Abstract
Ceramide induces cell death in response to many stimuli. Its mechanism of action, however, is not completely understood. Ceramide induces autophagy in mammalian cells maintained in rich media and nutrient permease downregulation in yeast. These observations suggested to us that ceramide might kill mammalian cells by limiting cellular access to extracellular nutrients. Consistent with this proposal, physiologically relevant concentrations of ceramide produced a profound and specific downregulation of nutrient transporter proteins in mammalian cells. Blocking ceramide-induced nutrient transporter loss or supplementation with the cell-permeable nutrient, methyl pyruvate, reversed ceramide-dependent toxicity. Conversely, cells became more sensitive to ceramide when nutrient stress was increased by acutely limiting extracellular nutrients, inhibiting autophagy, or deleting AMP-activated protein kinase (AMPK). Observations that ceramide can trigger either apoptosis or caspase-independent cell death may be explained by this model. We found that methyl pyruvate (MP) also protected cells from ceramide-induced, nonapoptotic death consistent with the idea that severe bioenergetic stress was responsible. Taken together, these studies suggest that the cellular metabolic state is an important arbiter of the cellular response to ceramide. In fact, increasing nutrient demand by incubating cells in high levels of growth factor sensitized cells to ceramide. On the other hand, gradually adapting cells to tolerate low levels of extracellular nutrients completely blocked ceramide-induced death. In sum, these results support a model where ceramide kills cells by inducing intracellular nutrient limitation subsequent to nutrient transporter downregulation.
Keywords: autophagy, caspase-independent cell death, daunorubicin, bioenergetics, sphingolipid
Ceramide and related sphingolipids play an evolutionarily conserved role in the cellular response to stress by regulating cell growth, differentiation, senescence, and survival (1). Uncovering the mechanisms by which ceramide regulates these processes is of paramount importance given the wide range of human diseases that result from altered ceramide metabolism including cancer, type II diabetes, and neurodegenerative disease (2–4). Ceramide plays a particularly well-established role in cancer. Decreasing cellular ceramide levels increases tumor growth and metastasis and can lead to multidrug resistance, a major cause of cancer treatment failure (2, 5, 6). The ability of ceramide to trigger programmed cell death in response to growth factor withdrawal, death receptor ligation, hypoxia, and chemotherapeutic drugs is likely integral to its role in suppressing cancer initiation and progression. Although many of the downstream, executioner pathways that are activated by ceramide are known, how ceramide triggers these pathways is not completely understood.
Autophagy, a process by which cells catabolize their own components, is induced in ceramide-treated cells (7–9). Autophagy has been conserved throughout evolution as a cytoprotective mechanism that sustains cells during periods of nutrient limitation. Conversely, autophagy has been shown to facilitate mammalian cell death under some conditions (10, 11). Increases or decreases in autophagy have been associated with many of the same pathological conditions that are characterized by altered ceramide metabolism suggesting a mechanistic link between ceramide, autophagy, and disease (3, 12). We report here that ceramide induces homeostatic autophagy in response to a bioenergetic crisis resulting from the rapid and profound downregulation of nutrient transporter proteins.
Results
Ceramide Triggers Homeostatic Autophagy.
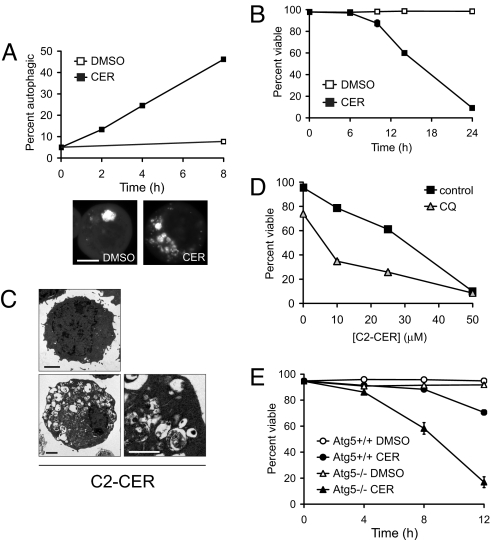
Ceramide triggers the starvation response of autophagy in rich media (7, 9). To determine whether ceramide-treated cells were dying because of or despite the induction of autophagy, we compared the kinetics of ceramide-induced cell death and autophagy. GFP-LC3 positive structures (autophagosomes) began to accumulate by 2 h and nearly half of the cells induced autophagy after 8 h of ceramide exposure (Fig. 1A). In contrast, ceramide-dependent cell death was not observed until >6 h after ceramide addition (Fig. 1B). Moreover, when apoptosis was blocked by Bcl-XL expression, ceramide-treated cells progressed to a severely autophagic phenotype (Fig. 1C). These studies demonstrate that ceramide-induced autophagy precedes and is not a consequence of cell death. Blocking autophagosome maturation with the lysosomal acidification inhibitor chloroquine (CQ) sensitized cells to ceramide exposure (Fig. 1D). Consistent with this, deletion of calpain, a protein required for autophagy, increases cellular sensitivity to ceramide (8). Similarly, fibroblasts lacking Atg5, a protein required for the induction of autophagy (13), were hypersensitive to ceramide (Fig. 1E). These results establish that autophagy is a homeostatic, protective response to increasing ceramide levels.
Fig. 1.
Ceramide triggers homeostatic autophagy. (A) Cells expressing GFP-LC3 were treated with DMSO or 50 μM C2-cer for the indicated intervals. Representative cells at 4 h are shown. Scale bar, 10 μm. (B) Viability of cells treated with DMSO or with 50 μM C2-cer. (C) Cells expressing Bcl-XL treated with DMSO or 50 μM C2-cer for 24 h were examined by electron microscopy. Scale bars, 2 μm or 1 μm. (D) Viability of cells treated for 24 h with C2-cer with or without 10 μM CQ. 3-MA was toxic even in the absence of ceramide (data not shown). (E) Viability of wild-type and Atg5−/− MEFs treated with 20 μM C2-cer in 1% FCS. Error bars, SD.
Ceramide produces cellular starvation in rich media by downregulating nutrient transporter proteins.
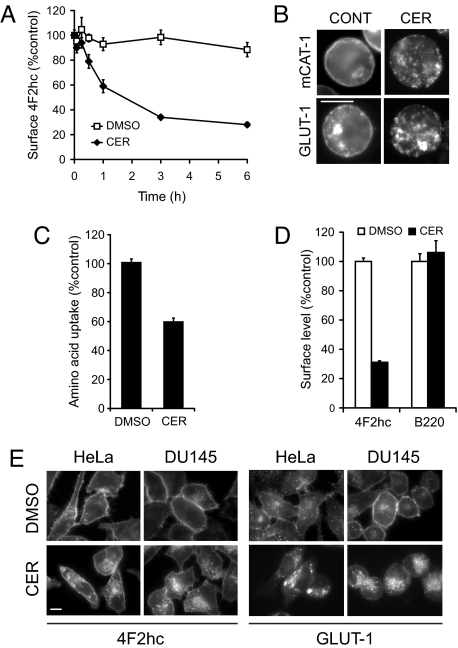
Heat-stressed yeast generate sphingoid bases related to ceramide that adaptively slow cell growth by downregulating nutrient permeases (14). We hypothesized that ceramide stimulates autophagy in mammalian cells by inducing nutrient transporter downregulation. As amino acid restriction is a well-established trigger for autophagy, we first examined amino acid transporter expression in ceramide-treated cells. Within minutes of its addition, ceramide decreased the surface expression of 4F2 heavy chain (4F2hc) (Fig. 2A). By 3 h, 4F2hc surface expression dropped to one-third of control levels. Another ubiquitously expressed amino acid transporter, mCAT-1, was also cleared from the cell surface by ceramide (Fig. 2B). These changes translated into a substantial decrease in amino acid uptake in ceramide-treated cells (Fig. 2C). The glucose transporter GLUT-1 was also downregulated by ceramide (Fig. 2B) demonstrating that this response was not limited to amino acid transporters.
Fig. 2.
Ceramide decreases nutrient transporter expression. (A) Surface 4F2hc was measured by flow cytometry in cells treated with DMSO or 25 μM C2-cer. Similar results were obtained with 50 μM C2-cer. (B) mCAT-1 and GLUT-1 expression in cells treated with DMSO or 50 μM C2-cer for 7 h (mCAT-1) or 18 h (GLUT-1, cells expressed Bcl-XL to maintain viability). Scale bar, 10 μm. (C) Amino acid uptake in cells treated with 25 μM C2-cer for 4 h. (D) Surface levels of 4F2hc and B220 were measured in cells expressing Bcl-XL 6 h after treatment with DMSO or 50 μM C2-cer. (E) 4F2hc and GLUT-1 localization in HeLa or DU145 cells treated with DMSO or 50 μM C2-cer for 9 h. Scale bar, 10 μm. Error bars: A, SEM; C and D, SD.
One explanation for the decreased nutrient transporter expression in cells exposed to ceramide is that dying cells have a reduced need for nutrients and therefore downregulate their transporter proteins. However, nutrient transporters were also lost in cells protected from apoptosis by Bcl-XL expression (Fig. 2D). Moreover, ceramide addition did not cause the nonspecific internalization of all plasma membrane proteins as surface levels of the B cell marker, B220, were not affected by ceramide treatment (Fig. 2D). Nutrient transporter proteins were also downregulated in ceramide-treated HeLa and DU145 cells (Fig. 2E). Taken together, these results suggest that ceramide triggers homeostatic autophagy by causing the downregulation of nutrient transporter proteins.
Ceramide Starves Cells to Death.
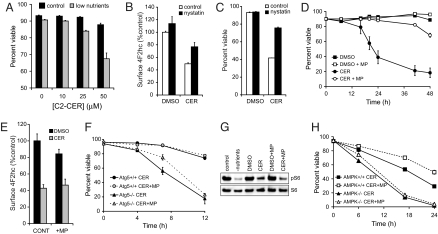
Consistent with this model, the ability of ceramide to induce cell death closely paralleled its ability to downregulate nutrient transporter proteins (supporting information (SI) Fig. S1 a and b). These experiments also showed that relatively low, sublethal concentrations of ceramide decreased nutrient transporter expression. Additional experiments demonstrated a nearly linear relationship between GLUT-1 expression and proliferation rate (Fig. S1c); this confirms that the degree of transporter loss in ceramide-treated cells is sufficient to cause nutrient stress, particularly when it is taken into account that ceramide decreases nutrient uptake much faster than RNAi would and affects multiple transporters. The synergistic effect of lowering extracellular nutrient levels and treating cells with ceramide (Fig. 3A) is also consistent with this hypothesis.
Fig. 3.
Ceramide induces a bioenergetic crisis subsequent to nutrient transporter downregulation. (A) Viability 7 h after C2-cer treatment in full nutrients (control) or in medium containing 0.5% the normal levels of amino acids and glucose. (B) Surface 4F2hc in cells treated for 4 h with DMSO, 25 μM C2-cer, or 25 μg/ml nystatin as indicated. (C) Viability of cells in B at 24 h. (D) Viability of cells treated with DMSO, 25 μM C2-cer, or 11 mM MP. (E) Surface expression of 4F2hc in cells treated for 6 h with DMSO, 25 μM C2-cer, or MP. (F) Viability of wild-type or Atg5−/− MEFs treated with 20 μM C2-cer in the presence or absence of MP. (G) Wild-type MEFs were withdrawn from nutrients or treated with 20 μM C2-cer for 3 h with or without MP supplementation and the levels of phospho- and total S6 protein evaluated. (H) Wild-type or AMPK−/− MEFs were treated with 20 μM C2-cer +/−MP in media containing 2% FCS. Error bars: D, SEM; A–C and E–H, SD.
If nutrient transporter downregulation kills ceramide-treated cells, then stabilizing these proteins at the cell surface should protect cells from ceramide. The molecules responsible for the specific internalization and degradation of nutrient transporter proteins have yet to be identified. However, several nutrient transporter proteins are internalized through raft-dependent processes (15, 16) and lipid raft organization is affected by ceramide (17). We found that the raft disrupting agent nystatin preserved both nutrient transporter surface expression (Fig. 3B) and viability (Fig. 3C) following ceramide treatment. As would be predicted by our model, nystatin failed to protect cells from ceramide in the absence of extracellular nutrients (data not shown). Ceramide is a direct activator of PP2A (2), a negative regulator of several signaling pathways that promote nutrient transporter expression (18). Okadaic acid, a PP2A inhibitor, also blocked nutrient transporter loss in the presence of ceramide (Fig. S1d). Because okadaic acid itself was toxic, we could not evaluate whether this increased nutrient transporter expression translated into increased cell survival.
If ceramide starves cells by downregulating nutrient transporters, then providing a transporter-independent nutrient should protect cells. Methyl pyruvate (MP) is a membrane-permeant form of pyruvate that can be oxidized in the tricarboxylic acid (TCA) cycle to produce ATP or used to generate amino acids, fatty acids, and nucleotides either directly or by way of TCA cycle intermediates. Supplementation with MP provided robust protection from ceramide-dependent cell death in multiple cell types (Fig. 3D, Fig. S2 a and b). Clonogenic survival assays confirmed that rescued cells excluding vital dyes were viable (Fig. S2c). In contrast to our results with MP, supplementation with membrane-impermeant sodium pyruvate or with additional glucose did not block ceramide-dependent cell death (Fig. S2d). Importantly, MP had no effect on nutrient transporter downregulation (Fig. 3E).
Consistent with our proposal that MP blocks ceramide-dependent death by serving as a membrane-permeable nutrient, MP slowed the induction of autophagy by ceramide (Fig. S2e). However, autophagy was required for the full protective effect of MP (Fig. 3F and Fig. S2f). This is likely because MP cannot substitute for all nutrients. For example, the essential amino acid leucine activates the nutrient-sensitive kinase mTOR (19). The decrease in mTOR activity in ceramide-treated cells was not corrected by MP (Fig. 3G). Interestingly, MP could not protect AMPK−/− MEFs (Fig. 3H). AMP-activated protein kinase (AMPK) is activated by bioenergetic stress and coordinates a homeostatic response (20). The lack of protection in AMPK−/− cells suggests that AMPK-dependent reprogramming of cellular bioenergetics was essential for MP-mediated rescue. Consistent with the idea that ceramide produces bioenergetic stress, AMPK−/− MEFs were more sensitive to ceramide than wild-type cells (Fig. 3H).
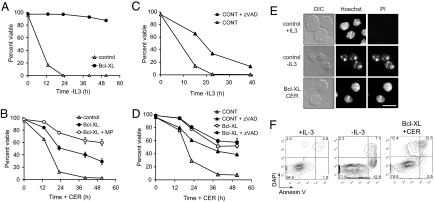
Ceramide induces caspase-independent cell death by decreasing nutrient transporter expression.
If ceramide starves cells, inhibiting apoptosis should not prevent cell death. In keeping with this model, Bcl-XL expression blocked growth factor withdrawal-induced apoptosis (Fig. 4A) but only delayed ceramide-dependent cell death (Fig. 4B). Bcl-XL-expressing cells underwent caspase-independent cell death (CICD) in response to ceramide. zVAD inhibited growth factor withdrawal-induced apoptosis (Fig. 4C) and protected cells from ceramide to a similar degree as Bcl-XL expression, but did not provide an additional survival advantage to Bcl-XL cells treated with ceramide (Fig. 4D). In addition, apoptotic morphology was not observed and no annexin V positive/DAPI negative cells were detected in ceramide-treated Bcl-XL-expressing cultures (Fig. 4 E and F). Because autophagy was protective (Fig. 1 D and E), these cells likely died necrotically. Ceramide-induced necrosis was also inhibited by MP supplementation consistent with the proposal that nutrient transporter loss was responsible (Fig. 4B).
Fig. 4.
Ceramide-induced nutrient transporter loss leads to CICD in the absence of apoptosis. (A) Viability of control or Bcl-XL-expressing FL5.12 cells following growth factor withdrawal. (B) Control or Bcl-XL-expressing cells were treated with 25 μM C2-cer with or without MP supplementation. (C) FL5.12 cells were withdrawn from IL-3 in the presence or absence of 50 μM zVAD. (D) The indicated cells were treated with 25 μM C2-cer with or without zVAD. (E) Nuclear morphology of FL5.12 cells maintained +/−IL-3 for 17 h or Bcl-XL-expressing cells treated with 25 μM C2-cer for 24 h. PI is a vital dye, Hoechst 33342 stains DNA in live cells. Scale bar, 10 μm. (F) Apoptosis was measured in control FL5.12 cells maintained +/−IL-3 for 9 h or in Bcl-XL-expressing cells treated with 25 μM C2-cer for 18 h. Error bars, SD.
Endogenous ceramide production downregulates nutrient transporter proteins.
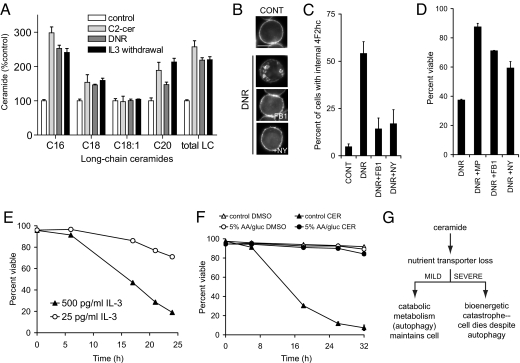
Because of their relatively high solubility in aqueous media, short-chain ceramides have been used extensively to study the effects of ceramide on cells. Exogenous, short-chain ceramides are converted into long-chain ceramides within the cell (21, 22). We performed HPLC ESI-MS/MS to evaluate whether the levels and types of long-chain ceramide produced in C2-ceramide-treated cells were similar to those produced when ceramide was generated endogenously (Fig. 5A). The increase in long-chain ceramides in cells treated with C2-ceramide was of similar magnitude to that observed in cells treated with the chemotherapeutic daunorubicin (DNR), a drug known to increase ceramide levels (5, 23, 24), and in response to growth factor withdrawal, also previously shown to increase ceramide levels (2). With all stimuli, the largest increase was in C16:0 ceramide. These results confirm that C2-ceramide treatment can be used to study the effects of ceramide generation in isolation from the other effects of chemotherapeutic agents or growth factor deprivation.
Fig. 5.
Ceramide kills cell through its effects on nutrient transporter expression. (A) Ceramide levels in FL5.12 cells treated with 25 μM C2-CER (3 h), 1 μM DNR (7 h), or withdrawn from IL-3 (9 h) were determined by HPLC ESI-MS/MS. Error bars, SD. Cells treated with 50 μM C2-cer produced twice as much ceramide as those treated with 25 μM. (B) 4F2hc staining in cells left untreated (CONT) or incubated with 1 μM DNR for 7 h and 100 μM FB1 or 25 μg/ml nystatin as indicated. Scale bar, 10 μm. (C) Quantification of B. Error bars, SEM. (D) Cells were treated for 13 h with 1 μM DNR in the absence or presence of MP, 100 μM FB1, or 25 μg/ml nystatin. Error bars, SD. (E) FL5.12 cells were grown in high levels of IL-3 or adapted to reduced levels and then treated with 25 μM C2-cer. Error bars, SD. (F) FL5.12 cells were adapted to grow in RPMI containing 10% FCS but 5% of the normal levels of amino acids and glucose and then treated with DMSO or 25 μM C2-cer. Error bars, SD. (G) Model for how ceramide affects cell growth and survival.
We next tested whether endogenously generated ceramide also decreased nutrient transporter expression. Treatment with bacterial sphingomyelinase (SMase) reduced 4F2hc surface expression by >50% and this effect was enhanced by the ceramidase inhibitor, D-MAPP (Fig. S3). Similarly, ceramide generated in response to DNR caused a dramatic relocalization of 4F2hc from the cell surface to the cytoplasm (Fig. 5 B and C). Both DNR-induced nutrient transporter loss (Fig. 5 B and C) and cell death (Fig. 5D) were inhibited by fumonisin B1 (FB1), a ceramide synthase inhibitor, demonstrating that ceramide generation was responsible for these effects. As with exogenous ceramide (Fig. 3 B and C), nystatin treatment prevented DNR-induced nutrient transporter loss (Fig. 5 B and C) and protected cells from DNR-dependent death to a similar degree as MP supplementation (Fig. 5D). Thus, nutrient transporter downregulation may make a previously unappreciated contribution to DNR-mediated toxicity.
Cellular bioenergetic state modulates sensitivity to ceramide.
Growth factors not only block apoptosis, but also drive cellular bioenergetics. To evaluate whether altering the metabolic demand for nutrients affects ceramide sensitivity, we adapted FL5.12 cells to grow in high levels (500 pg/ml) or low levels (25 pg/ml) of IL-3, conditions that produce highly glycolytic or less nutrient-dependent cells, respectively (25, 26). In keeping with a bioenergetic mechanism for ceramide-induced death, cells grown in low levels of IL-3 were much more resistant to ceramide than cells maintained in high levels of growth factors (Fig. 5E). We also shifted cellular bioenergetics by gradually adapting cells to tolerate low levels of extracellular nutrients. In contrast to the enhanced ceramide sensitivity seen in cells subjected to acute nutrient limitation (Fig. 3A), cells adapted to low nutrient levels exhibited a hormetic response and were completely insensitive to a lethal dose of ceramide (Fig. 5F). The finding that the metabolic state of the cell determines ceramide sensitivity supports our model that ceramide kills cells by inducing a bioenergetic catastrophe subsequent to nutrient transporter downregulation (Fig. 5G).
Discussion
We identify a novel mechanism for ceramide-induced death: starvation subsequent to nutrient transporter loss. This model provides a metabolic explanation for the increased sensitivity of cancer cells to ceramide (2). Cancer cells express constitutively active oncogenes that drive cellular bioenergetics and suppress autophagy (27). Moreover, tumor cells have deleted tumor suppressor proteins that facilitate metabolic quiescence. Thus, similar to what we observed in cells maintained in high levels of growth factors (Fig. 5E), transformed cells would be less able than normal cells to adapt to ceramide-induced nutrient transporter downregulation. The importance of basal metabolic state in determining ceramide sensitivity is further emphasized by the opposite consequences of acute (Fig. 3A) and gradual (Fig. 5F) extracellular nutrient restriction.
Blocking apoptosis in growth factor-deprived cells is sufficient to prevent cell death despite the fact that nutrient transporter proteins are also downregulated by growth factor withdrawal (Fig. 4A) (18). Why then is autophagy insufficient to meet the needs of ceramide-treated cells? One important difference is that, in growth factor withdrawn cells, nutrient transporter expression levels decrease relatively slowly. For example, 4F2hc levels decrease by ∼20% after 12 h of growth factor withdrawal (data not shown). By contrast, cells exposed to a dose of ceramide that causes cell death with similar kinetics lose 70% of their nutrient transporter proteins in 3 h (Fig. 2A). In addition, transcription and translation decline in growth factor withdrawn cells, decreasing metabolic demand. In ceramide-exposed cells, energy-consuming processes would only slow secondarily as a part of the response to starvation. In combination, these factors would make the bioenergetic insult associated with ceramide treatment more severe than that associated with growth factor deprivation.
These studies identify the molecules that specifically control nutrient transporter trafficking as key mediators of ceramide-dependent cell death. At present, the molecules that coordinate the turnover of most nutrient transporter proteins remain undefined, although our results suggest that lipid rafts (Fig. 3B) and PP2A (Fig. S1d) may be involved. Our work also highlights the fact that nutrient transporter expression should be evaluated in other cases where cells become autophagic despite an abundance of extracellular nutrients, particularly when the stimulus is known to generate ceramide. Additional studies will be required to determine whether nutrient transporter loss contributes to other ceramide-dependent phenotypes such as proliferative arrest, differentiation, and senescence. Given the central role of ceramide in type II diabetes and cancer (2, 4, 28), future studies may identify a role for ceramide-induced nutrient transporter downregulation in the pathogenesis of these diseases.
Materials and Methods
Reagents.
Chemicals: C2-CER, FB1, and D-MAPP (Biomol International); MP, CQ, and SMase (Sigma); PI and DAPI (Invitrogen); and DNR and nystatin (Calbiochem). Cells were pretreated with nystatin and FB1 for 30 min to 1 h. Antibodies: 4F2hc and B220 (BD Biosciences); HA (Roche Applied Science); GLUT-1 (Research Diagnostics Inc., note that the new lot of antibody does not recognize mouse GLUT-1); and S6 (Cell Signaling). Secondary antibodies: Invitrogen, Jackson Immunoresearch, or LI-COR. MIGR1 GFP-LC3 was kindly provided by Julian Lum. pcDNA3 HA-mCAT-1 was generously provided by Jim Cunningham. Lentiviral RNAi vectors were obtained from Open Biosystems.
Cell Culture.
FL5.12 cells were used in all experiments unless otherwise indicated. FL5.12 cells were maintained at 200,000–400,000 cells/ml in RPMI (Mediatech) supplemented with 10% FCS (HyClone), 350 pg/ml IL-3 (BD PharMingen), 10 mM Hepes (Mediatech), 55 μM β-mercaptoethanol (Sigma), antibiotics, and L-glutamine (Mediatech). Glucose and amino acid deficient FL5.12 medium was prepared from chemical components. HeLa, DU145, and MEFs were maintained in DMEM (Mediatech) supplemented with 10% FCS and antibiotics. MP was used at 11 mM, the concentration at which glucose is present in RPMI. Atg5-deficient MEFs were generously provided by Noboru Mizushima while AMPK+/+ and −/− cells were kindly sent by Rueben Shaw with permission from Keith Laderoute.
Amino Acid Uptake.
Cells were pretreated with DMSO or C2-CER for 2 h and then labeled for 2 h in complete medium supplemented with 1 μCi/ml tritiated amino acid mixture (MP Biomedicals). Cells were washed with ice-cold RPMI, lysed in RIPA, and tritium levels determined by scintillation counting. Tritium uptake was linear under the experimental conditions (R2 = 0.99).
Flow Cytometry.
4F2hc or B220 surface expression: 200,000–400,000 cells were washed (2% FCS and 0.05% NaN3 in PBS), incubated on ice for 10 min with 5 μg of mouse Ig (Jackson Immunoresearch) in blocking buffer (PBS containing 10% FCS and 0.05% NaN3) to block Fc receptors, and primary antibody was added. Secondary antibodies coupled to R-PE or APC were used. Annexin V-APC (eBioscience) was added to cells in HBSS with Ca2+ and Mg2+. Viability was determined by vital dye exclusion (PI or DAPI) or by the ability to form colonies after limiting dilution. Cells were analyzed on a BD LSR II flow cytometer.
Electron Microscopy.
FL5.12 cells were washed once with PBS then fixed in 2.5% glutaraldehyde/2.5% formaldehyde in 0.1 M sodium cacodylate buffer (Electron Microscopy Systems) and stored at 4 °C until embedding. Cells were postfixed with 1% osmium tetroxide, serially dehydrated, embedded in eponat12 resin, ultra-thin sections cut, mounted on grids, and stained with uranyl acetate and lead citrate. Samples were analyzed on a Philips CM10 transmission electron microscope.
Fluorescence Microscopy.
FL5.12 cells were fixed in 1% paraformaldehyde in PBS, washed in PBS containing 2% FCS and 0.03% saponin, and then incubated sequentially with primary and secondary antibodies in blocking buffer (PBS with 0.3% saponin and 10% FCS). HeLa and DU145 cells were grown on polylysine-coated coverslips, fixed in 4% paraformaldehyde, permeablized with 0.1% Triton X-100 or 0.3% saponin, blocked in 10% FCS, and stained. Cells were examined using a Nikon Eclipse TE2000 fluorescence microscope.
Mass Spectrometry.
Treated FL5.12 were washed three times with PBS and the cell pellet snap frozen. Mass spectrometry was performed as previously described (29). Ceramides were normalized to lipid phosphates.
Supplementary Material
Acknowledgments.
We thank Ralph DeBerardinis and Julian Lum for helpful discussions and reagents and Carrie Brachmann and David Fruman for their comments on the manuscript. This work was supported in part by National Institutes of Health Grants K08 CA100526 (to A.L.E.), and F31 CA126494 (to K.R.R.) and R01AG016583 and the Veteran Administration Research Enhancement Achievement Program (which supported L.J.S.).
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission. D.R.G. is a guest editor invited by the Editorial Board.
This article contains supporting information online at www.pnas.org/cgi/content/full/0802781105/DCSupplemental.
References
- 1.Obeid LM, Hannun YA. Ceramide, stress, and a “LAG” in aging. Sci Aging Knowledge Environ. 2003;39:PE27. doi: 10.1126/sageke.2003.39.pe27. [DOI] [PubMed] [Google Scholar]
- 2.Ogretmen B, Hannun YA. Biologically active sphingolipids in cancer pathogenesis and treatment. Nat Rev Cancer. 2004;4:604–616. doi: 10.1038/nrc1411. [DOI] [PubMed] [Google Scholar]
- 3.Schenck M, Carpinteiro A, Grassme H, Lang F, Gulbins E. Ceramide: Physiological and pathophysiological aspects. Arch Biochem Biophys. 2007;462:171–175. doi: 10.1016/j.abb.2007.03.031. [DOI] [PubMed] [Google Scholar]
- 4.Holland WL, et al. Inhibition of ceramide synthesis ameliorates glucocorticoid-, saturated-fat-, and obesity-induced insulin resistance. Cell Metab. 2007;5:167–179. doi: 10.1016/j.cmet.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 5.Morales A, et al. Pharmacological inhibition or small interfering RNA targeting acid ceramidase sensitizes hepatoma cells to chemotherapy and reduces tumor growth in vivo. Oncogene. 2007;26:905–916. doi: 10.1038/sj.onc.1209834. [DOI] [PubMed] [Google Scholar]
- 6.Selzner M, et al. Induction of apoptotic cell death and prevention of tumor growth by ceramide analogues in metastatic human colon cancer. Cancer Res. 2001;61:1233–1240. [PubMed] [Google Scholar]
- 7.Daido S, et al. Pivotal role of the cell death factor BNIP3 in ceramide-induced autophagic cell death in malignant glioma cells. Cancer Res. 2004;64:4286–4293. doi: 10.1158/0008-5472.CAN-03-3084. [DOI] [PubMed] [Google Scholar]
- 8.Demarchi F, et al. Calpain is required for macroautophagy in mammalian cells. J Cell Biol. 2006;175:595–605. doi: 10.1083/jcb.200601024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scarlatti F, et al. Ceramide-mediated macroautophagy involves inhibition of protein kinase B and up-regulation of beclin 1. J Biol Chem. 2004;279:18384–18391. doi: 10.1074/jbc.M313561200. [DOI] [PubMed] [Google Scholar]
- 10.Levine B, Yuan J. Autophagy in cell death: An innocent convict? J Clin Invest. 2005;115:2679–2688. doi: 10.1172/JCI26390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Debnath J, Baehrecke EH, Kroemer G. Does autophagy contribute to cell death? Autophagy. 2005;1:66–74. doi: 10.4161/auto.1.2.1738. [DOI] [PubMed] [Google Scholar]
- 12.Rubinsztein DC. The roles of intracellular protein-degradation pathways in neurodegeneration. Nature. 2006;443:780–786. doi: 10.1038/nature05291. [DOI] [PubMed] [Google Scholar]
- 13.Kuma A, et al. The role of autophagy during the early neonatal starvation period. Nature. 2004;432:1032–1036. doi: 10.1038/nature03029. [DOI] [PubMed] [Google Scholar]
- 14.Cowart LA, Obeid LM. Yeast sphingolipids: Recent developments in understanding biosynthesis, regulation, and function. Biochim Biophys Acta. 2007;1771:421–431. doi: 10.1016/j.bbalip.2006.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rubin D, Ismail-Beigi F. Distribution of Glut1 in detergent-resistant membranes (DRMs) and non-DRM domains: Effect of treatment with azide. Am J Physiol Cell Physiol. 2003;285:C377–C383. doi: 10.1152/ajpcell.00060.2003. [DOI] [PubMed] [Google Scholar]
- 16.Lu X, Silver J. Ecotropic murine leukemia virus receptor is physically associated with caveolin and membrane rafts. Virology. 2000;276:251–258. doi: 10.1006/viro.2000.0555. [DOI] [PubMed] [Google Scholar]
- 17.van Blitterswijk WJ, van der Luit AH, Veldman RJ, Verheij M, Borst J. Ceramide: Second messenger or modulator of membrane structure and dynamics? Biochem J. 2003;369:199–211. doi: 10.1042/BJ20021528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edinger AL. Controlling cell growth and survival through regulated nutrient transporter expression. Biochem J. 2007;406:1–12. doi: 10.1042/BJ20070490. [DOI] [PubMed] [Google Scholar]
- 19.Proud CG. Amino acids and mTOR signalling in anabolic function. Biochem Soc Trans. 2007;35:1187–1190. doi: 10.1042/BST0351187. [DOI] [PubMed] [Google Scholar]
- 20.Carling D. The AMP-activated protein kinase cascade–a unifying system for energy control. Trends Biochem Sci. 2004;29:18–24. doi: 10.1016/j.tibs.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Le Stunff H, et al. Recycling of sphingosine is regulated by the concerted actions of sphingosine-1-phosphate phosphohydrolase 1 and sphingosine kinase 2. J Biol Chem. 2007;282:34372–34380. doi: 10.1074/jbc.M703329200. [DOI] [PubMed] [Google Scholar]
- 22.Ogretmen B, et al. Biochemical mechanisms of the generation of endogenous long chain ceramide in response to exogenous short chain ceramide in the A549 human lung adenocarcinoma cell line. Role for endogenous ceramide in mediating the action of exogenous ceramide. J Biol Chem. 2002;277:12960–12969. doi: 10.1074/jbc.M110699200. [DOI] [PubMed] [Google Scholar]
- 23.Bose R, et al. Ceramide synthase mediates daunorubicin-induced apoptosis: An alternative mechanism for generating death signals. Cell. 1995;82:405–414. doi: 10.1016/0092-8674(95)90429-8. [DOI] [PubMed] [Google Scholar]
- 24.Ogretmen B, et al. Role of ceramide in mediating the inhibition of telomerase activity in A549 human lung adenocarcinoma cells. J Biol Chem. 2001;276:24901–24910. doi: 10.1074/jbc.M100314200. [DOI] [PubMed] [Google Scholar]
- 25.Vander Heiden MG, et al. Growth factors can influence cell growth and survival through effects on glucose metabolism. Mol Cell Biol. 2001;21:5899–5912. doi: 10.1128/MCB.21.17.5899-5912.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bauer DE, et al. Cytokine stimulation of aerobic glycolysis in hematopoietic cells exceeds proliferative demand. Faseb J. 2004;18:1303–1305. doi: 10.1096/fj.03-1001fje. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DeBerardinis RJ, Lum JJ, Hatzivassiliou G, Thompson CB. The biology of cancer: Metabolic reprogramming fuels cell growth and proliferation. Cell Metab. 2008;7:11–20. doi: 10.1016/j.cmet.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 28.Swanton C, et al. Regulators of mitotic arrest and ceramide metabolism are determinants of sensitivity to paclitaxel and other chemotherapeutic drugs. Cancer Cell. 2007;11:498–512. doi: 10.1016/j.ccr.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 29.Bielawski J, Szulc ZM, Hannun YA, Bielawska A. Simultaneous quantitative analysis of bioactive sphingolipids by high-performance liquid chromatography-tandem mass spectrometry. Methods. 2006;39:82–91. doi: 10.1016/j.ymeth.2006.05.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.