Abstract
Background/Objective:
To collect data from therapists regarding criteria for use and activities that individuals with C4–C5 tetraplegia can perform using a mobile arm support (MAS) that they otherwise could not. Reasons for nonuse, equipment design limitations, and therapist training needs were also studied.
Methods:
A modified Delphi approach was used to conduct an e-mail survey for which the response to each question was analyzed and used to formulate the subsequent question.
Setting:
Rehabilitation centers.
Participants:
Eighteen occupational therapists (most affiliated with 1 of the federally designated Model Spinal Cord Injury Systems) with extensive experience in the treatment of individuals with spinal cord injury (SCI).
Results:
The key physical prerequisite for successful use of the MAS was at least minimal strength of the deltoid and biceps muscles; 92% of respondents indicated that they would fit an MAS for motivated patients having very weak (<2/5) biceps and deltoid muscles. According to the therapists, 100% (n = 30) of their clients were able to perform at least 1 activity using a MAS that they were unable to perform without the device. These activities included (in descending frequency) eating, page turning, driving a power wheelchair, brushing teeth, keyboarding, writing, name signing, drawing, painting, scratching nose, playing board games, accessing electronic devices, drinking, and grooming. Equipment design limitations included increased wheelchair width and problems managing the arms while reclining.
Conclusions:
Mobile arm supports allow persons with C4–C5 tetraplegia to engage in activities that they otherwise cannot perform with their arms.
Keywords: Spinal cord injuries, Tetraplegia, Wheelchair, Mobile arm support, Assistive device, Guillain Barré, Syndrome, Amyotrophic lateral sclerosis, Spinal muscular atrophy, Duchenne muscular dystrophy, Peripheral neuropathy, Activities of daily living
INTRODUCTION
Mobile arm supports (MASs; aka ball-bearing feeders), metal mechanical devices mounted on the wheelchair that support weak upper limbs to enhance function, have been used since the 1950s (1). These devices allow individuals with significant proximal upper limb (UL) weakness to perform activities of daily living such as feeding (2), hygiene, grooming, power wheelchair (WC) propulsion, writing, and page turning, as well as facilitating gravity-eliminated exercise (1,3,4). Potential MAS users include individuals with tetraplegia, Guillain Barré syndrome, amyotrophic lateral sclerosis, spinal muscular atrophy, Duchenne muscular dystrophy, peripheral neuropathy, and other conditions presenting with severe shoulder weakness (5). Complete (ASIA A) (6) spinal cord injuries (SCIs) at the C3–C4 level may result in limited neurologic return in the C5 muscles, primarily deltoids and biceps. Distal UL musculature remains absent. Options for engaging in functional activities are limited to mouthstick use, high-tech assistive devices, and the use of MASs in conjunction with adaptive equipment.
The design of the MAS, a sturdy metal linkage system manufactured exclusively in the United States by JAECO Orthopedic (Hot Springs, AR), has been virtually unchanged for 50 years (Figure 1). With no competing products, consumers and therapists alike have had to make do with its flaws (7). Some of the design limitations include a significantly wider wheelchair profile, making it difficult to navigate doorways, parts that are difficult to attach and adjust, and the need for frequent and time-consuming readjustment. Design changes supported by grants from the National Institute on Disability and Rehabilitation Research (NIDRR) have resulted in the recent commercial production of the technologically updated JAECO/Rancho MultiLink MAS, shown in Figure 2 (JAECO Orthopedics). Another device, the newly developed Wilmington Robotic Exoskeleton (WREX; JAECO Orthopedics) (8) is being studied primarily with children who have arthrogryposis but may also prove beneficial for persons with SCI. In addition, the 2006 ARMON (RTD Het Dorp Rehabilitation Technology, Amhem, The Netherlands), (9) a new MAS designed in The Netherlands for individuals with spinal muscular atrophy, may also hold promise for individuals with SCI. The deltoid aid, a freestanding arm support apparatus, which consists of a frame of pulleys, springs, and slings, has been widely used in clinics for UL exercise and for function. Excellent for quick arm suspension in the clinic, this device does not attach to a wheelchair, takes much horizontal and vertical space, and is rarely supplied for outpatient use.
Figure 1. MAS.

Figure 2. JAECO/Rancho MultiLink MAS.
Despite the long history and wide potential application of MASs, little has been studied about them. The authors found few studies investigating the MAS in general and none about MAS use specific to tetraplegia. Haworth et al (5) conducted a retrospective survey on 124 MAS users with various diagnoses who were fitted with MASs from 1970 through 1976 in Oxford, England. After initial fitting, MASs were used for feeding (n = 84), writing (n = 52), page turning/reading (n = 37), hobbies/use at home (n = 32), and work/school/center activities (n = 17). They concluded that MASs are helpful devices, used primarily for specific activities rather than for general function. They noted that fitting and adjusting MASs is a complex, time consuming, and recurring task that requires strong commitment on the part of both therapist and user (5). Yasuda et al (10) examined the criteria for MAS use in patients with muscle disease, considering physical and psychosocial factors that contributed to successful use of the device. They concluded that successful use declined with elbow flexor strength of less than “poor” (2/5). MAS use was also successful when the only means of performing a desired task was by using the device (10). Garber and Gregorio (11) studied the patterns of prescription and use of upper limb devices in persons with tetraplegia. They counted the number of devices prescribed for patients during rehabilitation and studied the long-term use of these devices. Although the article does not provide specific information on MASs, the authors commented: “The devices retained in use most often were the more costly orthoses such as reciprocal orthoses and ball-bearing feeders” (11).
This study explores therapists' perspective on criteria for MAS use for persons with tetraplegia, anticipated functional goals and outcomes, and the reasons for nonprescription for individuals who otherwise meet the criteria for use. In addition, specific data are collected with regard to MAS design limitations and professional training needs.
In an SCI treatment guide for occupational therapists, Wilson et al (1) stated that, to warrant a MAS, a patient must have sufficient muscle weakness to benefit functionally and/or have limited muscular endurance. The guideline criteria for MAS use are:
Absent or weak elbow flexion (0 to fair* grades)
Absent to weak shoulder flexion and abduction (0 to fair* grades)
Absent or weak external rotation (0 to fair* grades)
Limited endurance for sustained upper extremity activity (Wilson et al, 1984, pg. 64). (*fair is equivalent to 3/5 MMT grade)
Baumgarten (12) and Atkins et al (13) have outlined the use of MASs for the tetraplegic population. They emphasize the merits of long-term MAS use for individuals with C4 tetraplegia with minimal C5 return, whose arms are essentially nonfunctional without the MAS. They also advocate temporary use for early initiation of functional activities and strengthening in a protected environment for those patients in which limited endurance impacts function or when further return of functional strength in the C5 muscle groups is anticipated. (12,13). Hill and Presperin (14) discuss the advantages of the MAS for people with tetraplegia for exercising select muscle groups, protecting weak muscles, and controlling musculoskeletal deformities. Strengthening is achieved by MAS adjustments that challenge individual muscles while assisting others while allowing for repetitive movements during functional activities (14).
The purpose of this study was to determine therapists' criteria for MAS use with tetraplegia, to identify which functional activities were successfully achieved, and to discover roadblocks to effective use of the MAS and therapist training needs.
METHODS
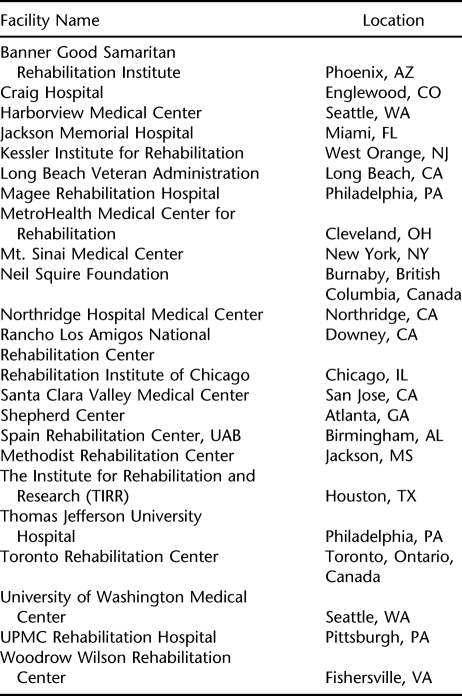
A modified Delphi approach was used to conduct an e-mail survey. This method was selected to allow geographically dispersed experts to answer a series of questions, and by their answers, influence the content and direction of subsequent inquiries. This format focuses on the issues identified by the participants and minimizes extraneous data collection. The process allowed the attention to be focused on the most relevant and important concerns of the participants. Participants in the survey were occupational therapists with extensive experience (3–25 years) in the treatment of SCI. Therapists were primarily identified from a list of OT/PT SCI specialists from the Regional SCI Centers, as listed in Table 1. Institutional review board approval was obtained for this project before conducting the research. The initial question was sent to 21 therapists, and 18 responded. Replies were analyzed, and the results led to the formulation of the subsequent question. Feedback regarding the results of each question was sent to the participants with the following question. During the course of the survey, the number of responses dropped to 8 (question 6). It is believed that this was because of the length of time between questions, which was a result of the time necessary to obtain enough responses (resending questions) and the time spent analyzing responses and formulating the question to follow. Staff turnover at some of the centers also accounted for lost participants. Data were gathered from September 2004 through October 2006.
Table 1.
Facilities From Which Participants Were Recruited
RESULTS
Question 1 asked the therapists to identify the physical prerequisite capabilities of individuals with SCI who could benefit from the use of MASs. Of the 23 questionnaires that were sent, 18 were returned. Sixteen of the respondents identified the ability to move the MAS as the primary necessary characteristic. The deltoid (n = 12) and biceps muscles (n = 11) were identified most frequently as key power sources necessary to operate a MAS, as well as the shoulder rotators (n = 6). Two respondents stated that strength of at least 2-/5 in these muscle groups was necessary for use, whereas 4 indicated that a minimum of 2/5 strength was needed (2-/5 muscle strength is defined as the capacity to move a part through a partial range of motion in a gravity-eliminated positon. Although not a standard manual muscle testing grade, its use is widely accepted by therapists to accurately assess and describe emerging volitional movement). Two clinicians indicated that deltoid and biceps strength of at least 3/5 was their minimal criterion for use, and 1 stated that 3/5 or less strength was a prerequisite for use. This respondent did not specify the minimum strength needed. Three respondents listed individuals with incomplete injuries such as central cord syndrome as good candidates. Intact sensation was identified as helpful but not critical. Two respondents stated that the patient must have functional passive range of motion. Other key factors identified as prerequisites to successful use included proper WC positioning (upright or only minimally reclined) with lateral trunk supports if needed (n = 5), upper extremity endurance (n = 5), no greater than minimally increased muscle tone/spasticity (n = 4), absence of severe pain (n = 2), and functional sitting tolerance (n = 2). In addition to these physical characteristics, motivation (n = 4), ability to accept the device (n = 2), intact cognition (n = 1), and available care providers (n = 1) were identified as necessary for successful use.
Questions 2 and 3 addressed the minimum physical capabilities of individuals with SCI necessary to engage in successful MAS use. Question 2 asked whether therapists would fit a MAS to a very weak but motivated patient (2/5 deltoid and biceps, 0 wrist extensors, absent sensation at C5 and below). Thirteen of 14 respondents indicated that they would prescribe a MAS for this type of patient. The respondent who would opt not to fit the patient cited patient frustration as the reason and would wait until the patient had more muscle strength to use an MAS. Reasons for fitting among the positive respondents included strengthening (55%), function (15%), strengthening and function (15%), and unspecified (15%).
Question 3 addressed fitting a patient with the same clinical picture as question 2 but with further strengthening no longer a goal, because of length of time since onset. Fourteen participants responded, and once again all but 1 indicated that such a patient would be a candidate for MAS use. The remaining therapist indicated cost to be the prohibitive factor, especially when considering the continued need for caregiver assistance. Of those affirming a MAS fitting for such a patient, all but 1 gave improvement in function as the reason for prescription. One respondent indicated WC mobility as a priority, and 1 did not specify a reason.
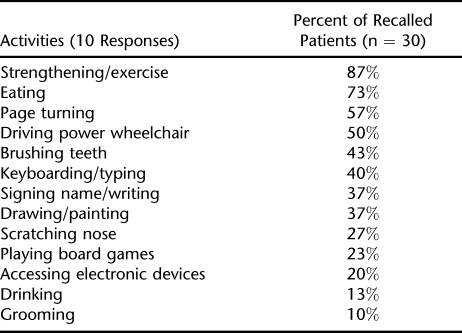
Question 4 asked the therapists to reflect back on the last 3 patients they had fitted with a MAS. For each patient, they were asked to select which activities from a provided list that the patient was able to do with the device that he/she was unable to do without the MAS. Data collected on 30 patients are shown in Table 2.
Table 2.
Functional Activities Performed With MAS
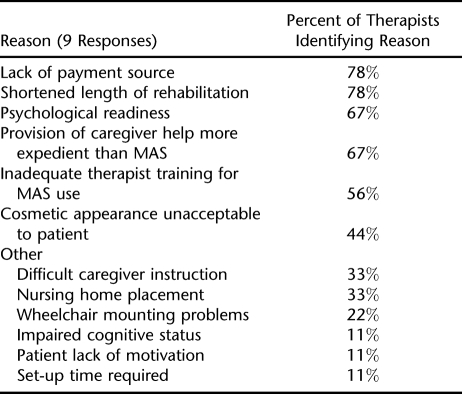
Question 5 instructed the therapists to identify reasons that MASs were not prescribed for patients who they believed could benefit from using the device. Nine clinicians responded to this question, as shown in Table 3.
Table 3.
Reasons for Nonprescription of MAS
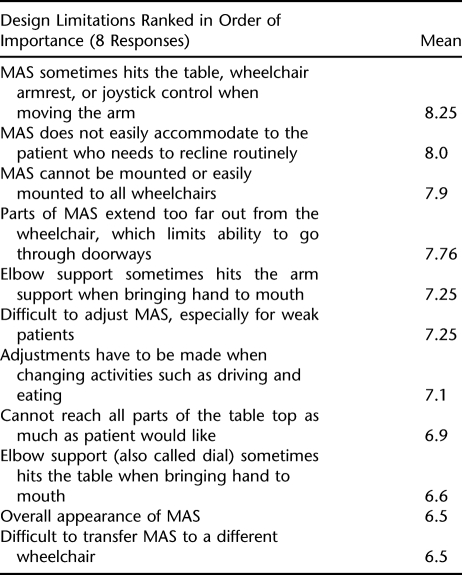
Question 6 identified 20 possible design limitations of the MAS that interfere with successful use. Therapists were asked to rate each item on a scale of 1 to 10, with 1 being less significant and 10 being very significant. Eight responses were received. Because the study was conducted from September 2004 through October 2006, the authors did not ask the respondents to differentiate between the newly designed JAECO/Rancho MultiLink MAS and the original JAECO MAS. The MultiLink MAS had only recently become commercially available, and most therapists were just beginning to learn about it and use it. The authors therefore assumed that most, if not all, answers referred to the original JAECO model. The most significant design limitations identified by the respondents are listed in Table 4. Increased wheelchair width and problems managing the ULs while reclining for pressure relief were identified as significant design limitations. The need for complex, frequent, and time-consuming adjustments and readjustments was another significant deterrent to successful use, particularly after hospitalization. Problems with the MAS or forearm support hitting the table, WC armrest, or WC joystick were identified as a significant interfering factor as well. Difficulty accessing multiple work heights without time-consuming adjustment to engage in a variety of functional activities was also identified as routinely problematic. Overall appearance was listed as a deterrent for some potential users.
Table 4.
Design Limitations
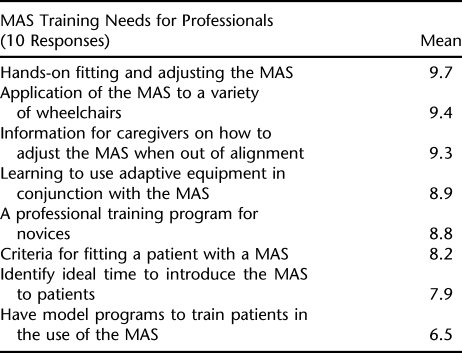
Question 7 asked therapists to rate 8 potential training needs for using the MAS for clients with SCI. Therapists were again asked to use a scale of 1 to 10, with 1 indicating not important and 10 indicating very important. Ten responses were received as shown in Table 5.
Table 5.
Training Needs
DISCUSSION
This study supports the practice of prescribing MASs for persons with tetraplegia who have significant proximal UL weakness. According to the therapists' accounts, MASs allow these individuals to engage in a strengthening program and perform functional activities with their arms that they were unable to do without the device instead of relying exclusively on head and neck motions, mouth sticks, or other assistive technology. This may explain the fact that, despite the cost, time spent fitting and adjusting the MAS, and the identified design limitations, therapists and consumers are frequently willing to overlook these obstacles in their efforts to maximize functional use of the ULs. Activities that weak individuals were able to perform only with a MAS include (in descending order of frequency) eating, page turning, driving a power WC, brushing teeth, keyboarding/typing, signing name/writing, drawing/painting, scratching nose, playing board games, accessing electronic devices, drinking, and grooming.
A chasm exists between the number of newly injured individuals who meet the criteria for MAS use each year and the number of MAS units that are ordered by the treating therapists. This is perhaps a function of the design limitations and inadequate therapist training in their application and use. Shorter rehabilitation stays may also be a contributing factor to nonuse.
Some of the MAS design limitations, including overall WC width (with MAS) and cosmetic appearance, have been improved on during the past decade with the introduction of the JAECO/Rancho MultiLink MAS (Figure 2). The authors measured the increase in wheelchair width caused by applying a MAS. Although the traditional JAECO MAS increased the overall width of the wheelchair by 8.5 in, the new JAECO/Rancho MultiLink MAS increased WC width by only 6 in. This difference is significant for many MAS users in the home setting, because they are potentially able to negotiate through doorway passages, which they might not have been able to with the traditional MAS. The new design is also credited with significantly decreasing fitting and adjustment time, as well as providing improved solutions for vertical movement (7). Sales trends reported by JAECO Orthopedic indicate that most consumers favor the new JAECO/Rancho MultiLink over the traditional JAECO MAS. According to JAECO's figures, 93 JAECO/Rancho MultiLink MASs were sold in 2003 (M. Conry, written communication, October 2006). Since then, sales have tripled, whereas sales of the traditional device have decreased (J. Reynolds, written communication, February 2008).
STUDY LIMITATIONS
The small number of participants does not allow for generalization of the data, and the reliance on therapists' recall and perceptions may have led to inaccuracies. Therapists' recall may be biased by either overly positive or negative perceptions about the MAS rather than on precise knowledge of individuals' successes or failures with the device that direct observations of device use would have provided.
CONCLUSION
Of the therapists surveyed, 92% would prescribe a mobile arm support for very weak (2-/5 deltoid and biceps) but motivated persons with high-level tetraplegia. The primary physical prerequisite for use was adequate muscle strength in the deltoids and biceps to power the MAS. According to therapists' recall of their last 3 MAS users, all (30 individuals) were able to perform 1 or more functions with the MAS that they were unable to perform without it. As in the study of Haworth et al (5) functional activities that were performed with the MAS included table top activities such as keyboarding and light self-care skills, with eating being the most frequent task. This study also identified the importance of the MAS for driving a power WC with the arm instead of using head/neck controls.
These positive findings support the continued use and development of the MAS for persons with tetraplegia. Further research efforts can be directed at reducing mechanical limitations of the device and at understanding users' habits and perceptions of the device. Further study can also include direct observations of MAS use.
Acknowledgments
No funds were received from JAECO Orthopedic Specialties, and none of the authors are employees or contractors of this company. Summary of e-mail communications from Mark Conry and Jason Reynolds of JAECO Orthopedic Specialties were printed with their permission. We thank Mark Corny, CEO, for his collaboration and immediate responsiveness, as well as for making new grant-developed products available to patients.
Footnotes
This study was funded by Grant H133E020732 from the National Institute on Disability and Rehabilitation Research, “Keep moving: RERC on Technologies to Enhance Mobility and Function for individuals with Spinal Cord Injury.”
REFERENCES
- Wilson DJ, McKenzie MW, Barber LM, Watson KL. Spinal Cord Injury: A Treatment Guide for Occupational Therapists. 2nd ed. Thorofare, NJ: Slack; 1984. [Google Scholar]
- Ford JR, Duckworth B. Physical Management for the Quadriplegic Patient. Philadelphia, PA: FA Davis; 1974. [Google Scholar]
- Thenn JE. Mobile Arm Support Installation and Use: A Guide for the Occupational Therapist. Brookfield, IL: Fred Sammons; 1975. [Google Scholar]
- Hill J. Spinal Cord Injury: A Guide to Functional Outcomes in Occupational Therapy. Rockville, MD: Aspen Publishers; 1986. [Google Scholar]
- Haworth R, Dunscombe S, Nichols PJR. Mobile arm supports: an evaluation. Rheumatol Rehabil. 1978;17:240–244. doi: 10.1093/rheumatology/17.4.240. [DOI] [PubMed] [Google Scholar]
- American Spinal Injury Association. International Standards for Neurological Classification of Spinal Injury Patients. Chicago, IL: American Spinal Injury Association; 2002. [Google Scholar]
- Landsberger S, Leung P, Vargas V, et al. Mobile arm supports: history, application, and work in progress. Top Spinal Cord Inj Rehabil. 2005;11:74–94. [Google Scholar]
- Rahman T, Sample W, Jayakumar S, et al. Passive exoskeletons for assisting limb movement. J Rehabil Res Dev. 2006;43:583–590. doi: 10.1682/jrrd.2005.04.0070. [DOI] [PubMed] [Google Scholar]
- Herder JL, Vrijlandt N, Antonides T, et al. Principle and design of a mobile arm support for people with muscular weakness. J Rehabil Res Dev. 2006;43:591–604. doi: 10.1682/jrrd.2006.05.0044. [DOI] [PubMed] [Google Scholar]
- Yasuda YL, Bowman K, Hsu JH. Mobile arm supports: criteria for successful use in muscle disease patients. Arch Phys Med Rehabil. 1986;67:253–256. [PubMed] [Google Scholar]
- Garber S, Gregorio T. Upper extremity assistive devices: assessment of use by spinal cord-injured patients with quadriplegia. Am J Occup Ther. 1990;44:126–131. doi: 10.5014/ajot.44.2.126. [DOI] [PubMed] [Google Scholar]
- Baumgarten JM. Upper extremity adaptations for the person with quadriplegia. In: Adkins H, editor. Spinal Cord Injury Clinics in Physical Therapy. New York: Churchill Livingston; 1985. pp. 219–241. [Google Scholar]
- Atkins MS, Clark D, Waters R. Upper limb orthoses. In: Lin VW, editor. Spinal Cord Medicine: Principles and Practice. New York: Demos Publishing; 2003. pp. 663–674. [Google Scholar]
- Hill J, Presperin J. Deformity control. In: Hill J, editor. Spinal Cord Injury: A Guide to Functional Outcomes in Occupational Therapy. Rockville, MD: Aspen Publishers; 1986. pp. 49–89. [Google Scholar]