Abstract
The fear avoidance model (FAM) postulates that fear of pain or reinjury is a risk factor for persistent pain and disability, because it leads to avoidance of physical activity. Research on the FAM has not yielded consistent results, which may be attributed to the model itself, but could also be a product of the way fear of movement is assessed. Studies of the FAM have measured fear using verbal scales consisting of items that are often vague and have only an indirect relationship with fear. This study reports on the development of a Pictorial Fear of Activity Scale – Cervical (PFActS-C). The instrument consists of a set of photographs depicting movements in which 4 factors that determine biomechanical demands on the neck are systematically varied - Direction of Movement, Arm Position, Weight Bearing, and Extremity of Movement. Patients (n = 355) who had been involved in motor vehicle collisions with minimal symptoms (n = 143) and moderate to severe symptoms (n = 212) rated their fear of engaging in a set of activities depicted in the PFActS-C. Based on a principle components analysis, a 19-item measure was developed. Internal consistency (alpha = .98), stability over time (n = 44, IntraClass Correlation = .72), and construct validity were all good to excellent. The results indicate that the PFActS-C may be a useful tool for assessing fear of movement in patients with cervical pain. Research is needed to confirm the factor structure of the PFActS-C and to assess the generalizability of the results to other samples with neck pain.
Keywords: Fear of movement, instrument development, motor vehicle collisions, neck pain, cervical injury
1. Introduction
The etiology of persistent cervical pain following motor vehicle collisions (MVCs) is poorly understood. However, psychological factors have been shown to be important predictors of chronicity [6,8]. Fear of activities that might cause increased pain or re-injury represents one such factor. The fear avoidance model (FAM [34, 36]) postulates that cognitive responses (e.g., excessive negative thinking) following painful experiences lead to fear of movement. This fear of movement induces the person to avoid activities believed to aggravate the injury and cause additional pain. In the long run, however, it may reinforce “catastrophizing”, fear responses, and continued avoidance of movement and promote de-conditioning and disability.
The FAM has stimulated research demonstrating that fear of activity is common among individuals with persistent pain following musculoskeletal injuries [19], and that a high fear level shortly after injury is a risk factor for the subsequent development of disability [10, 23, 26, 29]. However, the results of studies on the FAM have not been consistent [see 25, 25]. One possible interpretation of the inconsistent empirical support for the FAM is that the model itself is inherently flawed. However, it is also possible that the model is valid, but that the inconsistencies observed relate to problems in the measurement of the key construct in the model – fear of activity.
The Tampa Scale of Kinesiophobia (TSK [16]) is the instrument that has been used most to assess fear of movement/(re)injury in research on the FAM (e.g., 7, 13, 30]. Despite its widespread use, the TSK has limitations. The verbal items that make up the scale are abstract and several have little direct relationship to fear of activity (e.g., “My body is telling me I have something dangerously wrong.”). At least in some samples of chronic pain patients the factor structure of the scale is problematic [2].
The present paper describes the Pictorial Fear of Activity Scale-Cervical (PFActS-C), a tool for assessing fear among individuals with neck pain. The PFActS-C differs from the TSK in 3 crucial respects. First, it assesses fear specifically related to neck pain, rather than attempting to assess fear in the context of any painful condition. Second, it uses pictorial stimuli rather than verbal statements to elicit fear ratings. Third, the PFActS-C permits assessments to be made of the extent to which specific kinds of biomechanical loads – such as direction of neck movement and position of arms - influence participants’ fear ratings. The only other fear of movement instrument to use of pictorial stimuli is the Photograph Series of Daily Activities (PHODA [17, 20]; however the pictures used do not vary mechanical loads in a systematic way and involve potential stresses on multiple musculoskeletal structures. The objectives of the present study were to describe the development of the PFActS-C and provide initial evidence for its validity and reliability.
2. Methods
2.1. Construction of the PFactS-C
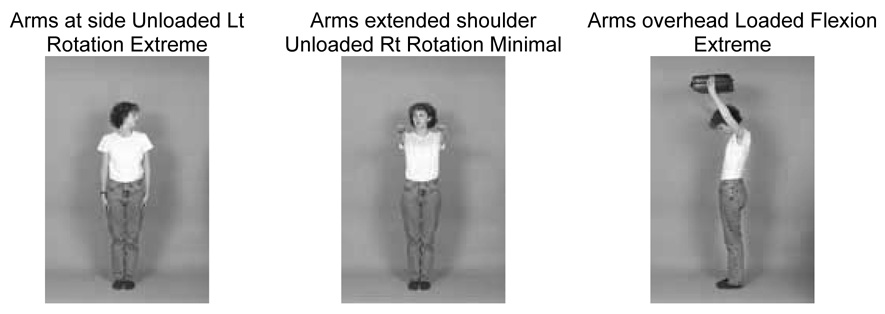
The initial version of the PFactS-C consisted of 77 photographs of a female model engaged in a variety of activities that place biomechanical stresses on the neck, and thus might be viewed as threatening by individuals with neck injuries. Several variables thought to influence fear ratings were systematically manipulated in the pictures – Direction of Movement (Flexion, Extension, Right lateral bending, Left lateral bending, Right rotation, Left rotation), Arm Position (At sides, At shoulder height, Overhead), Weight Bearing (Holding an attaché case vs. nothing held in her arms), and Extremity of Movement (Moderate excursion vs. Extreme excursion). These 4 factors were varied in a 6×3×2×2 factorial design to yield 702 “active” pictures. In addition, the PFActS-C contains 5 Control pictures in which the model engages in activities that are unlikely to stress the neck directly, and, therefore are less likely to provoke fear among respondents who have sustained neck pain. Examples of PFActS pictures illustrating the variable manipulated are shown in Figure 1. Each photograph was presented to participants in a random order. Respondents were asked to view each picture and indicate “how worried or fearful you would be to carry out the activity shown in the picture” on a scale from 0 (“no fear at all”) to 10 (“extremely fearful”).
Figure 1.
Examples of PFActS-C Photographs
2.2. Participants
Item analysis and psychometric assessment of the PFActS-C were conducted on a sample of 355 (242 female) participants. Participants were recruited from community physicians and media announcements describing a treatment study for people who had been involved in motor vehicle collisions (MVCs) and who had sustained a neck injury. Inclusion criteria were: (1) involvement in a MVC in past 1–3 months, (2) some degree neck pain, (3) meet the criteria of the Quebec Task Force on Whiplash Associated Disorders (WAD), levels 1 and 2 (i.e., muscular symptoms and neurological signs but not hospitalized following collision, no loss of consciousness, no fractures or dislocations [27]) assessed by a physical examination performed by a physician board-certified in Physical Medicine and Rehabilitation with extensive experience with patients with WADs (J.P.R,), (4) no current substance abuse, and (5) fluency in the English language. Participants were divided into 2 subgroups on the basis of their ratings of their maximal neck pain during the previous week. Those who gave a rating of 4 or more over 10 were described as moderately to severely symptomatic, designated SX (n=212; 149 females) and those who gave a rating of 3 or less were described as minimally symptomatic, designated MSX (n=143; 93 females).
2.3. Procedure
Participants were examined by a physician and a psychologist. The physician took a detailed history and performed a physical examination (described below). Participants completed the PFActS-C and a set of self-report inventories used for validation purposes (described below). The Institutional Review Board at the University of Washington approved this study. All participants completed an informed consent document prior to participation in the study.
2.4. Validation Measures
2.4.1. Tampa Scale of Kinesophobia (TSK)
The TSK is a self-report instrument designed to assess fear of pain and reinjury due to activity. It consists of 17 items, each rated on a 4-point Likert-type scale [16]. Kori et al. originally developed the measure in English and did not systematically evaluated its psychometric properties, although it was later translated into Dutch by Vlaeyen and colleagues [34] and subsequently used in research related to fear of activity among patients with chronic low back pain patients. Test-retest reliability of the Total Score of the TSK has been established in a sample of patients with acute low back pain (Pearson’s r = .78) [30] and internal consistency reliability has been reported in studies of patients with chronic low back pain (Cronbach’s alpha ranges from .68 to.80) using the Dutch translation. Most recently, the psychometric properties of the original English version were evaluated and demonstrated to be acceptable [7]. Several authors have advocated for a 2-factor structure of the TSK [10, 13], however, the Total Score has been used more frequently and is recommended by authors who initially presented a factor analysis of the TSK [35]. The TSK, the only FAM measure used with cervical pain available [11], was used in this study to determine the convergent validity of the PFActS-C (discussed below).
2.4.3. Physical Examination Measures
Cervical Range of Motion was evaluated by the examining physician, using the methods described by Gerhardt et al. [12]. Flexion, extension, right and left rotation, and right and left lateral flexion were measured. The examiner also used a force transducer (JAMAR) to determine the isometric strength of participants’ neck flexors, extensors, and right and left lateral flexors.
2.4.4. Other validation measures
A set of self-report measures were used to assess the convergent and discriminant validity of the PFActS-C. These consisted of the Neck Disability Index (NDI [32]) Multidimensional Pain Inventory (MPI [15], Pain Anxiety Symptoms Scale (PASS [21]), and the Pain Catastrophizing Scale (PCS [28]). Each of these measures has been used with various samples of patients with pain and has been shown to have good to excellent psychometric properties.
3. Statistical Analysis
3.1 Face Validity
A 6×3×2×2 repeated measures ANOVA was performed on fear ratings, with Direction of Movement, Position of Arms, Weight bearing (loaded) versus Unloaded, and Extremity of Movement as independent variables. This analysis was performed to test our a priori hypotheses that fear levels would be relatively high for pictures depicting Extreme movement, Weight bearing, and Arms extended overhead.
3.1. Item Reduction
As discussed below, the 36 Moderate Excursion PFActS-C pictures were eliminated from further consideration based on their high correlation with the 36 Extreme Excursion items. The remaining 41 items (36 Extreme Excursion items + 5 control items) were entered into a factor analysis using a principal component factoring method and an orthogonal varimax rotation with Kaiser Normalization [14] to further reduce the measures length and preliminarily examine its factor structure.
3.2. Reliability
Cronbach's coefficient alpha [4] was calculated to determine the internal consistency of the PFActS-C. A subset of 44 patients completed the PFActS-C at 2 time periods (mean time between first and second administrations was 18.53 days (SD = 9.30). Stability was calculated using the Intra Class Correlation (ICC) as an alternative to the Pearson’s product moment correlation. ICCs vary from 0, indicating complete lack of reliability to one indicating perfect reliability with no measurement error. ICC values above .75 indicate good reliability [22].
3.3. Validity
Convergent validity was assessed by correlating the PFActS-C with other measures of fear/anxiety (TSK, PASS, PCS), as well as with pain intensity, and neck disability. Convergent validity was further assessed using a multimethod approach by correlating the PFActS-C with indices of neck function (Cervical Range of Motion). Discriminant validity was assessed by correlating the PFActS-C with measures hypothesized to have little or no association with the PFActS-C (i.e., demographic variables, MPI Support, TSK Importance of Exercise subscale [35]).
The construct validity of the PFActS-C was evaluated utilizing the known groups method, as well as by convergent and discriminant validity. The known-groups method compares scale scores across groups known to differ in the construct being investigated. In this study, groups differing in known health status (moderate-to-severely symptomatic vs. minimally symptomatic) were computed using independent sample t-tests. We hypothesized that individuals with moderate to severe symptoms would report higher scores on the PFActS-C than minimally symptomatic people. All analyses were conducted using SPSS for Windows version 14.0.
4. Results
4.1. Sample Characteristics
Participants were 355 people with reported cervical pain following a MVC and who met the Quebec Task Force Classification of WADs level 1 or 2. Demographics for both groups are presented in Table 1. A majority of the participants in the full sample were female (n = 242, 68.2%) and Caucasian (n = 261, 73.5%), with an average age of 36.60 years (SD = 12.90, Range = 16–71 years).
Table 1.
Demographic Variables by Symptoms Group
| Minimally Symptomatic (N=143) | Moderately to Severely Symptomatic (N=212) | |
|---|---|---|
| Age (years, SD) | 34.82 (13.57) | 37.80 (12.33) |
| Sex (%) | ||
| Female/Male | 65/35 | 70.3/29.7 |
| Marital Status (%) | ||
| Married | 27.7 | 30.8 |
| Single | 44.7 | 29.8 |
| Divorced | 12.1 | 14.2 |
| Living with partner | 12.8 | 12.3 |
| Other | 2.7 | 12.9 |
| Education (%) | ||
| Less than 12th grade | 1.4 | 1.4 |
| High School Grad | 2.9 | 9.1 |
| Some college | 26.4 | 35.9 |
| College degree | 45.7 | 34.9 |
| Post graduate degree | 23.6 | 18.7 |
| Race (%) | ||
| White, non hispanic | 73.6 | 74.9 |
| Hispanic | 2.9 | 6.6 |
| Black, non Hispanic | 2.1 | 4.7 |
| Asian or Pacific Islander | 9.3 | 4.3 |
| Am Indian/Alaska Native | 1.4 | 2.4 |
| Other | 10.7 | 7.1 |
| Household Income (%) | ||
| <$10,000 | 9.0 | 10.3 |
| $10,000–$20,000 | 18.0 | 18.7 |
| $20,001–$30,000 | 14.3 | 16.3 |
| $30,001–$40,000 | 10.5 | 16.3 |
| $40,001–$50,000 | 10.5 | 5.9 |
| $50,001–$60,000 | 9.8 | 5.9 |
| $60,001–$70,000 | 6.8 | 7.4 |
| >$70,001 | 21.1 | 19.2 |
| TSK Total Score (SD) | 35.4 (6.2) | 40.2 (5.8) |
| PASS Total Score (SD) | 54.6 (24.0) | 68.7 (27.8) |
| PCS Total Score (SD) | 9.8 (8.2) | 15.8 (10.5) |
| NDI (SD) | 8.1 (5.9) | 16.5 (7.3) |
TSK, Tampa Scale of Kinesiophobia; PASS, Pain Anxiety Symptom Scale; PCS, Pain Catastrophizing Scale; NDI, Neck Disability Index
MVC related characteristics and means (SD) for the self-report instruments for both groups are presented in Table 2. Prior to the MVC, 85.4% of the full sample was employed. At the time of assessment, 77.5% of the sample was employed, of whom only 48.2% were employed full-time. 6.2% of the sample reported that they were not working due to pain. The onset of pain following the MVC was variable, with 43.0% of the full sample reporting pain immediately, 30.2% later the same day as the collision, 23.6% between 1–3 days following the MVC, and 3.2% more than 4 days afterwards. Participants reported that they experienced pain primarily in the neck (90.4%), shoulders (72.8%), head (71.1%), and upper back (64.9).
Table 2.
Accident Related Characteristics
| Minimally Symptomatic (N=143) | Moderately to Severely Symptomatic (N=212) | |
|---|---|---|
| Employed prior to MVC | ||
| Yes | 85.8% | 85.8% |
| Employed after MVC | ||
| Yes | 86.3% | 80.9% |
| Onset of pain | ||
| Immediately | 41.5% | 44.0% |
| Later, same day | 31.0% | 29.7% |
| 1–3 days after MVC | 24.6% | 23.0% |
| 4–5 days after MVC | 1.4% | 1.9% |
| >5 days after MVC | 1.4% | 1.4% |
| Location of pain | ||
| Neck | 93.0% | 91.0% |
| Shoulders | 65.5% | 77.7% |
| Head | 68.3% | 73.0% |
| Upper back | 64.1% | 65.4% |
| Other symptoms | ||
| Stiffness in neck | 64.8% | 94.8% |
| Muscle tenderness | 53.5% | 77.7% |
| Sleep disturbance | 53.5% | 76.8% |
| Headaches | 43.7% | 69.7% |
| Morning Stiffness | 38.3% | 61.9% |
| Fatigue | 34.5% | 56.4% |
Age, marital status, education level, annual household income, current employment status, and ethnicity were not significantly associated with the PFACTS-C total score. However, females scored significantly higher (Mean = 2.38, SD = 2.19) on the PFActS-C total score than males (Mean = 1.66, SD = 1.68; t = −3.09, p < 0.05).
4.2. Face Validity
We predicted that fear ratings of participants would be affected: (1) by arm position, with arms overhead eliciting the highest ratings, and arms at sides eliciting the lowest ones; (2) by Weight Bearing condition, with Loaded pictures eliciting higher ratings than Unloaded ones; and (3) by Extremity of motion, with Extreme movements eliciting higher ratings than Moderate ones. To test these predictions, a 6×3×2×2 repeated measures ANOVA was performed on SX participants, with Direction of Movement, Arm Position, Weight Bearing Condition, and Extremity of Movement as the independent variables, and fear ratings as the dependent variable.
As predicted, there was a significant effect of Arm Position (F2,202 = 150.92, p < 0.001), with arms extended overhead eliciting the highest ratings (Mean = 3.61, SD =2.26), and arms at sides eliciting the lowest ones (Mean =2.47, SD =1.8). Also, as predicted participants gave higher fear ratings to Weight bearing pictures (Mean =3.98, SD =2.45) than to Non-weight bearing (Mean =2.07 SD =1.81) ones (F1,203 = 269.04, p < 0.001), and to ones demonstrating Extreme movements (Mean =3.43, SD =2.09) compared to ones demonstrating Moderate movements (Mean =2.54, SD =1.98) (F1,203 = 164.12, p < 0.001). Although no predictions were made about the effect of Direction of Movement, it is interesting that this variable was also statistically significant (F5,199 = 14.47, p < 0.001). Fear ratings as a function of Direction of Movement were ordered as follows: Extension > Flexion > Left Lateral Bending > Left Rotation > Right Rotation > Right Lateral Bending.
4.5. Item Reduction
Since fear ratings for the 36 Extreme movement photographs were highly correlated with fear ratings for the 36 Moderate movement pictures (r =.86, p < 0.001), we decided to reduce the length the PFActS-C and hence respondent burden by eliminating the Moderate movement pictures. All analyses described below were performed on the 36 Extreme movement pictures and the 5 Control pictures.
An exploratory factor analysis was conducted on the remaining 41 (36 extreme excursion, 5 control) items using a Principal Components Axis Factoring method. The Kaiser-Guttman criterion, which suggests retaining all components with an eigenvalue >1.0, resulted in a 5 factor solution with eigenvalue magnitudes of 23.43, 3.93, 2.44, 1.48, and 1.22. These factors explained 57.16%, 9.61%, 5.97%, 3.61%, and 2.98% of the variance. Examination of these eigenvalues and factor loadings suggests that the most parsimonious solution is a single factor solution. Table 3 presents the rotated component matrix using the principal components extraction method and varimax rotation. Items were retained if their loadings were greater than .40 on the single underlying factor as suggested by Bordens and Abbot [1]. Using this criterion, 19 items were retained. These included all of the photographs in which the model was weight bearing (18 pictures) and 1 photograph where the model was non-weight bearing (Arms overhead, flexion).
Table 3.
Rotated Component Matrix Using the Principal Components Extraction Method and Varimax with Kaiser Normalization.
| Item | Factor 1 |
|---|---|
| Weight Bearing Photographs | |
| Arms at side – flexion | .607 |
| Arms at side – extension | .673 |
| Arms at side – R lateral bending | .742 |
| Arms at side – L lateral bending | .770 |
| Arms at side – R rotation | .664 |
| Arms at side – L rotation | .680 |
| Arms at shoulders – flexion | .724 |
| Arms at shoulders – extension | .730 |
| Arms at shoulders – R lateral bending | .821 |
| Arms at shoulders – L lateral bending | .844 |
| Arms at shoulders – R rotation | .668 |
| Arms at shoulders – R rotation | .684 |
| Arms overhead – flexion | .750 |
| Arms at overhead – extension | .844 |
| Arms at overhead – R lateral bending | .860 |
| Arms at overhead – L lateral bending | .862 |
| Arms at overhead – R rotation | .828 |
| Arms at overhead – R rotation | .843 |
| Non-weight Bearing Photographs | |
| Arms at side – flexion | .184 |
| Arms at side – extension | .151 |
| Arms at side – R lateral bending | .255 |
| Arms at side – L lateral bending | .294 |
| Arms at side – R rotation | .213 |
| Arms at side – L rotation | .238 |
| Arms at shoulders – flexion | .346 |
| Arms at shoulders – extension | .278 |
| Arms at shoulders – R lateral bending | .247 |
| Arms at shoulders – L lateral bending | .312 |
| Arms at shoulders – R rotation | .274 |
| Arms at shoulders – L rotation | .312 |
| Arms overhead – flexion | .461 |
| Arms at overhead – extension | .332 |
| Arms at overhead – R lateral bending | .348 |
| Arms at overhead – L lateral bending | .333 |
| Arms at overhead – R rotation | .317 |
| Arms at overhead – L rotation | .331 |
| Control Photographs | |
| Arms at side left leg flexed forward 90°, side view | .234 |
| Arms at side left leg extended forward at 90°, front view | .259 |
| Arms at side, left leg extended backward at 90°, side view | .181 |
| Arms at side legs split side-to-side 60°, front view | .094 |
| Arms at side, rising up at toes 45°, side view | .096 |
4.6. Reliability
The internal consistency (coefficient Alpha) of the 19 item scale was .978. Temporal stability (test-retest reliability) based on both Pearson’s product moment (r = .749, p < 0.001) and ICC (.856, 95% confidence interval = .74–.92) was judged to be acceptable given the length of time between administrations (mean = 22.9 days, SD = 11.59 days).
4.7. Convergent and Discriminant Validity
Convergent and discriminant validity were established by computing correlations with measures of similar and dissimilar constructs. Results are reported in Table 4. Briefly, the PFActS-C total score correlated significantly with the other measures of fear and pain anxiety (TSK, PASS, PCS), and general measures of pain severity (MPI Pain Severity). Similarly, the PFActS-C correlated significantly with other self-report instruments of neck pain-related disability (i.e., NDI). Finally, The PFActS-C correlated with measures assessing neck-related impairment using objective examiner measurement (Neck Range of Motion, Neck Strength). The PFActS-C did not correlate with measures considered on a priori grounds to be unrelated to fear(TSK Importance of Exercise, MPI Support, Demographic variables), supporting the instrument’s discriminant validity.
Table 4.
PFActS-C Correlations With Other Measures
| PFActS-C TOTAL (N) |
|
|---|---|
| TSK total | .372** (208) |
| TSK Harm | .394** (208) |
| TSK Fear of Injury | .320** (208) |
| TSK Importance of Exercise | .012 (208) |
| TSK Avoid Activity | .265** (208) |
| PASS Fearful thinking | .330** (207) |
| PASS Cog Anx | .376** (207) |
| PASS Esc/Avoid | .271** (207) |
| PASS Physiol Anx | .405** (207) |
| PASS Total | .411** (207) |
| PCS Rumination | .346** (205) |
| PCS Magnification | .343** (205) |
| PCS Helplessness | .382** (205) |
| PCS Total | .403** (205) |
| MPI Pain Sev | .504** (208) |
| MPI Support | .107 (201) |
| NDI | .562** (208) |
| Neck strength flexion | −.241** (202) |
| Neck strength extension | −.308** (207) |
| Neck strength R lateral bend | −.294 ** (207) |
| Neck strength L lateral bend | −.323** (207) |
| Neck ROM extension | −.218** (207) |
| Neck ROM extension | −.281** (207) |
| Neck ROM R lateral bend | −.184 ** (206) |
| Neck ROM L lateral bend | −.209** (207) |
| Neck ROM R rotation | −.302** (207) |
| Neck ROM L rotation | −.323** (207) |
| Age | .159* (208) |
| Marital Status | −.022 (208) |
| Household income | −.082 (200) |
| Education | .076 (206) |
TSK, Tampa Scale of Kinesiophobia; PASS, Pain Anxiety Symptom Scale; PCS, Pain Catastrophising Scale; MPI, Multidimensional Pain Inventory; ROM, Range of Motion
4.8. Criterion Validity
T-tests comparing moderate to severely SX and minimally symptomatic (MSX) participants were conducted for total PFActS-C scores and for scores on each of the 19 items. SX participants scored higher (Mean=4.29, SD = 2.38) on the total 19 item scale when compared to MSX participants (Mean=1.14, SD=1.45; t353 = 14.13, p < 0.001). They also had significantly higher mean scores on each of the 19 items.
4.9 Construct Validity
A hierarchical multiple regression was conducted to examine the PFActS-C (19 item version) as a unique predictor of neck disability after controlling for the influence of demographics (age, sex), pain (MPI Pain Severity Scale), and other measures of pain related fear and anxiety (PASS, TSK, PCS). These results are summarized in Table 5. After controlling for all predictors at each step of the regression, the PFActS-C (19 item version) explained a significant additional increment in neck related disability (R2 change = .03, p=.00).
Table 5.
Hiearchical regression analysis to predict neck disability (NDI)
| Independent Variables | R2 | R2 Change | F Change | Beta | Beta p value |
|---|---|---|---|---|---|
| Step 1 | .027 | .027 | F(2,201)=2.83, p<.061 | ||
| Age | .102 | .042 | |||
| Sex | ..069 | .173 | |||
| Step 2 | .370 | .342 | F(1,200)=108.59, p<.00 | ||
| MPI Pain Sev | .304 | .000 | |||
| Step 3 | .502 | .132 | F(3,197)=17.42, p<.00 | ||
| PASS | .292 | .000 | |||
| TSK | .113 | .056 | |||
| PCS | .002 | .980 | |||
| Step 4 | .532 | .030 | F(1,196)=12.61, p<.00 | ||
| PFactS-C (19) | .217 | .000 | |||
MPI Pain Sev, Multidimensional Pain Inventory Pain Severity Scale; PASS, Pain Anxiety Symptom Scale; TSK, Tampa Scale of Kinesiophobia; PCS, Pain Catastrophizing Scale
5. Discussion
The PFActS-C was developed as a specific measure of fear of activity for people with cervical pain. To our knowledge, no other measure of fear of specific, relevant activities is available for this population. The current study was conducted to examine and validate the psychometric properties of the PFActs-C. An initial analysis of the entire 77-item PFActS demonstrated that the instrument had face validity. A truncated, 19-item subset of the original instrument demonstrated good test-retest reliability and internal consistency. It also demonstrated good discriminant validity and convergent validity using a multimethod procedure. In sum, the PFActS has psychometric properties that justify its use in research on neck pain from whiplash injuries.
The original 77-item PFActS was developed for 2 reasons: (1) to assess fear of movement globally among patients with whiplash injuries, and (2) to provide specific information that could be used in desensitization treatment of the patients. When the PFActS is used to guide desensitization treatment, the entire instrument is needed, so that the clinician can expose patients to the specific stresses that are particularly fear-provoking for them. When the goal of assessment is to determine the overall severity of fear of movement, the 19-item reduced of the PFActS is preferable, since it poses less patient burden.
A key issue regarding a new instrument like the PFActS-C is whether there is a need for additional tools to assess fear of activity. There are several considerations that support the contention that such a need exists.
Empirical evidence regarding any conceptual model depends not only on the inherent validity of the model, but also on the appropriateness of instruments used to assess key constructs in the model. As described earlier, research on the FAM has produced somewhat mixed results [25, 26]. One possible interpretation of the empirical data is that the model is inherently limited in its utility. However, it is equally possible that the TSK and other instruments used to measure fear of movement and (re)injury are suboptimal. This possibility gains credence when one considers the fact that the TSK was developed in isolation from the FAM, and may have been selected by Vlaeyen and colleagues [34] as a matter of convenience. Thus, there is no a priori reason to believe that the TSK is an optimal instrument for assessing fear of activity.
Moreover, although the TSK has appeal because of its potential relevance to any painful condition and the ease with which it can be administered, inspection of its items raises questions about what it actually measures [1]. A key point is that the term “fear” has multiple meanings, and instruments to assess it can diverge sharply in their designs and purposes. For example, instruments can be designed to assess fear as an emotional state characterized by a sense of threat, autonomic arousal, and strong impulses to engage in behaviors that reduce the threat. But instruments can also be developed in which “fear” is construed as an enduring disposition or propensity to experience fear. For example, a man could say that he fears walking up stairs, even though he is not currently in the presence of a stairs, and is not actually experiencing fear. Such an assertion would be understood as a hypothetical statement: “If I needed to walk up a flight of stairs, I would experience fear.” Finally, instruments can be designed to assess anticipated adverse consequences that individuals perceive they might encounter if they engage in various activities. The assumption underlying these instruments is that if individuals expect adverse consequences from certain activities, they are likely to avoid the activities and experience fear when confronted by a need to engage in the activities.
Based on the considerations enumerated above, the TSK represents a rather abstract verbal instrument that could best be described as assessing individuals’ concerns about adverse consequences from certain kinds of physical activities. In contrast, since the PFActS-C requires individuals to respond to specific pictorial stimuli reflecting cervical movement, it has the potential to provoke increased emotional reactions from them. The importance of the immediacy and specificity of fear provoking stimuli has been noted by several theorists and investigators [18, 38].
As noted, there was a significant difference in mean fear for the PFActS-C for males and females. This result may have been a chance finding given the number of analyses performed. However, another possible explanation for these differences may be that a female figure was used in all photographs. Men may have responded differently due to the sex of the model. At the present time, it is prudent to use the different mean ratings on the PFActS-C for the 2 sexes for comparisons to males and female respondents in other studies that may use the PFActS-C. Future research needs to replicate the results with a male model.
A limitation of our study is that we only included people with relatively minor cervical injuries sustained in MVCs (WAD levels I and II). Future research needs to extend the sample to other neck pain groups including those with more severe injuries. Moreover, at least by some standards [31], our sample size was small relative to the number of items in the instrument that we factor analyzed, It should be noted, however, that statisticians disagree on the issue of appropriate sample size for factor analyses. Although Tinsley has suggested 5–10 subjects per item, others note that as the sample size gets larger, the relative number of respondents per item can diminish [5] and that a sample of 200 is adequate in most cases [3].
The preliminary data indicate that the PFActS-C (19 item version) has promising psychometric properties for use as an instrument to assess fear in individuals with cervical pain in the research setting. It has the advantage over other commonly used measures of fear of activity such as the TSK and Fear Avoidance and Beliefs Questionnaire [37] of providing respondents with specific, unambiguous stimuli rather than abstract verbal statements that are more open to respondent interpretation. In addition to research applications, the PFActS-C 19 item version and the full version may have a number of clinical applications. Both measures can be used as an initial screen for fear generated from very specific movements. For clinical screening purposes, the full version may offer a wider variety of movements to capture the many possible idiosyncratic fears with which patients present. Following initial screening, the items may be readministered in the context of repeated testing during exposure based treatment.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bordens K, Abbot B. Research Design and Methods: A Process Approach. 3rd ed. Mountain View, CA: Mayfield; 1996. [Google Scholar]
- 2.Burwinkle T, Robinson JP, Turk DC. Fear of movement: factor structure of the Tampa Scale of Kinesiophobia in patients with fibromyalgia syndrome. J Pain. 2005;6:384–391. doi: 10.1016/j.jpain.2005.01.355. [DOI] [PubMed] [Google Scholar]
- 3.Comrey AL. Factor analytic methods of scale development in personality and clinical psychology. J Consult Clin Psychol. 1988;56:754–761. doi: 10.1037//0022-006x.56.5.754. [DOI] [PubMed] [Google Scholar]
- 4.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 5.DeVellis RF. Scale Development Theory and Applications. Sage Publications; 1991. [Google Scholar]
- 6.Drottning M, Staff P, Levin L, et al. Acute emotional response to common whiplash predicts subsequent pain complaints. A prospective study of 107 subjects sustaining whiplash injury. Nordic J Psychiatry. 1995;49:292–299. [Google Scholar]
- 7.French DL, France CR, Vigneau F, French JA, Evans T. Fear of movement/(re)injury in chronic pain: a psychometric assessment of the original English version of the Tampa Scale for Kinesiophobia. Pain. 2007;127:42–51. doi: 10.1016/j.pain.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 8.Gargan M, Baniseter G, Main C, et al. The behavioural response to whiplash injury. J Bone Joint Surg (Br) 1997;79:523–526. doi: 10.1302/0301-620x.79b4.6940. [DOI] [PubMed] [Google Scholar]
- 9.George SZ, Bialosky JE, Donald DA. The centralization phenomenon and fear-avoidance beliefs as prognostic factors for acute low back pain: a preliminary investigation involving patients classified for specific exercise. J Orthop Sports Phys Ther. 2005;35:580–588. doi: 10.2519/jospt.2005.35.9.580. [DOI] [PubMed] [Google Scholar]
- 10.Geisser ME, Haig AJ, Theisen ME. Activity avoidance and function in persons with chronic back pain. J Occup Rehabil. 2000;10:215–227. [Google Scholar]
- 11.George SZ, Fritz JM, Erhard RE. A comparison of fear-avoidance beliefs in patients with lumbar spine pain and cervical spine pain. Spine. 2001;26:2139–2145. doi: 10.1097/00007632-200110010-00019. [DOI] [PubMed] [Google Scholar]
- 12.Gerhardt J, Cocchiarella L, Lea R. The Practical Guide to Range of Motion Assessment. Chicago: American Medical Association; 2002. [Google Scholar]
- 13.Goubert L, Crombez G, Van Damme S, Vlaeyen JWS, Bijttebier P, Roelofs J. Confirmatory factor analysis of the Tampa Scale for Kinesiophobia: invariant two-factor model across low back pain patients and fibromyalgia patients. Clin J Pain. 2004;20:103–110. doi: 10.1097/00002508-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Kaiser HF. An index of factoral simplicity. Psychometrika. 1974;39:31–36. [Google Scholar]
- 15.Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- 16.Kori S, Miller R, Todd D. Kinesiophobia: a new view of chronic pain behavior. Pain Management. 1990 Jan/Feb;:35–43. [Google Scholar]
- 17.Kugler K, Wijn J, Geilen M, deJong J, Vlaeyen JWS. The Photograph series of Daily Activities (PHODA). CD-rom version 1.0. Heerlen, The Netherlands: Institute for Rehabilitation Research and School for Physiotherapy; 1999. [Google Scholar]
- 18.Lang PJ. The emotion probe: studies of motivation and attention. Am Psychol. 1995;50:372–385. doi: 10.1037//0003-066x.50.5.372. [DOI] [PubMed] [Google Scholar]
- 19.Leeuw M, Goossens MEJB, Linton SJ, Crombez G, Boersma K, Vlaeyen JWS. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2006;30:77–94. doi: 10.1007/s10865-006-9085-0. [DOI] [PubMed] [Google Scholar]
- 20.Leeuw M, Goosens MEJB, van Bruekelen GJP, Boersma K, Vlaeyen JWS. Measuring perceived harmfulness of physical activities in patients sith chronic low back pain: the Photograph Series of Daily Activities – Short Electronic Version. J Pain. 2007;11:840–849. doi: 10.1016/j.jpain.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 21.McCracken LM, Zayfert C, Gross RT. The Pain Anxiety Symptoms Scale: development and validation of a scale to measure fear of pain. Pain. 1992;50:67–73. doi: 10.1016/0304-3959(92)90113-P. [DOI] [PubMed] [Google Scholar]
- 22.Nunnally JC, Bernstein IH. Psychometric Theory. 3rd ed. NY: McGraw Hill; 1994. [Google Scholar]
- 23.Picavet HS, Vlaeyen JWS, Schouten JS. Pain catastrophizing and kinesiophobia: predictors of chronic low back pain. Am J Epidemiol. 2002;156:1028–1034. doi: 10.1093/aje/kwf136. [DOI] [PubMed] [Google Scholar]
- 24.Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine. 2002;27:E109–E120. doi: 10.1097/00007632-200203010-00017. [DOI] [PubMed] [Google Scholar]
- 25.Pincus T, Vogel S, Burton AK, Santos R, Field AP. Fear avoidance and prognosis in back pain: a systematic review and synthesis of current evidence. Arthritis Rheum. 2006;54:3999–4010. doi: 10.1002/art.22273. [DOI] [PubMed] [Google Scholar]
- 26.Sieben JM, Vlaeyen JWS, Tuerlinck S, Portegijs PJ. Pain-related fear in acute low back pain: the first two weeks of a new episode. J Pain. 2002;6:229–237. doi: 10.1053/eujp.2002.0341. [DOI] [PubMed] [Google Scholar]
- 27.Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining "whiplash" and its management. Spine. 1995;20:1S–73S. [Publish erratum appears in Spine 1995 20(21):2372]. [PubMed] [Google Scholar]
- 28.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1993;7:524–532. [Google Scholar]
- 29.Swinkels-Meewisse EJCM, Roelofs J, Schouten EGW, Verbeek ALM, Oostendorp RAB, Vlaeyen JWS. Fear of movement/(re)injury predicting chronic disabling low back pain: a prospective inception cohort study. Spine. 2006;31:658–664. doi: 10.1097/01.brs.0000203709.65384.9d. [DOI] [PubMed] [Google Scholar]
- 30.Swinkels-Meewisse EJCM, Swinkels RAHM, Verbeek ALM, Vlaeyen JWS, Oostendorp RAB. Psychometric properties of the Tampa Scale for Kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Man Ther. 2003;8:29–36. doi: 10.1054/math.2002.0484. [DOI] [PubMed] [Google Scholar]
- 31.Tinsley HEA, Tinsley DJ. Uses of factor analysis in counseling psychology research. J Counsel Psychol. 1973;34:414–424. [Google Scholar]
- 32.Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–415. [PubMed] [Google Scholar]
- 33.Vlaeyen JWS, Crombez G. Fear of movement/(re)injury, avoidance and pain disability in chronic low back pain patients. Man Ther. 1999;4:187–195. doi: 10.1054/math.1999.0199. [DOI] [PubMed] [Google Scholar]
- 34.Vlaeyen JW, Kole-Snijders AM, Boeren RG, et al. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62:363–372. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- 35.Vlaeyen JWS, Kole-Snijders AMJ, Rotteveel AM, Ruesink R, Heuts PHTG. The role of fear of movement/(re)injury in pain disability. J Occup Rehabil. 1995;5:235–252. doi: 10.1007/BF02109988. [DOI] [PubMed] [Google Scholar]
- 36.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: state of the art. Pain. 2000;85:317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 37.Waddell G, Newton M, Henderson I, Somerville D, Main C. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:1570168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 38.Wessa M, Karl A, Flor H. Central and peripheral psychophysiological responses to trauma-related cues in subclinical posttraumatic stress disorder: a pilot study. Exp Brain Res. 2005;167:56–65. doi: 10.1007/s00221-005-0007-0. [DOI] [PubMed] [Google Scholar]