glucose tolerance and accompany peripheral neuropathy in man. Diabetes. 2003;52:2615–2622. [DOI] [PubMed] [Google Scholar]
- 38.Yang Q, Kaji R, Takagi T, et al. Abnormal axonal inward rectifier in streptozocin-induced experimental diabetic neuropathy. Brain. 2001;124:1149–1155. [DOI] [PubMed] [Google Scholar]
- 39.Malik RA, Newrick PG, Sharma AK, et al. Microangiopathy in human diabetic neuropathy: relationship between capillary abnormalities and the severity of neuropathy. Diabetologia. 1989;32:92–102. [DOI] [PubMed] [Google Scholar]
- 40.Mueller MJ, Zou D, Bohnert KL, et al. Plantar stresses on the neuropathic foot during barefoot walking. Phys Ther. 2008;88:1375–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.LeMaster JW, Mueller MJ, Reiber GE, et al. Effect of weight-bearing activity on foot ulcer incidence in people with diabetic peripheral neuropathy: Feet First randomized controlled trial. Phys Ther. 2008;88:1385–1398. [DOI] [PubMed] [Google Scholar]
- 42.Hilton TN, Tuttle LJ, Bohnert KL, et al. Excessive adipose tissue infiltration in skeletal muscle in individuals with obesity, diabetes mellitus, and peripheral neuropathy: association with performance and function. Phys Ther. 2008;88:1336–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dyck PJ, Giannini C. Pathologic alterations in the diabetic neuropathies of humans: a review. J Neuropathol Exp Neurol. 1996;55:1181–1193. [DOI] [PubMed] [Google Scholar]
- 44.Ibrahim S, Harris ND, Radatz M, et al. A new minimally invasive technique to show nerve ischaemia in diabetic neuropathy. Diabetologia. 1999;42:737–742. [DOI] [PubMed] [Google Scholar]
- 45.Young MJ, Veves A, Walker MG, Boulton AJ. Correlations between nerve function and tissue oxygenation in diabetic patients: further clues to the aetiology of diabetic neuropathy? Diabetologia. 1992;35:1146–1150. [DOI] [PubMed] [Google Scholar]
- 46.Malik RA, Tesfaye S, Thompson SD, et al. Endoneurial localisation of microvascular damage in human diabetic neuropathy. Diabetologia. 1993;36:454–459. [DOI] [PubMed] [Google Scholar]
- 47.Yagihashi S, Kamijo M, Baba M, et al. Effect of aminoguanidine on functional and structural abnormalities in peripheral nerve of STZ-induced diabetic rats. Diabetes. 1992;41:47–52. [DOI] [PubMed] [Google Scholar]
- 48.Cotter MA, Jack AM, Cameron NE. Effects of the protein kinase C beta inhibitor LY333531 on neural and vascular function in rats with streptozocin-induced diabetes. Clin Sci (Lond). 2002;103:311–321. [DOI] [PubMed] [Google Scholar]
- 49.Nakamura J, Kato K, Hamada Y, et al. A protein kinase C-beta-selective inhibitor ameliorates neural dysfunction in streptozocin-induced diabetic rats. Diabetes. 1999;48:2090–2095. [DOI] [PubMed] [Google Scholar]
- 50.Vlassara H, Brownlee M, Cerami A. Accumulation of diabetic rat peripheral nerve myelin by macrophages increases with the presence of advanced glycosylation end products. J Exp Med. 1984;160:197–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vinik AI, Ziegler D. Diabetic cardiovascular autonomic neuropathy. Circulation. 2007;115:387–397. [DOI] [PubMed] [Google Scholar]
- 52.Cheng YJ, Lauer MS, Earnest CP, et al. Heart rate recovery following maximal exercise testing as a predictor of cardiovascular disease and all-cause mortality in men with diabetes. Diabetes Care. 2003;26:2052–2057. [DOI] [PubMed] [Google Scholar]
- 53.Witte DR, Tesfaye S, Chaturvedi N, et al. Risk factors for cardiac autonomic neuropathy in type 1 diabetes mellitus. Diabetologia. 2005;48:164–171. [DOI] [PubMed] [Google Scholar]
- 54.Drummond K, Mauer M. The early natural history of nephropathy in type 1 diabetes, II: early renal structural changes in type 1 diabetes. Diabetes. 2002;51:1580–1587. [DOI] [PubMed] [Google Scholar]
- 55.Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345:861–869. [DOI] [PubMed] [Google Scholar]
- 56.Adler AI, Stevens RJ, Manley SE, et al. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 2003;63:225–232. [DOI] [PubMed] [Google Scholar]
- 57.Friedman E. Diabetic renal disease. In: Rifkin H, Porte D Jr, eds. Ellenberg and Rifkin's Diabetes Mellitus: Theory and Practice. 4th ed. New York, NY: Elsevier; 1990:684–709.
- 58.Chen S, Hong SW, Iglesias-de la Cruz MC, et al. The key role of the transforming growth factor-beta system in the pathogenesis of diabetic nephropathy. Ren Fail. 2001;23:471–481. [DOI] [PubMed] [Google Scholar]
- 59.van Dijk C, Berl T. Pathogenesis of diabetic nephropathy. Rev Endocr Metab Disord. 2004;5:237–248. [DOI] [PubMed] [Google Scholar]
- 60.Hasslacher C, Ritz E, Wahl P, Michael C. Similar risks of nephropathy in patients with type I or type II diabetes mellitus. Nephrol Dial Transplant. 1989;4:859–863. [DOI] [PubMed] [Google Scholar]
- 61.Linseman DA, Branstetter DG, Yu RL, Aaron CS. Lung tumor induction in A/J mice and clastogenic effects in CD-1 mice of the sequence-selective DNA alkylating agents (+)-CC-1065 and (−)-CC-1065. Nat Toxins. 1995;3:32–40. [DOI] [PubMed] [Google Scholar]
- 62.Kramer H, Luke A, Bidani A, et al. Obesity and prevalent and incident CKD: the Hypertension Detection and Follow-Up Program. Am J Kidney Dis. 2005;46:587–594. [DOI] [PubMed] [Google Scholar]
- 63.Laakso M. Hyperglycemia and cardiovascular disease in type 2 diabetes. Diabetes. 1999;48:937–942. [DOI] [PubMed] [Google Scholar]
- 64.American Heart Association. The heart of diabetes. Available at: http://www.americanheart.org/presenter.jhtml?identifier=3044762. Accessed December 3, 2007.
- 65.Buyken AE, von Eckardstein A, Schulte H, et al. Type 2 diabetes mellitus and risk of coronary heart disease: results of the 10-year follow-up of the PROCAM Study. Eur J Cardiovasc Prev Rehabil. 2007;14:230–236. [DOI] [PubMed] [Google Scholar]
- 66.Bonora E, Formentini G, Calcaterra F, et al. HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects: prospective data from the Verona Diabetes Complications Study. Diabetes Care. 2002;25:1135–1141. [DOI] [PubMed] [Google Scholar]
- 67.Haffner SM, Lehto S, Ronnemaa T, et al. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–234. [DOI] [PubMed] [Google Scholar]
- 68.Malmberg K, Yusuf S, Gerstein HC, et al. Impact of diabetes on long-term prognosis in patients with unstable angina and non-Q-wave myocardial infarction: results of the OASIS (Organization to Assess Strategies for Ischemic Syndromes) Registry. Circulation. 2000;102:1014–1019. [DOI] [PubMed] [Google Scholar]
- 69.Facchini FS, Hua N, Abbasi F, Reaven GM. Insulin resistance as a predictor of age-related diseases. J Clin Endocrinol Metab. 2001;86:3574–3578. [DOI] [PubMed] [Google Scholar]
- 70.Mufunda J, Chatora R, Ndambakuwa Y, et al. Emerging non-communicable disease epidemic in Africa: preventive measures from the WHO Regional Office for Africa. Ethn Dis. 2006;16:521–526. [PubMed] [Google Scholar]
- 71.Turner R, Cull C, Holman R. United Kingdom Prospective Diabetes Study 17: a 9-year update of a randomized, controlled trial on the effect of improved metabolic control on complications in non-insulin-dependent diabetes mellitus. Ann Intern Med. 1996;124:136–145. [DOI] [PubMed] [Google Scholar]
- 72.Reusch JE, Draznin BB. Atherosclerosis in diabetes and insulin resistance. Diabetes Obes Metab. 2007;9:455–463. [DOI] [PubMed] [Google Scholar]
- 73.Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–2497. [DOI] [PubMed] [Google Scholar]
- 74.Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287:2570–2581. [DOI] [PubMed] [Google Scholar]
- 75.Centers for Disease Control and Prevention. Stroke. Available at: http://www.cdc.gov/stroke/. Accessed January 5, 2008.
- 76.Abbott RD, Curb JD, Rodriguez BL, et al. Age-related changes in risk factor effects on the incidence of thromboembolic and hemorrhagic stroke. J Clin Epidemiol. 2003;56:479–486. [DOI] [PubMed] [Google Scholar]
- 77.Ohira T, Shahar E, Chambless LE, et al. Risk factors for ischemic stroke subtypes: the Atherosclerosis Risk in Communities Study. Stroke. 2006;37:2493–2498. [DOI] [PubMed] [Google Scholar]
- 78.Folsom AR, Rasmussen ML, Chambless LE, et al. Prospective associations of fasting insulin, body fat distribution, and diabetes with risk of ischemic stroke: the Atherosclerosis Risk in Communities (ARIC) Study Investigators. Diabetes Care. 1999;22:1077–1083. [DOI] [PubMed] [Google Scholar]
- 79.Rohr J, Kittner S, Feeser B, et al. Traditional risk factors and ischemic stroke in young adults: the Baltimore-Washington Cooperative Young Stroke Study. Arch Neurol. 1996;53:603–607. [DOI] [PubMed] [Google Scholar]
- 80.Tuomilehto J, Rastenyte D, Jousilahti P, et al. Diabetes mellitus as a risk factor for death from stroke: prospective study of the middle-aged Finnish population. Stroke. 1996;27:210–215. [DOI] [PubMed] [Google Scholar]
- 81.Haheim LL, Holme I, Hjermann I, Leren P. Nonfasting serum glucose and the risk of fatal stroke in diabetic and nondiabetic subjects: 18-year follow-up of the Oslo Study. Stroke. 1995;26:774–777. [DOI] [PubMed] [Google Scholar]
- 82.Ribo M, Molina C, Montaner J, et al. Acute hyperglycemia state is associated with lower tPA-induced recanalization rates in stroke patients. Stroke. 2005;36:1705–1709. [DOI] [PubMed] [Google Scholar]
- 83.Parsons MW, Barber PA, Desmond PM, et al. Acute hyperglycemia adversely affects stroke outcome: a magnetic resonance imaging and spectroscopy study. Ann Neurol. 2002;52:20–28. [DOI] [PubMed] [Google Scholar]
- 84.Megherbi SE, Milan C, Minier D, et al. Association between diabetes and stroke subtype on survival and functional outcome 3 months after stroke: data from the European BIOMED Stroke Project. Stroke. 2003;34:688–694. [DOI] [PubMed] [Google Scholar]
- 85.Sprafka JM, Virnig BA, Shahar E, McGovern PG. Trends in diabetes prevalence among stroke patients and the effect of diabetes on stroke survival: the Minnesota Heart Survey. Diabet Med. 1994;11:678–684. [DOI] [PubMed] [Google Scholar]
- 86.Elneihoum AM, Goransson M, Falke P, Janzon L. Three-year survival and recurrence after stroke in Malmo, Sweden: an analysis of stroke registry data. Stroke. 1998;29:2114–2117. [DOI] [PubMed] [Google Scholar]
- 87.Fabris F, Zanocchi M, Bo M, et al. Carotid plaque, aging, and risk factors: a study of 457 subjects. Stroke. 1994;25:1133–1140. [DOI] [PubMed] [Google Scholar]
- 88.Friedlander AH, Maeder LA. The prevalence of calcified carotid artery atheromas on the panoramic radiographs of patients with type 2 diabetes mellitus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:420–424. [DOI] [PubMed] [Google Scholar]
- 89.Stegmayr B, Asplund K. Diabetes as a risk factor for stroke: a population perspective. Diabetologia. 1995;38:1061–1068. [DOI] [PubMed] [Google Scholar]
- 90.Niskanen L, Turpeinen A, Penttila I, Uusitupa MI. Hyperglycemia and compositional lipoprotein abnormalities as predictors of cardiovascular mortality in type 2 diabetes: a 15-year follow-up from the time of diagnosis. Diabetes Care. 1998;21:1861–1869. [DOI] [PubMed] [Google Scholar]
- 91.Sasaki A, Horiuchi N, Hasegawa K, Uehara M. Mortality from coronary heart disease and cerebrovascular disease and associated risk factors in diabetic patients in Osaka District, Japan. Diabetes Res Clin Pract. 1995;27:77–83. [DOI] [PubMed] [Google Scholar]
- 92.Shinozaki K, Naritomi H, Shimizu T, et al. Role of insulin resistance associated with compensatory hyperinsulinemia in ischemic stroke. Stroke. 1996;27:37–43. [DOI] [PubMed] [Google Scholar]
- 93.Zunker P, Schick A, Buschmann HC, et al. Hyperinsulinism and cerebral microangiopathy. Stroke. 1996;27:219–223. [DOI] [PubMed] [Google Scholar]
- 94.Davis TM, Millns H, Stratton IM, et al. Risk factors for stroke in type 2 diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS) 29. Arch Intern Med. 1999;159:1097–1103. [DOI] [PubMed] [Google Scholar]
- 95.Guerrero-Romero F, Rodriguez-Moran M. Proteinuria is an independent risk factor for ischemic stroke in non-insulin-dependent diabetes mellitus. Stroke. 1999;30:1787–1791. [DOI] [PubMed] [Google Scholar]
- 96.Lehto S, Niskanen L, Ronnemaa T, Laakso M. Serum uric acid is a strong predictor of stroke in patients with non-insulin-dependent diabetes mellitus. Stroke. 1998;29:635–639. [DOI] [PubMed] [Google Scholar]
- 97.Engstrom G, Stavenow L, Hedblad B, et al. Inflammation-sensitive plasma proteins, diabetes, and mortality and incidence of myocardial infarction and stroke: a population-based study. Diabetes. 2003;52:442–447. [DOI] [PubMed] [Google Scholar]
- 98.American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care. 2003;26:3333–3341. [DOI] [PubMed] [Google Scholar]
- 99.Kullo IJ, Bailey KR, Kardia SL, et al. Ethnic differences in peripheral arterial disease in the NHLBI Genetic Epidemiology Network of Arteriopathy (GENOA) Study. Vasc Med. 2003;8:237–242. [DOI] [PubMed] [Google Scholar]
- 100.Schainfeld RM. Management of peripheral arterial disease and intermittent claudication. J Am Board Fam Pract. 2001;14:443–450. [PubMed] [Google Scholar]
- 101.Vogt MT, Cauley JA, Kuller LH, Nevitt MC. Functional status and mobility among elderly women with lower extremity arterial disease: the Study of Osteoporotic Fractures. J Am Geriatr Soc. 1994;42:923–929. [DOI] [PubMed] [Google Scholar]
- 102.McDermott MM, Liu K, Greenland P, et al. Functional decline in peripheral arterial disease: associations with the ankle brachial index and leg symptoms. JAMA. 2004;292:453–461. [DOI] [PubMed] [Google Scholar]
- 103.Adler AI, Boyko EJ, Ahroni JH, Smith DG. Lower-extremity amputation in diabetes: the independent effects of peripheral vascular disease, sensory neuropathy, and foot ulcers. Diabetes Care. 1999;22:1029–1035. [DOI] [PubMed] [Google Scholar]
- 104.Dickinson PJ, Carrington AL, Frost GS, Boulton AJ. Neurovascular disease, antioxidants and glycation in diabetes. Diabetes Metab Res Rev. 2002;18:260–272. [DOI] [PubMed] [Google Scholar]
- 105.Forsblom CM, Sane T, Groop PH, et al. Risk factors for mortality in type II (non-insulin-dependent) diabetes: evidence of a role for neuropathy and a protective effect of HLA-DR4. Diabetologia. 1998;41:1253–1262. [DOI] [PubMed] [Google Scholar]
- 106.Jude EB, Oyibo SO, Chalmers N, Boulton AJ. Peripheral arterial disease in diabetic and nondiabetic patients: a comparison of severity and outcome. Diabetes Care. 2001;24:1433–1437. [DOI] [PubMed] [Google Scholar]
- 107.Al-Delaimy WK, Merchant AT, Rimm EB, et al. Effect of type 2 diabetes and its duration on the risk of peripheral arterial disease among men. Am J Med. 2004;116:236–240. [DOI] [PubMed] [Google Scholar]
- 108.Selvin E, Marinopoulos S, Berkenblit G, et al. Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med. 2004;141:421–431. [DOI] [PubMed] [Google Scholar]
- 109.American Heart Association. Peripheral arterial disease risk factors and possible complications. Available at: http://www.americanheart.org/presenter.jhtml?identifier=3020256. Accessed January 5, 2008.
- 110.Wattanakit K, Folsom AR, Selvin E, et al. Risk factors for peripheral arterial disease incidence in persons with diabetes: the Atherosclerosis Risk in Communities (ARIC) Study. Atherosclerosis. 2005;180:389–397. [DOI] [PubMed] [Google Scholar]
- 111.Brownlee M, Cerami A, Vlassara H. Advanced glycosylation end products in tissue and the biochemical basis of diabetic complications. N Engl J Med. 1988;318:1315–1321. [DOI] [PubMed] [Google Scholar]
- 112.Stitt AW, Jenkins AJ, Cooper ME. Advanced glycation end products and diabetic complications. Expert Opin Investig Drugs. 2002;11:1205–1223. [DOI] [PubMed] [Google Scholar]
- 113.Giardino I, Edelstein D, Brownlee M. Nonenzymatic glycosylation in vitro and in bovine endothelial cells alters basic fibroblast growth factor activity: a model for intracellular glycosylation in diabetes. J Clin Invest. 1994;94:110–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Yamagishi S, Hsu CC, Taniguchi M, et al. Receptor-mediated toxicity to pericytes of advanced glycosylation end products: a possible mechanism of pericyte loss in diabetic microangiopathy. Biochem Biophys Res Commun. 1995;213:681–687. [DOI] [PubMed] [Google Scholar]
- 115.Campochiaro PA. Retinal and choroidal neovascularization. J Cell Physiol. 2000;184:301–310. [DOI] [PubMed] [Google Scholar]
- 116.Yamagishi S, Amano S, Inagaki Y, et al. Advanced glycation end products-induced apoptosis and overexpression of vascular endothelial growth factor in bovine retinal pericytes. Biochem Biophys Res Commun. 2002;290:973–978. [DOI] [PubMed] [Google Scholar]
- 117.Benjamin LE, Hemo I, Keshet E. A plasticity window for blood vessel remodelling is defined by pericyte coverage of the preformed endothelial network and is regulated by PDGF-B and VEGF. Development. 1998;125:1591–1598. [DOI] [PubMed] [Google Scholar]
- 118.Chibber R, Ben-Mahmud BM, Chibber S, Kohner EM. Leukocytes in diabetic retinopathy. Curr Diabetes Rev. 2007;3:3–14. [DOI] [PubMed] [Google Scholar]
- 119.Boeri D, Maiello M, Lorenzi M. Increased prevalence of microthromboses in retinal capillaries of diabetic individuals. Diabetes. 2001;50:1432–1439. [DOI] [PubMed] [Google Scholar]
- 120.Schmidt AM, Stern DM. RAGE: a new target for the prevention and treatment of the vascular and inflammatory complications of diabetes. Trends Endocrinol Metab. 2000;11:368–375. [DOI] [PubMed] [Google Scholar]
- 121.Silbiger S, Crowley S, Shan Z, et al. Nonenzymatic glycation of mesangial matrix and prolonged exposure of mesangial matrix to elevated glucose reduces collagen synthesis and proteoglycan charge. Kidney Int. 1993;43:853–864. [DOI] [PubMed] [Google Scholar]
- 122.Matsumura T, Yamagishi S, Brownlee M. Advanced glycation end products and the pathogenesis of diabetic complications. In: LeRoith D, Taylor S, Olefsky JM, eds. Diabetes Mellitus: A Fundamental and Clinical Text. Philadelphia, PA: Lippincott Williams & Wilkins; 2000:983–991.
- 123.Osterby R, Parving HH, Nyberg G, et al. A strong correlation between glomerular filtration rate and filtration surface in diabetic nephropathy. Diabetologia. 1988;31:265–270. [DOI] [PubMed] [Google Scholar]
- 124.Spranger J, Osterhoff M, Reimann M, et al. Loss of the antiangiogenic pigment epithelium-derived factor in patients with angiogenic eye disease. Diabetes. 2001;50:2641–2645. [DOI] [PubMed] [Google Scholar]
- 125.Kinoshita JH, Nishimura C. The involvement of aldose reductase in diabetic complications. Diabetes Metab Rev. 1988;4:323–337. [DOI] [PubMed] [Google Scholar]
- 126.Sima AA. New insights into the metabolic and molecular basis for diabetic neuropathy. Cell Mol Life Sci. 2003;60:2445–2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Vincent AM, Feldman EL. New insights into the mechanisms of diabetic neuropathy. Rev Endocr Metab Disord. 2004;5:227–236. [DOI] [PubMed] [Google Scholar]
- 128.Gilbert RE, Krum H, Wilkinson-Berka J, Kelly DJ. The renin-angiotensin system and the long-term complications of diabetes: pathophysiological and therapeutic considerations. Diabet Med. 2003;20:607–621. [DOI] [PubMed] [Google Scholar]
- 129.Yamagishi S, Imaizumi T. Diabetic vascular complications: pathophysiology, biochemical basis and potential therapeutic strategy. Curr Pharm Des. 2005;11:2279–2299. [DOI] [PubMed] [Google Scholar]
- 130.Girach A, Manner D, Porta M. Diabetic microvascular complications: can patients at risk be identified? A review. Int J Clin Pract. 2006;60:1471–1483. [DOI] [PubMed] [Google Scholar]
- 131.Williams SB, Cusco JA, Roddy MA, et al. Impaired nitric oxide-mediated vasodilation in patients with non-insulin-dependent diabetes mellitus. J Am Coll Cardiol. 1996;27:567–574. [DOI] [PubMed] [Google Scholar]
- 132.De Vriese AS, Verbeuren TJ, Van de Voorde J, et al. Endothelial dysfunction in diabetes. Br J Pharmacol. 2000;130:963–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Milstien S, Katusic Z. Oxidation of tetrahydrobiopterin by peroxynitrite: implications for vascular endothelial function. Biochem Biophys Res Commun. 1999;263:681–684. [DOI] [PubMed] [Google Scholar]
- 134.Grant PJ. Diabetes mellitus as a prothrombotic condition. J Intern Med. 2007;262:157–172. [DOI] [PubMed] [Google Scholar]
- 135.Hennes MM, O'Shaughnessy IM, Kelly TM, et al. Insulin-resistant lipolysis in abdominally obese hypertensive individuals: role of the renin-angiotensin system. Hypertension. 1996;28:120–126. [DOI] [PubMed] [Google Scholar]
- 136.Inoguchi T, Li P, Umeda F, et al. High glucose level and free fatty acid stimulate reactive oxygen species production through protein kinase C–dependent activation of NAD(P)H oxidase in cultured vascular cells. Diabetes. 2000;49:1939–1945. [DOI] [PubMed] [Google Scholar]
- 137.Linden E, Cai W, He JC, et al. Endothelial dysfunction in patients with chronic kidney disease results from advanced glycation end products (AGE)-mediated inhibition of endothelial nitric oxide synthase through RAGE activation.Clin J Am Soc Nephrol. 2008;3:691–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Rask-Madsen C, King GL. Mechanisms of disease: endothelial dysfunction in insulin resistance and diabetes. Nat Clin Pract Endocrinol Metab. 2007;3:46–56. [DOI] [PubMed] [Google Scholar]
- 139.Assert R, Scherk G, Bumbure A, et al. Regulation of protein kinase C by short- term hyperglycaemia in human platelets in vivo and in vitro. Diabetologia. 2001;44:188–195. [DOI] [PubMed] [Google Scholar]
- 140.Carr ME. Diabetes mellitus: a hypercoagulable state. Journal of Diabetes Complications. 2001;15:44–54. [DOI] [PubMed] [Google Scholar]
- 141.Hansson GK, Robertson AK, Soderberg-Naucler C. Inflammation and atherosclerosis. Annu Rev Pathol. 2006;1:297–329. [DOI] [PubMed] [Google Scholar]
- 142.Williams MD, Nadler JL. Inflammatory mechanisms of diabetic complications. Curr Diab Rep. 2007;7:242–248. [DOI] [PubMed] [Google Scholar]
- 143.Suzuki LA, Poot M, Gerrity RG, Bornfeldt KE. Diabetes accelerates smooth muscle accumulation in lesions of atherosclerosis: lack of direct growth-promoting effects of high glucose levels. Diabetes. 2001;50:851–860. [DOI] [PubMed] [Google Scholar]
- 144.Mankovsky BN, Ziegler D. Stroke in patients with diabetes mellitus. Diabetes Metab Res Rev. 2004;20:268–287. [DOI] [PubMed] [Google Scholar]
- 145.Hoxworth JM, Xu K, Zhou Y, et al. Cerebral metabolic profile, selective neuron loss, and survival of acute and chronic hyperglycemic rats following cardiac arrest and resuscitation. Brain Res. 1999;821:467–479. [DOI] [PubMed] [Google Scholar]
- 146.Siesjo BK, Zhao Q, Pahlmark K, et al. Glutamate, calcium, and free radicals as mediators of ischemic brain damage. Ann Thorac Surg. 1995;59:1316–1320. [DOI] [PubMed] [Google Scholar]
- 147.Li PA, Shuaib A, Miyashita H. Hyperglycemia enhances extracellular glutamate accumulation in rats subjected to forebrain ischemia. Stroke. 2000;31:183–192. [DOI] [PubMed] [Google Scholar]
- 148.Giannini C, de Giorgis T, Mohn A, Chiarelli F. Role of physical exercise in children and adolescents with diabetes mellitus. J Pediatr Endocrinol Metab. 2007;20:173–184. [DOI] [PubMed] [Google Scholar]
- 149.O'Gorman DJ, Karlsson HK, McQuaid S, et al. Exercise training increases insulin-stimulated glucose disposal and GLUT4 (SLC2A4) protein content in patients with type 2 diabetes. Diabetologia. 2006;49:2983–2992. [DOI] [PubMed] [Google Scholar]
- 150.Sato Y, Nagasaki M, Kubota M, et al. Clinical aspects of physical exercise for diabetes/metabolic syndrome. Diabetes Res Clin Pract. 2007;77(suppl 1):S87–S91. [DOI] [PubMed] [Google Scholar]
- 151.Ivy JL. Role of exercise training in the prevention and treatment of insulin resistance and non-insulin-dependent diabetes mellitus. Sports Med. 1997;24:321–336. [DOI] [PubMed] [Google Scholar]
- 152.Bruce DG, Davis WA, Davis TM. Longitudinal predictors of reduced mobility and physical disability in patients with type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care. 2005;28:2441–2447. [DOI] [PubMed] [Google Scholar]
- 153.Smith DW, McFall SL. The relationship of diet and exercise for weight control and the quality of life gap associated with diabetes. J Psychosom Res. 2005;59:385–392. [DOI] [PubMed] [Google Scholar]
- 154.Wallberg-Henriksson H, Rincon J, Zierath JR. Exercise in the management of non-insulin-dependent diabetes mellitus. Sports Med. 1998;25:25–35. [DOI] [PubMed] [Google Scholar]
- 155.Turcotte LP, Fisher JS. Skeletal muscle insulin resistance: roles of fatty acid metabolism and exercise. Phys Ther. 2008;88:1279–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Gulve EA. Exercise and glycemic control in diabetes: benefits, challenges, and adjustments to pharmacotherapy. Phys Ther. 2008;88:1297–1321. [DOI] [PubMed] [Google Scholar]
- 157.Fried LF, Lee JS, Shlipak M, et al. Chronic kidney disease and functional limitation in older people: health, aging and body composition study. J Am Geriatr Soc. 2006;54:750–756. [DOI] [PubMed] [Google Scholar]
- 158.Tawney KW, Tawney PJ, Kovach J. Disablement and rehabilitation in end-stage renal disease. Semin Dial. 2003;16:447–452. [DOI] [PubMed] [Google Scholar]
- 159.Boyce ML, Robergs RA, Avasthi PS, et al. Exercise training by individuals with predialysis renal failure: cardiorespiratory endurance, hypertension, and renal function. Am J Kidney Dis. 1997;30:180–192. [DOI] [PubMed] [Google Scholar]
- 160.Johansen KL, Shubert T, Doyle J, et al. Muscle atrophy in patients receiving hemodialysis: effects on muscle strength, muscle quality, and physical function. Kidney Int. 2003;63:291–297. [DOI] [PubMed] [Google Scholar]
- 161.Moore GE, Brinker KR, Stray-Gundersen J, Mitchell JH. Determinants of VO2peak in patients with end-stage renal disease: on and off dialysis. Med Sci Sports Exerc. 1993;25:18–23. [DOI] [PubMed] [Google Scholar]
- 162.McManus D, Shlipak M, Ix JH, et al. Association of cystatin C with poor exercise capacity and heart rate recovery: data from the Heart and Soul Study. Am J Kidney Dis. 2007;49:365–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Finkelstein J, Joshi A, Hise MK. Association of physical activity and renal function in subjects with and without metabolic syndrome: a review of the Third National Health and Nutrition Examination Survey (NHANES III). Am J Kidney Dis. 2006;48:372–382. [DOI] [PubMed] [Google Scholar]
- 164.Lazarevic G, Antic S, Vlahovic P, et al. Effects of aerobic exercise on microalbuminuria and enzymuria in type 2 diabetic patients. Ren Fail. 2007;29:199–205. [DOI] [PubMed] [Google Scholar]
- 165.Brearley S, Shearman CP, Simms MH. Peripheral pulse palpation: an unreliable physical sign. Ann R Coll Surg Engl. 1992;74:169–171. [PMC free article] [PubMed] [Google Scholar]
- 166.McDermott MM, Greenland P, Liu K, et al. The ankle brachial index is associated with leg function and physical activity: the Walking and Leg Circulation Study. Ann Intern Med. 2002;136:873–883. [DOI] [PubMed] [Google Scholar]
- 167.Criqui MH, Denenberg JO, Bird CE, et al. The correlation between symptoms and non-invasive test results in patients referred for peripheral arterial disease testing. Vasc Med. 1996;1:65–71. [DOI] [PubMed] [Google Scholar]
- 168.Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary—a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006;47:1239–1312. [DOI] [PubMed] [Google Scholar]
- 169.Greig C, Butler F, Skelton D, et al. Treadmill walking in old age may not reproduce the real life situation. J Am Geriatr Soc. 1993;41:15–18. [DOI] [PubMed] [Google Scholar]
- 170.Gardner AW, Katzel LI, Sorkin JD, et al. Exercise rehabilitation improves functional outcomes and peripheral circulation in patients with intermittent claudication: a randomized controlled trial. J Am Geriatr Soc. 2001;49:755–762. [DOI] [PubMed] [Google Scholar]
- 171.Regensteiner JG, Steiner JF, Hiatt WR. Exercise training improves functional status in patients with peripheral arterial disease. J Vasc Surg. 1996;23:104–115. [DOI] [PubMed] [Google Scholar]
- 172.Dawson DL, Cutler BS, Meissner MH, Strandness DE Jr. Cilostazol has beneficial effects in treatment of intermittent claudication: results from a multicenter, randomized, prospective, double-blind trial. Circulation. 1998;98:678–686. [DOI] [PubMed] [Google Scholar]
- 173.Boulton AJ. Diabetic neuropathy: classification, measurement and treatment. Curr Opin Endocrinol Diabetes Obes. 2007;14:141–145. [DOI] [PubMed] [Google Scholar]
- 174.Garrow AP, Boulton AJ. Vibration perception threshold: a valuable assessment of neural dysfunction in people with diabetes. Diabetes Metab Res Rev. 2006;22:411–419. [DOI] [PubMed] [Google Scholar]
- 175.Boulton AJ, Malik RA, Arezzo JC, Sosenko JM. Diabetic somatic neuropathies. Diabetes Care. 2004;27:1458–1486. [DOI] [PubMed] [Google Scholar]
- 176.Boulton AJ. Treatment of prediabetic neuropathy. Curr Diab Rep. 2006;6:415–416. [DOI] [PubMed] [Google Scholar]
- 177.Gibbons CH, Griffin JW, Polydefkis M, et al. The utility of skin biopsy for prediction of progression in suspected small fiber neuropathy. Neurology. 2006;66:256–258. [DOI] [PubMed] [Google Scholar]
- 178.The definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. J Auton Nerv Syst. 1996;58:123–124. [DOI] [PubMed] [Google Scholar]
- 179.Colberg SR, Swain DP, Vinik AI. Use of heart rate reserve and rating of perceived exertion to prescribe exercise intensity in diabetic autonomic neuropathy. Diabetes Care. 2003;26:986–990. [DOI] [PubMed] [Google Scholar]