Abstract
Objective
To measure the length of time spent discussing all aspects of new prescriptions and guideline-recommended aspects of counseling, and to evaluate factors associated with duration of discussion.
Methods
We analyzed tape recordings in which 181 patients received 234 new medication prescriptions from 16 family physicians, 18 internists, and 11 cardiologists in 2 healthcare systems in Sacramento, California between January and November 1999.
Results
Of the mean total visit time of 15.9 minutes (SD=434 seconds), a mean of 26 seconds (SD=28 seconds) was allocated to guideline-recommended components and a mean of 23 seconds (SD=25 seconds) was allocated to discussion of all other aspects of new prescription medications. The majority of time spent discussing individual new prescriptions was dedicated to: medication purpose or justification, directions and duration of use, and side effects. On average, more complete discussion of these components was associated with more time. More time was spent talking about guideline-recommended information if patients were in better health, if there was a third party in the room, and if the medication belonged to a psychiatric, compared to an ear, nose, throat medication class. Less time was spent discussing over-the-counter medications and those prescribed to patients with a previous visit to the physician.
Conclusion
Higher quality information transmission between physicians and patients about new medications requires more time, and may be difficult to achieve in short office visits.
Practice Implications
Time-compressed office visits may need to be redesigned to promote improved provider-patient communication about new medications.
Keywords: provider-patient communication, physician-patient relations, time, prescription medication
1. Introduction
The mean office visit time in the United States and the United Kingdom has measurably increased over the past few decades (1–3). However, physicians feel more time pressure due to higher expectations to provide quality medical care, a greater range of treatment options to discuss (4), and patients with more complex and chronic conditions (2). Physicians must provide a large number of preventive services (5) in addition to taking a history, performing a physical examination, and detailing treatment plans for patients. Documentation requirements have expanded. Because nearly two-thirds of office visits include a medication prescription (6), medication discussions are integral to the time spent in the physician-patient encounter.
The Agency for Healthcare Research and Quality recommends that patients receiving new medications ask about information such as the medication name, directions, purpose or reason for taking the medication, anticipated side effects, and duration of use (7, 8). Similarly, guidelines suggest that physicians educate older patients receiving new prescriptions about the medication’s purpose, side effects, and directions for use (9, 10). However, physicians offer only spotty counseling about these topics (11–17).
Prior studies suggest that up to one-quarter of primary care visit time may be devoted to discussions of treatment planning (18) or medication discussion (19). However, it is not known what proportion of visits is spent discussing issues pertaining to new medications, how time spent talking about new medications is allocated, and whether more time dedicated to medication-related topics is associated with more information being transmitted. In addition, little is known about which physician and patient characteristics are associated with the amount time spent discussing medications. Studies have shown that female physicians spend more time overall with patients than their male counterparts (20, 21); in addition, older patients (3, 21, 22), women (21), those with more problems to discuss (21), and those who are new to a physician’s practice (22) have longer visits. Whether these factors affect time discussing medications, however, has not been studied.
Because time limitations are a major constraint to transmitting information in the clinical setting and physicians miss many essential aspects of information about new medications, understanding how physicians spend time discussing core elements, as opposed to other aspects concerning new prescriptions, is important to developing strategies for improving communication about new prescriptions. To fill this research gap, this study posed the following questions: 1) How much time is spent discussing guideline-recommended and other information concerning new medications, and how is this time allocated? 2) Is the amount of time spent discussing new medications related to the quality of information transmitted? 3) What factors are associated with more time spent covering guideline-recommended new medication topics?
2. Methods
We analyzed data from the Physician-Patient Communication Project, a study of physician-patient interactions in two healthcare systems in Sacramento, California that was conducted between January and November 1999. The study audiotaped 909 patient encounters with 18 internists, 16 family physicians and 11 cardiologists. Twenty-two physicians were from Kaiser Permanente and 23 from the University of California-Davis Medical Group. One family physician prescribed no new medications and was dropped from our sample. Patients and physicians were surveyed prior to and immediately after office visits. Study details are described elsewhere (23).
2.1 Patient, Physician, and Visit Characteristics
Patients were queried about their demographics, physical functioning at the time of the visit (using the 36-item Short-Form Health Survey physical functioning scale, version 1, with 100 indicating maximum functioning; α = 0.93 (24)), and whether they had a prior visit with the physician seen on the day of the visit. Physicians were queried about their demographics, specialty, and site of practice. The presence of an adult third party in the room was determined by listening to the audiotapes and reading the transcripts.
2.2 Medication Characteristics
We defined a new prescription as one that a patient had never before taken (and that did not belong in the same class as a previously taken medication), or one prescribed for an acute condition or symptom (such as an antibiotic or analgesic). In a post-visit survey, physicians identified 270 patients, among the 860 who had their visits successfully audiotaped and transcribed, as receiving new prescriptions. We reviewed 90 randomly selected transcripts and demonstrated that physicians correctly identified 24 of 25 encounters (96%) in which new medications were prescribed. We subsequently identified 185 encounters in which 243 new medications were prescribed (11). Four audiotapes were lost, so our final sample consisted of 181 encounters, encompassing 234 new prescriptions.
Each new medication prescription was categorized into an appropriate medication category. In addition, over-the-counter (OTC) medications were defined as medications that could be bought without a prescription. Over-the-counter medications recommended at prescription strength were classified as non-OTC medications.
2.3 Medication Communication Index (MCI)
The Medication Communication Index (MCI) measures the quality of physician-patient communication about important elements of communication about new medications (11). Its components are specified by physician- and patient-directed guidelines and recommendations about new medication discussions (7–10). The MCI is a 5-point index that ranges from 0–5. Physicians receive one point for making statements that fulfill each of the following four topics: medication name; purpose or justification for taking the medication; duration of intake; and anticipated side effects. They also receive 0.5 point for discussing the number of pills or sprays to take and 0.5 point for discussing either the frequency or timing of medication intake. These reflect “directions for medication use,” which carries equal weight with the other MCI components. Physicians prescribing dermatologic medications receive a full point if they discuss either the frequency or timing of medication use, since it is difficult to quantify an amount for these medications.
2.4 Development of Codes Describing New Medication Discussions
Two coders of different disciplines (JH and DMT) worked together and used visit transcripts to develop an initial set of codes to describe all conversations about new medication prescriptions in the visits. These codes were based on previous literature (14–16) and clinical experience. The coders used analytic induction to split, merge, and adjust the codes until they were mutually exclusive, yet still described every conversational element concerning new prescriptions. One coder (DMT) applied these codes to all 185 visit transcripts, and a third coder (DAP) independently coded 16% of the transcripts, achieving a mean kappa score with the first coder (DMT) of 0.90 (range 0.79 to 0.98).
The 76 final codes included topics such as: medication name, directions and duration of use, purpose or justification for the medication, side effects, medication adherence, potential interactions and medication safety, cost and insurance issues, logistics of obtaining medications, medication supply and refills, and direct-to-consumer advertising. More details on how the codes were defined have been previously described (11, 25, 26).
2.5 Measurement of Time
Audiotapes of the 181 encounters examined in this study were digitized. We listened to the digitized files to quantify all of the time measurements. Time was measured by determining the number of seconds which physicians or patients spent discussing topics of interest. We quantified total visit length by measuring the amount of face-to-face time in the examining room to the tenth of a second. To determine the total time spent discussing information about each new medication, we timed physician- and patient-initiated statements corresponding to the codes describing new medication discussions. Each medication was analyzed separately, even if a visit contained multiple medication prescriptions. Statements applying to more than one medication counted toward the time for both medications. Quotes fulfilling two topics of conversation were counted toward the time for both categories, but were counted only once toward the total time spent discussing new medications during the visit.
The total time spent discussing components of the MCI and other aspects of individual medications was calculated by adding the time physicians and patients spent on the individual topics. Time discussing the MCI components for each new medication was calculated by adding the time spent on: medication directions, duration of use, purpose or justification for use, and side effects. Medication name, the fifth component of the MCI, was not timed separately because references to medication names were nearly always incorporated in the other statements Each encounter for which less than 20 seconds was spent discussing a new medication was reviewed for accuracy by a second person.
2.6 Statistical Analyses
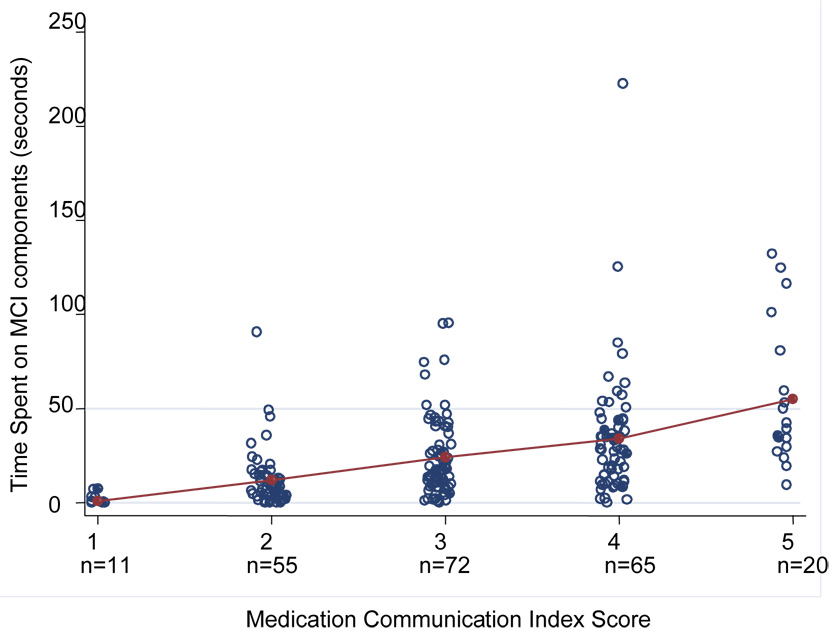
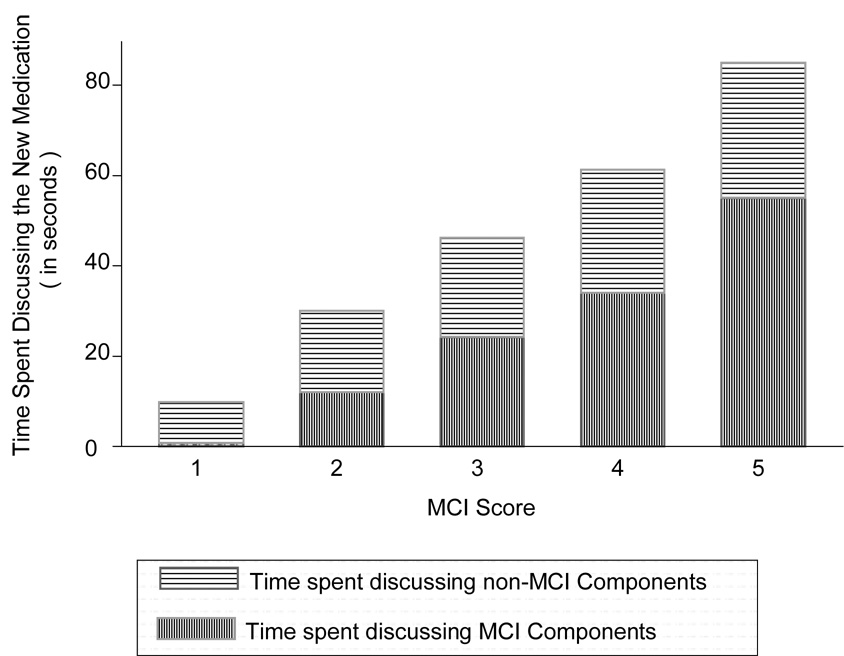
We addressed Question 1 by using STATA statistical software, version 8.0 (StataCorp, College Station, TX) to tabulate total visit length, and time spent discussing: MCI components; other aspects of individual medications; and specific topics concerning individual medications. Using graphical representation, we addressed Question 2 by exploring the relationship between the MCI score and the time spent discussing MCI components. In order to better visualize data points, we added a small amount of random noise to data that would normally be plotted on top of each other (jittering). We also graphically assessed the relationship between the MCI score and a comparison of the mean time spent on the MCI and non-MCI aspects of individual medications. We graphed only values corresponding to whole-number MCI scores.
To assess Question 3, we conducted bivariate analyses to assess the relationship between the time spent discussing new medications and patient, physician, visit, and medication characteristics. T-tests, analysis of variance and correlation coefficients, as appropriate for categorical and continuous variables, were performed. Parametric and non-parametric testing (using Wilcoxon, Kruskal-Willis and Spearman rank-order correlation tests) gave similar significant results for all variables except for patient age. Continuous variables included patient and physician age, patient physical functioning, and total number of new medications prescribed. Categorical variables included patient gender, ethnicity (Caucasian versus non-Caucasian), prior visit to the physician, physician gender, specialty and site of practice, medication class (analgesic; antibiotic; cardiovascular; dermatological; ear, nose, throat; gastrointestinal; respiratory; psychiatric; other), OTC status; and presence of a third party in the room during the office visit.
Independent variables were included in a multiple linear regression model looking at the time spent discussing MCI aspects of individual new medications. The independent variables described above were included with the time spent discussing MCI components in another multiple linear regression model with the MCI score as the dependent variable. Multiple imputation by chained equations (ICE and MICOMBINE) was used to impute missing data for 9 medications. Standard errors were adjusted for clustering within physician for the first model. Intraclass correlation estimates for second model were small (p<0.001) at the physician, patient, specialty and site levels, so this model was not adjusted. Model goodness of fit was evaluated using R2. No multicollinearity was found among the predictor variables.
3. RESULTS
3.1 Patient and Physician Characteristics
Of the 181 patients in the study, 51% were male and 83% Caucasian. They had a mean age of 56 years (SD=16), and 80% had at least some college education. Thirty-two percent visited family physicians, 45% saw internists, and 23% went to cardiologists, and 75% had previously visited the same physician (Table 1). The 44 physicians in this study had a mean age (SD) of 44 years (8.4), approximately 71% were male, and 89% were Caucasian. The mean MCI score for the 234 medications prescribed was 3.1 (SD=1.0). Only gender was different between patients prescribed new medications and the full sample.
Table 1.
Patient and visit characteristics for all patients and patients prescribed new medications†
| Characteristic | Patients Prescribed New Medications | All Patients | ||
|---|---|---|---|---|
| n | n | |||
| Age, mean years (SD) | 180 | 55.6 (15.7) | 905 | 57.0 (15.3) |
| Male, n (%) * | 181 | 92 (50.8) | 908 | 398 (43.8) |
| Caucasian, n (%) | 178 | 147 (82.6) | 904 | 736 (81.4) |
| Educational level, n (%) | 178 | 904 | ||
| High school or less | 35 (19.6) | 208 (23.0) | ||
| Some college education | 86 (48.3) | 423 (46.8) | ||
| College graduate | 57 (32.0) | 273 (30.2) | ||
| Has health insurance, n (%) | 181 | 170 (93.9) | 905 | 869 (96.0) |
| UC-Davis patient, n (%) | 181 | 85 (47.0) | 909 | 443 (48.7) |
| Had prior visit to same doctor, n (%) | 180 | 135 (75.0) | 892 | 714 (80.0) |
| Specialty of physician, n (%) | 181 | 909 | ||
| Family Medicine | 57 (31.5) | 333 (36.6) | ||
| Internal Medicine | 82 (45.3) | 363 (39.9) | ||
| Cardiology | 42 (23.2) | 213 (23.4) | ||
| Number of new medications prescribed during visit, mean (SD) | 181 | 1.3 (0.6) | N/A | |
A total of 181 patients were prescribed new medications, and there were 909 total patients in the study. Variations in the n reflect missing data.
p<0.05 for comparison between patients prescribed new medications and full sample of 909 patients
3.2 Duration of Time for New Medication Discussions
The mean total visit length was 952 (SD=434) seconds, or 15.9 minutes. Approximately 5% of this time, or a mean of 49 seconds (SD=47), was spent discussing all aspects of newly prescribed medications. Approximately 2.7% of the total visit length, or a mean of 26 seconds (SD=28) was spent discussing MCI components of new medications. Physicians spent between 1.9 and 351 seconds discussing all aspects of new prescriptions, and between 0 and 210 seconds conveying MCI information (Table 2).
Table 2.
Duration of physician-patient discussions about new medications
| N | % of total | Mean time, in seconds (SD), when communication occurred | Range | Mean time, in seconds (SD), for all medications; n=234 | |
|---|---|---|---|---|---|
| Total visit length | 181 | 100 | 952 (434) | 283 – 2642 | N/A |
| Time spent discussing MCI components of individual new medications | 234 | 100 | 25.9 (27.8) | 0 – 210 | N/A |
| Time spent discussing all other aspects of individual new medications | 234 | 100 | 22.9 (25.2) | 0 – 147 | N/A |
| Physician communication about newmedications | |||||
| Cost / insurance issues | 22 | 9.4 | 14.9 (13.0) | 1.1 – 39 | 1.39 (5.78) |
| Side effects * | 88 | 37.6 | 12.6 (16.6) | 0.8 – 77 | 4.72 (11.8) |
| Purpose / justification for medication * | 189 | 80.8 | 12.4 (12.2) | 0.9 – 75 | 10.0 (12.0) |
| Directions for taking medications * | 178 | 76.1 | 11.1 (11.8) | 0.7 – 95 | 8.45 (11.4) |
| Medication interactions | 23 | 9.8 | 6.47 (6.02) | 1.0 – 28 | 0.64 (2.67) |
| Direct-to-consumer advertising | 1 | 0.4 | 10.65 (N/A) | N/A | 0.05 (0.70) |
| Adherence | 19 | 8.1 | 5.50 (5.83) | 1.5 – 27 | 0.45 (2.21) |
| Logistics of obtaining medications | 38 | 16.2 | 5.26 (6.34) | 0.8 – 26 | 0.85 (3.19) |
| Duration of medication use * | 61 | 26.1 | 4.57 (4.45) | 0.5 – 23 | 1.19 (3.02) |
| Prior history of use | 61 | 26.1 | 3.52 (2.76) | 0.7 – 13 | 0.92 (2.09) |
| Allergies | 19 | 8.1 | 3.47 (4.56) | 0.3 – 21 | 0.28 (1.58) |
| Medication refills | 13 | 5.6 | 3.15 (2.10) | 1.1 – 7.2 | 0.18 (0.87) |
| Medication supply | 22 | 9.4 | 2.85 (2.59) | 0.7 – 13 | 0.27 (1.14) |
| Safety | 16 | 6.8 | 2.50 (1.16) | 0.7 – 4.2 | 0.17 (0.70) |
| Patient-initiated statements and questions | |||||
| Patient request for medications | 27 | 11.5 | 8.72 (9.25) | 1.0 – 45 | 1.01 (4.17) |
| Direct-to-consumer advertising / internet | 6 | 2.6 | 7.04 (7.56) | 1.6 – 22 | 0.18 (1.57) |
| Resistance to starting medications | 14 | 6.0 | 6.34 (5.79) | 1.1 – 19 | 0.38 (2.03) |
| Cost / insurance issues | 10 | 4.3 | 6.25 (4.80) | 0.9 – 17 | 0.27 (1.58) |
| Medication supply | 5 | 2.1 | 6.20 (4.99) | 1.4 – 14 | 0.13 (1.11) |
| Medication interactions | 15 | 6.4 | 4.79 (3.38) | 1.2 – 12 | 0.31 (1.44) |
| Side effects | 26 | 11.1 | 4.70 (4.13) | 1.4 – 20 | 0.52 (2.01) |
| Logistics of obtaining medications | 23 | 9.8 | 3.91 (2.80) | 0.8 – 11 | 0.38 (1.45) |
| Directions for taking medications | 45 | 19.2 | 3.59 (3.01) | 0.6 – 13 | 0.69 (1.93) |
| Duration of medication use | 7 | 3.0 | 3.14 (2.90) | 0.9 – 7.4 | 0.09 (0.71) |
| Purpose / justification for medication | 19 | 8.1 | 2.75 (2.49) | 0.9 – 11 | 0.22 (1.02) |
| Medication refills | 2 | 0.8 | 1.82 (0.66) | 1.4 – 2.3 | 0.02 (0.17) |
Components of the MCI along with medication name
Table 2 also depicts the amount of time that physicians spent communicating about medication-related topics, and the length of time spent by patients when they initiated statements or questions about a new prescription. In visits during which a particular medication-related topic was broached, physicians spent the most time talking about: cost and insurance issues, explaining medication side effects, discussing medication purpose or justification for use, and giving directions for taking medications. For the 22 new medications for which cost/insurance was discussed, physicians spent a mean of 14.9 seconds (SD=13) commenting about the issue. Across all medications, a mean of 1.4 seconds (SD=5.8) was spent on cost/insurance. Topics consuming the most time during the office visit were medication purpose or justification for use (mean of 10 seconds (SD=12)), directions (mean of 8.5 seconds (SD=11)), and side effects (mean of 4.7 seconds (SD=12)).
Patients rarely initiated conversations or questions during office visits. When they did, they spent the most time, a mean of 8.7 seconds (SD=9.3), requesting medications. They also spent a mean of 4.7 seconds (SD=4.1) on queries about medication side effects and a mean of 3.6 seconds (SD=3.0) asking about medication directions. When patients brought up not wanting to start medications, cost/insurance issues, and medication supply, they spent a mean of over 6 seconds on each of the topics (Table 2).
When patients requested medications, significantly more time was spent discussing the new medication (mean 86 seconds (SD=71) versus 44 seconds (SD=41) when patients did not request medications), though there were no significant differences in visit length. Similarly, when cost/insurance issues were raised, significantly more time was spent conversing about the new medication (mean 52 seconds (SD=31) versus 42 seconds (SD=38) when cost was not brought up).
3.3 Discussion Duration and Medication Communication Index
There was wide variation in the discussion time needed to complete all the MCI components. Fulfillment of more elements of the MCI on average involved more discussion time (Figure 1). When physicians fulfilled all elements of the MCI for a medication, they spent 11 to 133 seconds (mean=55 seconds (SD=38)) discussing these issues. For those medications with an MCI score of 5, overall discussions about the new prescription took a mean of 85 seconds (SD=64 seconds) with a range of 21 to 263 seconds. The amount of time spent discussing non-MCI aspects of medications remained relatively constant when physicians fulfilled more MCI elements. When the MCI was low, most of the medication-related discussion time was spent discussing non-MCI elements, but as the MCI increased, a greater proportion of the time was dedicated to communicating about the MCI components. To achieve an MCI score of 5, approximately 55 of the total 85 seconds spent discussing a new medication was dedicated to the MCI aspects (Figure 2). There was no correlation between the MCI score and total visit length (not shown). In a multivariate analysis of predictors of the MCI score, time spent discussing MCI components was independently related to covering more MCI information components (p<0.001).
Figure 1.
Relationship of Medication Communication Index (MCI) score to time (in seconds) spent discussing MCI components of individual medications. Mean times for discussion are represented by the lines in the graph. Each dot represents data for an individual medication. A small amount of random jitter is added to each MCI score to better visualize overlapping data points.
Figure 2.
Relationship of MCI score and mean time (in seconds) spent discussing the MCI and non-MCI aspects of individual medications, by MCI score.
3.4 Factors Associated with MCI Discussion Duration
In bivariate analyses, significantly more time was spent on the MCI components of new medication discussions if the medications were non-OTC; if patients were Caucasian or new to the physician; and if there was a third party in the room. The more medications prescribed during the visit, the less time that was spent on each new medication. There also were significant differences among medication class and physician specialty, but not between sites.
In multivariate analyses of the time spent discussing the MCI components of new medications, significantly more time was spent if patients were in better health, and if there was a third party in the room. More time also was spent discussing psychiatric, compared to ear, nose, throat medications. Significantly less time was spent when medications were OTC, and when patients had previously seen the physician. Compared to cardiologists, family physicians spent less time discussing MCI components (Table 3).
Table 3.
Multivariate model predicting amount of time discussing MCI components of individual new medications
| Bivariate Relationships | Multivariate Relationship | ||||
|---|---|---|---|---|---|
| Independent Variables † | n | Mean time in seconds (SD) | Correlation Coefficient | β-coefficient (95% Confidence Interval) | P-value |
| Medication Class | |||||
| Analgesics | 34 | 17.8 (18.8) * | 0.91 (−8.59, 10.4) | 0.84 | |
| Antibiotics | 34 | 18.1 (22.2) * | −4.92 (−15.0, 5.13) | 0.33 | |
| Cardiovascular | 46 | 41.1 (38.6) * | 10.6 (−0.19, 21.3) | 0.05 | |
| Dermatologic | 20 | 15.1 (19.4) * | 1.66 (−10.1, 13.4) | 0.78 | |
| Ear, nose and throat | 39 | 16.0 (12.1) * | N/A | N/A | |
| Gastrointestinal | 15 | 15.0 (10.6) * | −0.53 (−9.15, 8.09) | 0.90 | |
| Psychiatric | 19 | 42.3 (23.2) * | 24.3 (13.0, 35.7) | <0.001 | |
| Pulmonary | 10 | 28.0 (29.2) * | 10.4 (−9.40, 30.1) | 0.30 | |
| Other | 17 | 23.2 (19.5) * | 2.55 (−21.4, 26.5) | 0.83 | |
| Over-the-counter medication | 39 | 11.2 (11.4) * | −13.5 (−21.1, −5.81) | 0.001 | |
| Non over-the-counter medication | 195 | 27.0 (27.4) * | N/A | N/A | |
| # of new medications prescribed during visit | 234 | −0.03 | 0.44 (−3.17, 4.05) | 0.81 | |
| Patient Age | 229 | 0.003 | −0.08 (−2.63, 2.48) | 0.95 | |
| Female patient | 114 | 23.9 (24.1) | 2.69 (−3.19, 8.57) | 0.36 | |
| Male patient | 120 | 24.9 (28.0) | N/A | N/A | |
| Caucasian patient | 181 | 26.5 (27.1) | 5.97 (−3.86, 15.8) | 0.23 | |
| Non-Caucasian patient | 46 | 17.1 (21.9) | N/A | N/A | |
| Prior visit to same doctor | 176 | 19.9 (17.9) * | −12.7 (−22.1, −3.31) | <0.01 | |
| New to doctor | 57 | 38.7 (39.3) * | N/A | N/A | |
| Physical functioning (time of visit) | 233 | 0.007 | 1.65 (0.63, 2.68) | <0.01 | |
| Specialty | |||||
| Family Medicine | 76 | 19.1 (17.8) * | −12.6 (−24.7, −0.63) | 0.04 | |
| Internal Medicine | 111 | 21.9 (22.1) * | −5.48 (−18.0, 7.08) | 0.38 | |
| Cardiology | 47 | 38.7 (38.7) * | N/A | N/A | |
| Kaiser | 125 | 22.8 (26.4) | −2.06 (−9.62, 5.50) | 0.59 | |
| UC-Davis Medical Group | 109 | 26.2 (25.7) | N/A | N/A | |
| Female physician | 75 | 23.7 (29.3) | 6.41 (−4.09, 16.9) | 0.23 | |
| Male physician | 159 | 24.7 (24.5) | N/A | N/A | |
| Third party in the room | 32 | 44.4 (44.7) * | 18.7 (4.43, 32.9) | 0.01 | |
| No third party in the room | 202 | 23.0 (22.9) * | N/A | N/A | |
Boldface entries indicate p<=0.05
p <=0.001
n=234; mean model R2 = 0.34 (range 0.332-0.337). Independent variables have reference groups as follows: medication class: ear, nose and throat medications; over-the-counter medication: non-over-the-counter medication; # of new meds prescribed during visit: per medication; patient age: per decade; Caucasian patient: non-Caucasian patient; physical functioning at time of visit: per 10 points on 100-point scale (higher score represents better function); specialty: cardiology; Kaiser site: UC-Davis Medical Group; female physician: male physician; third party in the room: no third party in the room.
4. Discussion and Conclusions
4.1 Discussion
This study provides an in-depth understanding of how office visit time is allocated to conversations concerning new medication prescriptions. Approximately 5% of the 16 minute office visit length in this study was spent introducing and explaining newly prescribed medications. The average visit time is similar to those reported in previous studies (1, 19, 27, 28). More than half of this time was dedicated to discussing the core issues contained in the MCI of how many, when, why and for how long to take the medication, and medication side effects. Discussion of all five components of the MCI consumed between 11 and 133 seconds, with a mean time expenditure of nearly a minute.
Prior studies have demonstrated that physicians typically address two to six topics during an office visit (28–31). But the contents of a visit do not substantially change the total visit length; physicians perform tradeoffs in their discussions to maintain similar overall visit times (27). Indeed, although physicians in this study required more time to more thoroughly cover the basics of new medication information, this was not reflected in the total office visit length. Given that visit length is generally fixed, other visit components may need to be displaced when prescribing new medications, especially when multiple medications are prescribed during a visit, and for physicians with a more deliberate education style. Prior work showed that physicians often did not discuss important elements of new medication prescribing information, such as how to take the medication and how long to keep taking it (11, 12, 14, 16). This study suggests that time pressure and other competing demands may contribute to inadequate prescribing communication.
When prescribing new medications, physicians spent more overall time when discussing more guideline-recommended MCI information. This increase was due primarily to increased time spent conveying MCI information, since the time spent on non-MCI information varied little as physicians fulfilled more MCI elements. Time spent discussing non-MCI aspects may reflect conversation addressing patient concerns, or patient-centered communication, and may not be as amenable to modification.
When they arose, conversations related to cost/insurance involved the greatest amount of time, and led to longer overall discussions about the medication prescribed. However, these discussions occurred infrequently in this and other studies (26, 32), despite patient desires to converse about out-of-pocket expenses (32). In other settings with greater diversity of insurance plans and formularies, medication cost and insurance may be discussed more, though time constraints may be a universal barrier to these conversations (33). When patients initiated questions or statements, they spent the most time discussing medications they had heard about via direct-to-consumer advertising or the internet, requesting medications, and expressing reluctance to start medications. Longer discussions about a medication occurred when patients requested a drug, though visit length did not change. Although patients ask medication-related questions in less than half of office visits (19), time spent addressing patient medication requests may come at the expense of other office visit activities.
The variation in time dedicated to discussions of the MCI aspects of new prescriptions is due to patient, visit and medication characteristics. This also may reflect physician perspectives concerning patient potential for information recall and medication adherence, and attitudes toward shared decision making and patient-centered practice. In general there is little evidence of shared decision making concerning new medication discussions (17), or that physicians assess patient understanding of information provided (28), though patients retain more information when they are asked to repeat instructions (34). Whether physicians can learn to more efficiently cover all aspects of the MCI while ensuring patient understanding about a new medication requires study.
More time was spent discussing new medications with patients who were in better health. Healthier patients may have more questions and concerns due to their inexperience with medications, and may be more anxious if they are receiving a new diagnosis. Alternatively, fewer competing demands may permit physicians to have longer discussions with patients about new prescriptions. This is concerning because more ill patients may require more thorough explanations about how to take their medication and increased coordination of drug-drug and drug-disease interactions. The presence of a third party in the room significantly increased the amount of time spent discussing the MCI aspects of new medications. These individuals may ask additional questions on a patient’s behalf, which could lead to more complete medication discussions. Less time was spent discussing medications prescribed to patients with prior visits to physicians. This suggests more efficient communication between a physician and patient who know each other, but also could reflect more focus being placed on other topics, or on increased social exchange, which could detract from discussions about new prescriptions. Physicians also may feel more comfortable imparting less information to patients with whom they have a prior relationship, since patient trust is associated with medication adherence (35, 36).
More time was spent discussing psychiatric medications, versus ear, nose, throat preparations. This is encouraging because these medications have greater potential for serious side effects and often require careful titration at initiation. Significantly less time was spent when over-the-counter medications were prescribed or recommended, perhaps because physicians feel less need to counsel about medications that patients can buy without a prescription. In combination with inadequate patient knowledge about the use of OTC medications (37, 38), these findings support the need for careful evaluation of safety concerns and educational materials when prescription drugs are converted to OTC status (39, 40).
Study limitations include the Hawthorne effect of having a tape recorder in the room, which may have increased physician attention to communicating with patients. The patient population in this study was mostly Caucasian, all spoke English, most had at least some college education, and almost all had health insurance. Thus, these results may not be generalizable to patients of other ethnicities or to those with lower educational achievement or lack of English proficiency. Further research should assess potential differences in counseling based on patient race, educational level, and health literacy. These data were collected in 1999; now there may be even more time pressure on physicians. In addition, direct-to-consumer advertising was in its infancy at that time, and may play a larger role in current office visits. This study did not collect patient medication-related and health outcomes; the relationship between time spent discussing medications and patient outcomes warrants future investigation.
Estimates of the amount of time physicians spent discussing MCI and non-MCI components may be overestimated, since statements fulfilling more than one category were counted in the time for both categories. For example, a statement such as “taking medications five times a day is tough,” which expresses understanding about the difficulty of adherence and gives the patient directions about the frequency of use, was counted toward the discussion time of both categories. In addition, all directions about new medications were timed, including directions concerning dose adjustment and inhaler use. The coding framework was generous in giving credit for fulfillment of MCI components. For example, a comment such as: “So I wouldn’t expect any major problems,” was counted as a side effect discussion. A full description of information that patients may desire might far exceed the mean of about one minute that physicians in this study required to cover the 5 MCI components.
4.2 Conclusion
The present study quantifies the time needed to provide information to patients about new medications, showing that more time is required to cover the important elements of education to prescribe a new medication. In time-compressed visits, physicians may focus on addressing patient concerns or on conducting patient-centered discussions at the expense of discussions about guideline-recommended information. Given time constraints, increased time dedicated to discussions about new prescriptions may detract from conversations about other issues. It is not known whether the time delegated to medication discussions affects patient adherence or outcomes.
4.3 Practice Implications
Physicians can take away from this study that inadequate information about new medications is transmitted to patients and that the remedy could be more efficient transmission of information, new ways of getting this job done, or longer office visits. Yet prior work has shown that highly technically efficient but short office visits garner patient dissatisfaction and ratings of poor communication (41). One study suggests that physicians in high-volume practices sacrifice the delivery of preventive services and have less positive relationships with their patients (42). Though interventions to increase appointment duration did not change prescribing rates or patient satisfaction (43), they can increase physician health education (44) and prevention activities (45), and promote psychosocial discussions (45). Results from this study suggest that office visits may need to be restructured in order to promote improved communication about new prescriptions. Future research should investigate potential solutions, such as delegating some aspects of the office visit away from the physician, teaching physicians to become more efficient communicators, having other healthcare providers or computers communicate prescribing information, or increasing office visit length. Physicians might ask what they can do to ensure that every patient given a new prescription receives information about each of the basic elements of new medication education.
Acknowledgements
Data used in this study were collected with support from the Robert Wood Johnson Foundation (Grant #034384). Dr. Tarn was supported by a UCLA Mentored Clinical Scientist Development Award (5K12AG001004). Dr. Kravitz was supported in part by a mid-career research and mentoring award from the National Institute of Mental Health (1K24MH072756-01). The authors wish to express their gratitude to Netta Avineri, B.A, for her help with timing the transcripts, to their UC-Davis colleagues, and to the physicians, staff and patients at participating offices.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mechanic D, McAlpine DD, Rosenthal M. Are patients' office visits with physicians getting shorter? N Engl J Med. 2001;344(3):198–204. doi: 10.1056/NEJM200101183440307. [DOI] [PubMed] [Google Scholar]
- 2.Freeman GK, Horder JP, Howie JG, et al. Evolving general practice consultation in Britain: issues of length and context. Brit Med J . 2002;324(7342):880–882. doi: 10.1136/bmj.324.7342.880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stafford RS, Saglam D, Causino N, et al. Trends in adult visits to primary care physicians in the United States. Arch Fam Med. 1999;8(1):26–32. doi: 10.1001/archfami.8.1.26. [DOI] [PubMed] [Google Scholar]
- 4.Mechanic D. How should hamsters run? Some observations about sufficient patient time in primary care. Brit Med J . 2001;323(7307):266–268. doi: 10.1136/bmj.323.7307.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93(4):635–641. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hing E, Cherry DK, Woodwell DA. National Ambulatory Medical Care Survey: 2004 summary. Adv Data. 2006;(374):1–33. [PubMed] [Google Scholar]
- 7.Rockville, MD: Agency for Healthcare Research and Quality; Quick Tips--When Getting a Prescription. AHRQ Publication No. 01-0040c. 2002 May; Retrieved December 6, 2007 from http://www.ahrq.gov/consumer/quicktips/tipprescrip.htm.
- 8.Rockville, MD: Agency for Healthcare Research and Quality; Questions are the Answer: Getting a Prescription. Retrieved December 6, 2007 from http://www.ahrq.gov/questionsaretheanswer/level3col_1.asp?nav=3colNav05&content=05_0_prescription.
- 9.Knight EL, Avorn J. Quality indicators for appropriate medication use in vulnerable elders. Ann Intern Med. 2001;135(8 Pt 2):703–710. doi: 10.7326/0003-4819-135-8_part_2-200110161-00009. [DOI] [PubMed] [Google Scholar]
- 10.Shrank WH, Polinski JM, Avorn J. Quality indicators for medication use in vulnerable elders. J Am Geriatr Soc. 2007;55 Suppl 2:S373–S382. doi: 10.1111/j.1532-5415.2007.01345.x. [DOI] [PubMed] [Google Scholar]
- 11.Tarn DM, Heritage J, Paterniti DA, Hays RD, Kravitz RL, Wenger NS. Physician communication when prescribing new medications. Arch Intern Med. 2006;166(17):1855–1862. doi: 10.1001/archinte.166.17.1855. [DOI] [PubMed] [Google Scholar]
- 12.Richard C, Lussier MT. Nature and frequency of exchanges on medications during primary care encounters. Patient Educ Couns. 2006;64(1–3):207–216. doi: 10.1016/j.pec.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Makoul G, Arntson P, Schofield T. Health promotion in primary care: physician-patient communication and decision making about prescription medications. Soc Sci Med. 1995;41(9):1241–1254. doi: 10.1016/0277-9536(95)00061-b. [DOI] [PubMed] [Google Scholar]
- 14.Svarstad BL. The Doctor-Patient Encounter: An observational study of communication and outcome. University of Wisconsin; 1974. [Google Scholar]
- 15.Scherwitz L, Hennrikus D, Yusim S, Lester J, Vallbona C. Physician communication to patients regarding medications. Patient Educ Couns. 1985;7(2):121–136. doi: 10.1016/0738-3991(85)90003-5. [DOI] [PubMed] [Google Scholar]
- 16.Cockburn J, Reid AL, Sanson-Fisher RW. The process and content of general-practice consultations that involve prescription of antibiotic agents. Med J Aust. 1987;147(7):321–324. [PubMed] [Google Scholar]
- 17.Stevenson FA, Barry CA, Britten N, Barber N, Bradley CP. Doctor-patient communication about drugs: the evidence for shared decision making. Soc Sci Med. 2000;50(6):829–840. doi: 10.1016/s0277-9536(99)00376-7. [DOI] [PubMed] [Google Scholar]
- 18.Stange KC, Zyzanski SJ, Jaen CR, et al. Illuminating the 'black box'. A description of 4454 patient visits to 138 family physicians. J Fam Pract. 1998;46(5):377–389. [PubMed] [Google Scholar]
- 19.Sleath B, Roter D, Chewning B, Svarstad B. Asking questions about medication: analysis of physician-patient interactions and physician perceptions. Med Care. 1999;37(11):1169–1173. doi: 10.1097/00005650-199911000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. J Amer Med Assoc . 2002;288(6):756–764. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- 21.Deveugele M, Derese A, van den Brink-Muinen A, Bensing J, De Maeseneer J. Consultation length in general practice: cross sectional study in six European countries. Brit Med J . 2002;325(7362):472. doi: 10.1136/bmj.325.7362.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blumenthal D, Causino N, Chang YC, et al. The duration of ambulatory visits to physicians. J Fam Pract. 1999;48(4):264–271. [PubMed] [Google Scholar]
- 23.Kravitz RL, Bell RA, Azari R, Krupat E, Kelly-Reif S, Thom D. Request fulfillment in office practice: antecedents and relationship to outcomes. Med Care. 2002;40(1):38–51. doi: 10.1097/00005650-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Ware J. The use of psychological testing for treatment planning and outcomes assessment. 2 ed. Mahwah, NJ: Lawrence Album; 1999. SF-36 health survey; pp. 1227–1246. [Google Scholar]
- 25.Tarn DM. Dissertation Abstracts International, 69(9); 4955 B. (UMI No AAT3234390). Retrieved December 6, 2007 from Digital Dissertations Database. California: University of Los Angeles; 2006. What Do Doctors Communicate when Prescribing New Medications? [Google Scholar]
- 26.Tarn DM, Paterniti DA, Heritage J, Hays RD, Kravitz RL, Wenger NS. Physician communication about the cost and acquisition of newly prescribed medications. Am J Manag Care. 2006;12(11):657–664. [PubMed] [Google Scholar]
- 27.Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42(5):1871–1894. doi: 10.1111/j.1475-6773.2006.00689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Braddock CH, 3rd, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: time to get back to basics. J Amer Med Assoc . 1999;282(24):2313–2320. doi: 10.1001/jama.282.24.2313. [DOI] [PubMed] [Google Scholar]
- 29.Beasley JW, Hankey TH, Erickson R, et al. How many problems do family physicians manage at each encounter? A WReN study. Ann Fam Med. 2004;2(5):405–410. doi: 10.1370/afm.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Flocke SA, Frank SH, Wenger DA. Addressing multiple problems in the family practice office visit. J Fam Pract. 2001;50(3):211–216. [PubMed] [Google Scholar]
- 31.Tai-Seale M, Bramson R, Bao X. Decision or no decision: how do patient-physician interactions end and what matters? J Gen Intern Med. 2007;22(3):297–302. doi: 10.1007/s11606-006-0086-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alexander GC, Casalino LP, Meltzer DO. Patient-physician communication about out-of-pocket costs. J Amer Med Assoc . 2003;290(7):953–958. doi: 10.1001/jama.290.7.953. [DOI] [PubMed] [Google Scholar]
- 33.Alexander GC, Casalino LP, Tseng CW, McFadden D, Meltzer DO. Barriers to patient-physician communication about out-of-pocket costs. J Gen Intern Med. 2004;19(8):856–860. doi: 10.1111/j.1525-1497.2004.30249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bertakis KD. The communication of information from physician to patient: a method for increasing patient retention and satisfaction. J Fam Pract. 1977;5(2):217–222. [PubMed] [Google Scholar]
- 35.Schneider J, Kaplan SH, Greenfield S, Li W, Wilson IB. Better physician-patient relationships are associated with higher reported adherence to antiretroviral therapy in patients with HIV infection. J Gen Intern Med. 2004;19(11):1096–1103. doi: 10.1111/j.1525-1497.2004.30418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Piette JD, Heisler M, Krein S, Kerr EA. The role of patient-physician trust in moderating medication nonadherence due to cost pressures. Arch Intern Med. 2005;165(15):1749–1755. doi: 10.1001/archinte.165.15.1749. [DOI] [PubMed] [Google Scholar]
- 37.Shi CW, Asch SM, Fielder E, Gelberg L, Nichol MB. Consumer knowledge of over-the-counter phenazopyridine. Ann Fam Med. 2004;2(3):240–244. doi: 10.1370/afm.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wilcox CM, Cryer B, Triadafilopoulos G. Patterns of use and public perception of over-the-counter pain relievers: focus on nonsteroidal antiinflammatory drugs. J Rheumatol. 2005;32(11):2218–2224. [PubMed] [Google Scholar]
- 39.Brass EP. Changing the status of drugs from prescription to over-the-counter availability. N Engl J Med. 2001;345(11):810–816. doi: 10.1056/NEJMra011080. [DOI] [PubMed] [Google Scholar]
- 40.Francis SA, Barnett N, Denham M. Switching of prescription drugs to over-the-counter status: is it a good thing for the elderly? Drugs Aging. 2005;22(5):361–370. doi: 10.2165/00002512-200522050-00001. [DOI] [PubMed] [Google Scholar]
- 41.Goedhuys J, Rethans JJ. On the relationship between the efficiency and the quality of the consultation A validity study. Fam Pract. 2001;18(6):592–596. doi: 10.1093/fampra/18.6.592. [DOI] [PubMed] [Google Scholar]
- 42.Zyzanski SJ, Stange KC, Langa D, Flocke SA. Trade-offs in high-volume primary care practice. J Fam Pract. 1998;46(5):397–402. [PubMed] [Google Scholar]
- 43.Wilson AD, Childs S. Effects of interventions aimed at changing the length of primary care physicians' consultation. Cochrane Database Syst Rev. 2006;(1) doi: 10.1002/14651858.CD003540.pub2. CD003540. [DOI] [PubMed] [Google Scholar]
- 44.Wilson A, McDonald P, Hayes L, Cooney J. Health promotion in the general practice consultation: a minute makes a difference. Brit Med J. 1992;304(6821):227–230. doi: 10.1136/bmj.304.6821.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Roland MO, Bartholomew J, Courtenay MJ, Morris RW, Morrell DC. The "five minute" consultation: effect of time constraint on verbal communication. Br Med J (Clin Res Ed) 1986;292(6524):874–876. doi: 10.1136/bmj.292.6524.874. [DOI] [PMC free article] [PubMed] [Google Scholar]