Abstract
Numerous factors play a part in health disparities. Although health disparities are manifested at the level of the individual, other contexts should be considered when investigating the associations of disparities with clinical outcomes. These contexts include families, neighborhoods, social organizations, and healthcare facilities. This paper reports on health disparities research as a multilevel research domain from the perspective of a large national initiative. The Centers for Population Health and Health Disparities (CPHHD) program was established by the NIH to examine the highly dimensional, complex nature of disparities and their effects on health. Because of its inherently transdisciplinary nature, the CPHHD program provides a unique environment in which to perform multilevel health disparities research. During the course of the program, the CPHHD centers have experienced challenges specific to this type of research. The challenges were categorized along three axes: sources of subjects and data, data characteristics, and multilevel analysis and interpretation. The CPHHDs collectively offer a unique example of how these challenges are met; just as importantly, they reveal a broad range of issues that health disparities researchers should consider as they pursue transdisciplinary investigations in this domain, particularly in the context of a large team science initiative.
Introduction and Rationale
It has been well-established that racial and ethnic minorities and individuals with fewer economic resources suffer a disproportionate burden of illness and death in the U.S. Such health disparities have been documented in many diseases and conditions, including cardiovascular disease,1,2 cancer,3 HIV/AIDS,4 and infant mortality.5 Additionally, racial and socioeconomic disparities have been observed for health behaviors, such as cancer screening6,7 and smoking.8–10
Although gaps have narrowed over time for some health behaviors, many have not. Moreover, health services research indicates that even where disparities in processes of care (e.g., screening) have been addressed, disparities in general, as well as gaps in intermediate outcomes (e.g., achieving control of blood sugar,11 blood pressure,12 and cholesterol13), persist. However, a recent survey of Medicare recipients found that self-reports failed to identify racial/ethnic disparities in mammography screening that were apparent from claims data.14 This, in combination with a recent meta-analysis of the inaccuracy of cancer screening self-reports,15 suggests that significant disparities in cancer-screening prevalence in the U.S. are being masked by differential over-reporting. Despite these biases, the problem of health disparities is so great that the USDHHS has made the elimination of disparities in health and health care one of the two major objectives of Healthy People 2010.16
Trends in Health Disparities
In some instances, disparities in health by race/ethnicity and SES have been increasing over the past decade.17 Silva et al.18 reported findings on changes in both black–white and low–high income disparities over time for 22 select causes of death, communicable diseases, and birth outcomes in Chicago between 1979–1981 and 1996–1998. The authors reported that for 19 of the 22 causes, the black–white rate ratio significantly increased over time, suggesting that racial disparities have increased over the 18-year period. Similarly, for 14 of the 16 measures included in the low–high income disparities analysis, the rate ratio increased between 1979–1981 and 1996–1998.
Starting around 1980, different trends in coronary heart disease (CHD) mortality have been observed for black and white men and women.19–21 Since 1980, the rate of CHD mortality has declined more rapidly among white men compared to black men in the U.S. While a similar pattern has emerged among women, more striking is the observation that the trend lines crossed in the mid-1980s, and now black women have higher death rates than white women. These and other studies of health disparity make it clear that progress toward reducing health disparities in the U.S. is, at best, much slower than hoped, and in many cases disparities have increased rather than decreased.
Traditional etiologic approaches to studying disparities have often been limited in scope with respect to data-collection and analysis strategies, leaving researchers to draw conclusions that are consistent with their data but sometimes require large inferential leaps. For example, many studies have found that census-tract SES explains much of the black–white disparity in breast cancer stage at diagnosis.22 While these studies suggest that disparities are largely driven by social factors, they say little about the exact proximal or distal causes of the disparity. Conclusions about the causes of disparity that are drawn from such studies are potentially and justifiably open to criticism.23 For example, individual-level health behaviors may or may not be influenced by environmental factors that may be bundled with SES; in a real sense, SES proxies these other factors without providing any real information about them. In their work on transdisciplinary approaches to the etiology of cancer, Hiatt and Breen24 note the importance of environmental and socioeconomic factors as part of the web of causation, specifically at the level of social determinants; these factors include characteristics of the built environment. Whereas their model was developed from a focus on cancer, it is applicable to many other health outcomes such as heart disease, hypertension, and diabetes, all of which may be mediated by broadly defined social determinants. Focusing on such characteristics as census tract-specific SES as a sole predictor of such outcomes ignores the influence of more specific and potentially more informative variables such as the neighborhood availability of sidewalks, grocery stores, and recreational facilities.
A Multilevel Approach to Studying Health Disparities
A growing body of research demonstrates that health disparities constitute a highly complex problem domain that both exists and operates on many different levels.25–32 In other words, many disparities that affect an individual’s opportunity to pursue a healthy life occur above and beyond individual-level characteristics, resources, and behaviors. One example is residential environment: An individual living in a high-risk or resource-poor environment may acquire over time a biological disadvantage relative to someone with similar personal characteristics living in a more salutary environment.33 This example suggests only one of many ways in which health disparities may be attributable to a wide range of contextual factors operating beyond the individual level.
Advantages of Multilevel Research in Studying Health Disparities
There are several reasons for applying the concepts and tools of multilevel research to health disparities. First, only multilevel research can examine the effects of one factor at one level (e.g., personal behaviors) while controlling for potential confounding at another level (e.g., neighborhood differences), or examine the interactions among factors situated at different levels. An example of such an interaction is seen in the effect of social isolation on the expression of genes in breast cancer.34 This potentially complex interaction had previously been identified as a limitation of disparities research, requiring that the researcher assume that an effect is not confounded by a factor at another level of analysis. Only multilevel research can examine how individual behaviors that influence risk for disease are themselves influenced by larger societal factors such as access to quality health care, social networks, and neighborhood resources. Larger societal factors, such as poverty, can also influence the risk of disease through mechanisms other than health behaviors. Social isolation is higher in neighborhoods with outdated infrastructure, characterized by such features as poorly maintained and inadequate utility systems, the lack of availability of services and commerce, and the inadequate ability of public safety agencies to respond to emergencies.35 Understanding the interplay among etiologic factors situated at different levels of analysis will enable interventions to be targeted with greater precision, thus better ensuring their success.
Multilevel studies are not easy to undertake; they require a comprehensive conceptual model of etiologic factors that are distributed across multiple levels, data collection from multiple sources, and appropriate statistical models to account for the relationships among various levels of analysis. With this in mind, NIH recently funded eight Centers for Population Health and Health Disparities (CPHHDs) whose mission is to foster and conduct transdisciplinary health disparities research across multiple levels, pathways, or contexts. This paper highlights some of the key lessons learned through the authors’ transdisciplinary collaborations within and among centers. First described is the conceptual model that forms the basis for the CPHHD initiative; then specific examples from the various CPHHD centers are provided to highlight the special issues and challenges encountered in multilevel statistical analyses. Finally, the authors’ experience in the CPHHD is summarized, and suggestions for future directions in evaluating transdisciplinary research are presented.
The Centers for Population Health and Health Disparities
In September 2003, the NIH established the eight CPHHDs to conduct cutting-edge research to understand and reduce differences in health outcomes, access, and care: the ways the social and physical environment, behavioral factors, and biologic pathways interact to determine health and disease in populations. The centers include the University of Illinois at Chicago, the University of Chicago, Tufts and Northeastern universities, the RAND Corporation, the University of Texas Medical Branch, The Ohio State University, Wayne State University, and the University of Pennsylvania. Projects at the centers focus variously on obesity, cardiovascular disease, breast cancer, prostate cancer, cervical cancer, mental health, gene–environment interactions, psychosocial stress, and other factors affecting low-income whites, African Americans, Hispanics, and the elderly.
The CPHHDs as a Laboratory for Transdisciplinary Research
Before examining the transdisciplinarity of the CPHHDs, it is important to consider the distinctions among multidisciplinary, interdisciplinary, and transdisciplinary research. In multidisciplinary research, scientists from different fields work independently but bring their expertise to solve a problem that is addressed through a mosaic of activity; each scientist represents and acts only within his or her own domain. Interdisciplinary research requires more integration of multiple scientific perspectives, but researchers retain their discipline-specific grounding. Transdisciplinary research differs from these in that scientists not only collaborate and integrate their respective discipline-specific expertise, but do so within the context of a new, common conceptual framework that transcends the frameworks used within their respective disciplines.36,37
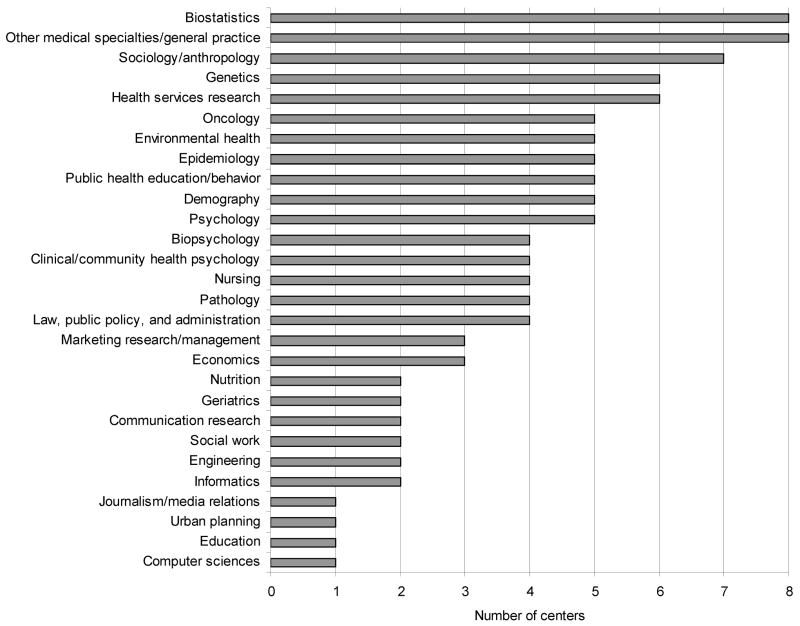
The CPHHDs are intrinsically multidisciplinary in that many disciplines are represented within and across them, as illustrated in Figure 1. Specifically, the eight CPHHDs together represent 42 disciplines, which can be grouped into biological and clinical sciences; media and communications; public health, policy, and planning; social and behavioral sciences; and biomechanics/statistics.38
Figure 1.
Disciplines represented across the CPPHDs, ranked by prevalence
While Figure 1 reveals that many different disciplines are represented in the CPHHD program, it does not show how these disciplines are spread across the centers, nor does it suggest the interdisciplinary nature of the CPHHD. In fact, the individual centers and the CPHHD initiative as a whole are highly interdisciplinary, in that many different disciplines are represented on each component project at each center. Furthermore, these projects typically require considerable collaboration and a degree of integration. Table 1 shows the various disciplines involved in the CPHHD initiative grouped by center, and represents the opportunities for horizontal and vertical integration that are critical to ransdisciplinary research.39,40
Table 1.
The disciplines of the CPHHDs
| UIC | Chicago | OSU | Penn | UTMB | WSU | Tufts | RAND | |
|---|---|---|---|---|---|---|---|---|
| Biological sciences | ||||||||
| Biopsychology | X | X | X | X | ||||
| Genetics | X | X | X | X | X | X | ||
| Nutrition | X | X | ||||||
| Oncology | X | X | X | X | X | |||
| Clinical sciences | ||||||||
| Clinical/community/health psychology | X | X | X | X | ||||
| Geriatrics | X | X | ||||||
| Nursing | X | X | X | X | ||||
| Pathology | X | X | X | X | ||||
| Other medical specialties, general practice | X | X | X | X | X | X | X | X |
| Media and communications | ||||||||
| Communication research | X | X | ||||||
| Journalism/media relations | X | |||||||
| Marketing research/management | X | X | X | |||||
| Public health, policy, and planning | ||||||||
| Environmental health | X | X | X | X | X | |||
| Epidemiology | X | X | X | X | X | X | ||
| Health services research | X | X | X | X | X | X | ||
| Law, public policy, and administration | X | X | X | X | ||||
| Public health education/behavior | X | X | X | X | X | |||
| Urban planning | X | |||||||
| Social and behavioral sciences | ||||||||
| Demography | X | X | X | X | X | |||
| Economics | X | X | X | |||||
| Education | X | |||||||
| Psychologya | X | X | X | X | X | |||
| Sociology/anthropology | X | X | X | X | X | X | ||
| Social work | X | X | ||||||
| Biomechanics/statistics | ||||||||
| Biostatistics | X | X | X | X | X | X | X | X |
| Computer sciences | X | |||||||
| Engineering | X | X | ||||||
| Informatics | X | X | ||||||
Includes cognitive, developmental, educational, and social psychology.
Chicago, University of Chicago; OSU, The Ohio State University; Penn, University of Pennsylvania; RAND, the RAND Corporation; Tufts, Tufts and Northeastern universities; UIC, University of Illinois at Chicago; UTMB, University of Texas Medical Branch; WSU, Wayne State University
The CPHHD initiative fosters both vertical-integration dimensions in supporting collaborative, integrative health disparities research at the centers as well as horizontal collaboration and integration across the centers. This suggests that the CPHHD initiative is not only interdisciplinary but transdisciplinary as well, but transdisciplinarity can be an elusive characteristic to measure.37,39
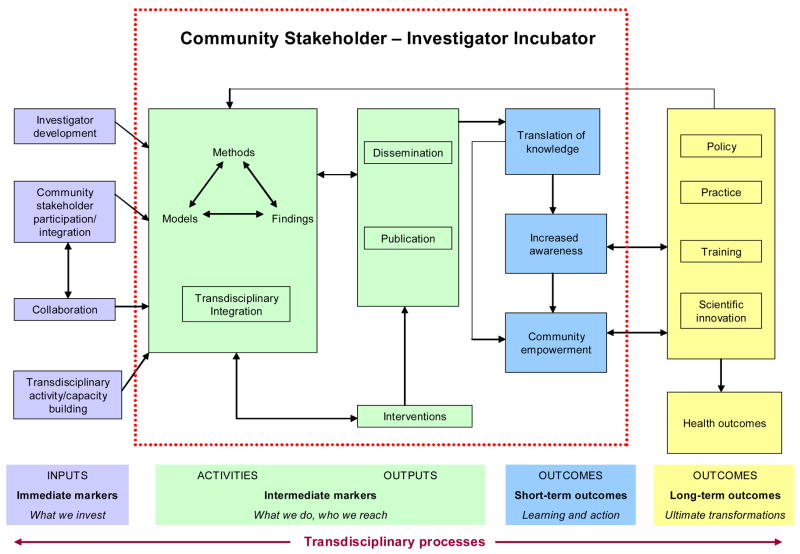
To capture evidence of collaboration and the emergence of transdisciplinary research, the CPHHD evaluation working group conducts an annual survey of the investigators at each center. The conceptual model shown in Figure 2 was used both to develop the survey instrument and as a guide for evaluating the CPHHD program as a whole. In this model, a temporal series of transdisciplinary processes are grouped as immediate markers, intermediate markers, short-term outcomes, and long-term outcomes. (The CPHHD model is similar to the antecedent–process–outcome model proposed by Stokols et al.37) The responses to the survey were coded, using the specific markers and outcomes represented in the boxes. For example, transdisciplinary integration would be evidenced by the integration of methods, models, and findings from at least two disciplines. To this end, the surveys focused on five domains of transdiciplinary science. Evidence of (1) collaboration was seen in the participation of schools, healthcare institutions, and community organizations; of (2) capacity building in new seminars and conference series, and increased institutional commitment to infrastructure and other support; of (3) integration in the development of new, multipurpose databases; common conceptual language pertaining to health disparities; and new analytic methods; of (4) knowledge in the emergence of new lines of inquiry; multicenter and transdisciplinary manuscripts (such as this one); and new grant applications; and of (5) innovation in the development of new instruments and analytic methods. In addition to the annual survey, progress toward transdisciplinarity was assessed using social-network analysis.41 Investigators and researchers at each center participated in a self-administered survey aimed at identifying collaborators and their disciplines. The social-network data are currently being analyzed.
Figure 2.
The logic model for the CPPHDs
There is substantial evidence of the emergence of a new, transdisciplinary science of health disparities research across the CPHHD program. The CPHHDs face a number of challenges to achieving transdisciplinary functioning, such as developing a shared lexicon, pooling the best of disciplinary theories, deciding upon a shared research design or designs, and determining the best methods for analyzing data. Nevertheless, multilevel analysis distinguishes itself among these significant challenges, and in a mid-course survey conducted in 2006, CPHHD investigators listed multilevel analysis as the single greatest challenge facing their centers. One reason for this is that multilevel research demands a level of interaction that is much greater than is characteristic of monodisciplinary or traditional multidisciplinary collaboration. In the multilevel research discussed in this paper, clinicians, social scientists, informaticians, statisticians, and health communication experts have worked together in highly evolved teams that address facets of health disparities issues that are out of their normal disciplinary sphere. Accordingly, the authors found that multilevel research provides an extraordinary domain for transdisciplinary research, in that investigators form and participate in highly collaborative, integrative relationships that transcend their own disciplines. In addition, through its focus on linking science, training, and application to public health practice and policy, the CPHHD initiative provides a unique environment for multilevel health disparities research—one that connects the scientific discovery and training phases of team science with the translational, health-improvement goals of transdisciplinary action research.40
Challenges and Solutions of Multilevel Analysis and the CPHHDs
The following section outlines shared challenges to performing multilevel analyses across the CPHHD program and the solutions that have been developed to address them. Most of these challenges parallel the issues raised in the introduction to this supplement, including the need for conceptual frameworks, methodologic and analytic issues, and translational initiatives. The focus here is on the first two sets of issues, grouping specific challenges along three conceptual axes: sources of subjects and data, data characteristics, and multilevel analysis and interpretation.
Sources of Subjects and Data
Challenge: the number of sites (clusters) for study
An unusually large or small number of sites (clusters) from which participants are recruited may affect a statistical analysis. For example, the original Ohio State University CPHHD analysis plan was to use a survey approach to account for interclass correlation among subjects at the same clinic. However, computational issues resulting from the small number of clinics (N=14) prevented investigators from developing models with adequate numbers of covariates. The current analysis strategy is to fit mixed models (i.e., hierarchical linear models) that incorporate the site as a random effect rather than survey-based models.
Challenge: a limited number of observations per cluster
The University of Illinois at Chicago is examining the hypothesis that the racial and ethnic disparities in stage at diagnosis and treatment for breast cancer can be explained in part by differences in healthcare facilities. Random-intercept models will be used to account for the clustering of patients within facilities. The roughly 900 patients in the study are distributed across more than 60 facilities in Chicago that detect, diagnose, and treat breast cancer, and many facilities have only one patient associated with them. For example, there are more than 40 breast-surgery facilities with only one affiliated patient in the study. Because clusters with a single observation contribute only to the estimation of between-level parameters and not to within-level parameters, the variation associated with smaller facilities (i.e., cluster size=1) would be missed. One solution to this problem would be to group facilities when cluster size=1 into a smaller number of clusters with common attributes (e.g., facility type, location) so that most or all clusters would have a sample size >1.
Challenge: incorporating census information
Analyses across CPHHDs will almost certainly incorporate census information at some point. Decisions, therefore, must be made about how to define variables appropriately, to deal effectively with sparse populations in census regions, and to geocode participants’ addresses. The Ohio State University CPHHD recruits patients from clinics in 14 counties in Appalachian Ohio. In order to geocode the location of each participant, interviewers were given a hand-held device which measured the latitude and longitude at the site of the interview. The data were then used to determine the census tract for each participant.
Because of the rural locations as well as issues with the devices, it has been difficult to assign the proper census tract for some of the observations based on the device data. The investigators have been able to determine the census tracts for some of the participants by entering the street address in the Census Bureau’s website. They are currently working to resolve the few cases where the calculated tract and the tract from the Census Bureau’s website do not agree.
A challenge faced by the University of Illinois at Chicago CPHHD is how to obtain the best imputation of patient SES using census data derived at the level of the census tract. Census-data associations with disease represent a mixture of area-level and individual-level effects. In order to impute patient-level SES as accurately as possible, this CPHHD stratified census-tract information into nine separate cross-classifications of age and race. They then assigned census tract–, age-, and race-specific estimates for the percentage below the federal poverty level to each individual accordingly, and used these estimates as imputations of individual-level poverty status. An alternative and more traditional approach is to assign the mean poverty level in a census tract to all patients residing in that tract without regard to other patient attributes. The investigators here found that the former approach resulted in more parsimonious models than the latter. When poverty status was assigned solely based on patient census tract, models of poverty and race in predicting stage at breast-cancer diagnosis contained nonlinear effects, and race and poverty interacted. On the other hand, when poverty status was assigned based on patient census tract, age, and race, all effects were linear, and the final model did not contain any interactions among age, race, and census tract. Because of the availability of common demographic variables such as age and race, this approach could be generalized to other settings where researchers need to develop a poverty-status indicator.
Another problem was encountered when imputing poverty status from census data. Estimates of poverty within census age–race groups are often based on sparse data, and therefore are less precise and more likely to be biased. One possible solution to this problem is to use empirical Bayes approach-to-model estimates in a manner that would shrink unstable estimates toward the overall census tract mean, with the extent of shrinkage depending on how sparse the stratum-specific data are relative to the data for that census tract. University of Illinois at Chicago investigators found that using empirical Bayes to estimate poverty within census age–race groups provided no advantage over using more traditional (and simpler) estimation methods, and the results were similar in both cases. This finding made sense, given that sparsely populated census age–race strata would tend to contribute little to the overall association between poverty and stage at diagnosis.
The RAND project examining data from the third national health and nutrition examination survey (NHANES III) focuses on the socioeconomic environment, the socio-structural environment, and the quality of neighborhoods. Many contextual variables were derived from the U.S. Census 1990 and 2000 data (interpolating for intercensal years and extrapolating from 2000 forward); neighborhood characteristics were measured at the census-tract level. To link the geographic- and individual-level data, study participants’ residential addresses required geocoding, which in turn necessitated a decision about the level of geocoding to be performed (e.g., ZIP code, census tract, or block group). Other considerations included determining which geocoded measures of physical and social characteristics of neighborhoods were most relevant to individual health, and whether the potential effects of continuously measured neighborhood characteristics were likely to manifest themselves across a continuum or emerge at some threshold level. The RAND project focused on the effects of environments at the most immediate level of living—the neighborhood. Environment at the census tract was first considered, to ensure homogenous populations and smaller spatial areas. However, the characteristics of larger administrative units (e.g., county or metropolitan statistical area) were also considered, to investigate whether larger economic considerations (e.g., job availability, unemployment, levels of inequality within regions) may play a role in outcomes.
Challenge: using existing data from other research studies
Health disparities research often incorporates existing data from studies that were not designed to collect multilevel data. These data present special challenges for researchers wishing to use multilevel analysis. In particular, CPHHD researchers have encountered challenges using existing-survey data as well as clinical-trials data.
Working with existing survey data typically does not allow researchers to consider examining self-defined neighborhood levels. This limitation is both advantageous and disadvantageous; for example, individuals may infrequent contact with areas of their census tract that drive many of the average characteristics of the entire census tract. However, the existence of objective data avoids the problems of reverse causality whereby individuals with poorer health may report more negatively on their residential environment, either because of differences in their perceptions of the environment (e.g., reporting more or less disorder or disadvantage) or because of their experience of the environment (e.g., greater difficulty with poor air quality).
As with many large sample surveys, NHANES III data are not limited to questionnaire items, but include physical exam and biomarker information as well. With the addition of census data, multilevel models could explore potential interactions that may arise from social-determinants-of-health outcome etiology; among others, these include whether the impact of neighborhood SES and built-environment characteristics varies with individual SES, how it varies, and whether such interactions help to explain health disparities.24 For example, do the effects of neighborhood SES on specific health behaviors vary by gender or race/ethnicity?
Other types of studies offer the potential for multilevel research, but pose challenges as well. For example, the RAND CPHHD is developing multilevel models using observational and clinical-trial data from the women’s health initiative. These data pose a particular challenge in that there is clustering at the level of “medical center.” In addition, some metropolitan statistical areas may have several medical centers, while participants may be enrolled in a center that serves several metropolitan statistical areas. Investigators at the University of Pennsylvania are using data from an existing case–control study to investigate the possible interactions of neighborhood characteristics with genes and screening behaviors in explaining racial differences in prostate cancer outcomes.
Challenge: accessing detailed neighborhood-characteristics data
Census data do not provide researchers with detailed neighborhood characteristics that could be useful in multilevel health disparities analysis. For example, property-specific or parcel-specific data are not available through the census. Researchers seeking to use property size, value, or length of ownership as possible covariates or predictors in multilevel models need to identify other sources of these characteristics. Two CPHHDs have identified local neighborhood characteristics data, but these sources are not without their challenges. The University of Pennsylvania CPHHD has a resource on campus, the cartographic modeling laboratory, that provides access to detailed neighborhood data. However, the data are restricted to Philadelphia, and the use of some data requires special approval from city agencies. Similarly, the University of Chicago CPHHD has access to data from the Chicago Area Study,42 but it is unique to the city of Chicago, was collected more than a decade ago, and may not represent the current characteristics of neighborhoods that have undergone gentrification or other demographic changes since then.
The Ohio State University CPHHD had a slightly different experience with this challenge. Early in the planning stages of the projects, researchers needed a list of all providers (in clinics, health departments, and other healthcare facilities) that performed Pap screening in their 14 Appalachian counties. Because there was no resource that could easily provide this inventory, the investigators had to work with local agencies, key informants, and local field staff to develop a list of providers, using a snowball-sampling approach.
Challenge: issues in recruiting from special populations that affect multilevel analysis
The Ohio State University CPHHD recruits patients from clinics in 14 counties in Appalachian Ohio. Researchers there have experienced challenges in patient sampling (e.g., it is inconsistent across clinics; patient lists are difficult and time-consuming to obtain); in rates of response among these populations (e.g., how to extrapolate to all of Appalachian Ohio); and in interview and follow-up burden due to travel difficulties, contact challenges, and lack of incentives. The potential effects of these issues on outcomes will be explored during the analysis phase, and their impact on the interpretation of results will be carefully considered.
The CPHHD at Tufts/Northeastern universities recruits Puerto Rican adults from the Boston area. Although a growing population, they constitute less than 10% of households in the city. Further, the presence of Puerto Ricans is identified by the census only at the tract level. At the block level, there may be many Hispanic individuals, but none who are Puerto Rican. Sampling proceeded by identifying tracts that contain at least ten Puerto Ricans, and then moving to the block level, with door-to door enumeration of blocks that, according to the census, contain at least four Hispanics. To use lower cutoff points would be prohibitive in cost, but as the study is designed, many blocks are enumerated with no Puerto Ricans identified.
This has several consequences, because Puerto Ricans at lower SES levels are most likely to live in more-concentrated communities. First, the sample will not include Puerto Ricans with higher-level SES who live in more-integrated environments; second, SES distribution is therefore truncated, resulting in lower variability across sampled neighborhoods. This results in limitations in generalizability to those Puerto Ricans living in neighborhoods with other Hispanics, and limits power for multilevel analyses.
To improve this, these researchers have included participants who are recruited from community gatherings, such as Puerto Rican festivals. This method does identify individuals who live in less Hispanic-dense neighborhoods (although they remain underrepresented), but it may complicate analyses. One such complication is the lack of homogeneity within the study sample.
Community gatherings may draw people from outside the neighborhood under study. In addition, the people who attend such gatherings may be nonrepresentative of the neighborhood as a whole, even if they live in that neighborhood.
Characteristics of Data for Multilevel Research
Challenge: dealing with significantly inter-correlated variables
Every CPHHD considers both SES and race/ethnicity, which are highly correlated, in analyses. A number of solutions have been devised to address this conundrum. Researchers at the University of Illinois at Chicago CPHHD undertook a secondary data analysis, linking data on breast cancer stage at diagnosis from the Illinois State Cancer Registry for the years 1994–2000 with census data for Chicago. Their initial plan was to limit the geographic region to Chicago. They initially encountered a high correlation between census-tract SES and census-tract composition by race/ethnicity within the city limits. This made it virtually impossible to tease apart the separate effects of SES and race/ethnicity on stage at diagnosis. As a solution to the problem, the group expanded the geographic region of interest to include all of Cook County, in which there are suburbs with substantial numbers of relatively affluent minority populations.
The RAND CPHHD addressed the issue by examining the distribution of each race/ethnicity on its measure of neighborhood SES to determine the degree of overlap. They determined that there was insufficient overlap to ensure that neighborhood SES effects occur for all groups by race/ethnicity, and they are conducting stratified analyses by race/ethnicity in order to test for effects based on the actual range of the data within each subgroup. Similarly, RAND CPHHD investigators have found that, although men and women are not differentially distributed across census tracts (because neighborhoods are not gender-segregated), there are myriad gender differences in contextual effects that necessitate the use of either multiple interaction terms or, in some cases, gender-stratified models in order to capture the differential effects of specific aspects of neighborhood contexts on men compared to women.
Challenge: justifying community- and neighborhood-level data from two sites that were conceptualized and gathered in different ways
The University of Chicago CPHHD originally planned to work only on the South Side of Chicago. Thus, all neighborhood and community data were from the same sources (e.g., the city of Chicago). Then the group began to work in Gary, Indiana, in order to increase sample size. That posed a problem, because the data had been gathered by another source and were not completely comparable to the Chicago data. The approach to this challenge was to explore how each respective source defined each variable that was measured (e.g., violent crime or safety of housing) and to find the lowest common denominator among measures across sources.
Challenge: making the most of administrative data to examine contextual effects
In some cases, tract-level data fail to capture important aspects of residential exposure—for example, because otherwise-similar tracts are surrounded by differing concentrations of poverty or by built environments of varying quality. A solution developed by RAND and University of Chicago investigators was to examine a combination of census-tract characteristics and the characteristics of a buffer area around each tract. In additional work, the RAND CPHHD has begun to use GIS-based measures to capture distance and exposure—for example, to alcohol outlets.43 Because businesses are often in separate areas that are not zoned for housing and thus are not classified as census tracts, measuring exposure to alcohol outlets only in tracts (or in grocery stores or fast-food outlets) results in a systematic undercount of residents’ exposure to these businesses. In other projects, RAND investigators have employed similar models to capture distance from parks and other green space.44
Analyzing Multilevel Data and Interpreting the Results
Transdisciplinary research requires collaborative and integrative thinking. Multilevel analysis provides a natural environment for this in that it requires substantial input from experts in a variety of content and methodologic domains. Effective collaboration in multilevel research is facilitated to the extent that team members share an interdisciplinary or transdisciplinary research orientation from the outset of the project. Yet the progression from multidisciplinary to transdisciplinary collaboration in the context of multilevel, multisite team initiatives is a gradual process that poses various conceptual and methodologic challenges along the way. It is clear, for example, that engaging in multilevel analysis has challenged CPHHD investigators, especially in their efforts to apply theoretical concepts to practical settings.
Challenge: providing proper explanatory schemes for observed multilevel effects
Many researchers agree that the most important challenge for multilevel analysis is not merely to apply advanced statistical models but also to provide proper theoretical frameworks for framing studies. This is especially challenging because it is very easy to draw conclusions based on an ecologic fallacy when trying to explain neighborhood effects at a high level when the actual effect-modifiers are low-level factors associated with “neighborhood.” Ecologic fallacy arises when inferences about low-level factors, such as SES, are made from high-level factors, such as ZIP code or census tract. Sound theoretical frameworks can provide the scaffolding that guides the development of research questions, collection of data, and the analytic process. One approach is taken by researchers at the University of Pennsylvania, who have used the systems model of clinical preventive care45 to frame a study on determinants and interventions to improve discussions about prostate screening. This study is one example of a translational initiative that seeks to implement a novel computer-assisted, patient-oriented behavioral intervention that is informed by a highly transdisciplinary research enterprise. The systems model is an excellent choice for the project, given that it considers individual-, environmental-, and system-level factors that influence behaviors by patients and practitioners that affect health outcomes. lthough not specifically used by the CPHHD, the model developed by Hiatt and Breen24 shares the translational nature of the systems model by considering the continuum of the disease process, from pre-disease to death, and suggests families of interventions that address this continuum.
Challenge: low statistical power for testing neighborhood effects
In some centers, participants are drawn from a relatively small number of relatively homogeneous census tracts. At Wayne State University, all of the studies are intervention studies, and the studies are powered to detect differences among interventions, not the effects of neighborhoods. There are small differences between the census tracts from which the participants were drawn, and in each study there may be too few tracts to detect neighborhood effects. This challenge is presented here as a cautionary tale: Health disparities researchers need to be aware of the effects of neighborhood characteristics on statistical power, and these characteristics need to be considered in calculating sample size.
Challenge: heterogeneous variable representation
Whenever possible, the CPHHDs would like to avoid excluding variables simply because they were measured or collected at different levels or used different coding schemes. How variables are defined at one level (e.g., the neighborhood level) so that they may be used in analyses with variables at other levels (e.g., the individual level) poses a challenge to those engaged in multilevel analyses. The University of Chicago CPHHD is faced with determining which features of the neighborhood built-environment (i.e., neighborhood level) are most salient to women’s individual levels of felt loneliness, depression, and perceived stress. More specifically, they would like to understand the relationships between the neighborhood social environment—measured both at the individual level (with measures of women’s perceived neighborhood safety, social cohesion, collective efficacy) and at the neighborhood level (with area major-crime rates related to violence such as homicide and sexual assault)—and psychosocial-stress response, measured at the individual level (determined both subjectively and objectively). The University of Chicago CPHHD’s solution to the challenge is to gather data in a number of ways to provide as much flexibility as possible in selecting and constructing variables for analysis.
Challenge: the need for new multilevel-analysis methods
The increasing interest in translational research, which encompasses the continuum of bench to bedside to populations, highlights the importance of extending current multilevel research methods in new directions. The University of Chicago CPHHD, for example, is developing new methods to correlate patterns and features of dynamic cortisol metabolism with cumulative genetic-expression alterations in breast cancer tissue pathology (e.g., intranuclear glucocorticoid receptor activation immunohistology). Those researchers are working with faculty associates on the University of Chicago campus to expand the methods of hierarchical linear models to allow for the inclusion of variables from molecular to community levels on each research subject. This endeavor brings together pathologists, geneticists, social and behavioral scientists, statisticians, and immunologists to develop a new multilevel analytic approach.
Summary
This paper has described several challenges faced by researchers at the CPHHDs as they pursue rigorous programs of health disparities research in a variety of domains. Each of these challenges represents an opportunity for transdisciplinary science to evolve. For example, the substantive data issues that pervade multilevel disparities research could not be addressed without the collaboration of social scientists, data-systems experts, clinicians, and others. But this collaboration is not a simple multidisciplinary one in which each specialist practices his or her craft. Rather, these collaborations require the transcendence of each researcher’s domain. Thus, while the challenges presented here may not be unique to multilevel health disparities research, the environment within which they emerged, and in many cases met, is unique. Defining and working through these challenges suggests three strengths of this work and this paper.
First, the CPHHDs collectively offer examples of how these challenges are met within the initiative, but, just as importantly, they offer an extensive compendium of issues that other health disparities researchers should consider, particularly in transdisciplinary environments such as the CPHHD initiative. The work put into rigorous multilevel approaches to health disparities research, exemplified by the efforts reported here, is contributing to a better understanding of health disparities: where they come from, whom they affect and why, and how they might be reduced. Even so, the diversity of the challenges and solutions described here suggests a degree of uniqueness that depends heavily on the research domain under investigation. While the story of multilevel analysis in health disparities research, told through the experience of the CPHHD centers, is compelling, it is not the last chapter. Investigators are urged to be watchful for challenges unique to their research and to consider other solutions that are not described here. It is hoped that this paper stimulates the recognition that such vigilance is a necessary component of health disparities research and of multilevel research approaches in general.
Second, the CPHHDs now have extensive, hands-on experience with multilevel research. There are numerous reports on multilevel research theory and analytic methods, but relatively few that provide insight into the practical, day-to-day problems of conducting this kind of work. This paper provides such a report that, again, is intended to be of value to the broader research community, not just to those currently working in health disparities.
Finally, the CPHHD program facilitates cross-center collaboration in health disparities research, and the centers have in turn taken up the mantle of collaboration. Researchers at the CPHHDs have worked on finding and sharing solutions to the practical and theoretical challenges in multilevel research, not only as it applies to health disparities, but to other research domains as well.
The CPHHD experience suggests the need for new directions in evaluating transdisciplinary science. At the least, a transdisciplinary research evaluation “toolkit” initiated through this endeavor would provide a useful and constructive model for investigators and funding agencies. When fully developed, such a toolkit would contain quantitative tools, such as validated scales that could be used in creating evaluation instruments, as well as qualitative tools, such as semi-structured questionnaires that could be used to elicit attitudes and opinions. The toolkit could be framed within a methodology for evaluating transdisciplinary science so that any evaluations would be as accurate and robust as possible. This methodology would borrow from the best traditions of research evaluation, but would need to extend the boundaries to include new methods and to apply existing methods in new ways.
Transdisciplinarity does not exist automatically, nor all at once; rather, it emerges over time, within and among individuals, groups of individuals, departments, schools, institutions, and organizations. Ultimately, there is a need to foster team science so that transdisciplinarity is given a chance to emerge. The authors’ experience with conducting multilevel research in health disparities underscores this need. As an example, their survey-based evaluation efforts have provided insight into the number and types of collaborations across the CPHHD program, but were unable to capture the evolution of team science, even with annual evaluations, which had focused on such characteristics as publication counts and self-reported data on collaboration. This experience suggests that instruments requiring self-report may not be the optimal way to capture team science-related evaluation data, and the authors are hopeful that the social-network analyses will provide more substantive information, particularly with regard to the scientific collaboration and integration that are central to transdisciplinary research.
However, two potentially more-powerful approaches would be the use of temporal social-network analysis and a formal bibliometric analysis of not only published but cited publications as ways to investigate the emergence of “new science.” These approaches would be particularly valuable, given that increasing numbers of CPHHD investigators identified multilevel research as a major challenge. A final lesson learned from the authors’ experience is that multilevel research should be considered in a transdisciplinary context. Multilevel research has often been conducted without consideration of this context, perhaps to its detriment.46 The CPHHD initiative (and others like it) offers the opportunity for conducting multilevel research in a variety of application domains, within a new, rigorous, and inherently transdisciplinary environment.
Acknowledgments
No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the U. S Circulation. 2005;111(10):1233–41. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 2.Sharma S, Malarcher AM, Giles WH, Myers G. Racial, ethnic and socioeconomic disparities in the clustering of cardiovascular disease risk factors. Ethn Dis. 2004;14(1):43–8. [PubMed] [Google Scholar]
- 3.Bradley CJ, Given CW, Roberts C. Race, socioeconomic status, and breast cancer treatment and survival. J Natl Cancer Inst. 2002;94(7):490–6. doi: 10.1093/jnci/94.7.490. [DOI] [PubMed] [Google Scholar]
- 4.CDC. Racial/ethnic disparities in diagnoses of HIV/AIDS—33 States, 2001–2004. MMWR Morb Mortal Wkly Rep. 2006;55(5):121–5. [PubMed] [Google Scholar]
- 5.CDC. Racial/ethnic disparities in infant mortality—U.S. 1995–2002. MMWR Morb Mortal Wkly Rep. 2005;54(22):553–6. [PubMed] [Google Scholar]
- 6.Ananthakrishnan AN, Schellhase KG, Sparapani RA, Laud PW, Neuner JM. Disparities in colon cancer screening in the Medicare population. Arch Intern Med. 2007;167(3):258–64. doi: 10.1001/archinte.167.3.258. [DOI] [PubMed] [Google Scholar]
- 7.Sassi F, Luft HS, Guadagnoli E. Reducing racial/ethnic disparities in female breast cancer: screening rates and stage at diagnosis. Am J Public Health. 2006;96(12):2165–72. doi: 10.2105/AJPH.2005.071761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernandez E, Schiaffino A, Borrell C, et al. Social class, education, and smoking cessation: long-term follow-up of patients treated at a smoking cessation unit. Nicotine Tob Res. 2006;8(1):29–36. doi: 10.1080/14622200500264432. [DOI] [PubMed] [Google Scholar]
- 9.Honjo K, Tsutsumi A, Kawachi I, Kawakami N. What accounts for the relationship between social class and smoking cessation? Results of a path analysis. Soc Sci Med. 2006;62(2):317–28. doi: 10.1016/j.socscimed.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 10.Kesteloot H. Social class, all-cause, cardiovascular and cancer mortality: the importance of cigarette smoking. Acta Cardiol. 2003;58(4):285–7. doi: 10.2143/AC.58.4.2005284. [DOI] [PubMed] [Google Scholar]
- 11.Heisler M, Faul JD, Hayward RA, Langa KM, Blaum C, Weir D. Mechanisms for racial and ethnic disparities in glycemic control in middle-aged and older Americans in the health and retirement study. Arch Intern Med. 2007;167(17):1853–60. doi: 10.1001/archinte.167.17.1853. [DOI] [PubMed] [Google Scholar]
- 12.Giles T, Aranda JM, Jr, Suh DC, et al. Ethnic/racial variations in blood pressure awareness, treatment, and control. J Clin Hypertens. 2007;9(5):345–54. doi: 10.1111/j.1524-6175.2007.06432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stuart-Shor EM, Nannini A, Ostrem M, Russell GE, Mittleman MA. The prevalence of blood pressure and cholesterol monitoring in Boston among non-Hispanic blacks, Hispanics, and non-Hispanic whites. Ethn Dis. 2006;16(2):375–83. [PubMed] [Google Scholar]
- 14.Holt K, Franks P, Meldrum S, Fiscella K. Mammography self-report and mammography claims: racial, ethnic, and socioeconomic discrepancies among elderly women. Med Care. 2006;44(6):513–8. doi: 10.1097/01.mlr.0000215884.81143.da. [DOI] [PubMed] [Google Scholar]
- 15.Rauscher GH, Johnson TP, Cho YI, Walk JA. Accuracy of self-reported cancer screening histories: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2008;17(4):748–57. doi: 10.1158/1055-9965.EPI-07-2629. [DOI] [PubMed] [Google Scholar]
- 16.USDHHS. Healthy People 2010. www.healthypeople.gov/publications/
- 17.Keppel KG, Pearcy JN, Wagener DK. Statistical Note No. 23. Hyattsville MD: National Center for Health Statistics; 2002. Healthy People 2000: Trends in racial and ethnic-specific rates for the health status indicators: U.S., 1990–1998. [PubMed] [Google Scholar]
- 18.Silva A, Whitman S, Margellos H, Ansell D. Evaluating Chicago’s success in reaching the Healthy People 2000 goal of reducing health disparities. Public Health Rep. 2001;116(5):484–94. doi: 10.1016/S0033-3549(04)50076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnett E, Halverson J. Disparities in premature coronary heart disease mortality by region and urbanicity among black and white adults ages 35–64, 1985–1995. Public Health Rep. 2000;115(1):52–64. [PMC free article] [PubMed] [Google Scholar]
- 20.Cooper R, Cutler J, Svigne-Nickens P, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the U.S: findings of the National Conference on Cardiovascular Disease Prevention. Circulation. 2000;102(25):3137–47. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 21.Liao Y, Cooper RS. Continued adverse trends in coronary heart disease mortality among blacks, 1980–91. Public Health Rep. 1995;110(5):572–9. [PMC free article] [PubMed] [Google Scholar]
- 22.Newman LA, Mason J, Cote D, et al. African-American ethnicity, socioeconomic status, and breast cancer survival: a meta-analysis of 14 studies involving over 10,000 African-American and 40,000 white American patients with carcinoma of the breast. Cancer. 2002;94(11):2844–54. doi: 10.1002/cncr.10575. [DOI] [PubMed] [Google Scholar]
- 23.Bloche MG. Health care disparities—science, politics, and race. New Engl J Med. 2004;350(15):1568–70. doi: 10.1056/NEJMsb045005. [DOI] [PubMed] [Google Scholar]
- 24.Hiatt RA, Breen N. The social determinants of cancer: a challenge for transdisciplinary science. Am J Prev Med. 2008;35(2S):XXX–XXX. doi: 10.1016/j.amepre.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Subramanian SV, Chen JT, Rehkopf DH, Waterman PD, Krieger N. Racial disparities in context: a multilevel analysis of neighborhood variations in poverty and excess mortality among black populations in Massachusetts. Am J Public Health. 2005;95(2):260–5. doi: 10.2105/AJPH.2003.034132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fone DL, Lloyd K, Dunstan FD. Measuring the neighbourhood using UK benefits data: a multilevel analysis of mental health status. BMC Public Health. 2007;7(147):69. doi: 10.1186/1471-2458-7-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93(2):215–21. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson NB. Levels of analysis in health science a framework for integrating sociobehavioral and biomedical research. Ann N Y Acad Sci. 1998;840:563–76. doi: 10.1111/j.1749-6632.1998.tb09595.x. [DOI] [PubMed] [Google Scholar]
- 29.Poortinga W, Dunstan FD, Fone DL. Perceptions of the neighbourhood environment and self rated health: a multilevel analysis of the Caerphilly Health and Social Needs Study. BMC Public Health. 2007;7(147):285. doi: 10.1186/1471-2458-7-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fitzsimon N, Shiely F, Corradino D, Friel S, Kelleher CC. Predictors of self-reported poor mental health at area level in Ireland: a multilevel analysis of deprivation and social capital indicators. Ir Med J. 2007;100(8):49–52. [PubMed] [Google Scholar]
- 31.Blumenthal RN, Do DP, Finch B, Martinez A, Edlin BR, Kral AH. Community characteristics associated with HIV risk among injection drug users in the San Francisco Bay area: a multilevel analysis. J Urban Health. 2007;84(5):653–66. doi: 10.1007/s11524-007-9213-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, Huebner CE. Birth outcomes among urban African-American Women: a multilevel analysis of the role of racial residential segregation. Soc Sci Med. 2006;63(12):3030–45. doi: 10.1016/j.socscimed.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 33.Bird CE, Rieker PP. Gender and health: the effects of constrained choices and social policies. Cambridge: Cambridge University Press; 2008. [Google Scholar]
- 34.McClintock MK, Conzen SD, Gehlert S, Masi C, Olopade F. Mammary cancer and social interactions: identifying multiple environments that regulate gene expression throughout the life span. J Gerontol B Psychol Sci Soc Sci. 2005;60(1):32–41. doi: 10.1093/geronb/60.special_issue_1.32. [DOI] [PubMed] [Google Scholar]
- 35.Kleinenberg E. Heat wave: a social autopsy of disaster in Chicago. Chicago: University of Chicago Press; 2002. [DOI] [PubMed] [Google Scholar]
- 36.Rosenfield PL. The potential of transdisciplinary research for sustaining and extending linkages between the health and social sciences. Soc Sci Med. 1992;35:1343–57. doi: 10.1016/0277-9536(92)90038-r. [DOI] [PubMed] [Google Scholar]
- 37.Stokols D, Hall KL, Taylor BK, Moser RP. The science of team science: overview of the field and introduction to the supplement. Am J Prev Med. 2008;35(2S):XXX–XXX. doi: 10.1016/j.amepre.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 38.Warnecke RB, Oh A, Breen N, Gehlert S, et al. Approaching health disparities from a population perspective: the NIH Centers for Population Health and Health Disparities. Am J Public Health. 2008 doi: 10.2105/AJPH.2006.102525. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stokols D, Fuqua J, Gress J, et al. Evaluating transdisciplinary science. Nicotine Tob Res. 2003;5(1S):S21–S39. doi: 10.1080/14622200310001625555. [DOI] [PubMed] [Google Scholar]
- 40.Stokols D. Toward a science of transdisciplinary action research. Am J Community Psychol. 2006;38(1):63–77. doi: 10.1007/s10464-006-9060-5. [DOI] [PubMed] [Google Scholar]
- 41.Gehlert S, Rebbeck T, Lurie N, Warnecke R, Paskett E, Goodwin J. Cells to society: overcoming health disparities. Washington DC: National Cancer Institute; 2007. [Google Scholar]
- 42.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–24. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 43.Truong KD, Sturm R. Alcohol outlets and problem drinking among adults in California. J Stud Alcohol Drugs. 2007;68(6):923–33. doi: 10.15288/jsad.2007.68.923. [DOI] [PubMed] [Google Scholar]
- 44.Cohen D, McKenzie TL, Sehgal A, Williamson S, Golinelli D, Lurie N. Park use and physical activity in a sample of public parks in the City of Los Angeles. Am J Public Health. 2007;97(3):509–14. doi: 10.2105/AJPH.2005.072447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Walsh JME, McPhee SJ. A systems model of clinical preventive care: an analysis of factors influencing patient and physician. Health Educ Q. 1992;19(2):157–75. doi: 10.1177/109019819201900202. [DOI] [PubMed] [Google Scholar]
- 46.Gehlert S, Murray A, Sohmer D, McClintock M, Conzen S, Olopade O. The importance of transdisciplinary approaches for understanding and ameliorating health disparities. J Health Soc Policy. 2008 doi: 10.1080/19371910903241124. In press. [DOI] [PubMed] [Google Scholar]