Abstract
In recent years patients with respiratory diseases use various devices, which help the removal of mucus from the airways and the improvement of pulmonary function. The aim of the present study is to determine the effectiveness of the current devices of respiratory physiotherapy, as it comes from the review of literature. The current devices of physiotherapy for patients with respiratory diseases, are presented as an alternative therapy method or a supplemental therapy and they can motivate patients to apply therapy by themselves. These devices seem to increase patients' compliance to daily treatment, because they present many benefits, as independent application, full control of therapy and easy use. These devices are the Positive Expiratory Pressure, the High Frequency Chest Wall Oscillation, the Oral High Frequency Oscillation, the Intrapulmonary Percussive Ventilation, the Incentive Spirometry the Flutter and the Acapella and the Cornet. Current devices seem to be effective in terms of mucus expectoration and pulmonary function improvement, as it is shown by published studies. The choice of the suitable device for each patient is a challenge for the physiotherapist in order to achieve better compliance in daily treatment. More controlled studies are needed due to the fact that the number of published studies is limited.
Keywords: devices of respiratory physiotherapy, respiratory physiotherapy, clearance of bronchi, chronic respiratory diseases
Chest physiotherapy (CPT) with bronchial drainage is the standard treatment for mobilization and removal of airway secretions in many types of respiratory dysfunction especially in chronic lung disease, such as cystic fibrosis, brochiectasis, bronchitis, bronchial asthma, primary ciliary dyskinesia syndrome. CPT has been shown to be effective in maintaining pulmonary function and prevention or reduction of respiratory complications in patients with chronic respiratory diseases1–4.
However, standard CPT is very labor–intensive and time–consuming both for hospitalized and non-hospitalized patients with impaired airway clearance. For this reason many patients refuse to do daily physiotherapy and interrupt it with all bad consequences.
In recent years, devices of respiratory physiotherapy have emerged which offer alternatives to standard CPT which are less time–consuming and offer greater independence to the patient with chronic lung disease. According to recent literature, devices of respiratory physiotherapy are introduced as alternative therapy methods5–8 in order to facilitate and improve mobilization of mucus from airways, through which better lung ventilation and improved pulmonary function can be achieved. These devices are safe and offer acceptable airway clearance to conventional CPT.
Patients with chronic respiratory diseases prefer to use devices of respiratory physiotherapy because of their benefits, such as the independent application and the reduced cost of therapy. Aerosol treatments may be given while the patient is using these devices, if needed. The current devices of respiratory physiotherapy are: Positive Expiratory Pressure, High Frequency Chest Wall Oscillation, Oral High Frequency Oscillation, Intrapulmonary Percussive Ventilation, Incentive Spirometry and the Flutter device.
Positive Expiratory Pressure (PEP) device
Positive expiratory pressure (PEP) therapy was developed in the 1970s and has been introduced in the United States as an alternative to conventional physiotherapy9,10.
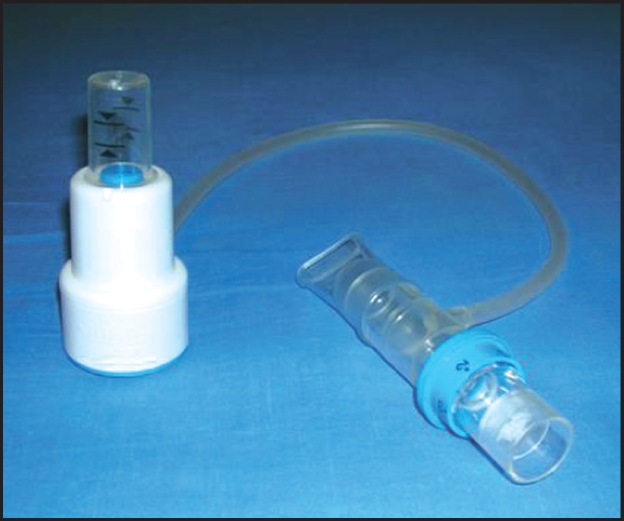
The device consists of (Figures1,2): a face–mask or mouthpiece, a one–way valve, to which expiratory resistances can be attached and a manometer between the valve and the resistance, to monitor the actual value of pressure, which should be between 10 and 20 cm H2O during mid–expiration10–12.
Figure 1: Positive expiratory pressure (PEP) – mask.

Figure 2: Positive expiratory pressure Thera–PEP.
This device is considered to allow more air to enter peripheral airways via collateral channels, to allow pressure air to go behind secretions, moving them towards larger airways where they can easily be expelled and to prevent the alveoli from collapsing8,13,14–16.
Application: Patient must be able to perform certain manoeuvres in an upright or sitting position. The patient slowly inspires to vital capacity and then holds his breath for about 3 seconds. Then slowly exhales through the mouthpiece with the fixed orifice resister that is usually set to create an expiratory pressure resistance between 10–20 cm H2O. This slow deep breathing manoeuvre is repeated anywhere from 10 to 20 times. Then a "huff" or a forced exhalation should follow to clean secretions that have been mobilized. Periods for relaxation and breathing control for about 1–2 minutes are necessary17,18. Full expiration should be avoided. Therapy duration and frequency are adjusted according to individual's needs19. Treatment is usually performed for about 15–20 minutes twice a day in patient with stable clinical condition12.
PEP device may give independence to patients with chronic respiratory diseases, as it can be carried out without an assistant and is easy and convenient in use20–22. Small clinical studies have reported improved tracheobronchial clearance and patient comfort with PEP devices compared to standard CPT23,24. Reduction in pulmonary infections/antibiotic courses and improved bronchodilation is also reported24–26. In addition, there has also been reported improvement in compliance and shorter hospital stays27. Other studies report PEP as an acceptable and effective treatment regimen to lung function8,16,28.
High Frequency Chest Wall Oscillation (HFCWO) device
HFCWO is performed with a mechanical device (ThAIRaphy® bronchial drainage system, Hayek Oscillator). During HFCWO, positive pressure air pulses are applied to the chest wall, for example by means of an inflatable vest and an air pulse generator (Figures 3,4). The generator produces pressures of about 50 cm H2O at a frequency of around 525 Hz delivered via a pneumatic vest which surrounds the thorax. These air pulses oscillate the chest and the vibrations reportedly cause transient flow increases in the airways, loosening mucus and producing cough like sheer forces29.
Figure 3: High frequency chest wall oscillation device.
Figure 4: Using HFCWO device–Vest.
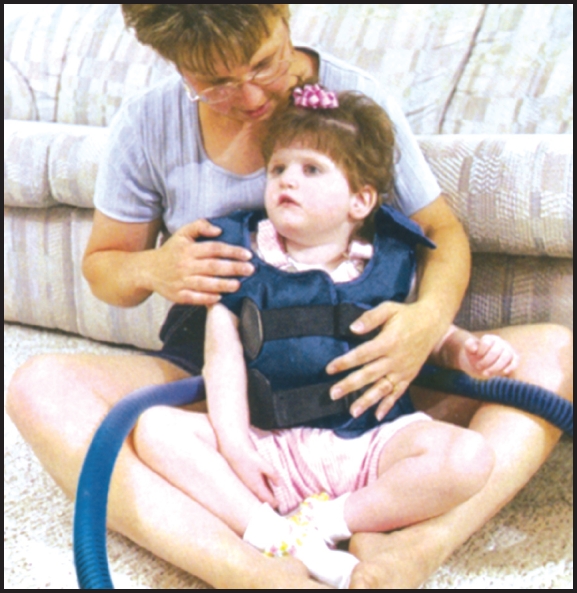
It is hypothesized that increases in cough clearing ability may be due to an increase in mucus/ airflow interaction and/or a shearing mechanism leading to a decrease in the viscoelasticity of mucus30–32. Several studies1–4,33 report that the high frequency chest wall oscillation device: a) provides an adequate physiotherapy method to conventional physiotherapy, b) helps sputum expectoration, c) contributes in stabilization or improvement of respiratory function and d) increases airflow in low lung volumes.
Application: The manufacturers recommend that the patient must undergo this therapy while on upright or sitting position and concomitantly receiving aerosol bronchodilator therapy. The HFCWO treatment is started at low pressures and frequency and then increased to the recommended pressure/frequency as per patient tolerance29.
These therapy sessions generally last about 30 minutes and should not be performed on patients with significant hemoptysis. Despite these restrictions, these devices have been shown to mobilize more secretions than standard CPT in small clinical trials1,31. More research is needed to determine its efficancy, cost benefits and optimum treatment strategies29,34.
Oral High Frequency Oscillation (OHFO) device
Oral high frequency oscillation has been developed from the technique of high frequency jet ventilation. Oscillation of the air within the lungs at high frequency is associated with an increased clearance of CO2. Because of the high frequency and low volume of these oscillations, spontaneous breathing is unhindered and the technique has potential value as a supplement to ventilation35. Sine wave oscillations are produced by an eccentric cam piston or the diaphragm of a loudspeaker and can be superimposed on normal tidal breathing. The low volumes of approximately 48 ml and pressures approximately 0.2 cm–2.0 cm H2O with a mean pressure of zero allow patients to breath spontaneously36,37.
This device provides a practical and simple method of supplementing breathing in conscious subjects, and it may also have application in the management of patients with acute or chronic respiratory failure, where intubation and conventional ventilation might be avoided35.
In normal subjects under laboratory conditions OHFO has been shown that increases mucocilliary clearance38 and reduces minute ventilation35.
Data on the effect on mucociliary clearance of oral high frequency oscillation is conflicting. Nevertheless this device has not been demonstrated to be more effective than other techniques in patients with cystic fibrosis39 or chronic bronchitis40, it may be an alternative for some patients7. Increase in mucociliary clearance in normal man induced by oral high frequency oscillation OHFO has considerable potential in the management of patients with chronic airflow obstruction (CAO), where it may be of value as an assistance to breathing and in the relief of breathlessness41.
This device of chest wall oscillation is widely used in the USA. Direct comparisons with other airway clearance treatments more commonly used in other countries, are difficult to make42.
Intrapulmonary Percussive Ventilation (IPV) device
Intrapulmonary percussive ventilation (IPV) combines aerosol inhalation and internal thoracic percussion applied via a mouthpiece. The IPV is the delivery of a pulsatile flow of gas released with each pulse that can be preset and the pulsation frequency adjusted to each individual43.
Application: The patient initiates the flow of gas and during inspiration the pulsatile flow results in an internal percussion. Interruption of the respiratory flow allows for passive expiration. According to some researchers the device of intrapulmonary percussive ventilation is as effective as «standard» respiratory physical therapy, assists mucus clearance and may be an alternative for some patients6,44,45.
Further studies are need to determine the short–term and long–term goals and to establish the rank of IPV in airway clearance in patients with chronic diseases7,43.
Incentive Spirometry (I.S.) device
Incentive spirometry provides feedback at a preset inspiratory flow of volume of air42 (Figure 5). Incentive Spirometry is designed to mimic natural sighing or yawning by encouraging the patient to take slow, deep breaths. A device called Incentive Spirometer is used to provide information about patient's inspiratory effort by measuring the air flow (FEV1) and the air volume (FVC).
Figure 5: Incentive spirometry device.
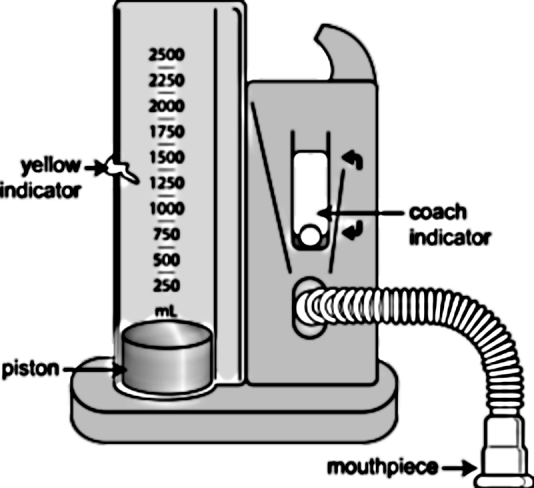
The use of incentive spirometer has been supported to increase or maintain inhaled lung volume, improve sputum expectoration and to avoid serious lung infection, especially after surgery46.
Application: Holding the incentive spirometer upright, patient is encouraged to take a slow and deep breath with his lips sealed around the mouthpiece and is motivated to achieve a preset volume by visual feedback, such as a piston rising to a preset marker. Holding breath for 2–3 sec at full inspiration is very important. Expiration is slow and calm42. After each set of 10 breaths, cough should be encouraged in order to clear the lungs from mucus. It is recommended a repetition of at least ten breaths every hour on the incentive spirometer. The pattern of breathing while using incentive spirometry is important. Emphasis should be given in the expansion of the lower chest during full inspiration, rather than the use of the accessory muscles of respiration, which would encourage expansion of the upper chest. IS has been compared with few of the airway clearance regimens and it is difficult to ascertain its effectiveness42.
There is little evidence to support the use of IS in airway clearance7,47 but it is thought to be an important factor in the reduction or prevention of postoperative pulmonary complications and its use in those patients is frequent. Using incentive spirometer after surgery help keeping lungs clear. Deep inhalations promote the mobilization of secretions and the opening up of lung areas that may have become collapsed. Also it exercises the lungs, keeping them active, especially during the recovery from surgery, as if the patient was at home performing daily activities48. The use of IS appears to improve arterial blood gases and health–related quality of life in patients with COPD exacerbations, although it does not alter pulmonary function parameters46.
Flutter Device
The Flutter device was developed in Switzerland and combines positive expiratory pressure therapy with high–frequency oscillations within the airway29. It is a controlled vibration system which produces positive expiratory pressure and cyclic oscillation of the airways during expiration. The Flutter device is a portable device designed to help clear mucus in patients with lung disorders.
The device consists of a tube based on oscillations of a steel ball during expiration through a pipe–type device47. The principle behind this device is that exhalation into the Flutter valve causes a steel ball–bearing to oscillate at a high frequency, resulting in vibration of the airways and intermittent positive expiratory pressure, to facilitate mucus expectoration29,50 (Figures 6,7).
Figure 6: Flutter device.

Figure 7: Representation of oscillations of the steel ball.
Exhalation through the Flutter results in oscillations of expiratory pressure and airflow, which vibrate the airway walls (loosening mucus), decrease the collapsibility of the airways and accelerate airflow facilitating movement of mucus up the airways and improving lung function and oxygenation5,8,49,51.
Application: Flutter device must be used in the sitting or supine lying position42. The patient is instructed to inhale deeply and hold his breath for 2 to 3 sec. Expiration should be slow8 through the Flutter valve, causing oscillations of the steel ball inside the cone of the Flutter (Figure 8). Patients apply repeated exhalations through the Flutter valve. Routinely, three sets of 15 exhalations are performed over 12–20 min. After each series of exhalations, patients were instructed to "huff" and cough, thereby aiding expectoration19.
Figure 8: Using Flutter device.
The frequency of the oscillations can be modulated by changing the inclination of the Flutter device slightly up or down from its horizontal position (Figure 9). The patient selects the position that results in the best transmission of vibration to chest wall, optimizing the mobilization of mucus19,51.
Figure 9: Holding Flutter device.
Effective use of the Flutter device requires training, concentration, and appropriate positioning of the mouthpiece. The Flutter device is simple to use inexpensive and easily portable and once the patient and his family are instructed in its use it does not require the assistance of a caregiver.
Additionally, patients with severe obstruction may not be able to generate sufficient airflow to cause vibration of the steel ball housed in the pipe–like extension of the Flutter valve, thus limiting the effectiveness of this device in these patients.
Long–term studies of the use of the Flutter seem justified to determine its effects on pulmonary function and outcome5,8,51,52.
For hospitalized patients elimination of the need for a therapist could reduce health care costs53.The Flutter therapy is an acceptable alternative to standard RPT during in–hospital of patients with CF5.
Other devices producing similar effect such as Flutter device, based in different mechanism of oscillations and vibration effect within chest wall can be used by patients with chronic respiratory diseases. These devices are Acapella and Cornet.
Acapella device
The Acapella (Smiths Medical Inc, Carlsbad, California, USA) is a handheld airway clearance device (Figure 10) that operates on the same principle as the Flutter, i.e. a valve interrupting expiratory flow generating oscillating PEP. Utilizing a counterweighted plug and magnet to achieve valve closure, the Acapella is not gravity dependent like the Flutter. The Acapella comes in three models, a low flow (<15 L/min), high flow (>15 L/min) and the Acapella Choice. The high and low flow models have a dial to set expiratory resistance while the Choice model has a numeric dial to adjust frequency. All models can be used with a mask or mouthpiece and can be used in line with a nebulizer. While these attributes may offer the Acapella some advantage over the Flutter, no long–term studies have been done in CF patients. A bench study of the performance characteristics of the two devices showed a slight advantage for the Acapella, with more stable wave form and a wider range of PEP at low air flow 54.
Figure 10: Acapella device.
Cornet device
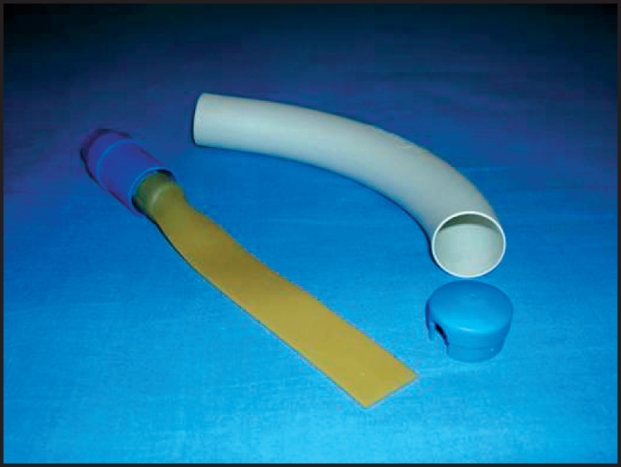
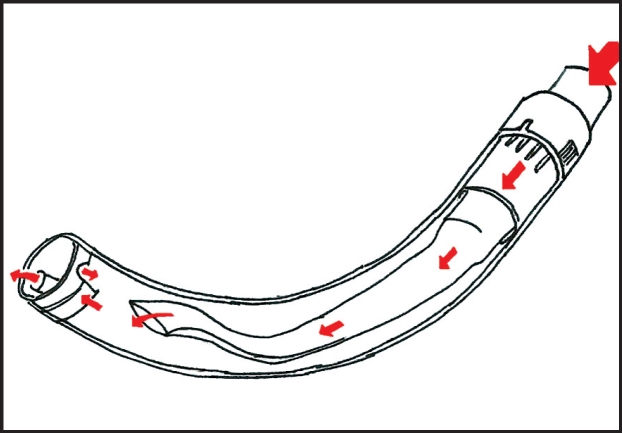
The Cornet device (R. Cegla, Montabaur, Germany) consists of a semi–circular tube containing a flexible latex– free hose (Figure 11). Expiration through the Cornet causes the hose to flex, buckle and unbuckle, causing oscillating positive pressure in the airways which fluctuates many times per second. The mouthpiece can be adjusted to produce the optimal effect. Operating principle and use are similar to the Flutter valve, although the Cornet is not gravity dependent and can be used in any position. Like the Flutter the Cornet cannot be used in line with a nebulizer. No studies showing the long–term effectiveness of the Cornet in CF patients are available yet. The Cornet is available in Europe but not in the USA.
Figure 11: Cornet device.
Critical analysis of Research studies
Sixty eight studies regarding devices of respiratory physiotherapy published to PubMed the last twenty years were studied in order to define their effectiveness. The effectiveness of standard chest physiotherapy (CPT) has been confirmed by many studies. CPT is considered the base of respiratory physiotherapy and is characterized as 'gold standard' of physiotherapy.
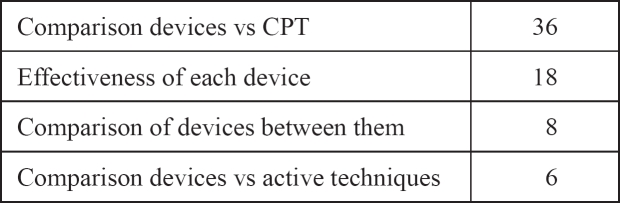
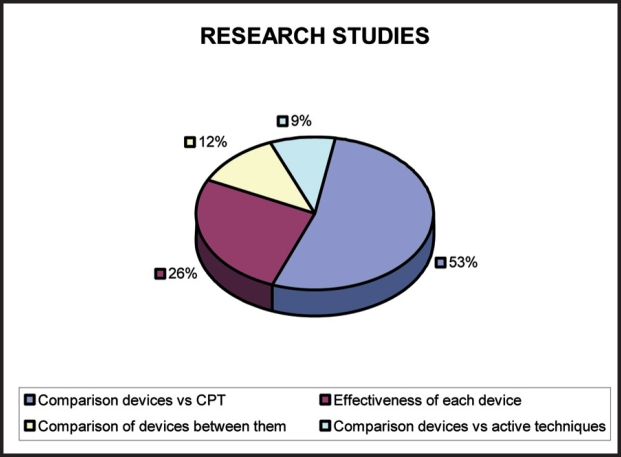
A great number of the published studies (36 studies–percentage 53%) compare the devices of respiratory physiotherapy with standard CPT. Eighteen studies (percentage 26%) are referred to the effectiveness of each device separately, while a small number of reports (8 reports–percentage 12%) compare the devices between them. Limited number of studies compares the devices with other active techniques of respiratory physiotherapy (6 studies–percentage 9%) (Table 1, Figure 13).
Table 1: Published studies.
Figure 13: Percentages of published studies.
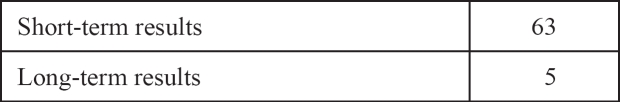
The greater number of published studies (63 studies– percentage 93%) is concerned the short–term effects, while only 5 studies (percentage 7%) were referred to long–term results of devices (Table 2, Figure 14).
Table 2: Results of studies.
Figure 14: Percentages of results of studies.
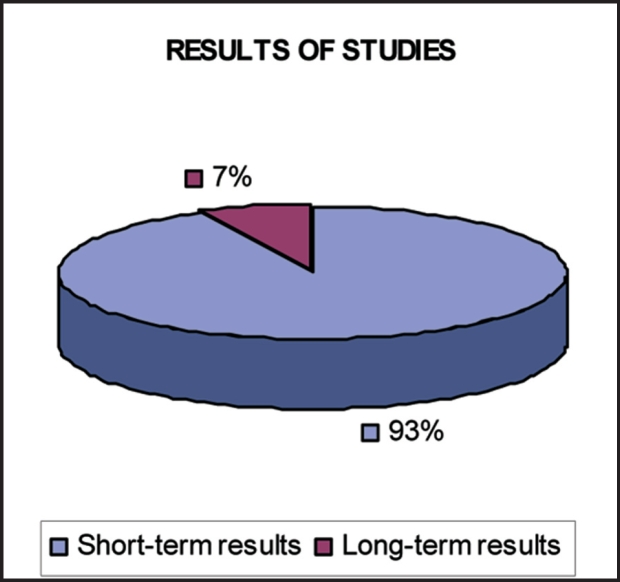
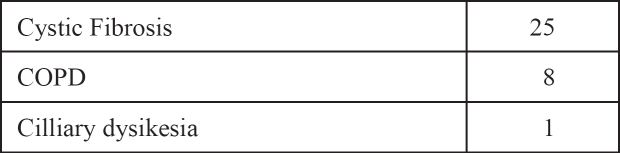
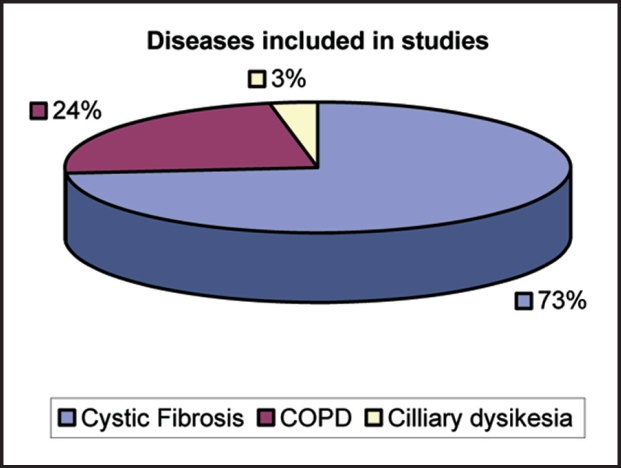
A great number of studies (25 studies– percentage 73%) determine the results of devices in patients with cystic fibrosis. Eight reports (percentage 24%) refer to patients with COPD and only 1 study (percentage 3%) to patients with primary cilliary dyskinesia. (Table 3, Figure 15)
Table 3: Diseases included in studies.
Figure 15: Percentages of diseases included in studies.
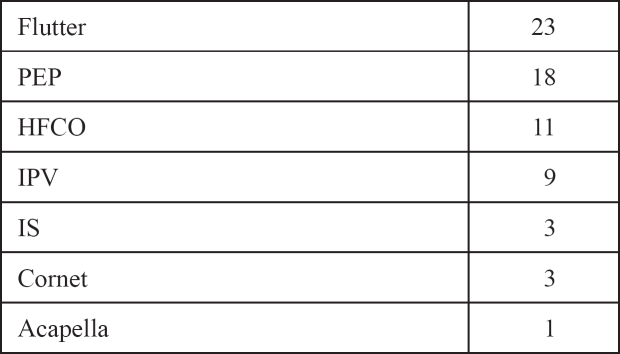
The devices used more often according to published researches are Flutter device (23 studies) percentage 35%, PEP device (18 studies) percentage 27% and HFCWO device (11 studies) percentage 16%. Following the IPV device (9 studies) percentage13% and in the same number of reports the IS device and Cornet device (3 studies) percentage 4%, while the less used device is Acapella device (1 study) percentage 1% (Table 4, Figure 16).
Table 4: Devices.
Figure 16: Percentages of devices.
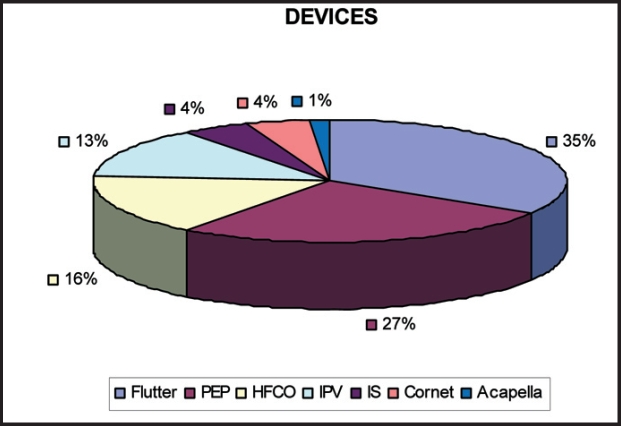
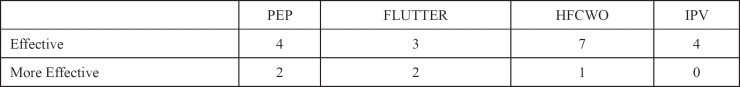
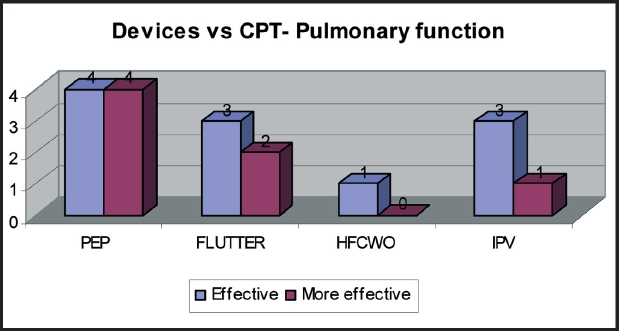
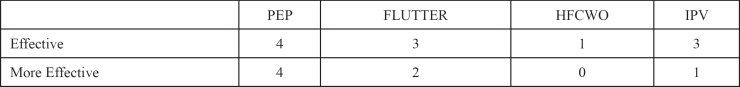
The analysis of research studies that compared devices to standard CPT regarding sputum expectoration and pulmonary function showed that PEP device (2 studies) and Flutter device (2 studies) are superior to standard physiotherapy, while HFCWO device and IPV device are proved to be as effective as standard CPT. Only 1 study reports that HFCWO device is more effective than standard physiotherapy in sputum expectoration (Figure 17, Table 5). Similarly 1 study reports that IPV device is more effective than standard CPT in pulmonary function (Figure 18, Table 6).
Figure 17: Percentages of comparison devices vs CPT- Sputum Expectoration.
Table 5: Comparison devices vs CPT- Sputum Expectoration.
Figure 18: Percentages of comparison devices vs CPT- Pulmonary Function.
Table 6: Comparison devices vs CPT- Pulmonary Function.
Conclusively, according to the results of published studies we support that more research is needed to define the long–term outcomes of the devices of respiratory physiotherapy, to evaluate patients' compliance to therapy and to underline their effect to quality of life. It is difficult to determine which device of respiratory physiotherapy is better since there are no long–term trials that compare the devices between them. Flutter and PEP device are the most popular used devices, even though this is not confirmed by long–term studies, while for the other devices the literature is limited and ambiguous.
Discussion
Stasis of secretions in respiratory diseases leads to chronic infection, inflammation and lung destruction44. Respiratory physiotherapy has been used for many years to help in removal of secretions. However the denial of the patients to do daily physiotherapy especially in chronic obstructive diseases leads to the creation of regimens which provide independent application.
The current respiratory devices have been designed to enhance patients' compliance and independence.
According to the research studies the current devices of respiratory physiotherapy are effective in improving pulmonary function, lung oxygenation, clearing mucus from bronchi and making feasible better compliance of patients in treatment. Also they decrease the respiratory complications1–4,8,35,38,49–51. Furthermore these devices are easy in use and they reduce cost of therapy8.
The number of published reports is limited, though more research is needed to define the effectiveness of the devices of respiratory physiotherapy and their place among the current techniques available.
Physiotherapists should be informed about current devices of respiratory physiotherapy in order to choose the appropriate device for each patient, according to patient's age and clinical condition. Also they should teach patient the direct use of the device and give practical advices. Also the patient must be informed that these devices must not replace the programme of respiratory physiotherapy, because they have a supplemental role to respiratory physiotherapy, contributing to better results in pulmonary function. Alternation of using the devices, according to the patient's condition will give a motivation to the patients in order to continue their treatment.
Figure 12: Representation of oscillations of the latex-free hose.
References
- 1.Arens R, Gozal D, Omlin KJ, et al. Comparison of high–frequency chest compression and conventional chest physiotherapy in hospitalized patients with cystic fibrosis. Am J Respir Crit Care Med. 1994;150:1154–1157. doi: 10.1164/ajrccm.150.4.7921452. [DOI] [PubMed] [Google Scholar]
- 2.Kluft J, Baker L, Castagnino M, Gaiser J, Chaney H, Fink RJ. A comparison of bronchial drainage treatments in cystic fibrosis. Pediatr Pulmonol. 1996;22:271–274. doi: 10.1002/(SICI)1099-0496(199610)22:4<271::AID-PPUL7>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 3.Phillips GE, Pike S, Jaff A, Bush A. Comparison of the active cycle of breathing techniques and external high frequency oscillation jacket for clearance of secretions in children with cystic fibrosis. Thorax. 1998;5(suppl.4):A61. [Google Scholar]
- 4.Warwick WJ, Hansen LG. The long term effect of high frequency compression therapy on pulmonary complications of cystic fibrosis. Pediatr Pulmonol. 1994;88:677–681. doi: 10.1002/ppul.1950110314. [DOI] [PubMed] [Google Scholar]
- 5.Gondor M, Nixon PA, Mutich R, Rebovich P, Orenstein DM. Comparison of flutter device and chest physical therapy in the treatment of cystic fibrosis pulmonary exacerbation. Pediatr Pulmonol. 1999;28:255–260. doi: 10.1002/(sici)1099-0496(199910)28:4<255::aid-ppul4>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 6.Homnick DN, White F, de Castro C. Comparison of effects of an intrapulmonary percussive ventilator to standard aerosol and chest physiotherapy in treatment of cystic fibrosis. Pediatr Pulmonol. 1995;20:50–55. doi: 10.1002/ppul.1950200110. [DOI] [PubMed] [Google Scholar]
- 7.Langenderfer B. Alternatives to percussion and postural drainage. A review of mucus clearance therapies: percussion and postural drainage, autogenic drainage, positive expiratory pressure, flutter valve, intrapulmonary percussive ventilation and high-frequency chest compression with the ThAIRapy Vest. J Cardiopulm Rehabil. 1998;18:283–289. doi: 10.1097/00008483-199807000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Mcllwaine PM, Wong LT, Peacock D, Davidson AG. Long-term comparative trial of positive expiratory pressure versus oscillating positive expiratory pressure (flutter) physiotherapy in the treatment of cystic fibrosis. J Pediatr. 2001;138:845–849. doi: 10.1067/mpd.2001.114017. [DOI] [PubMed] [Google Scholar]
- 9.Aloan AC, Hill VT. Respiratory care of the newborn and child. 2nd ed. Philadelphia: Lippincott; 1997. pp. 391–394. [Google Scholar]
- 10.Gaskin L, Corey M, Shin J, Reisman JJ, Thomas J, Tullis DE. Long–term trial of conventional postural drainage and percussion versus positive expiratory pressure. Pediatr Pulmonol. 1998;(Suppl17):345. [Google Scholar]
- 11.Hofmeyr JL, Webber BA, Hodson ME. Evaluation of positive expiratory pressure as an adjunct to chest physiotherapy in the treatment of cystic fibrosis. Thorax. 1986;41:951–954. doi: 10.1136/thx.41.12.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Falk M, Andersen JB. Positive expiratory pressure (PEP) mask. In: Pryor JA, editor. Respiratory Care. Edinburgh: Churchill Living-stone; 1991. pp. 51–63. [Google Scholar]
- 13.Andersen JB, Qvist J, Kann T. Recruiting collapsed lung through collateral channels with positive end–expiratory pressure. Scand J Respir Dis. 1979;60:260–266. [PubMed] [Google Scholar]
- 14.Darbee JC, Ohtake PJ, Grant BJ, Cerny FJ. Physiologic evidence for the efficacy of positive expiratory pressure as an airway clearance technique in patients with cystic fibrosis. Phys Ther. 2004;84:524–537. [PubMed] [Google Scholar]
- 15.Falk M, Kelstrup M, Andersen JB, et al. Improving the ketchup bottle method with positive expiratory pressure, PEP, in cystic fibrosis. Eur J Respir Dis. 1984;65:423–432. [PubMed] [Google Scholar]
- 16.Mcllwaine PM, Wong LT, Peacock D, Davidson AG. Long-term comparative trial of conventional postural drainage and percussion versus positive expiratory pressure physiotherapy in the treatment of cystic fibrosis. J Pediatr. 1997;131:570–574. doi: 10.1016/s0022-3476(97)70064-7. [DOI] [PubMed] [Google Scholar]
- 17.American Association for Respiratory Care Clinical practice guideline: Use of positive airway pressure adjuncts to bronchial hygiene therapy. Respir Care. 1993;38:516–521. [PubMed] [Google Scholar]
- 18.Malmeister MJ, Fink JB, Hoffman GL, Fifer LF. Positive expiratory pressure mask therapy: theoretical and practical considerations and review of the literature. Respir Care. 1991;36:1218–1229. [Google Scholar]
- 19.Webber AB, Pryor AJ. Physiotherapy for respiratory and cardiac problems. Edinburgh: Churchill Livingstone; 1993. pp. 156–159. [Google Scholar]
- 20.Davidson AGF, Mcllwaine PM, Wong LTK, Nakielma EM, Pirie GE. Comparative trial of positive expiratory pressure, autogenic drainage and conventional percussion and drainage technique. Pediatr Pulmonol. 1988;(Suppl2):132. [Google Scholar]
- 21.Tyrrell JC, Hiller EJ, Martin J. Face mask therapy in cystic fibrosis. Arch Dis Child. 1986;61:598–600. doi: 10.1136/adc.61.6.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elkins MR, Jones A, Van der Shans C. Positive expiratory pressure physiotherapy for airway clearance in people with cystic fibrosis. Cochrane Database Syst Rev. 2006;19 doi: 10.1002/14651858.CD003147.pub3. CD003147. [DOI] [PubMed] [Google Scholar]
- 23.Mortensen J, Falk M, Groth S, Jensen C. The effects of postural drainage and positive expiratory physiotherapy on tracheobronchial clearance in cystic fibrosis. Chest. 1991;100:1350–1357. doi: 10.1378/chest.100.5.1350. [DOI] [PubMed] [Google Scholar]
- 24.Steen HJ, Redmond AO, O'Neill D, Beattie F. Evaluation of the PEP mask in cystic fibrosis. Acta Paediatr Scand. 1991;80:51–56. doi: 10.1111/j.1651-2227.1991.tb11729.x. [DOI] [PubMed] [Google Scholar]
- 25.Plebani A, Pinzani R, Startari R, Brusa D, Padoan R. Usefulness of chest physiotherapy with positive expiratory pressure (PEP)– mask in HIV–infected children with recurrent pulmonary infections. Acta Paediatr. 1997;86:1195–1197. doi: 10.1111/j.1651-2227.1997.tb14844.x. [DOI] [PubMed] [Google Scholar]
- 26.Frischknecht–Christensen E, Norregaard O, Dahl R. Treatment of bronchial asthma with terbutaline inhaled by conespacer combined with positive expiratory pressure mask. Chest. 1991;100:317–321. doi: 10.1378/chest.100.2.317. [DOI] [PubMed] [Google Scholar]
- 27.Oberwaldner B, Theissl B, Rucker A, Zach MS. Chest physiotherapy in hospitalized patients with cystic fibrosis: a study of lung function effects and sputum production. Eur Respir J. 1991;4:152–158. [PubMed] [Google Scholar]
- 28.Christensen EF, Nedergaad T, Dahl R. Long–term treatment of chronic bronchitis with positive expiratory pressure mask and chest physiotherapy. Chest. 1990;97:645–650. doi: 10.1378/chest.97.3.645. [DOI] [PubMed] [Google Scholar]
- 29.Hardy KA. A review of airway clearance: new techniques indications and recommendations. Resp Care. 1994;39:440. [Google Scholar]
- 30.Tomkiewicz RP, Biviji A, King M. Effects of oscillating air flow on the rheological properties and clearability of mucus gel simulaunts. Biorheology. 1994;31:511–520. doi: 10.3233/bir-1994-31501. [DOI] [PubMed] [Google Scholar]
- 31.Majaestic C, Montgomery M, Jones R, King M. Reduction in sputum viscosity using high frequency chest compressions compared to conventional chest physiotherapy. Pediatr Pulmonol. 1996;(Suppl13):A358. [Google Scholar]
- 32.Darbee JC, Kanga JF, Ohtake PJ. Physiologic evidence for high–frequency chest wall oscillation and positive expiratory pressure breathing in hospitalised subjects with cystic fibrosis. Phys Ther. 2005;85:1278–1289. [PubMed] [Google Scholar]
- 33.Phillips GE, Pike SE, Jaffe A, Bush A. Comparison of active cycle of breathing and high–frequency oscillation jacket in children with cystic fibrosis. Pediatr Pulmonol. 2004;37:71–75. doi: 10.1002/ppul.10358. [DOI] [PubMed] [Google Scholar]
- 34.Oermann CM, Sockrider MM, Giles D, Sontag MK, Accurso FJ, Castile RG. Comparison of high–frequency chest wall oscillation and oscillating positive pressure in the home management of cystic fibrosis: a pilot study. Pediatr Pulmonol. 2001;32:372–377. doi: 10.1002/ppul.1146. [DOI] [PubMed] [Google Scholar]
- 35.George RJ, Winter RJ, Johnson MA, Slee IP, Geddes DM. Effect of oral high frequency ventilation by jet or oscillator on minute ventilation in normal subjects. Thorax. 1985;40:749–755. doi: 10.1136/thx.40.10.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pryor JA, Webber BA. Physiotherapy for cystic fibrosis. Physiotherapy. 1992;78:105–108. [Google Scholar]
- 37.Pryor JC. Mucociliary clearance. In: Ellis E, Alison J, editors. Key Issues in cardiorespiratory physiotherapy. Oxford: Butterworth-Heimann; 1992. pp. 105–130. [Google Scholar]
- 38.George RJD, Johnson MA, Pavia D, Agnew JE, Clarke SW, Geddes DM. Increase in mucociliary clearance in normal man induced by oral high frequency oscillation. Thorax. 1985;40:433–437. doi: 10.1136/thx.40.6.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Scherer TA, Barandun J, Martinez E, Wanner A, Rubin EM. Effect of high frequency oral airway and chest wall oscillation and conventional chest physiotherapy on expectoration in patients with stable cystic fibrosis. Chest. 1998;113:1019–1027. doi: 10.1378/chest.113.4.1019. [DOI] [PubMed] [Google Scholar]
- 40.Pryor JA, Wiggins J, Webber BA, Geddes DM. Oral high frequency oscillation (OHFO) as an aid to physiotherapy in chronic bronchitis with airflow limitation. Thorax. 1989;44:350. [Google Scholar]
- 41.George RJ, Winter RJ, Flockton SJ, Geddes DM. Ventilatory saving by external chest wall compression or oral high–frequency oscillation in normal subjects and those with chronic airflow obstruction. Clin Sci. 1985;69:349–359. doi: 10.1042/cs0690349. [DOI] [PubMed] [Google Scholar]
- 42.Pryor JA. Physiotherapy for airway clearance in adults. Eur Respir J. 1999;14:1418–1424. doi: 10.1183/09031936.99.14614189. [DOI] [PubMed] [Google Scholar]
- 43.Natale JE, Pfeifle J, Homnick DN. Comparison of intrapulmonary percussive ventilation and chest physiotherapy: a pilot study in patients with cystic fibrosis. Chest. 1994;105:1789–1793. doi: 10.1378/chest.105.6.1789. [DOI] [PubMed] [Google Scholar]
- 44.Newhouse PA, White F, Marks JH, Homnick DN. The intrapulmonary percussive ventilator and flutter device compared to standard chest physiotherapy in patients with cystic fibrosis. Clin Pediatr. 1998;37:427–432. doi: 10.1177/000992289803700705. [DOI] [PubMed] [Google Scholar]
- 45.Varekojis SM, Douce FH, Flucke RL, et al. A comparison of the therapeutic effectiveness of and preference for postural drainage and percussion, intrapulmonary percussive ventilation, and high–frequency chest wall compression in hospitalized cystic fibrosis patients. Respir care. 2003;48:24–28. [PubMed] [Google Scholar]
- 46.Basoglu OK, Atasever A, Bacakoglu F. The efficacy of incentive spirometry in patients with COPD. Respirology. 2005;10:349–353. doi: 10.1111/j.1440-1843.2005.00716.x. [DOI] [PubMed] [Google Scholar]
- 47.Hall JC, Tarala R, Harris J, Tapper J, Christiansen K. Incentive spirometry versus routine chest physiotherapy for prevention of pulmonary complications after abdominal surgery. Lancet. 1991;337:953–956. doi: 10.1016/0140-6736(91)91580-n. [DOI] [PubMed] [Google Scholar]
- 48.Gosselink R, Schrever K, Cops P, et al. Incentive spirometry does not enhance recovery after thoracic surgery. Crit Care Med. 2000;28:679–683. doi: 10.1097/00003246-200003000-00013. [DOI] [PubMed] [Google Scholar]
- 49.App EM, Kieselman R, Reinhardt D, et al. Sputum rheology changes in cystic fibrosis lung disease following two different types of physiotherapy: flutter vs autogenic drainage. Chest. 1998;114:171–177. doi: 10.1378/chest.114.1.171. [DOI] [PubMed] [Google Scholar]
- 50.Pryor JA, Webber BA. Physiotherapy for cystic fibrosis—which technique? Physiotherapy. 1992;78:105–108. [Google Scholar]
- 51.Konstan MW, Stern RC, Doershuk CF. Efficacy of the Flutter device for airway mucus clearance in patients with cystic fibrosis. J Pediatr. 1994;124:689–693. doi: 10.1016/s0022-3476(05)81356-3. [DOI] [PubMed] [Google Scholar]
- 52.Lindemann H. The valve of physical therapy with VRP 1-Desitin ("Flutter") Pneumologie. 1992;46:626–630. [PubMed] [Google Scholar]
- 53.Homnick DN, Anderson K, Marks JH. Comparison of the flutter device to standard chest physiotherapy in hospitalized patients with cystic fibrosis: a pilot study. Chest. 1998;114:993–997. doi: 10.1378/chest.114.4.993. [DOI] [PubMed] [Google Scholar]
- 54.Volsko TA, Difiore J, Chatburn RL. Performance comparison of two oscillating positive expiratory pressure devices: Acapella versus Flutter. Respir Care. 2003;48:124–130. [PubMed] [Google Scholar]