Abstract
Abnormal or excessive force on the anterior hip joint may cause anterior hip pain, subtle hip instability and a tear of the acetabular labrum. We propose that both the pattern of muscle force and hip joint position can affect the magnitude of anterior joint force and thus possibly lead to excessive force and injury. The purpose of this study was to determine the effect of hip joint position and of weakness of the gluteal and iliopsoas muscles on anterior hip joint force. We used a musculoskeletal model to estimate hip joint forces during simulated prone hip extension and supine hip flexion under 4 different muscle force conditions and across a range of hip extension and flexion positions. Weakness of specified muscles was simulated by decreasing the modeled maximum force value for the gluteal muscles during hip extension and the iliopsoas muscle during hip flexion. We found that decreased force contribution from the gluteal muscles during hip extension and the iliopsoas muscle during hip flexion resulted in an increase in the anterior hip joint force. The anterior hip joint force was greater when the hip was in extension than when the hip was in flexion. Further studies are warranted to determine if increased utilization of the gluteal muscles during hip extension and of the iliopsoas muscle during hip flexion, and avoidance of hip extension beyond neutral would be beneficial for people with anterior hip pain, subtle hip instability, or an anterior acetabular labral tear.
Keywords: acetabular labral tear, groin pain, hip instability, hip joint force, hip pain
1. Introduction
The estimation of forces across the hip joint may provide insight into the etiology of hip pain. Abnormal or excessive loading of the hip has recently been recognized as a potential cause of anterior hip pain and subtle hip instability (Shindle et al., 2006). Hip instability and excessive hip forces may cause a tear of the acetabular labrum even in the absence of a traumatic event (Mason, 2001; McCarthy et al., 2001; Shindle et al., 2006). Understanding these joint forces may improve rehabilitation outcomes (Heller et al., 2001)
Decreased force contribution from the gluteal and iliopsoas muscles and hip hyperextension may contribute to anterior hip forces. Increased anterior gliding of the femoral head is proposed to result from weakness or decreased utilization of the gluteal muscles during hip extension and the iliopsoas muscles during hip flexion (Sahrmann, 2002). Increased anteriorly directed hip force is the likely cause for the increased anterior glide. Distance runners may be particularly at risk for increased anterior gliding due to the exaggerated hip extension position inherent in running (Sahrmann, 2002). This subtle instability along with repeated hip extension position may also lead to a tear of the acetabular labrum (Guanche and Sikka, 2005).
People with hip instability, anterior hip pain or acetabular labral tear report pain with certain hip movements. Hip extension with external rotation produces pain in patients with anterior hip pain and subtle instability (Philippon, 2001). Pain with resisted supine hip flexion with the knee maintained in extension (straight leg raising) is a common finding in patients with anterior hip pain and an anterior labral tear (Binningsley, 2003; McCarthy et al., 2001).
From these observations, we theorize that the anterior hip joint force is affected by both the balance of muscles contributing force to the movement and the hip position, and that increases in this force may lead to subtle hip instability, hip pain and acetabular labral tears. The purpose of this study was to determine the effect of decreased gluteal and iliopsoas muscle force contribution and hip joint position on the anterior hip force using a 3-dimensional musculoskeletal model. Specifically, we hypothesized that decreased force contribution from the gluteal muscles during hip extension and the iliopsoas muscle during hip flexion would result in a higher anterior hip force than when those muscles were functioning optimally. We also hypothesized that the magnitude of the anterior force would increase as the hip extension angle increased beyond neutral.
2. Materials and methods
2.1 Musculoskeletal model
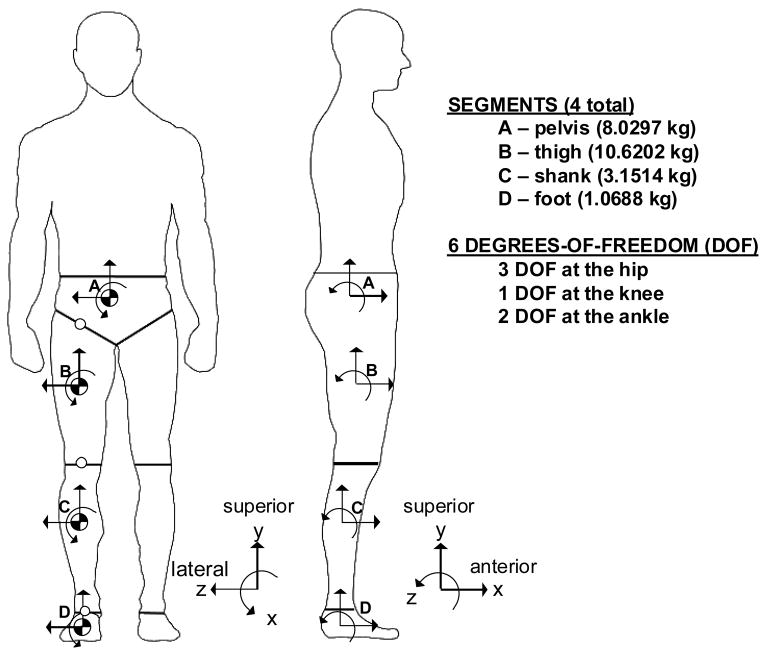
We used a 3-dimensional musculoskeletal model to estimate hip joint forces. The model was based on a bilateral model developed by Carhart (Carhart, 2003), that we simplified to include only 4 segments: the pelvis, thigh, shank and foot of the right leg. The model contained 6 degrees of freedom (DOF) to represent the primary motions at the hip, knee and ankle (Figure 1).
FIGURE 1.
Overview of the musculoskeletal model used in this study (adapted from Carhart (Carhart, 2003)). Illustration of the segmental reference frames in the frontal and sagittal plane for the pelvis (A), thigh (B), shank (C) and foot (D) with the subject standing in the anatomical position. In the pelvic reference frame, the superior/inferior axis is in line with the trunk when in a standing posture. The anterior/posterior axis is perpendicular to the superior/inferior axis and in line with the progression of movement in the anterior direction. The medial/lateral axis is defined as the cross product of the other two axes.
Musculoskeletal parameters, including muscle path and maximum isometric force, were adapted from work by Delp (Delp, 1990) for the 43 muscle units in the model. We modified the path of the iliopsoas muscle via an iterative process to be more consistent with the muscle moment arms as reported in a recent magnetic resonance imaging study of their architecture (Arnold et al., 2000). The muscle moment arms calculated by our model were in agreement with those calculated by SIMM (MusculoGraphics, Inc, Santa Rosa, CA) for the published models (Arnold et al., 2000; Delp et al., 1990). Kane’s Method (Kane and Levinson, 1985) and AUTOLEV 3.1 (OnLine Dynamics, Inc., Sunnyvale, CA) were used to generate the dynamic equations of motion. Because we were interested in hip joint forces when the limb was held in a position, we simplified the equations of motion to include only the torques due to muscle force and gravity. The general form of the simplified equations of motion is:
| (1) |
where M is the mass matrix, and Q⃗, T⃗, and G⃗ are the column vectors of the joint angles, the net joint torques due to muscle, and the torques due to gravity respectively. As we were modeling the limb in selected positions, and not when the limb was moving, the angular acceleration was always zero. Thus, the set of equations was simplified to:
| (2) |
indicating that the net muscle torques across all joints had to be equal and opposite the torques due to gravity. The torques due to gravity were estimated based on limb position, anthropometric parameters (Carhart, 2003), and gravity (9.81 m/s2). In a method similar to Yamaguchi and colleagues (Yamaguchi et al., 1995), we used an optimization routine (fmincon in MATLAB 6.5.1 (The MathWorks, Inc, Natick, MA)) to solve for the percentage of force contribution (PForce) from each muscle to generate net muscle torques which were equal and opposite to the torques due to gravity. PForce represents the level of force that the muscle is contributing as a percentage of the muscle’s maximal force, and was constrained between 0% (no force) and 100% (maximal force). The routine minimized the sum of the squared percentages of force contribution of the system. This routine is a scaled equivalent of minimizing muscle stress, which has the goal of maximum muscle endurance (Crowninshield and Brand, 1981). In this study, we manipulated the maximum muscle force values for selected muscles to test the effect of decreased muscle strength. This also allows us to indirectly test the effect of decreased muscle activation.
Once the optimized PForce for each muscle was solved simultaneously across all joints, the model estimated the resulting force in the hip joint due to muscle. We resolved the force into its three force components in the pelvic reference frame. As we were most interested in the forces which might result in anterior hip pain and acetabular labral injury, all forces are stated in terms of the force of the femur on the acetabulum. Specifically, an “anterior force” will indicate a force which is imparted from the femur onto the acetabulum, and is in the anterior direction without regard for the position of the femur.
2.2 Simulated hip exercises
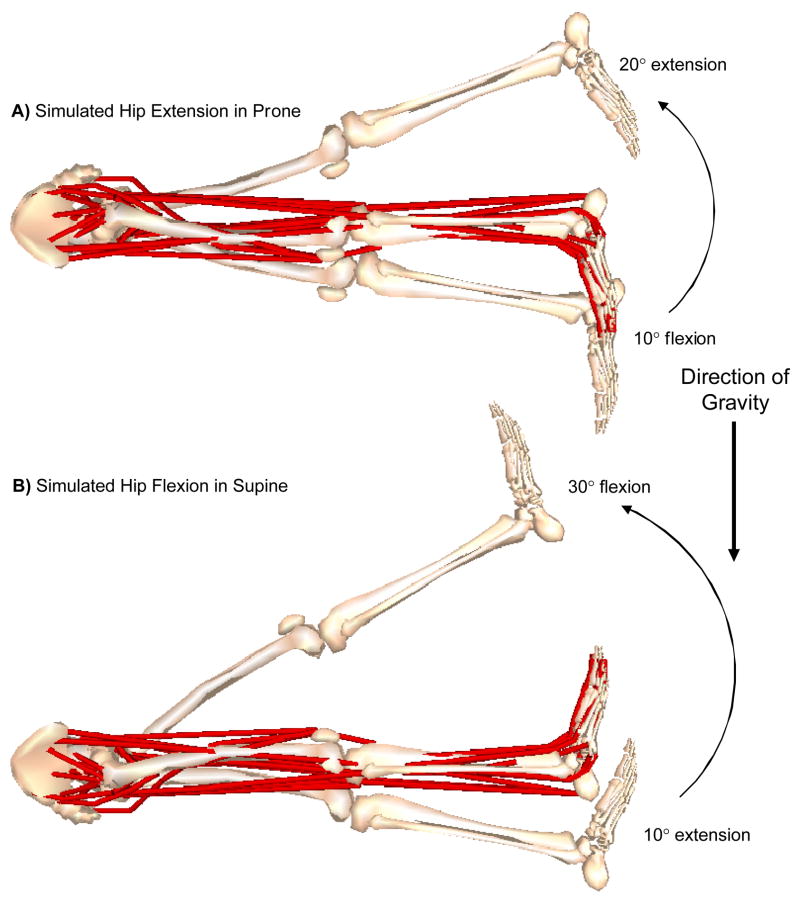
We estimated the anterior hip joint force during 2 simulated hip exercises: prone hip extension and supine hip flexion. To simulate prone and supine, we specified gravity as acting from posterior to anterior for prone and anterior to posterior for supine (Figure 2). We increased the hip joint angle in 1° increments from 10° of hip flexion to 20° of hip extension for prone hip extension and from 10° of hip extension to 30° of hip flexion for supine hip flexion. Prone hip extension started at 10° of hip flexion as it is recommended that patients start in hip flexion when performing this exercise to avoid hip hyperextension (Sahrmann, 2002). Supine hip flexion started at 10° of hip extension because this position is the presumed position of the hip when the lumbar spine is against the mat (Kendall et al., 1993) and should be the starting position for correct performance of a straight leg raise. For both exercises, we set the hip joint abduction/adduction and internal/external rotation angles, the knee joint angle and ankle joint angle at zero. These joint positions were maintained through balanced muscle torques about the joint degrees of freedom.
FIGURE 2.
Exercises simulated using the musculoskeletal model. A) Hip extension in prone: Gravity was specified as acting from posterior to anterior in line with the pelvic reference frame. The hip started in 10° of hip flexion and moved through 30° to a final position of 20° of hip extension. B) Hip flexion in supine: Gravity was specified as acting from anterior to posterior in line with the pelvic reference frame. The hip started in 10° of hip extension and was moved through 40° to a final position of 30° of hip flexion. (Image created in SIMM (MusculoGraphics, Inc, Santa Rosa, CA))
2.3 Conditions
We simulated 4 different conditions for each exercise to estimate the anterior hip force when the maximum muscle force value for selected muscles was reduced. For the hip extension simulation, we reduced the maximum force values of the gluteal muscles (gluteus maximus, medius, and minimus). For the hip flexion simulation, we reduced the maximum force values of the iliacus and psoas muscles. The first condition served as the control condition to which all other conditions were compared. For Condition 1, we solved for the set of muscle forces using the unaltered maximum muscle force values. For Conditions 2, 3, and 4, we reduced the maximum muscle force value for the selected muscles to 50%, 25% and 5% of normal to represent a range of strength and activation levels. The 5% of normal condition (Condition 4), in particular, represented the situation in which the muscle is significantly weak, is minimally activated, or a combination of the two. We recalculated the optimized set of muscle forces based on the reduced maximum muscle force values. For each set of muscle forces, we calculated the resulting hip joint forces.
2.4 Data analysis
The maximum anterior hip joint force under various conditions was the primary variable of interest. We determined the maximum anterior hip joint force per condition and calculated the percentage increase in joint force between Condition 1 and each condition ((Condition X − Condition 1)/Condition 1 × 100%). We also calculated the change in PForce between Condition 1 and every other condition for each muscle (PForce Condition X − PForce Condition 1). This change in PForce indicates which muscles increase (+) or decrease (−) their force contribution to compensate for the reduction in force from the gluteal or iliopsoas muscles. We then calculated the change in each individual muscle’s contribution to the anterior hip joint force as the difference between Condition 1 and every other condition (Muscle 1 Anterior Force Condition X − Muscle 1 Anterior Force Condition 1).
3. Results
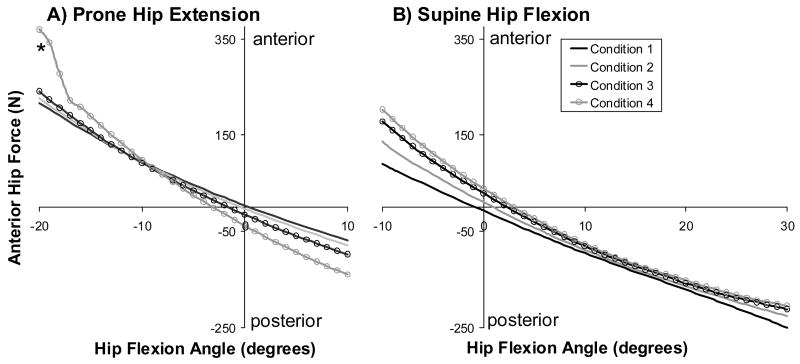
Decreased force contribution from the gluteal muscles during prone hip extension resulted in an increase in the anterior hip joint force (Figure 3). In Condition 4 at the end range of hip extension, the solution violates the PForce limit of 100% for muscles contributing to medial rotation torque, increasing PForce to 100.1% at 19° and 100.3 at 20° of hip extension. The maximum anterior joint force in Condition 4 was 152.6 N greater than in Condition 1, an increase of 19.2% of body weight (Table 1). As the maximum gluteal muscle force value decreased, the model increased the PForce of the semimembranosis muscle, the tensor fascia lata (TFL) muscle, and the sartorius muscle (Table 2). The majority of the increase in the maximum anterior hip joint force was due to the semimembranosis muscle. The anterior force due to the semimembranosis muscle alone in Condition 4 was 262.0 N, an increase of 172.8 N from Condition 1.
FIGURE 3.
Maximum anterior hip force with decreasing force contribution from: A) the gluteal muscles during prone hip extension and B) the iliopsoas muscle during supine hip flexion for each condition. Condition 1 is 100%, 2 is 50%, 3 is 25%, and 4 is 5% of the maximum isometric force for the gluteal and iliopsoas muscles for hip extension and hip flexion respectively. Regardless of changes in muscle force contribution, the anterior hip force increases with increasing hip extension. Reducing the force contribution from the gluteal muscles during hip extension and the iliopsoas muscle during hip flexion further increases the anterior hip joint force when the hip is in the extended position. * At the end range of hip extension in Condition 4, the solution violates the upper bound of percentage of muscle force (>100.0%) for muscles contributing to medial rotation torque.
TABLE 1.
Maximum anterior hip joint forces using different percentages of maximum muscle force. The maximum hip force occurs at the greatest hip extension angle, 20° for prone hip extension, and 10° for supine hip flexion. For both exercises, the maximum anterior force increases with decreasing force contribution from specific muscles. Condition 1 is 100%, 2 is 50%, 3 is 25%, and 4 is 5% of the maximum isometric force for the gluteal (hip extension) and iliopsoas (hip flexion) muscles.
| Condition | |||||
|---|---|---|---|---|---|
| Exercise | Variable | 1 | 2 | 3 | 4 |
| Prone hip extension | Maximum anterior hip joint force (N) | 217.1 | 226.8 | 241.2 | 369.7 |
| Percent increase from Condition 1 (%) | N/A | 4.5 | 11.1 | 70.3 | |
| Supine hip flexion | Maximum anterior hip joint force (N) | 90.6 | 136.3 | 178.3 | 203.0 |
| Percent increase from Condition 1 (%) | N/A | 50.5 | 96.8 | 124.1 | |
TABLE 2.
Changes in the percentage of muscle force contribution (PForce) with reduction of maximal force value for specified muscles. The primary hip muscles in which PForce increases from Condition 1 to Condition 4 during the two exercises are listed below. The change in maximum anterior hip joint force is the increase in the maximum anterior hip joint force contributed by each muscle between Condition 1 and Condition 4. Condition 1 is 100% and Condition 4 is 5% of the maximum isometric force for the gluteal and iliopsoas muscles.
| Exercise | Muscle | PForce Condition 1 (%) | PForce Condition 4 (%) | Change in PForce (%) | Change in maximum anterior hip joint force (N) |
|---|---|---|---|---|---|
| Prone hip extension | Semimembranosis | 26.5 | 77.9 | 51.4 | 172.8 |
| Tensor fascia lata | 1.0 | 100.3 | 99.3 | 32.9 | |
| Sartorius | 0.0 | 100.3 | 100.3 | 41.6 | |
| Supine hip flexion | Tensor fascia lata | 24.7 | 93.3 | 68.6 | 13.0 |
| Sartorius | 20.2 | 78.2 | 58.0 | 16.0 | |
| Adductor longus | 12.9 | 65.7 | 52.8 | 66.6 |
Similarly, decreased force contribution from the iliopsoas muscle during supine hip flexion resulted in an increase in the maximum anterior hip force. The maximum anterior hip force in Condition 4 was 112.4 N greater than in Condition 1, an increase of 14.1% of body weight (Table 1). As the maximum iliopsoas force value decreased, the model increased the PForce of the TFL, the sartorius, and the adductor longus (Table 2). The majority of the increase in the maximum anterior hip joint force was due to the adductor longus muscle (an increase of 66.6 N between Conditions 1 and 4).
In both simulations, the anterior hip force increased with increasing hip extension angle regardless of muscle participation. The maximum anterior force for each simulated exercise was at the maximum angle of hip extension, 20 degrees for prone hip extension and 10 degrees for supine hip flexion (Figure 3).
4. Discussion
The primary results of the musculoskeletal model indicate that the anterior hip joint force due to muscle increases with a) decreasing force contribution from the gluteal muscles during hip extension, b) decreasing force contribution from the iliopsoas muscle during hip flexion, and c) increasing hip extension angle. These results are consistent with reported pain behaviors associated with anterior hip pain and anterior labral tears.
Although the modeled weakness of specific muscles was based on the clinical observation, the resulting modifications in muscle forces to compensate for the weakened muscles are also consistent with clinical observations. Sahrmann reports that when patients with anterior hip pain and subtle instability perform prone hip extension only minimal contraction of the gluteal muscles is noted. In contrast, significant contraction of the hamstring muscles, especially the medial hamstring muscle is noted (Sahrmann, 2002). Similarly, the model predicts an increase in semimembranosis muscle force contribution when the force from the gluteal muscles is reduced. The semimembranosis is preferentially increased over the other hamstring muscles (semitendinosis and biceps femoris) as the semimembranosis muscle has the smallest lateral rotation and adduction moment arms of the three muscles relative to the hip extension moment arm in 20° of hip extension. The smaller lateral rotation moment appears to be important, especially in the 95% reduction condition, when the solution violates the upper PForce limit for muscles with medial rotation moment arms. This need for medial rotation and abduction torque to offset the lateral rotation and adduction torque generated by the semimembranosis also drives the increase in TFL and sartorius muscles despite producing hip flexion torques. Without this specific control of rotation, the femur would laterally rotate in extension, a position found to be painful for patients with hip pain and subtle hip instability (Philippon, 2001).
Sahrmann has also reported that in patients with anterior hip pain, the hip medially rotates during supine hip flexion suggesting that the action of the TFL is dominant over the iliopsoas muscle (Sahrmann, 2002). When performing supine hip flexion, the model predicts that the TFL, along with the sartorius and adductor longus muscles, increases its force contribution when the force contribution from the iliopsoas muscle was decreased. The TFL and sartorius act to flex the hip while the adductor longus counteracts the excessive hip abduction torque generated by the TFL and sartorius.
The increase in anterior hip force with increasing hip extension angle is also consistent with clinical observations of runners with hip pain, and may play a greater role in the development of anterior hip pain than changes in muscle force contribution. Anterior hip force consistently increased with increasing hip extension angle. This increase in anterior force may help explain the presence of subtle hip instability and acetabular labral tears reported in distance runners who frequently achieve angles of hip hyperextension (Sahrmann, 2002; Guanche and Sikka, 2005).
Although the magnitude of the of the change in anterior hip joint force (152.6 N, or 19.2% body weight) may seem minimal for a joint that is reported to withstand forces around four times body weight during walking and even higher during running or stumbling (Bergmann et al., 1993; Bergmann et al., 2004), two factors need to be considered when interpreting the forces reported here. First, the change in force is only the change in the anterior component of the force, and not the change in the total resultant force. Second, the anterior portion of the acetabulum has limited bony containment and gains the majority of its stability from soft tissues including acetabular labrum, joint capsule, ligaments and muscles (Lewis and Sahrmann, 2006). Although the bony structure of the acetabulum may be able to withstand forces up to four times body weight, the soft tissue structures of the anterior hip joint may become injured at much lower force levels, especially when the force is applied repeatedly. The critical threshold for injury for these tissues is unknown.
The results of this study may provide insight into the development of anterior hip pain, subtle hip instability and anterior acetabular labral tears. Positions of hip extension as well as certain alterations in muscle force contributions result in an increase in the anterior hip joint force. The increased anterior force, if repeated frequently over time, may lead to hip pain, instability and a tear of the acetabular labrum. The majority of these labral tears are reported to be in the anterior region (McCarthy et al., 2001; Farjo et al., 1999; Klaue et al., 1991; O’leary et al., 2001; Santori and Villar, 2000); a finding which may be explained, in part, by this increased anterior force in combination with the limited bony containment of the femoral head anteriorly within the acetabulum.
Understanding hip joint forces may also improve rehabilitation outcomes (Heller et al., 2001). Based on the results of this study, people with anterior hip pain and subtle hip instability or with an anterior acetabular labral tear may be able to decrease anterior hip joint forces by 1) increasing the force contribution of the gluteal muscles during hip extension, 2) increasing the force contribution of the iliopsoas muscle during hip flexion, and 3) avoiding hip extension beyond neutral. Distance runners with anterior hip pain and an acetabular labral tear may also benefit from decreasing the amount of hip hyperextension. The results of this simulation study provides a theoretical basis for conducting further clinical studies to quantify muscle strength and determine if these modifications are beneficial for patients with anterior hip pain.
To our knowledge, our study is the first to investigate anterior hip joint forces from the perspective of the acetabulum during hip exercises. Acetabular contact pressures during hip extension and hip flexion exercises have been evaluated previously by Tackson et al. in a single subject with an instrumented endoprosthesis (Tackson et al., 1997). They found that performing prone hip extension resulted in a maximum pressure of 4.4 MPa while supine hip flexion resulted in 3.7 MPa. However, Tackson et al. do not report in what area of the acetabulum these maximum pressures occurred. Furthermore, direct comparisons to our data are not possible as they measured pressures (pressure = force/area), and not joint forces.
As with all musculoskeletal models, there are limitations inherent in attempting to model complex human movement with simplified lines of action for muscles and computerized optimization routines for motor control. One major limitation specific to this study was our inability to accurately model the effect, if any, of the iliopsoas muscle as it passes over the front of the femoral head. The iliacus and psoas muscles may be similar to the rotator cuff muscles of the shoulder, applying forces to the femur not only through their muscle insertion, but also through their muscle bellies and tendons as they pass over the underlying structures. It has been suggested that the psoas muscle tendon adds strength to the anterior hip joint capsule when in hip extension (Philippon, 2001), especially in the presence of capsular laxity (Shindle et al., 2006). Another limitation is that we modified the maximum muscle force of only the gluteal muscles and the iliopoas muscle based on clinical observations (Sahrmann, 2002) that have yet to be objectively documented. Thus, there is a lack of evidence for actual compromised performance of these muscles. The optimization criterion used to determine Pforce is another limitation. We used an optimization routine which minimized the sum of the squared PForce over the system of muscles. Theoretically, this optimization function captures the physiological properties of muscle (muscle moment arm and maximum muscle strength), as well as the goal of maximum muscle endurance (Crowninshield and Brand, 1981). Similar optimization routines have been used with this model in the prediction of muscle forces during gait and have resulted in “intuitively reasonable” solutions (Carhart, 2003). Another limitation is that we modeled only static behavior. Because both of the exercises used in this study are typically performed at a slow velocity (30° per second) and within the normal range of motion, we did not include torques from inertia, passive joint structures or viscoelastic damping.
4.1 Summary
The musculoskeletal model predicted that decreased force contribution from the gluteal muscles during active hip extension and from the iliopsoas muscle during active hip flexion resulted in a higher anterior hip joint force than when those muscles contributed more force to the movement. Also, the model predicted that the anterior hip joint force increased with increasing hip extension range of motion. The increased anterior hip joint force may contribute to anterior hip pain, subtle hip instability and the development of anterior acetabular labral tears. Reduction in the anterior joint force may be beneficial for patients with these conditions.
Acknowledgments
This work was supported in part by the National Institutes of Health (HD07434 and HD007422). We would also like to thank Dominic Chaloner for help with the figures and Michael Carhart for assistance with the musculoskeletal model.
Footnotes
Conflict of interest
The three authors affirm that they have no financial affiliation or involvement with any commercial organization that has direct financial interest in any matter included in this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- Arnold AS, Salinas S, Asakawa DJ, Delp SL. Accuracy of muscle moment arms estimated from MRI-based musculoskeletal models of the lower extremity. Comput Aided Surg. 2000;5:108–119. doi: 10.1002/1097-0150(2000)5:2<108::AID-IGS5>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- Bergmann G, Graichen F, Rohlmann A. Hip joint loading during walking and running, measured in two patients. J Biomech. 1993;26:969–990. doi: 10.1016/0021-9290(93)90058-m. [DOI] [PubMed] [Google Scholar]
- Bergmann G, Graichen F, Rohlmann A. Hip joint contact forces during stumbling. Langenbecks Arch Surg. 2004;389:53–59. doi: 10.1007/s00423-003-0434-y. [DOI] [PubMed] [Google Scholar]
- Binningsley D. Tear of the acetabular labrum in an elite athlete. Br J Sports Med. 2003;37:84–88. doi: 10.1136/bjsm.37.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart MR. Biomechanical analysis of compensatory stepping: implications for paraplegics standing via FNS. Doctor of Philosophy Arizona State University; 2003. [Google Scholar]
- Crowninshield RD, Brand RA. A physiologically based criterion of muscle force prediction in locomotion. J Biomech. 1981;14:793–801. doi: 10.1016/0021-9290(81)90035-x. [DOI] [PubMed] [Google Scholar]
- Delp SL. Parameters for a model of the lower limb. http://www.isbweb.org/data/delp/. 1990. http://www.isbweb.org/data/delp/. 12-1-2005.
- Delp SL, Loan JP, Hoy MG, Zajac FE, Topp EL, Rosen JM. An interactive graphics-based model of the lower extremity to study orthopaedic surgical procedures. IEEE Trans Biomed Eng. 1990;37:757–767. doi: 10.1109/10.102791. [DOI] [PubMed] [Google Scholar]
- Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy. 1999;15:132–137. doi: 10.1053/ar.1999.v15.015013. [DOI] [PubMed] [Google Scholar]
- Guanche CA, Sikka RS. Acetabular labral tears with underlying chondromalacia: a possible association with high-level running. Arthroscopy. 2005;21:580–585. doi: 10.1016/j.arthro.2005.02.016. [DOI] [PubMed] [Google Scholar]
- Heller MO, Bergmann G, Deuretzbacher G, Durselen L, Pohl M, Claes L, Haas NP, Duda GN. Musculo-skeletal loading conditions at the hip during walking and stair climbing. J Biomech. 2001;34:883–893. doi: 10.1016/s0021-9290(01)00039-2. [DOI] [PubMed] [Google Scholar]
- Kane TR, Levinson DA. Dynamics: theory and application. McGraw-Hill; New York, NY: 1985. [Google Scholar]
- Kendall FP, McCreary EK, Provance PG. Muscles Testing and Function. Williams & Wilkins; Baltimore, MD: 1993. [Google Scholar]
- Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423–429. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]
- Lewis CL, Sahrmann SA. Acetabular labral tears. Phys Ther. 2006;86:110–121. doi: 10.1093/ptj/86.1.110. [DOI] [PubMed] [Google Scholar]
- Mason JB. Acetabular labral tears in the athlete. Clin Sports Med. 2001;20:779–790. doi: 10.1016/s0278-5919(05)70284-2. [DOI] [PubMed] [Google Scholar]
- McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop. 2001:25–37. doi: 10.1097/00003086-200112000-00004. [DOI] [PubMed] [Google Scholar]
- O’Leary JA, Berend K, Vail TP. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy. 2001;17:181–188. doi: 10.1053/jars.2001.21481. [DOI] [PubMed] [Google Scholar]
- Philippon MJ. The role of arthroscopic thermal capsulorrhaphy in the hip. Clin Sports Med. 2001;20:817–829. doi: 10.1016/s0278-5919(05)70287-8. [DOI] [PubMed] [Google Scholar]
- Sahrmann SA. Diagnosis and treatment of movement impairment syndromes. Mosby, Inc; St. Louis, MO: 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santori N, Villar RN. Acetabular labral tears: result of arthroscopic partial limbectomy. Arthroscopy. 2000;16:11–15. doi: 10.1016/s0749-8063(00)90121-x. [DOI] [PubMed] [Google Scholar]
- Shindle MK, Ranawat AS, Kelly BT. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med. 2006;25:309–326. doi: 10.1016/j.csm.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Tackson SJ, Krebs DE, Harris BA. Acetabular pressures during hip arthritis exercises. Arthritis Care Res. 1997;10:308–319. doi: 10.1002/art.1790100505. [DOI] [PubMed] [Google Scholar]
- Yamaguchi GT, Moran DW, Si J. A computationally efficient method for solving the redundant problem in biomechanics. J Biomech. 1995;28:999–1005. doi: 10.1016/0021-9290(94)00145-t. [DOI] [PubMed] [Google Scholar]