Abstract
Overswinging or CHAT (brief for Circadian Hyper-Amplitude-Tension), that is an excessive circadian variation in blood pressure (BP), has been associated with a large increase in cardiovascular disease risk, present even in the absence of an elevated BP itself. This usually asymptomatic condition is usually overlooked by current practice based on spot-checks, because to be diagnosed, measurements need to be taken around-the-clock, preferably for 7 days at the outset. Once diagnosed, however, a usual circadian BP pattern can be restored by means of certain non-pharmacologic or pharmacologic interventions timed appropriately. Thereby, it is possible to reduce the risk of cardiovascular morbidity and mortality, cerebral ischemic events and nephropathy in particular. For the preparation of guidelines regarding the diagnosis of BP disorders and for the institution of primary as well as secondary preventive measures, it is important to know what the incidence of CHAT is on a global basis. We found 191 cases of CHAT among 1602 mostly 7-day/24-h BP profiles, obtained from several centers in different countries participating in an ongoing project on the BIOsphere and the COSmos (BIOCOS). CHAT incidence is about the same between men and women, but it is diagnosed more often among patients with borderline hypertension or with glucose intolerance. It is also more common among MESOR-hypertensive than among MESOR-normotensive individuals. Priority should be given to the development of an unobtrusive and affordable device to automatically monitor BP and to analyze the data as-one-goes, so that cardiovascular disease risk can be prevented.
Keywords: BIOCOS, Blood pressure, Chat (circadian hyper-amplitude-tension), Glucose intolerance, Pre, hypertension, Worldwide incidence
1. Introduction
The need for an increase in awareness, treatment, and management of hypertension, afflicting over a quarter of the adult population [1] may take second place after efforts targeting primary prevention, our purpose herein. Hypertension is currently diagnosed mostly by means of single or a few measurements during a few consecutive examinations, a single visit in 27 of 30 studies summarized in Table 1 in [1]. This practice can be associated with over 40% false diagnoses [2], due in part to the large variability in BP, as such and in response to external factors. A diagnosis based on serial measurements taken at intervals, systematically around-the-clock for several days, obtained by manual or automatic monitoring, reduces misdiagnoses and hence morbidity and/or mortality. Home monitoring, becoming affordable is more widely used. Efforts to render automatic home monitoring within reach are underway [3,4], while the TM-2421 ambulatory monitors from A & D are available with an 80% reduction in cost with free data analyses, interpreted chronobiologically, provided worldwide through the BIOCOS project [5].
As compared to spot-checks or even 24-h profiles, week-long (or longer, once B P abnormality is diagnosed) ambulatory monitoring interpreted by the methods of chronobiology [3–5] provides a less unreliable diagnosis of “MESOR-hypertension”, an elevation of the average BP, estimated by accounting for its broad time structure or chronome. The MESOR, or Midline Estimating Statistic Of Rhythm, is a more accurate and more precise estimate of location than the arithmetic mean. We need to diagnose also abnormalities in the variability of BP (and heart rate), not assessable on the basis of single measurements, and associated with an increase in cardiovascular disease risk greater than MESOR-hypertension [3–5]. CHAT, an excessive circadian BP variation, is associated with a large increase in cardiovascular disease risk, notably cerebral ischemic events and nephropathy, observed in normotensive as well as in treated hypertensive patients [3–8], validated in a perspective of up to 28 years based on 144, 641 measurements from 2586 patients [9, 10], Table 1. Identifying patients with consistent CHAT could relieve the burden of hypertension by prompting the institution of preventive measures for people who would not be otherwise diagnosed.
Table 1.
Outcomes of chronobiological screens of blood pressure and heart rate*
| N of Patients (ref) | N at follow-up | Sampling | N measurements: Total (outcomes) | Finding |
|---|---|---|---|---|
| 10 (1) | 10 (up to 5 years) | 5/day daily | Up to 9,125 (only partially analyzed) | Among P. Scarpelli’s patients, the 4 who died with malignant hypertension had a larger circadian BP amplitude than the 6 who were still alive (SBP: t=1.84; P=0.103; DBP: t=2.99; P-0.017) |
| 63 (2, 3) | 21 after 28 years | ~q4h for 2 days | 756 (252) | 9 of 10 subjects without CHAT are alive while 7 of 11 subjects with CHAT are dead 28 years later (chi-square=6.390; PO.01) |
| 56 (4) | 56: Concomitant LVM1 | q15 min for 24 h | 5,376 (5,376) | Classification by Y. Kumagai of patients by LVMI (<100; 100–130; >130 g/m 2) Reveals elevation of circadian amplitude at LVMI in 100–130 range whereas MESOR elevation occurs only at LVMI > 130. |
| 221 (5,6) | 221 (time of delivery) | q1 h/48h in each trimester of pregnancy (336 profiles) | 16, 128 (16,128) | In addition to an 8 mm Hg difference in mean value between women who will or will not develop complications (gestational hypertension, preeclampsia) already observed during the first trimester of pregnancy, the occurrence of complications is also associated with BP profiles characterized by an elevated circadian BP amplitude. In particular, one case (JK) of CHAT where warning was not heeded, was followed 8 weeks later by severe pre-eclampsia, premature delivery and 26 months of hospitalization of offspring at a cost of about $1 million |
| 297 (7–12) | 297 after 6 years | q15 min for 48 h | 57,024 (57,024) | CHAT or a reduced circadian standard deviation of heart rate, or an excessive pulse pressure (>60 mm Hg) are large risk factors (larger than hypertension) for cerebral ischemic events, nephropathy and coronary artery disease, even when the blood pressure is within acceptable limits. |
| 2039 (13–15) | 2039 Concomitant LVMI | Hourly averages for 24 h | 48,936 (48,936) | LVMI is increased in patients with CHAT, a reduced circadian standard deviation of heart rate, or an elevated pulse pressure. The relation between LVMI and the circadian endpoints is nonlinear. |
| 23 (16) | 12 after 7 years | q15 min for 9 days | 19,872 (10,368) | 10 of 20 patients with no consistent BP abnormality are alive and well; 2 of 3 patients with consistent BP abnormality reported an adverse vascular event (P=0:015 by Fisher’s Exact Test). |
| 80 (17, 18) | 80 Response to treatment administered 2 h before daily BP peak vs. control group treated 3 times a day | q4 h for 24 h before and on treatment | 960 (960) | With smaller doses of medications, BP was lowered by R. Zaslavskaya to a larger extent and treatment was accompanied by fewer complications. Treatment: propranolol, clonidine, or alpha-methyldopa (P<0.05 for each effect) |
| 18 (19) | 18 (12 weeks) | q30 min (≥ 24h) on 3 regimens | ≥ 2592 (≥ 2592) | Treating CHAT may prevent adverse vascular events: As compared to placebo, nifedipine (1 mg b.i.d, at 08 & 20) increases and benidipine (4 mg/day at 08) decreases the circadian amplitude of blood pressure. The resulting increase vs. decrease in the incidence of CHAT on nifedipine vs. benidipine may account for the corresponding difference between the number of stroke events of 7.6 vs. 3.5 and the total number of cardiovascular events of 20.4 vs. 8.8 per 1,000 person-years. |
| Totals: | ||||
| 2,807 | 2.754 | 160.769 (>141.636) | ||
SBP and DBP: Systolic and Diastolic blood pressure; HR: heart rate; CHAT: Circadian Hyper-Amplitude-Tension, a condition defined by a circadian amplitude exceeding the upper 95% prediction limit of acceptability (in healthy peers matched by gender and age); LVMI: left ventricular mass index. By comparison with several classical studies, the number of measurements in chronobiological work completed thus far is likely to be larger, and confounding by inter-subject variability smaller (20).
2. Subjects and methods
As part of the ongoing BIOCOS project, BP records were obtained from several centers in different countries, using the TM-2421 ambulatory monitor from A&D (Tokyo, Japan). Most records covered 7 days or longer spans (except in China, where 24-h profiles were collected as a rule). The oscillometric BP and heart rate (HR) data were downloaded to a computer with the TM-2021 or TM-2023 interface, also from A&D (Tokyo, Japan).
Each record was analyzed by sphygmochron [11], a double-barreled parametric and non-parametric method comparing a person’s BP and HR characteristics with those of healthy individuals of the same gender and similar age (peers). A two-component model consisting of cosine curves with periods of 24 and 12 h approximating the circadian waveform is fitted by least squares to each data series. The MESOR, double 24-h amplitude (a measure of the extent of predictable variation within a day), and acrophase (a measure of the timing of overall high values recurring each day) are compared with 90% prediction limits derived from records of clinically healthy peers matched by gender and age. MESOR-hypertension and/or CHAT are diagnosed when the BP MESOR and/or circadian amplitude of BP are above the corresponding upper 95% prediction limit of peers. Ecphasia is diagnosed when the circadian acrophase is outside the 90% prediction limits of peers. All three conditions are associated with a large increase in cardiovascular disease risk, as are an excessive pulse pressure (MESOR difference between systolic and diastolic BP above 60 mmHg) and a decreased HR variability, gauged by a circadian standard deviation below the lower 5% prediction limit of peers. Non-parametric endpoints include the duration and the time(s) when time-specified values stacked over an idealized 24-h day exceed the upper 95% time-varying limits encountered in healthy peers, and the extent of any such excess (or deficit) (the hyperbaric or hypobaric indices, respectively). The hyperbaric index, expressed in mmHg × h, is calculated as the area delineated between excessive BP values and the upper 95% prediction limit.
3. Results
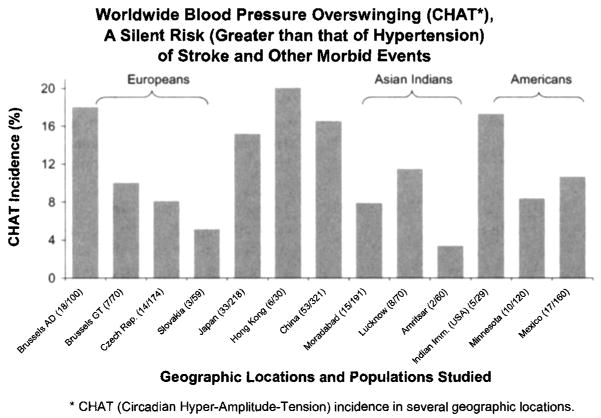
Abnormal BP variability can occur when measurements remain within the acceptable range. As a step toward world-wide statistics, Fig. 1 illustrates the incidence of CHAT in countries participating in the BIOCOS project, aimed at mapping biologic time structures and environmental ones influencing them. There were 191 cases of CHAT in 1602 profiles (many of them covering 7 days), the incidence of CHAT varying from about 2% to close to 20%, Fig. 1.
Fig. 1.
First summary of 191 cases of CHAT in 1602 profiles (many of them covering 7 days) aims at indicating that CHAT is present under various conditions in various populations in many geographic and geomagnetic locations, in the presence or absence of MESOR-hypertension. © Halberg.
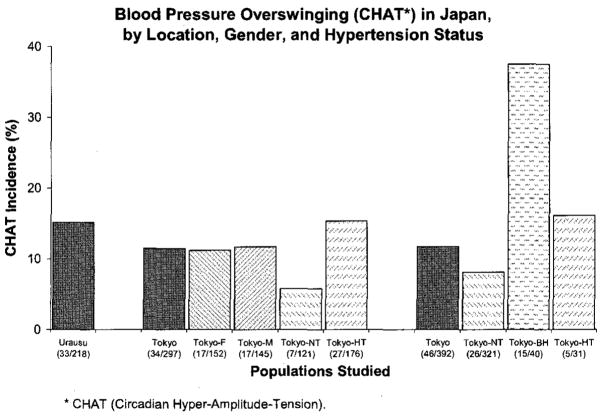
CHAT incidence was examined in more detail in three populations: a rural area of Japan (Urausu) also included in a worldwide comparison of CHAT incidence in Fig. 1, a multi-center clinical population in Tokyo, and another multi-centric subject population in Japan. As seen in Fig. 2, CHAT is diagnosed equally in women and men. It is more prevalent in borderline hypertension than in MESOR-hypertension [3–8,12], Fig. 2. It is also more frequently encountered in MESOR-hypertension than in MESOR-normotension [ 12,13], Fig. 2. CHAT incidence was also shown to be higher among patients with glucose intolerance than in health or non-insulin-dependent diabetes mellitus [14].
Fig. 2.
CHAT incidence in three populations: a rural area of Japan (Urausu) also included in a worldwide comparison of CHAT incidence in Fig. 1; a multi-center clinical population in Tokyo considered as a whole, separately for men and women, and separately for MESOR-normotensive and for treated MESOR-hypertensive patients; and another multi-centfic subject population considered as a whole and separately for patients with a MESOR of diastolic blood pressure below 80 mmHg (NT), between 80 and 90 mmHg (BH), and above 90 mmHg (HT). © Halberg.
4. Discussion and conclusion
CHAT is present under various conditions in various populations in many geographic and geomagnetic locations, in the presence or absence of MESOR-hypertension. Differences in CHAT incidence may be related in part to differences in target populations (private practices in Belgium, outpatient clinics in the Czech Republic, China, Mexico, and Moradabad, India, clinical trials in Slovakia and Hong Kong, hospital patients in Amritsar, India, health watch projects in Minnesota, Japan, Lucknow, India, and Indian immigrants in the USA). Record length and use of anti-hypertensive treatment, factors that affect the incidence of CHAT, remain to be standardized in follow-up studies.
As suggested by results in Fig. 2, CHAT may represent a pre-hypertensive state and thus a harbinger, if not a determinant of subsequent MESOR-hypertension [4,12]. CHAT may be more broadly a precursor of the metabolic syndrome since it is more frequent not only in patients with borderline hypertension [12] but also in patients with glucose intolerance than in normoglycemic controls or in patients with non-insulin-dependent diabetes mellitus [14] (not shown).
The diagnosis of CHAT can be explored by sending data, coded to protect anonymity, specified by gender, age, ethnicity and medical status (including treatment kind, dose and timing) to corne001@umn.edu, to receive chronobiological analyses free of charge, with no concern about the “complexity” of the computations involved (least squares fit of multiple cosine curves to the data and numerical integration of deviations of data stacked over idealized 24-h day from time-specified reference values from healthy peers matched by gender and age).
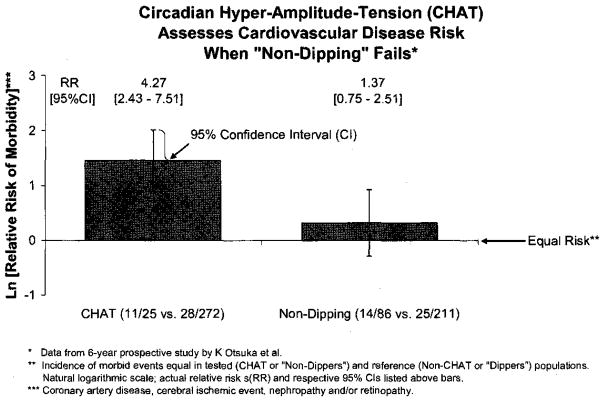
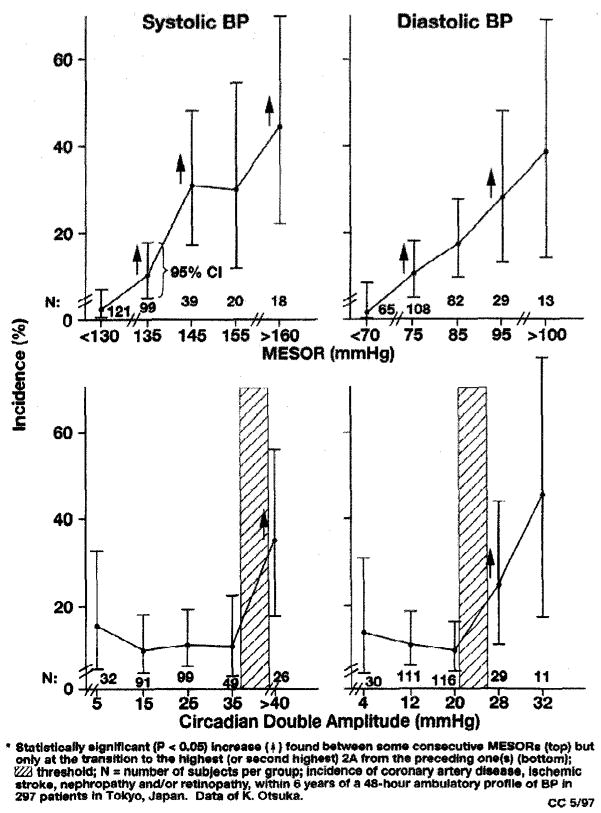
In a 6-year prospective study [6,7] (cf. [3–5,10]), CHAT was associated with an increase in cardiovascular disease risk of more than 300%, with a relative risk of 4.27 (95% confidence interval: 2.43–7.51; P < 0.001). By contrast, the relative risk of “non-dipping” [15], a diagnosis based on the more easily calculated day-night ratio, only averaged 1.37 (95% confidence interval: 0.75–2.51; not statistically significant), Fig. 3. A reason for the higher specificity of CHAT versus “non-dipping” may be that alterations in the circadian amplitude (and/or acrophase) are not confounded as they are in the computation of the day-night ratio. Another reason may relate to the use of gender- and age-specified reference values to detect abnormality in BP dynamics, rather than using the same norms for all adults above 18 years [16]. This is an important consideration when the relation between BP variability and cardiovascular disease risk is non-linear [17]. By contrast to the linear increase in risk with an increasing BP MESOR, risk increases statistically significantly only after the circadian BP amplitude exceeds a threshold [3–5,17], Fig. 4.
Fig. 3.
Patients with diastolic CHAT are 4.27 times more likely to experience a morbid event during 6 years following the initial around-the-clock BP monitoring than patients with an acceptable circadian variation in diastolic BP. This increase in risk is statistically significant, as evidenced by the 95% confidence interval of RR not overlapping 1 (or the 95% CI of the natural log of RR - Ln(RR) not overlapping 0), representing equal risk between tested and reference populations. By comparison, “non-dippers” are only 1.37 times more likely to have a morbid event as compared to “dippers”, and this increase in risk is not statistically significant. None of the patients had any morbidity prior to monitoring. Original data of K Otsuka et al. © Halberg.
Fig. 4.
The circadian double amplitude (2A) of BP must exceed a threshold (hatched; bottom) before cardiovascular disease risk increases. The circadian BP amplitude relates non-linearly to vascular disease incidence. By contrast, the BP MESOR relates linearly to the incidence of morbid events (top). Original data of K Otsuka et al. © Halberg.
The determination of CHAT incidence on a global basis, like that of MESOR-hypertension, is useful for the preparation of guidelines regarding the diagnosis of BP disorders and for the institution of primary and secondary preventive measures. This is particularly true since CHAT can be treated. In the absence of MESOR-hypertension, non-pharmacologic treatment with relaxation techniques such as autogenic training may be indicated [ 18,19]. In the presence of MESOR-hypertension, pharmacologic treatment may be optimized by timing anti-hypertensive drugs in relation to the chronodiagnosis (chronotheranostics), that is with a consideration of the variability in BP and HR. Some, but not all anti-hypertensive drugs lower an excessive circadian BP variation [19,20]. Scheduling the same dose of the same anti-hypertensive medication at different circadian stages may affect the circadian amplitude of BP differently, as assessed by parameter tests and a self-starting cumulative sum (CUSUM) control chart [3,11].
There is evidence that by treating CHAT, adverse vascular events may be prevented [21]. As compared to placebo, nifedipine (1 mg b.i.d, at 08 and 20) increased and benidipine (4 mg/day at 08) decreased the circadian amplitude of BP. The resulting increase vs. decrease in the incidence of CHAT on nifedipine vs. be nidipine treatment may account for the corresponding difference between the number of stroke events of 7.6 vs. 3.5 and the total number of cardiovascular events of 20.4 vs. 8.8 per 1000 person - years [21].
Priority should be given to the development of an unobtrusive and affordable device to automatically monitor B P and to analyze the data as-one-goes, so that cardiovascular disease risk can be prevented.
Acknowledgments
G M-13981 (F.H.), Dr. h.c. mult. Earl Bakken Fund (G.C., F.H.) and University of Minnesota Super computing Institute (G.C., F.H.).
References
- 1.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton P, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:247–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.Management Committee, Australian National Blood Pressure Study. The Australian Therapeutic Trial in Mild Hypertension. Lancet. 1980 June 14;i(8181):1261–7. [Google Scholar]
- 3.Cornélissen G, Halberg F, Bakken EE, Singh RB, Otsuka K, Tomlinson B, et al. 100 or 30 years after Janeway or Bartter, Healthwatch helps avoid “flying blind”. Biomed Pharmacother. 2004;58(Suppl 1):$69–86. doi: 10.1016/s0753-3322(04)80012-x. [DOI] [PubMed] [Google Scholar]
- 4.Halberg F, Cornélissen G, Wall D, Otsuka K, Halberg J, Katinas G, et al. Engineering and governmental challenge: 7-day/24-h chronobiologic blood pressure and heart rate screening. Biomed Instrum Techno 12002. 36183:89–122. 97. doi: 10.2345/0899-8205(2002)36[89:EAGCHC]2.0.CO;2. Part 1. Part II. [DOI] [PubMed] [Google Scholar]
- 5.Cornélissen G, Schwartzkopff O, Halberg F, Otsuka K, Watanabe Y. 7-day ambulatory monitoring for adults with hypertension and diabetes. Am J Kidney Dis. 2001;37:878. doi: 10.1016/s0272-6386(01)80145-1. [DOI] [PubMed] [Google Scholar]
- 6.Otsuka K, Cornélissen G, Halberg F. Predictive value of blood pressure dipping and swinging with regard to vascular disease risk. Clin Drug Invest. 1996;11:20–31. [Google Scholar]
- 7.Otsuka K, Cornélissen G, Halberg F, Oehlert G. Excessive circadian amplitude of blood pressure increases risk of ischemic stroke and nephropathy. J Med Eng Technol. 1997;21:23–30. doi: 10.3109/03091909709030299. [DOI] [PubMed] [Google Scholar]
- 8.Schaffer E, Cornélissen G, Rhodus N, Halhuber M, Watanabe Y, Halberg F. Outcomes of chronobiologically normotensive dental patients: a 7-year follow-up. JADA. 2001;132:891–9. doi: 10.14219/jada.archive.2001.0301. [DOI] [PubMed] [Google Scholar]
- 9.Miiller-Bohn T, Cornélissen G, Halhuber M, Schwartzkopff O, Halberg F. CHAT und Schlagfall. Deutsche Apotheker Zeitung. 2002;142:366–70. [Google Scholar]
- 10.Cornélissen G, Otsuka K, Chen CH-H, Singh RB, Halberg F. Circadian hyper-amplitude-tension (CHAT) and an elevated pulse pressure are separate cardiovascular disease risk factors. (in press) [Google Scholar]
- 11.Cornélissen G, Halberg F. Chronomedicine. In: Armitage P, Colton T, editors. Encyclopedia of biostatistics. Vol. 2. Chichester, UK: John Wiley & Sons Ltd.; 2005. pp. 796–812. [Google Scholar]
- 12.Watanabe Y, Cornélissen G, Halberg F, Bingham C, Siegelova J, Otsuka K, et al. Incidence pattern and treatment of a clinical entity, overswinging or circadian hyper-amplitude-tension (CHAT) Scr Med. 1997;70:245–61. [Google Scholar]
- 13.Cornélissen G, Scarpelli PT, Halberg F, Halberg J, Halberg Fr, Halberg E. Cardiovascular rhythms: their implications and applications in medical research and practice. In: Hekkens WThJM, Kerkhof GA, Rietveld WJ., editors. Trends in Chronobiology. Pergamon Press; Oxford: 1988. pp. 335–55. [Google Scholar]
- 14.Sanchez de la Pefia S, Gonzalez C, Cornélissen G, Halberg F. Blood pressure (BP), heart rate (HR) and non-insulin-dependent diabetes mellitus (NIDDM) chronobiology. Int J Cardiol. 2004;97(Suppl 2):S14. [Google Scholar]
- 15.Verdecchia P, Schillaci G, Guerrieri M, Gatteschi C, Benernio G, Boldrini F, et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation. 1990;81:528–36. doi: 10.1161/01.cir.81.2.528. [DOI] [PubMed] [Google Scholar]
- 16.Hagen P, editor. Mayo clinic guide to self-care: answers for everyday health problems. Rochester, MN/Jacksonville, FL/Scottsdale, AZ: Mayo Clinic; 2003. pp. 180–1. [Google Scholar]
- 17.Cornélissen G, Otsuka K, Chen C-H, Kumagai Y, Watanabe Y, Halberg F, et al. Nonlinear relation of the circadian blood pressure amplitude to cardiovascular disease risk. Scr Med. 2000;73:85–94. [Google Scholar]
- 18.Watanabe Y, Cornélissen G, Halberg F, Yoshiaki S, Fukuda K, Otsuka K, et al. Chronobiometric assessment of autogenic training effects upon blood pressure and heart rate. Percept Motor Skills. 1996;83:1395–410. doi: 10.2466/pms.1996.83.3f.1395. [DOI] [PubMed] [Google Scholar]
- 19.Watanabe Y, Cornélissen G, Watanabe M, Watanabe F, Otsuka K, Ohkawa S, et al. Effects of autogenic training and anti-hypertensive agents on circadian and circaseptan variation of blood pressure. Clin Exp Hypertens. 2003;25:405–12. doi: 10.1081/ceh-120024984. [DOI] [PubMed] [Google Scholar]
- 20.Tamura K, Kohno I, Saito Y, Wakasugi K, Achiwa S, Imanishi Y, et al. Anti-hypertensive individualized therapeutic strategy. Difesa Sociale. 1991;6:109–24. [Google Scholar]
- 21.Shinagawa M, Kubo Y, Otsuka K, Ohkawa S, Cornélissen G, Halberg F. Impact of circadian amplitude and chronotherapy: relevance to prevention and treatment of stroke. Biomed Pharmacother. 2001;55(Suppl 1):125–32. doi: 10.1016/s0753-3322(01)90017-4. [DOI] [PubMed] [Google Scholar]