Abstract
Objectives
To explore the association between implicit rationing of nursing care and selected patient outcomes in Swiss hospitals, adjusting for major organizational variables, including the quality of the nurse practice environment and the level of nurse staffing. Rationing was measured using the newly developed Basel Extent of Rationing of Nursing Care (BERNCA) instrument. Additional data were collected using an adapted version of the International Hospital Outcomes Study questionnaire.
Design
Multi-hospital cross-sectional surveys of patients and nurses.
Setting
Eight Swiss acute care hospitals
Participants
Nurses (1338) and patients (779) on 118 medical, surgical and gynecological units.
Main outcome measures
Patient satisfaction, nurse-reported medication errors, patient falls, nosocomial infections, pressure ulcers and critical incidents involving patients over the previous year.
Results
Generally, nurses reported rarely having omitted any of the 20 nursing tasks listed in the BERNCA over their last 7 working days. However, despite relatively low levels, implicit rationing of nursing care was a significant predictor of all six patient outcomes studied. Although the adequacy of nursing resources was a significant predictor for most of the patient outcomes in unadjusted models, it was not an independent predictor in the adjusted models. Low nursing resource adequacy ratings were a significant predictor for five of the six patient outcomes in the unadjusted models, but not in the adjusted ones.
Conclusion
As a system factor in acute general hospitals, implicit rationing of nursing care is an important new predictor of patient outcomes and merits further study.
Keywords: healthcare rationing, organizational factors, patient outcomes, quality of hospital care
Introduction
Over the past decade, economic and demographic forces influencing both the supply of and demand for nurses have led to shortfalls in the number of nurses, particularly in hospitals. Concurrently, cost-cutting strategies to stem exploding health care costs have raised the thresholds for hospital admissions and shortened lengths of stay. This has increased the average acuity of hospital in-patients, along with the intensity of nursing services they require; however, budgetary concerns have typically limited nursing staff numbers [1–3].
Nursing practice involves a wide range of daily tasks. When resources are limited, nurses are forced to ration their attention across their patients, using their clinical judgment to prioritize assessments and interventions [4–6]. On understaffed units, nurses are presumably forced to minimize or omit certain tasks, thereby increasing the risk of negative patient outcomes.
Worldwide, stakeholder groups consistently agree that many hospitals operate with suboptimal nursing staff levels [3, 7, 8], while a growing evidence base connects nurse understaffing with negative patient outcomes. Internationally, studies have shown significant relationships between reduced nurse practice environment quality, nurse staffing levels/skill mixes, and increased numbers of adverse events or outcomes (medication errors, falls, nosocomial infections, pressure scores, ‘failure-to-rescue’ events, and mortality rates) [9–14]. Furthermore, negative nurse practice environment features show significant associations with job dissatisfaction, burnout, work-related injuries and staff turnover [10, 15–18].
In fact, rationing of nursing care, defined as ‘the withholding or failure to carry out necessary nursing tasks due to inadequate time, staffing level, and/or skill mix,' may be a directly observable consequence of low staffing levels and poor practice environments. To our knowledge, the association between this type of implicit rationing of care and patient outcomes in hospitals has never been directly investigated.
In 2003–04, in an extension of the International Hospital Outcomes Study (IHOS) led by the Center for Health Outcomes and Policy Research at the University of Pennsylvania (USA), the Rationing of Nursing Care in Switzerland study (RICH Nursing study) measured levels of implicit rationing of nursing care in Swiss acute care hospitals to explore its association with selected patient outcomes. The International Hospital Outcomes Study is an international study of the organization of nursing care in hospitals and its impact on patient outcomes [6, 15, 19]. The Swiss study extended the research protocol of the international study by developing a new empirical measure of implicit rationing of nursing care. Specifically, it involved surveys of patients and nurses and analyses adjusting for major organizational variables shown in prior research to correlate with outcomes, including the quality of the nurse work environment and staffing/workload. The study's guiding hypothesis was that higher levels of implicit rationing of nursing care would be associated both with lower patient satisfaction and more frequent nurse-reported adverse patient outcome rates (medication errors, falls, nosocomial infections, critical incidents and pressure sores).
Conceptual framework
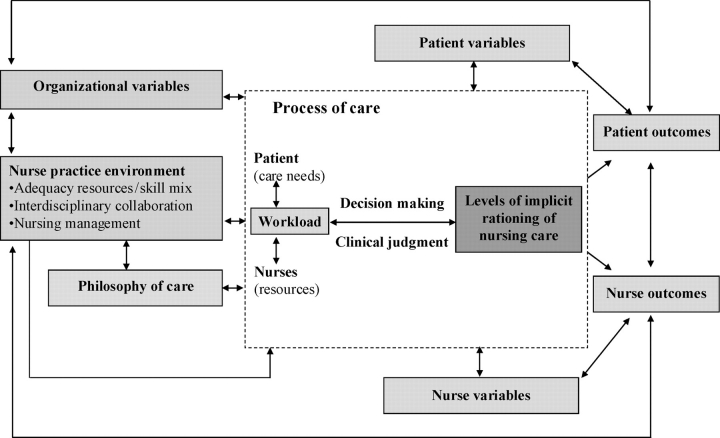
The Rationing of Nursing Care in Switzerland study elaborates on the conceptual framework of the International Hospital Outcomes Study, as well as on empirical findings regarding decision-making and prioritization of nursing care. Figure 1 shows that implicit rationing of nursing care occurs when nurses lack sufficient time to provide all the care they perceive is needed by their patients. Nurses' decisions to ration care may be influenced by hospital organizational attributes and the nurse practice environment. With our rationing measurement instrument, the Basel Extent of Rationing of Nursing Care (BERNCA), we found that reports of rationing were significantly associated with staffing and work environment conditions, thus supporting this contention [20].
Figure 1.
Conceptual framework for the RICH nursing study (this conceptual framework builds on the IHOS study and other evidence [20]).
Methods
This study used cross-sectional survey data from multiple sites and a modified version of the nurse questionnaire developed for the International Hospital Outcomes study [6, 10, 15]. The research ethics review committees of the eight participating hospitals approved the study.
Sample
Nurses and patients from a convenience sample of eight acute care hospitals in the German and French speaking regions of Switzerland were surveyed over an 11-month period in 2003 and 2004. Hospitals were selected if they had at least 100 beds, operated surgical, medical, and/or gynecological units, and if their administrators agreed to allow their facilities to participate. All nurses who held Swiss nursing or equivalent foreign credentials, who had worked in direct patient care at their hospitals for at least 3 months, including at least 1 month on their current unit, were approached. Patients hospitalized for at least 2 days on an eligible unit were approached if they could understand and read German or French, and if their physical and mental conditions were judged adequate for participation. Since the sample included nurses and patients speaking German and French, the original English questionnaires were translated into both languages using a modified Brislin protocol [21].
Variables and measures
Hospital characteristics
Hospital size (number of beds), ownership status (public vs. private), and location data were provided by the hospital administrations and the Swiss Federal Office of Statistics for 2002.
Nurse survey measures, analyzed at the unit level
Implicit rationing of nursing care was measured using the BERNCA instrument developed and validated within the Rationing of Nursing Care in Switzerland study. With 20 items, BERNCA asks nurses how frequently they were unable to perform basic nursing tasks in the past 7 working days due to inadequate time, staffing levels and/or skill mixes. Respondents rated each item on a 4-point Likert-type scale [never (0), rarely (1), sometimes (2) or often (3)] (Appendix 1, BERNCA instrument). Initial validity (content and construct validity) and reliability of the BERNCA were established using survey data from German speaking Swiss hospital nurses [20]. An explanatory factor analysis confirmed the internal structure and the hypothesized uni-dimensionality of the scale (construct validity). The Cronbach's alpha was 0.93 [20]. To calculate the average level of implicit rationing of nursing care on the unit, the scores for each nurse were averaged over all 20 items (summary score ranged from 0 to 60; means ranged from 0 to 3.0).
The quality of the nurse practice environment was measured with the Nurse Work Environment Index-Revised, a 51-item instrument [15, 22, 23]. Using 4-point Likert-type scales (from strongly disagree to strongly agree), nurses were asked whether specific elements were present in their workplace. A Principal Component Analysis with Varimax rotation of the Swiss data revealed that 17 items had communalities below 0.30; these items were deleted from further analysis. Subsequent rotation resulted in a three-factor solution: (i) nursing leadership and professional development (Leadership), (ii) nursing resources and autonomy (Resources) and (iii) interdisciplinary collaboration and competence (Collaboration) (Appendix 2). Cronbach's alphas for the subscales were 0.90, 0.84, and 0.73, respectively.
Patient-to-nurse staffing ratio, the number of patients assigned to a nurse on the last shift, the quality of care on unit, patients self-care ability and nurse job satisfaction were measured using items from the international study instrument battery (Table 1) [10].
Table 1.
Definitions and measures of the dependent, independent, and control variables
| Variables | Definition |
|---|---|
| Dependent variables | |
| Patient satisfactiona | Patients who are very satisfied with the care they received. |
| Medication administration errorsb | Medications administered at the wrong time, in the wrong dose and/or to wrong patient with or without consequences |
| Patient fallsb | Any patient fall with or without consequences |
| Nosocomial infectionsb | Hospital-acquired infections, e.g. urinary tract, respiratory tract, or wound infections experienced by patients |
| Critical incidentsb | Unexpected critical patient incidents, which might have been prevented through appropriate measures |
| Pressure ulcersb | Pressure ulcers at Stages 2 through 4 |
| Independent and control variables | |
| Rationing of nursing care | Average rationing score on unit |
| Quality of the nurse work environment [NWI-R (nursing work index – revised)] | Average score of each of two individual NWI-R subscales on unit |
| Resources | |
| Collaboration | |
| Patient-to-nurse ratio | Average number of patients cared for by nurses in the unit on their last shift |
| Age | Nurse age in categories of 10 years (nurse reported patient outcomes models) |
| Of the nurse | |
| Of the patient | Patient age in categories of 14–40, 41–50, 51–60, 61–70, >70 (patient satisfaction model) |
| Nurse education | Basic vs. specialized: e.g. intensive care, higher education in nursing level 1, clinical teacher) and/or graduate/postgraduate education: e.g. higher education in nursing level 2, higher education or university degree in nursing management, pedagogic, science, and public health (nurse reported patient outcomes models) |
| Percentage on nurses on the unit with specialization or graduate/postgraduate education (patient satisfaction model) | |
| Nurse experience | Years worked as a nurse (nurse reported patient outcomes models) Average years nurses on unit worked as a nurse (patient satisfaction model) |
| Hospital size | Number of beds in hospital |
| Department | Medical vs. surgical department |
| Patient health | Percent of patients on unit who considered themselves to be in good health compared with others of their age |
| Quality of care | Percentage of nurses on the unit who consider the quality of the nursing care on their unit to be good (patient satisfaction model) |
| Patient self-care ability | Percentage of nurses on the unit who are confident that their patients will be able to take care of themselves once they have left the hospital (patient satisfaction model) |
| Nurse job satisfaction | Percentage of nurses on the unit satisfied with their present job (patient satisfaction model) |
aPatient reported patient outcomes, bNurse reported patient outcomes.
Nurse survey measures, analyzed at the nurse level
The frequencies of adverse patient events, widely considered sensitive indicators of quality of nursing care, were assessed through nurses' reports regarding their patients over the past year on 4-point Likert-type scales ranging from never (1) to often (4). Building on questions developed for the international study, the following outcomes were assessed: (i) medication administration errors, (ii) patient falls, (iii) nosocomial infections, (iv) critical incidents and (v) pressure ulcers (Table 1). Based on the skewing of the data distribution, for the analyses reported here nurses' responses were dichotomized as ‘sometime’ and ‘often’ vs. ‘never’ and ‘rarely’ (i.e. infrequently vs. regularly).
Nurse characteristics, including age, sex, nationality, clinical specialty, employment status, education and experience were measured using questionnaire items from the international study [10].
Patient survey measures
Overall patient satisfaction with the care they received in their respective hospitals was assessed with one question using a 4-point Likert-type scale (from very satisfied to very dissatisfied). Patient demographics including age, sex and self-reported health status were measured. Patients were asked regarding the latter of these to assess their health status compared with others of their age on a 5-point Likert-type scale (from very poor to very good).
Data collection
Questionnaires were distributed on a defined day to all nurses and patients who met the inclusion criteria. For 4 weeks, completed questionnaires were collected in a closed box placed in a central location on each of the participating wards. An identification number allowed questionnaires to be linked with a specific hospital and unit, but not with specific respondents.
Data analysis
Descriptive statistics were used to analyze major variables at the nurse, patient, unit and hospital levels using techniques appropriate for their levels of measurement and data distributions. For analytical purposes, reflecting our understanding of rationing of nursing care, quality of the nurse practice environment and patient-to-nurse staffing ratios as nursing unit organizational properties, unit level mean scores were calculated for these variables.
Given the natural clustering of the data (patients and nurses within hospital units), the effects of implicit rationing of nursing care and organizational characteristics on the selected patient outcomes were assessed using multilevel multivariate regression analysis, with the unit included as a random effect. Six models were constructed – one for each dependent variable. Of these, five involved nurse reported data: medication errors, falls, nosocomial infections, critical incidents and pressure ulcers. The sixth was patient reported satisfaction with care. The main explanatory variables were rationing of nursing care, patient-to-nurse ratios, and two nurse practice environment dimensions: Resources and Collaboration. The nurse practice dimension of Leadership was excluded from the modeling due to its high correlation with the Resources dimension (r = 0.80). Patient and nurse characteristics and quality of care were included as control variables (Table 1). The level of significance was set at P < 0.05. All analyses were performed using Stata 9.2 (StataCorp LP, College Station, TX, USA) and SPSS 14 (SPSS for Windows, Rel. 14. 2005. Chicago: SPSS Inc.).
Results
Three of the eight hospitals studied were university-affiliated, three were cantonal and two were regional or local community hospitals. Seven were public, one was private-public and six had more than 300 beds. The majority of the included units were surgical (n = 60), followed by medical (n = 51) and gynecological (n = 7). Characteristics of nurses and patients are presented in Table 2. Of the 2052 nurses and 1190 patients approached, 1338 nurses and 779 patients participated, yielding a 65% response rate for both samples.
Table 2.
Nurse and patient characteristics
| Variables | |
|---|---|
| Nurse characteristics | |
| N | 1338 |
| Sex: female – n (%) | 1159 (90) |
| Nationality: non-Swiss – n (%) | 392 (31) |
| Age – n (%) | |
| 20–30 years | 544 (42) |
| 31–40 years | 398 (31) |
| 41–50 years | 249 (19) |
| > 50 years | 99 (8) |
| Employment – n (%) | |
| Full time (= 80–100%) | 937 (72) |
| Part-time (= 10–70%) | 365 (28) |
| Education – n (%) | |
| Specialized | 423 (32) |
| Graduate/postgraduate | 18 (1) |
| Years working – mean (SD) | |
| As a nurse | 10.3 (8.9) |
| In this hospital | 7.4 (7.4) |
| On this unit | 5.3 (6.0) |
| Patient characteristics | |
| N | 779 |
| Sex: females – n (%) | 403 (55) |
| Age in years – n (%) | |
| 14–20 years | 13 (2) |
| 21–40 years | 108 (14) |
| 41–60 years | 220 (30) |
| 61–70 years | 159 (21) |
| 71–80 years | 171 (23) |
| > 80 years | 75 (10) |
| State of health – n (%) | |
| Very poor | 19 (3) |
| Poor | 155 (21) |
| Fair | 216 (30) |
| Good | 252 (35) |
| Very good | 83 (11) |
The mean level of implicit rationing of nursing care across nursing units was 0.82 [standard deviation (SD) 0.26] indicating that, at the unit level, when asked how often she or he was unable to perform specific tasks, the average nurse on the units reported this occurred slightly less frequently than ‘rarely’ (0.80). Significant variability in the measured levels of implicit rationing of nursing care was found between hospitals (0.63–1.15, P < 0.001), departments [0.53 (gynecological) to 0.84 (medical) P < 0.001] and units (0.12–1.46, P < 0.001). Because of the limited range of the rationing scale and a SD of 0.54 points at the individual level, half-point measurement increments were used for modeling in the next phase of the analyses. Averaged data indicated neither strong agreement nor disagreement across units regarding nurse practice environment characteristics (Table 3). The average patient-to-nurse staffing ratio was eight patients per nurse (mean across nurses working on all the three shifts: morning, afternoon, and night). A moderate to strong correlation was found between implicit rationing and the three nurse practice environment dimensions. Patient-to-nurse staffing ratios were only weakly negatively correlated with implicit rationing (Table 3).
Table 3.
Descriptive statistics and correlations of the organizational variables
| Variables | Descriptive statistics (individual level measures, N = 1338 nurses) | Correlation matrix (unit level measures, N = 118 units) | |||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (minimum–maximum) | Rationing | NWI-R (nursing work index – revised) subscales | Patient-to-nurse ratio | |||
| Leadership | Resources | Collaboration | |||||
| Rationing (BERNCA)a | 0.82 (0.54) | 0.77 (0–2.68) | 1.00 | ||||
| NWI-R subscalesb | |||||||
| Leadership | 3.07 (0.50) | 3.13 (1.31–4.00) | −0.55 (*) | 1.00 | |||
| Resources | 2.51 (0.53) | 2.50 (1.00–4.00) | −0.67 (*) | 0.80 (*) | 1.00 | ||
| Collaboration | 3.14 (0.42) | 3.13 (1.75–4.00) | −0.44 (*) | 0.54 (*) | 0.54 (*) | 1.00 | |
| Patient-to-nurse ratio | 8.19 (5.57) | 7.00 (0–36) | 0.21 (*) | −0.32 (*) | −0.45 (*) | −0.23 (*) | 1.00 |
aRange from 0 = never to 3 = often, bRange from 1 = strongly disagree to 4 = strongly agree.
*P-value < 0.001.
Of the 779 patients, 566 (72%) were very satisfied with the care they received. The percentage of nurses who reported that adverse events had occurred sometimes or frequently during the previous year ranged from 16 (critical incidents) to 58% (nosocomial infections) (Table 4). A clear majority of nurses reported that all of the events under study had occurred with some frequency (i.e. rarely, sometimes or often). However, the regression results illustrated below lead to identical patterns of conclusions whether the dependent variables were constructed by contrasting responses of ‘rarely’, ‘sometimes’ or ‘often’ against ‘never’ (i.e. ever vs. never) or by contrasting ‘never’ and ‘rarely’ with ‘sometimes’ and ‘often’ (i.e. infrequently vs. regularly).
Table 4.
Nurse reported patient outcomes
| Nurses reported patient outcomes in the last year | Sometimes, often observed | Observed even once |
|---|---|---|
| Variables | ||
| N | 1338 | 1338 |
| Medication errors – n (%) | 380 (30) | 1089 (85) |
| Falls – n (%) | 558 (44) | 1127 (89) |
| Nosocomial infection – n (%) | 728 (58) | 1161 (93) |
| Critical incidents – n (%) | 203 (16) | 838 (67) |
| Pressure ulcers – n (%) | 313 (24) | 1053 (82) |
Impact of rationing of nursing care and organizational factors on patient outcomes
Implicit rationing of nursing care was a significant predictor for all six of the patient outcomes studied. Of the major organizational variables considered, the patient-to-nurse staffing ratio was not significantly related with any of the six investigated nurse-reported patient outcomes. The two measures of the nurse practice environment and the various control variables were not consistently related to any of the outcomes.
As hypothesized, implicit rationing of nursing care was consistently related to patient outcomes, both alone and after controlling for staffing and work environment measures. Higher levels of rationing were significantly related with a higher frequency of nurse-reported adverse patient outcomes. Specifically, in the full models, a .5-unit increase in rationing scores was associated with 10% to nearly tripled increases in the odds of reports that various adverse patient events occurred regularly over the past year. It was also associated in the fully adjusted model with a 37% decrease in the odds of patients reporting satisfaction with the care they received; however, this association was only marginally significant (at P = 0.08) (Table 5).
Table 5.
Variables influencing the six studied patient outcomes
| Variables | Unadjusted models | Adjusted models | ||
|---|---|---|---|---|
| Odds ratio (CI) | P-value | Odds ratio (CI) | P-value | |
| Patient reported patient outcome (N = 779) | ||||
| Patient satisfaction (patient very satisfied vs. satisfied, dissatisfied, very dissatisfied) | ||||
| Rationing (0.5 point increase in unit-level scores) | 0.57 (0.39, 0.84) | 0.004 | 0.63 (0.38, 1.05) | 0.08 |
| Patient-to-nurse ratio (1-patient-per-nurse increase unit-level score) | 0.98 (0.90, 1.06) | 0.64 | 0.97 (0.89, 1.06) | 0.50 |
| NWI-R (nursing work index – revised) subscales (1-point increase in unit-level scores) | ||||
| Resources | 1.83 (1.01, 3.32) | 0.045 | 0.78 (0.24, 2.57) | 0.68 |
| Collaboration | 1.91 (0.70, 5.23) | 0.21 | 1.51 (0.37, 6.24) | 0.57 |
| Nurse reported patient outcomes (N = 1338) | ||||
| Medication errors (sometimes, often observed vs. others) | ||||
| Rationing (0.5-point increase in unit-level scores) | 1.97 (1.51, 2.56) | <0.001 | 1.68 (1.17, 2.41) | 0.005 |
| Patient-to-nurse ratio (1-patient-per-nurse increase in unit-level score) | 1.03 (0.97, 1.09) | 0.37 | 1.00 (0.93, 1.07) | 0.99 |
| NWI-R subscales (1-point increase in unit-level scores) | ||||
| Resources | 0.48 (0.33, 0.71) | <0.001 | 0.71 (0.39, 1.31) | 0.28 |
| Collaboration | 0.57 (0.28, 1.17) | 0.12 | 1.37 (0.58, 3.24) | 0.47 |
| Patient falls (sometimes, often observed vs. others) | ||||
| Rationing (0.5-point increase in unit-level scores) | 2.79 (1.85, 4.21) | <0.001 | 2.81 (1.65, 4.78) | <0.001 |
| Patient-to-nurse ratio (1-patient-per-nurse increase in unit-level) | 1.00 (0.98, 1.17) | 0.15 | 1.01 (0.92, 1.11) | 0.87 |
| NWI-R subscales (1-point increase in unit-level scores) | ||||
| Resources | 0.87 (0.45, 1.70) | 0.70 | 1.00 (0.41, 2.43) | 0.99 |
| Collaboration | 0.57 (0.19, 1.73) | 0.32 | 1.63 (0.46, 5.58) | 0.45 |
| Nosocomial infections (sometimes, often observed vs. others) | ||||
| Rationing (0.5-point increase in unit-level scores) | 2.05 (1.44, 2.92) | <0.001 | 1.61 (1.03, 2.51) | 0.04 |
| Patient-to-nurse ratio (0.5-point increase in unit-level scores) | 1.03 (0.95, 1.12) | 0.42 | 1.00 (0.92, 1.08) | 0.93 |
| NWI-R subscale (1-point increase in unit-level scores) | ||||
| Resources | 0.38 (0.23, 0.64) | <0.001 | 0.48 (0.22, 1.03) | 0.06 |
| Collaboration | 0.45 (0.17, 1.19) | 0.11 | 1.48 (0.50, 4.35) | 0.48 |
| Critical incidents (sometimes, often observed vs. others) | ||||
| Rationing (0.5-point increase in unit-level scores) | 2.65 (1.79, 3.92) | <0.001 | 1.10 (1.04, 1.17) | 0.002 |
| Patient-to-nurse ratio (1-patient-per-nurse increase in unit-level ratio) | 1.01 (0.92, 1.10) | 0.88 | 0.99 (0.98, 1.00) | 0.15 |
| NWI-R subscales (1-point increase in unit-level scores) | ||||
| Resources | 0.34 (0.19, 0.61) | <0.001 | 0.96 (0.89, 1.07) | 0.45 |
| Collaboration | 0.18 (0.06, 0.48) | 0.001 | 0.93 (0.80, 1.07) | 0.31 |
| Pressure ulcers (sometimes, often observed vs. others) | ||||
| Rationing (0.5-point increase in unit-level scores) | 2.81 (1.88, 4.20) | <0.001 | 1.15 (1.06, 1.25) | 0.001 |
| Patient-to-nurse ratio (1-patient-per-nurse increase in unit-level ratio) | 1.08 (0.99, 1.18) | 0.09 | 1.00 (0.99, 1.02) | 0.86 |
| NWI-R subscales (1-point increase in unit-level scores) | ||||
| Resources | 0.30 (0.17, 0.55) | <0.001 | 0.96 (0.83, 1.10) | 0.55 |
| Collaboration | 0.35 (0.12, 1.02) | 0.05 | 1.01 (0.83, 1.24) | 0.91 |
Notes: CI = 95% confidence interval.
Before controlling for other major variables, the Resource dimension of the nurse practice environment was a significant predictor of five of the six patient outcomes investigated (i.e. higher scores were associated with higher patient satisfaction and lower likelihood of nurses reporting that negative events had occurred regularly). However, after controlling for rationing and patient-to-nurse ratios in the adjusted models, the Resource dimension was no longer significantly related to these outcomes. The one exception was a marginally significant association with nosocomial infections. The nurse practice environment dimension Collaboration was associated with critical incidents in the unadjusted models, but the relationship was not sustained after controlling for the other organizational factors.
Discussion
To our knowledge, this is the first study to measure implicit rationing of nursing care and to explore associations between this factor and the selected patient outcomes. The related analyses provided estimates of the effect of implicit rationing of nursing care after controlling for patient, nurse, and hospital-related covariates, as well as for the clustering of observations within hospital units. Variations in nurse reports of rationing at the unit level were the only factor significantly related with all six patient outcomes studied. While the frequency of rationing appeared relatively low overall, increases in the unit-level scores were associated with large decreases in patients' likelihood of being satisfied with care, and substantial increases in the odds of nurses reporting that selected adverse patient outcomes had occurred with regularity over the preceding year.
While prior research suggests that lower nurse staffing ratios are related to worse patient outcomes [11–14, 24, 25], in this study patient-to-nurse staffing ratios failed to predict nurse reports of any of the outcomes studied. As our conceptual model and the empirical evidence show, workload is influenced by a range of factors, including the amount and type of nursing resources needed to care for each patient, as well as patient case mix and complexity [26]. As such, the patient-to-nurse staffing ratio reflects only one aspect of nurses' workloads and may not have been sufficiently refined to show a relationship with the patient outcomes studied here. Placing this study's mean unit-level ratio of eight patients per nurse into context, it is similar to those of 7–14 patients per nurse described in acute care hospitals in the United Kingdom [14], but higher than the average ratio of five patients per registered nurse described in US hospitals [27, 28]. However, it should be borne in mind that patients in Swiss hospitals, particularly in the regional and cantonal hospitals, generally tend to be less acutely ill than those in some other countries (notably the US).
Higher nurse ratings of nursing resources and autonomy (as measured using the Resources subscale) were a consistent predictor of five of the six outcomes in unadjusted models, but did not remain statistically significant in models controlling for rationing and the other organizational variables. It was somewhat logical that the measure of interdisciplinary collaboration and competence (Collaboration subscale) would be associated with reports of avoidable critical patient incidents, but a significant relationship was only detected before controlling for other organizational variables. Such results are in line with prior research, which suggests that higher-quality practice environments in hospitals are associated with superior outcomes [15, 29]. However, the majority of studies in this area identify significant associations use nurse job outcomes or nurses' appraisals of care quality in general. Data has been much less clear in terms of showing work environments' effects on specific patient outcomes. For instance, McCusker et al. [30] also failed to find an association between practice environment features and the nurse-reported frequencies of various types of adverse patient events.
In summary, the results of this study suggest that rationing of nursing care, a process that occurs at the nurse–patient interface, is a strong independent predictor of patient outcomes, and may partially explain the effects of patient–to-nurse staffing ratios and nurse work environment factors on patients. Even low rationing levels were linked with deteriorating patient outcomes. Since rationing can never entirely be avoided, it is important to define the threshold above which rationing affects outcomes negatively. Such data would enable nursing administrators to use implicit rationing of nursing care (e.g., through surveys employing the BERNCA instrument) as an indicator of the impact of cost-cutting strategies and changes in the nurse practice environment on processes of care in their facilities (particularly changes in staffing levels, skill mix and other resources). Regular surveys of this (and perhaps other measures of rationing on the front lines of care) could provide data for health policy discussions about nurse staffing levels and decisions regarding mandated minimum patient-to-nurse ratios.
Limitations of the study
The Rationing of Nursing in Switzerland study, like other studies in the International Hospital Outcomes Study collaboration, used a cross-sectional design, which does not allow the direct assessment of causal relationships between implicit rationing of nursing care and patient outcomes. Furthermore, while nurses and patients from hospital units accounting for 10% of acute care beds in Switzerland were surveyed, the convenience sample here limits the generalizability of our findings, particularly for smaller facilities (<100 beds). In addition, all outcomes in this study except patient satisfaction were assessed through nurse reports. Validation of the measures in this study against hospital records of patient outcomes is currently underway.
Conclusion
Implicit rationing of nursing care is an important newly identified organizational variable reflecting processes in acute care nursing and appears to be directly linked to patient outcomes. Rationing offers promise as a measure of the impacts of staffing and the quality of the nurse practice environment on patient outcomes. As an indicator of the understudied processes of care affected by organizational conditions in hospitals, measures of rationing could assist in building theory in this area of outcomes research. Rationing levels, analyzed alongside other data, may help health systems and hospitals determine the minimum staffing and skill mix levels necessary to achieve desired patient outcomes and inform administrative decisions and policy.
Further studies are necessary to develop a deeper understanding of its mechanisms and effects. Such studies will need to incorporate prospectively collected data on patient outcomes sensitive to nursing care quality. Furthermore, studies are needed to investigate the applicability and sensitivity of rationing and the BERNCA instrument in international contexts, with different health care systems and in hospitals and units with various patient acuity levels. Also, as described above, studies are needed to define the threshold when rationing begins to affect patient outcomes negatively. A study to address this question using data from the Rationing of Nursing Care in Switzerland study is currently in preparation.
Acknowledgements
This study was funded by the Swiss Federal Office of Public Health. The authors thank the nurse leaders, resource nurses, staff nurses and patients in the study hospitals for their participation. The authors also acknowledge Chris Shultis for editing the article.
Appendix 1
BERNCA questionnaire
| How often in the last 7 working days did it happened that…..(question 1–5) | Never | Rarely | Sometimes | Often |
|---|---|---|---|---|
| 1. Activity of daily livings (ADLs) | □ | □ | □ | □ |
| 1(a) You could not assist a patient with a necessary sponge bath or skin care? | □ | □ | □ | □ |
| 1(b) You could not perform a necessary oral or dental hygiene to a patient? | □ | □ | □ | □ |
| 1(c) You could not feed the patient a needed? | □ | □ | □ | □ |
| 1(d) You were not able to mobilize or change the position of a patient? | □ | □ | □ | □ |
| 1(e) You had to leave a patient for longer than half an hour in urine, stool, or vomit? | □ | □ | □ | □ |
| 1(f) You could not put clean sheets on a dirty bed? | □ | □ | □ | □ |
| 2. Caring – support | □ | □ | □ | □ |
| 2(a) You could not offer emotional or psychosocial support to a patient even though you felt it was necessary e.g. dealing with insecurities and fear of his/her illness, the feeling of dependency? | □ | □ | □ | □ |
| 2(b) You could not have a necessary conversation with a patient or his/her family? | □ | □ | □ | □ |
| 3. Rehabilitation – instruction – education | □ | □ | □ | □ |
| 3(a) You had to put a patient in diapers or insert a catheter because you did not have time for toilet training? | □ | □ | □ | □ |
| 3(b) You could not perform activating or rehabilitating care? | □ | □ | □ | □ |
| 3(c) You could not teach and/or educate a patient and/or their family about their necessary self-care e.g. insulin injection, behavior or coping with illness- specific symptom (hypo-glycemia, dyspnea)? | □ | □ | □ | □ |
| 3(d) You could not prepare a patient or their family for his/her hospital discharge? | □ | □ | □ | □ |
| 4. Monitoring – safety | □ | □ | □ | □ |
| 4(a) You could not monitor a patient as closely as had been prescribed by a physician or as you felt was necessary? | □ | □ | □ | □ |
| 4(b) You had to restrain and/or give confused patients sedatives because you were not able to watch them carefully enough? | □ | □ | □ | □ |
| 4(c) A physician either did not come in person or took a long time to arrive after you called him/her because of an acute or sudden change in a patient's condition? | □ | □ | □ | □ |
| 4(d) You had to keep a patient who had rung for a nurse waiting longer than 5 min? | □ | □ | □ | □ |
| 4(e) You could not wash or disinfect your hands adequately? | □ | □ | □ | □ |
| 5. Documentation | □ | □ | □ | □ |
| 5(a) You did not have enough time to go over the patient documentation at the beginning of your shift? | □ | □ | □ | □ |
| 5(b) You could not set up or bring up to date a patient's care plan? | □ | □ | □ | □ |
| 5(c) You could not document the performed nursing care for a patient detailed enough? | □ | □ | □ | □ |
©December 2007, Schubert et al. Please contact the authors if you would like to use the instrument.
Appendix 2
Nursing work index – revised (NWI-R) subscales and related items
| For each item in this section, please indicate the extent to which you agree that the following items ‘are present in your current job' | Strongly agree | Somewhat agree | Somewhat disagree | Strongly disagree |
|---|---|---|---|---|
| 1 Nursing leadership and professional development (16 questions) | ||||
| 4 Supervisory staff that is supportive of nurses | □ | □ | □ | □ |
| 10 Support for new and innovative ideas about patient care | □ | □ | □ | □ |
| 13 A nurse managers who is a good manager and leader | □ | □ | □ | □ |
| 27 Nursing staff are supported in pursuing degrees in nursing | □ | □ | □ | □ |
| 8 Career development/clinical ladder opportunity | □ | □ | □ | □ |
| 41 Nurse managers consult with staff on daily problems and procedures | □ | □ | □ | □ |
| 37 A preceptor program for newly hired RNs | □ | □ | □ | □ |
| 26 Opportunities for advancement | □ | □ | □ | □ |
| 39 Staff nurses have the opportunity to serve on hospital and nursing committees | □ | □ | □ | □ |
| 18 Praise and recognition for a job well done | □ | □ | □ | □ |
| 3 A good orientation program for newly employed nurses | □ | □ | □ | □ |
| 7 Active staff development of continuing education programs for nurses | □ | □ | □ | □ |
| 28 A clear philosophy of nursing that pervades the patient care environment | □ | □ | □ | □ |
| 32 A nurse manager who backs up the nursing staff in decision-making, even if the conflict is with a physician | □ | □ | □ | □ |
| 19 The opportunity for staff nurses to consult with clinical nurse specialties or expert nurse clinicians | □ | □ | □ | □ |
| 34 An active quality assurance program | □ | □ | □ | □ |
| 2. Nursing resources and autonomy (10 questions) | ||||
| 16 Enough staff to get the work done | □ | □ | □ | □ |
| 12 Enough registered nurses on staff to provide quality patient care | □ | □ | □ | □ |
| 17 Freedom to make important patient care and work decisions | □ | □ | □ | □ |
| 11 Enough time and opportunity to discuss patient care problems with other nurses | □ | □ | □ | □ |
| 1 Adequate support services allow me to spend time with my patients | □ | □ | □ | □ |
| 14 A chief nursing officer who is highly visible and accessible to staff | □ | □ | □ | □ |
| 9 Opportunity for nurses to participate in policy decisions | □ | □ | □ | □ |
| 35 Staff nurses are involved in the internal governance of the hospital | □ | □ | □ | □ |
| 33 Administration that listens and responds to employee concerns | □ | □ | □ | □ |
| 40 The contributions that nurses make to patient care are publicly acknowledged | □ | □ | □ | □ |
| 3 Interdisciplinary Collaboration and Competence (8 questions) | ||||
| 36 Collaboration (joint practice) between nurses and physicians | □ | □ | □ | □ |
| 24 A lot of teamwork between nurses and physicians | □ | □ | □ | □ |
| 2 Physicians and nurses have good working relationships | □ | □ | □ | □ |
| 25 Physicians give high-quality medical care | □ | □ | □ | □ |
| 49 Working with experienced nurses who ‘know’ the hospital system | □ | □ | □ | □ |
| 50 RNs and assistive personnel have good working relationships | □ | □ | □ | □ |
| 30 Working with nurses who are clinically competent | □ | □ | □ | □ |
| 51 RNs and nursing students have good working relationships | □ | □ | □ | □ |
References
- Aiken LH, Clarke SP, Sloane DM. Hospital restructuring: does it adversely affect care and outcomes? J Health Hum Serv Adm. 2001;23:416–42. [PubMed] [Google Scholar]
- Norrish BR, Rundall TG. Hospital restructuring and the work of registered nurses. Milbank Q. 2001;79:55–79. doi: 10.1111/1468-0009.00196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCloskey BA, Diers DK. Effects of New Zealand's health reengineering on nursing and patient outcomes. Med Care. 2005;43:1140–6. doi: 10.1097/01.mlr.0000182549.85761.cd. [DOI] [PubMed] [Google Scholar]
- West E, Barron DN, Reeves R. Overcoming the barriers to patient-centred care: time, tools and training. J Clin Nurs. 2005;14:435–43. doi: 10.1111/j.1365-2702.2004.01091.x. [DOI] [PubMed] [Google Scholar]
- Kuenzi K, Schaer-Moser M. Synthesis Report. Bern (Switzerland): Büro Bass, Büro a&o; 2002. The labour situation in nursing in the canton of Bern [Die Arbeitssituation im Pflegebereich im Kanton Bern] (in German) p. 81. [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, et al. Nurses' reports on hospital care in five countries Health Aff (Millwood) 2001;20:43–53. doi: 10.1377/hlthaff.20.3.43. [DOI] [PubMed] [Google Scholar]
- Clarke SP. The Complexities of Care: Nursing Reconsidered. Ithaca, NY: Cornell University Press; 2006. Research on nurse staffing and its outcomes: the challenges and risks of grasping at shadows; pp. 161–84. [Google Scholar]
- Lang TA, Hodge M, Olson V, et al. Nurse-patient ratios: a systematic review on the effects of nurse staffing on patient, nurse employee, and hospital outcomes. J Nurs Adm. 2004;34:326–37. doi: 10.1097/00005110-200407000-00005. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Cheung RB, et al. Educational levels of hospital nurses and surgical patient mortality. JAMA. 2003;290:1617–23. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987–93. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Needleman J, Buerhaus P, Mattke S, et al. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346:1715–22. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- Blegen MA, Goode CJ, Reed L. Nurse staffing and patient outcomes. Nurs Res. 1998;47:43–50. doi: 10.1097/00006199-199801000-00008. [DOI] [PubMed] [Google Scholar]
- Kovner C, Gergen PJ. Nurse staffing levels and adverse events following surgery in U.S. hospitals. Image J Nurs Sch. 1998;30:315–21. [PubMed] [Google Scholar]
- Rafferty AM, Clarke SP, Coles J, et al. Outcomes of variation in hospital nurse staffing in English hospitals: cross-sectional analysis of survey data and discharge records. Int J Nurs Stud. 2007;44:175–82. doi: 10.1016/j.ijnurstu.2006.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM. Hospital staffing, organization, and quality of care: cross-national findings. Nurs Outlook. 2002;50:187–94. doi: 10.1067/mno.2002.126696. [DOI] [PubMed] [Google Scholar]
- Clarke SP, Rockett JL, Sloane DM, et al. Organizational climate, staffing, and safety equipment as predictors of needlestick injuries and near-misses in hospital nurses. Am J Infect Control. 2002;30:207–16. doi: 10.1067/mic.2002.123392. [DOI] [PubMed] [Google Scholar]
- Gunnarsdottir S, Clarke SP, Rafferty AM, et al. Front-line management, staffing and nurse-doctor relationships as predictors of nurse and patient outcomes. A survey of Icelandic hospital nurses. Int J Nurs Stud. 2007;15:1–9. doi: 10.1016/j.ijnurstu.2006.11.007. doi: 10.1016/j.ijnurstu.2006.11.007. [DOI] [PubMed] [Google Scholar]
- Vahey DC, Aiken LH, Sloane DM, et al. Nurse burnout and patient satisfaction. Med Care. 2004;42 doi: 10.1097/01.mlr.0000109126.50398.5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke SP. International collaborations in nursing research: the experience of the International Hospital Outcomes Study. Appl Nurs Res. 2004;17:134–6. [PubMed] [Google Scholar]
- Schubert M, Glass TR, Clarke SP, et al. Validation of the Basel Extent of Rationing of Nursing Care instrument. Nurs Res. 2007;56:416–24. doi: 10.1097/01.NNR.0000299853.52429.62. [DOI] [PubMed] [Google Scholar]
- Jones PS, Lee JW, Phillips LR, et al. An adaptation of Brislin's translation model for cross-cultural research. Nurs Res. 2001;50:300–4. doi: 10.1097/00006199-200109000-00008. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Patrician PA. Measuring organizational traits of hospitals: the Revised Nursing Work Index. Nurs Res. 2000;49:146–53. doi: 10.1097/00006199-200005000-00006. [DOI] [PubMed] [Google Scholar]
- Lake ET. Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25:176–88. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- McCloskey JM. Nurse staffing and patient outcomes. Nurs Outlook. 1998;46:199–200. doi: 10.1016/s0029-6554(98)90047-1. [DOI] [PubMed] [Google Scholar]
- Weissman JS, Rothschild JM, Bendavid E, et al. Hospital workload and adverse events. Med Care. 2007;45:448–55. doi: 10.1097/01.mlr.0000257231.86368.09. [DOI] [PubMed] [Google Scholar]
- O'Brien-Pallas L, Meyer R, Thomson D. Quality Work Environments for Nurse and Patient Safety. Boston: Jones and Bartlett Publishers; 2005. Workload and productivity; pp. 105–31. [Google Scholar]
- Bolton LB, Jones D, Aydin CE, et al. A response to California's mandated nursing ratios. J Nurs Scholarsh. 2001;33:179–84. doi: 10.1111/j.1547-5069.2001.00179.x. [DOI] [PubMed] [Google Scholar]
- Sochalski J. Is more better? The relationship between nurse staffing and the quality of nursing care in hospitals. Med Care. 2004;42:II67–73. doi: 10.1097/01.mlr.0000109127.76128.aa. [DOI] [PubMed] [Google Scholar]
- Aiken LH. Magnet Hospitals Revised. Attractions and Retention of Professional Nurses. Washington DC: American Nurses Association; 2002. Superior outcomes for magnet hospitals; pp. 61–7. [Google Scholar]
- McCusker J, Dendukuri N, Cardinal L, et al. Nursing work environment and quality of care: differences between units at the same hospital. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2004;17:313–22. doi: 10.1108/09526860410557561. [DOI] [PubMed] [Google Scholar]