Abstract
PURPOSE Although fatigue is a common presenting symptom in primary care and its course and outcomes often remain unclear, cohort studies among patients seeking care for fatigue are scarce. We therefore aimed to investigate patterns in the course of fatigue and relevant secondary outcomes in a large cohort of patients who sought care for a main symptom of fatigue.
METHODS We performed an observational cohort study in 147 primary care practices. Patients consulting their general practitioner for a new episode of fatigue were sent questionnaires at 1, 4, 8, and 12 months after baseline. We collected measures of fatigue, perceived health and functioning, absenteeism, psychological symptoms, and sleep using the Checklist Individual Strength, the 36-Item Short Form Health Survey, the Four-Dimensional Symptoms Questionnaire, and the Pittsburgh Sleep Questionnaire Inventory. Patients were classified into 4 subgroups based on fatigue severity scores over time. We assessed patterns in the course of all outcomes in these subgroups and in the total population, and tested changes over time and differences between subgroups.
RESULTS A total of 642 patients were enrolled in the study. Response rates during follow-up ranged between 82% and 88%. For 75% of the patients, 4 distinct groups could be discerned: 26% of patients had continuously high scores for fatigue, 17% had a fast recovery, 25% had a slow recovery, and 32% initially improved but then had a recurrence of fatigue. Patterns for the secondary outcomes of symptoms and functioning were all similar to the pattern for fatigue within each of the subgroups.
CONCLUSIONS The findings of this study suggest a longitudinal relationship between the severity of fatigue, impaired functioning, psychological symptoms, and poor sleep. Physicians should be aware that a substantial proportion of patients seeking care for fatigue have these additional health and psychosocial problems.
Keywords: Fatigue, prognosis, time course, recovery, sleep, physical functioning, primary care, practice-based research
INTRODUCTION
Fatigue is a nonspecific symptom and often the main one for which patients consult general practitioners; its prevalence ranges from 5% to 10%.1–4 Fatigue frequently remains the only (symptom) diagnosis in an episode of care.2 Serious functional impairment, psychological symptoms, and disturbed sleep often accompany fatigue.5–8 Knowledge about the course of fatigue and related problems in a heterogeneous primary care population is scarce, however, because most longitudinal studies on fatigued populations have been performed in highly selected groups, such as patients with chronic fatigue syndrome (CFS), postviral fatigue, or cancer.
Available studies on fatigue in primary care often concern a general population of primary care patients rather than patients seeking care for fatigue as a main symptom, have a follow-up limited to a single measurement rather than repeated measurements, or have a small sample size. Often, only patients with chronic fatigue have been included.9 We therefore investigated the course of fatigue in a large cohort of patients seeking care for a main symptom of fatigue using repeated measurements over a period of 1 year.
Additionally, as outcomes in available studies have been limited mainly to measures of fatigue, we assessed relevant secondary measures of daily functioning, work absence, psychological symptoms, and sleep. Our second aim was to examine whether the course of these secondary outcomes has a pattern similar to that of the fatigue itself.
METHODS
Design and Recruitment
The target population of our observational cohort study included adult patients who sought care for a main symptom of fatigue in Dutch primary care. We approached all general practitioners in several geographic areas, including rural and urban practices, and solo practitioners as well as group practices. From June 2005 to January 2006, 111 general practitioners and 57 trainees from 147 practices total recruited patients with a new episode of fatigue, meaning that the patient had not visited their physician for the same episode of fatigue at any time or for a different episode within the past 6 months. We excluded patients who were receiving or had received chemotherapy or radio-therapy in the preceding 3 months and women who were pregnant or less than 3 months postpartum. Eligible patients were informed about the study by their general practitioner and invited to participate. If the patients were interested, they were sent an information letter and the baseline questionnaire. Patients were enrolled when they returned a signed consent form. The participating patients completed questionnaires shortly after the consultation (baseline) and at 1, 4, 8, and 12 months after baseline. The study was approved by the Medical Ethical Committee of the VU University Medical Centre, Amsterdam.
Outcome Measures
Our primary outcome was fatigue. We measured the severity of fatigue at all time points with the Checklist Individual Strength (CIS), a 20-item questionnaire that has been validated in several fatigued populations.10 Items are scored on a 7-point Likert scale. A score of 34 or higher on the 8-item subscale of subjective fatigue has been used as a cutoff for severe fatigue.11,12
We assessed a variety of secondary outcomes. General health and functioning were measured at all time points with the 36-Item Short-Form Health Survey (SF-36), which includes subscales on physical functioning, physical role functioning, emotional role functioning, social functioning, bodily pain, mental health, vitality, and general health. The Dutch version has been validated in populations with various chronic diseases.13 Scores on all subscales range from 0 to 100, with higher scores indicating better functioning or health, or less pain. We measured absence from work or refraining from other activities during the past month due to the fatigue with a single question having response options of 0 days, 1 to 5 days, 6 to 10 days, 11 to 20 days, and greater than 20 days. In the descriptive analysis, answers were dichotomized into 0 days vs 1 or more days.
We measured psychological symptoms at baseline and after 1 year with the Four-Dimensional Symptoms Questionnaire (4DSQ). This scale has been validated in primary care populations and discerns levels of distress (16 items), somatization (16 items), depression (6 items), and anxiety (12 items).14 Scales for individual items range from 0 to 32 for distress and somatization, 0 to 12 for depression, and 0 to 24 for anxiety, with higher scores indicating more frequent psychological symptoms.
We measured sleep problems at baseline and after 12 months with the sleep subscale of the Symptom Checklist 90 (SCL-90), for which normative scores for the general population exist.15 This scale is scored on a 5-point Likert scale, with a total range of 3 to 15. Additionally, sleep quality was measured more extensively at the 1-month follow-up with the Pitts-burgh Sleep Questionnaire Inventory (PSQI) in those patients scoring above average on the SCL-90 subscale at baseline. The PSQI is a 19-item checklist validated in patients with depression and patients with sleep disorders. The list is used to evaluate general sleep quality and quantity, yielding a global score (range, 0–21) and 7 component scores.16 For both sleep scales, higher scores indicate poorer sleep.
Statistical Analysis
We used descriptive statistics to analyze the course of fatigue and secondary outcomes over the 12-month follow-up in the total study population. On the basis of the CIS severity score, we defined 4 subgroups of patients with a different course of fatigue over time: a chronic fatigue group having high scores on the CIS (>34) at all time points; a fast recovery group having low scores (≤34) at all follow-up measurements; a slow recovery group having low scores (≤34) after 4, 8, or 12 months; and a recurrent fatigue group having a recurrence of high fatigue scores after initial improvement. We assessed the course of fatigue and of the secondary outcomes over time for each of these 4 subgroups. To test the significance of changes in sleep and psychological symptom scores on the SCL-90 between baseline and 12 months, we performed dependent (paired) t tests and used analysis of variance to test differences in these measures between the 4 subgroups at baseline and after 12 months.
Changes over time in mean fatigue score in the total group were analyzed using multivariate analysis of variance (MANOVA) for repeated measures. To test changes over time and differences in the course of outcomes between the 4 fatigue subgroups, we used MANOVA for the continuous SF-36 outcomes and generalized estimating equations (GEE) for the dichotomous outcomes of refraining from daily activities. To assess whether differences between groups in fatigue and other measures were mainly explained by differences at baseline, analyses were also adjusted for baseline levels of outcome measures. For all analyses, we used an α of .05 to define statistical significance.
RESULTS
Recruitment and Response
The general practitioners invited 856 patients to participate in the study, of whom 642 (75%) consented to participate. Compared with nonparticipants, participants were on average 5 years older (P <.001) and more often female (73% vs 65%; P <.05). The number of patients remaining during follow-up was 562 (88%) at 1 and 4 months, 524 (82%) at 8 months, and 568 (88%) at 12 months.
Participating patients who did and did not subsequently complete any questionnaires did not differ significantly regarding sex or severity of fatigue at baseline; however, patients who completed the 4-, 8-, and 12-month questionnaires were on average 8 years older than the patients lost to follow-up (P <.001). Twenty-four patients completed only the baseline questionnaire, leaving 618 with at least 1 follow-up measurement.
The baseline characteristics of the 642 participating patients are presented in Table 1 ▶. The population was middle-aged and predominantly female and employed. The majority had been fatigued for more than 6 months before seeking care (58%) and had previously experienced an episode of fatigue (65%). Only small proportions had tried any treatment for their current fatigue.
Table 1.
Self-Reported Patient Characteristics at Baseline (N=642)
| Characteristic Social and demographic factors | No. (%) of Patients or Mean (SD) |
| Age, years | 41.8 (16.3) |
| Sex, female | 467 (73) |
| Married or living together | 411 (64) |
| Care for children | 242 (38) |
| Have paid work | 492 (77) |
| Educational level | |
| Primary | 40 (6) |
| Secondary | 483 (75) |
| College/university | 118 (18) |
| Fatigue | |
| Duration, months | |
| <1 | 44 (7) |
| 1–3 | 98 (16) |
| 3–6 | 115 (19) |
| 6–12 | 114 (18) |
| ≥12 | 252 (40) |
| Previous episode of fatigue | |
| No | 223 (35) |
| Yes, duration <6 months | 246 (38) |
| Yes, duration ≥6 months | 171 (27) |
| Treatment for fatigue | |
| Medicationa | 52 (8.1) |
| Psychologist or social worker | 26 (4.0) |
| Physical or manual therapy | 21 (3.3) |
| Diet | 9 (1.4) |
| Alternative or complementary | 31 (4.8) |
| Other treatment or care | 21 (3.3) |
a Various supplements (eg, vitamins, iron) (16 patients), benzodiazepines (7), antidepressants (5), thyroid hormones (4), pain medication (5), other medication for other indications (10), and missing or not clear (7).
Fatigue
The time course of fatigue is shown in Table 2 ▶. At baseline, 90% of all patients scored higher than 34 on the CIS severity scale, indicating that they were severely fatigued. Scores decreased significantly between all successive time points, but the decrease was greatest between baseline and 1 month.
Table 2.
Time Course of Fatigue and Other Symptoms in the Study Population
| Measure [Reference Score for General Population]a | Baseline (n=642) | 1 Month (n=562) | 4 Months (n=562) | 8 Months (n=524) | 12 Months (n=568) |
| Fatigue, CIS score | |||||
| Severity score, mean (SD) [17] | 45.8 (8.4) | 38.3 (11.2) | 35.4 (12.3) | 33.5 (13.4) | 32.0 (13.5) |
| Score >34, No. (%) (range, 8–56) | 578 (90) | 369 (66) | 324 (57) | 257 (49) | 259 (46) |
| Total score, mean (SD) [42] (range, 20–140) | 96 (20) | 84 (24) | 78 (26) | 75 (28) | 71 (28) |
| Health status, SF-36 score, mean (SD) | |||||
| Physical functioning [83] | 74 (23) | 78 (22) | 81 (20) | 82 (20) | 83 (20) |
| Physical role functioning [76] | 35 (36) | 51 (40) | 59 (40) | 62 (40) | 66 (40) |
| Emotional role functioning [82] | 64 (41) | 72 (39) | 75 (37) | 76 (38) | 77 (37) |
| Social functioning [84] | 60 (22) | 68 (22) | 71 (23) | 73 (22) | 76 (23) |
| Bodily pain [75] | 72 (24) | 77 (24) | 78 (24) | 78 (25) | 79 (24) |
| Mental health [77] | 63 (18) | 68 (18) | 68 (18) | 69 (18) | 71 (18) |
| Vitality [69] | 36 (16) | 46 (18) | 50 (19) | 53 (21) | 56 (21) |
| General health [71] | 60 (19) | 60 (20) | 61 (19) | 62 (21) | 63 (21) |
| Absent from work, No. (%)b | 238 (38) | 184 (33) | 138 (25) | 118 (23) | 109 (20) |
| Refrained from other activities, No. (%)b | 352 (56) | 281 (50) | 219 (40) | 212 (41) | 205 (38) |
| Psychological symptoms, 4DSQ score, mean (SD); % with elevated scorec | |||||
| Distress | 13.3 (7.4); 61 | – | – | – | 8.7 (7.0); 35 |
| Somatization | 11.0 (6.2); 48 | – | – | – | 7.9 (6.1); 30 |
| Depression | 1.7 (2.6); 24 | – | – | – | 1.0 (2.1); 15 |
| Anxiety | 2.5 (3.6); 10 | – | – | – | 1.7 (3.1); 5.3 |
| Sleep, SCL-90 score, mean (SD); % with score above meand | 7.0 (3.1); 65 | – | – | – | 6.4 (2.7); 58 |
CIS = Checklist Individual Strength; SF-36 = 36-Item Short Form Health Survey; 4DSQ = Four-Dimensional Symptoms Questionnaire; SCL-90=Symptom Checklist 90.
a Reference scores based on 53 healthy subjects for the CIS10 and a random sample of 1,742 people from the general population for the SF-36.17
b Percentages based on available data for each time point.
c On the 4DSQ, scores are elevated if they exceed 10 for distress, 2 for depression, 7 for anxiety, and 10 for somatization.
d On the sleep scale of the SCL-90, scores are elevated if they exceed 5 for women and 4 for men.
Because of missing values at 1 or more time points, 136 (22%) of 618 patients with follow-up data could not be classified into any of the 4 subgroups. Of the remaining 482 patients, 123 (26%) fell into the chronic fatigue subgroup, 83 (17%) patients fell into the fast recovery subgroup, 122 (25%) fell into the slow recovery subgroup, and 154 (32%) fell into the subgroup with recurrent fatigue.
Patients who could not be classified into 1 of the groups did not differ regarding sex, baseline severity of fatigue, or baseline levels of other outcomes, but were on average 8 years younger (95% confidence interval, −11 to −4.9) and slightly more often reported absence from work at baseline (44% vs 35% among those who could be classified; Pearson χ2, P <.05).
Figure 1 ▶ shows the mean scores of fatigue severity for the 4 subgroups having a different course of fatigue. The subgroups had distinct patterns of fatigue severity that differed significantly, both before and after adjustment for the severity of fatigue at baseline. On closer inspection, the duration of fatigue already differed at baseline; the proportions of patients with chronic fatigue (duration >6 months) at presentation ranged from 68% in the chronic fatigue group to 37% in the fast recovery group (Pearson χ2, P <.001).
Figure 1.
Course of the severity of fatigue in the 4 subgroups.
Note: 123 patients had a chronic course, 83 had a fast recovery, 122 had a slow recovery, and 154 had recurrent fatigue.
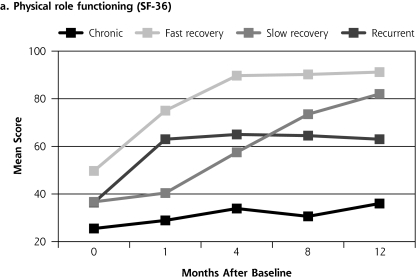
Perceived Health and Functioning
Changes in perceived health over time, assessed with the SF-36, were significant for all subscales (MANOVA, P <.001) (Table 2 ▶). Apart from vitality, baseline mean scores were particularly low for physical role functioning, social functioning, and emotional role functioning compared with the scores in a Dutch reference population.17 These areas, however, were also the areas showing the largest improvement over the year. Changes over time across the 4 subgroups for all SF-36 scales had a pattern similar to that of fatigue, with the most distinct differences evident between the chronic fatigue and fast recovery subgroups, as exemplified in Figure 2a ▶. Differences were also significant (P <.001) on all subscales after adjustment for baseline scores.
Figure 2.
Course of functional outcomes in the 4 subgroups.
SF-36 = 36-Item Short Form Health Survey.
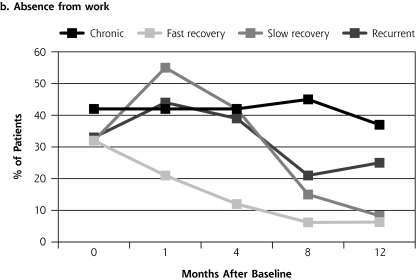
Missed Work or Other Activities
As shown in Table 2 ▶, a considerable proportion of patients reported that they were absent from work or refrained from other activities at least 1 day in the past month because of their fatigue. Figures 2b and 2c ▶ show the proportion of patients reporting these outcomes by subgroup. The patterns were in part similar to those for severity of fatigue and the SF-36 scores, with these outcomes more often reported in the chronic fatigue subgroup during the entire year of follow-up and least often reported in the fast recovery group. The (more heterogeneous) groups with slow recovery or a recurrent course of fatigue also had more work absence in the first months after consulting the general practitioner. Most of these absences, however, were of relatively short duration (1–5 days). Differences over time between subgroups were significant (GEE analyses, P <.001) for both outcomes (absence from work and refraining from other activities), before and after adjustment for differences in baseline values.
Psychological Symptoms
Whereas a minority of patients had symptoms of depression or anxiety, a substantial proportion had elevated scores on the 4DSQ distress and somatization scales at baseline, and one-third still had elevated scores after 1 year (Table 2 ▶). Mean scores on all scales had decreased significantly from baseline after 12 months (P <.01).
Among the 4 subgroups, differences in the change in psychological symptoms were significant for distress and somatization (P <.001), but not for depression (P = .34) and anxiety (P = .19) (Table 3 ▶). Mean changes between baseline and the 12-month follow-up were largest in patients having a fast or slow recovery in terms of fatigue severity. Changes over time were small and not significant for depression and anxiety in the chronic fatigue subgroup.
Table 3.
Measures of Psychological Symptoms (4DSQ) and Sleep (SCL-90) in the 4 Subgroups at Baseline and After 12 Months
| Baseline | 12 Months | ||||
| Measure by Subgroup | Score, Mean (SD) | Elevated Score,aNo. (%) | Score, Mean (SD) | Elevated Score,aNo. (%) | Mean Change in Score (95% CI) |
| Distress | |||||
| Chronic course | 15.8 (7.3) | 93 (76) | 13.1 (7.7) | 70 (58) | 2.6 (1.4–3.9) |
| Fast recovery | 9.5 (6.4) | 33 (40) | 3.7 (3.9) | 6 (7.3) | 5.8 (4.5–7.2) |
| Slow recovery | 13.8 (7.3) | 78 (64) | 7.3 (5.6) | 31 (26) | 6.5 (5.3–7.7) |
| Recurrent fatigue | 12.7 (6.9) | 90 (59) | 9.1 (6.2) | 56 (38) | 3.6 (2.5–4.8) |
| Somatization | |||||
| Chronic course | 13.6 (6.9) | 79 (64) | 11.6 (6.6) | 68 (57) | 2.1 (1.1–3.0) |
| Fast recovery | 8.1 (5.0) | 21 (25) | 3.8 (3.6) | 4 (4.9) | 4.3 (3.3–5.2) |
| Slow recovery | 11.2 (5.4) | 63 (52) | 6.7 (5.4) | 21 (17) | 4.5 (3.7–5.4) |
| Recurrent fatigue | 10.5 (5.6) | 67 (44) | 7.9 (5.3) | 43 (29) | 2.6 (1.7–3.4) |
| Depression | |||||
| Chronic course | 2.6 (3.2) | 46 (37) | 2.2 (3.0) | 43 (36) | 0.41 (–0.1 to 0.9)b |
| Fast recovery | 0.9 (2.1) | 13 (16) | 0.1 (0.5) | 1 (1.2) | 0.83 (0.4–1.3) |
| Slow recovery | 1.4 (2.2) | 28 (23) | 0.5 (1.3) | 8 (6.6) | 0.82 (0.5–1.2) |
| Recurrent fatigue | 1.3 (2.0) | 29 (19) | 0.8 (2.0) | 16 (11) | 0.48 (0.2–0.8) |
| Anxiety | |||||
| Chronic course | 3.4 (4.3) | 20 (16) | 2.9 (3.9) | 13 (11) | 0.53 (−0.1 to 1.2)b |
| Fast recovery | 1.1 (1.9) | 2 (2.4) | 0.4 (1.0) | 0 (0) | 0.66 (0.3–1.0) |
| Slow recovery | 2.6 (3.4) | 13 (11) | 1.4 (2.3) | 4 (3.3) | 1.20 (0.7–1.7) |
| Recurrent fatigue | 2.3 (3.5) | 15 (9.7) | 1.8 (3.4) | 8 (5.4) | 0.50 (0.0–1.0) |
| Sleep | |||||
| Chronic course | 7.4 (3.4) | 80 (66) | 7.5 (3.1) | 90 (73) | 0.16 (−0.6 to 0.3)b |
| Fast recovery | 6.0 (2.8) | 43 (52) | 5.1 (2.1) | 36 (43) | 0.88 (0.2–1.5) |
| Slow recovery | 7.7 (3.3) | 91 (75) | 6.2 (2.4) | 67 (55) | 1.50 (1.0–2.0) |
| Recurrent fatigue | 6.7 (3.0) | 96 (62) | 6.5 (2.6) | 91 (59) | 0.25 (−0.2 to 0.7)b |
4DSQ = Four-Dimensional Symptoms Questionnaire; SCL-90 = Symptom Checklist 90; CI = confidence interval.
Note: 123 patients had a chronic course, 83 had a fast recovery, 122 had a slow recovery, and 154 had recurrent fatigue.
a Cutoffs for elevations of 4DSQ scores and SCL-90 scores are as indicated in Table 2 ▶.
b Not significant.
Sleep
Two-thirds of all patients scored above average on the SCL-90 sleep scale at baseline (Table 2 ▶) and were asked to complete the PSQI after 1 month (response rate, 86%; n = 359). Results on the PSQI showed that these patients had high scores for sleep latency (time awake before sleeping), daytime dysfunction, sleep disturbances, and subjective sleep quality; nevertheless, 63% of this group said they slept “reasonably well” (Table 4 ▶). One-third of the cohort had global scores of 5 or higher, however, indicating that they had poor overall quality of sleep. Most patients reported that they slept more than 6 hours per night. Differences between subgroups were significant for each domain of the PSQI and again most pronounced between the chronic fatigue and fast recovery subgroups. After 12 months, SCL-90 sleep scores, which differed between subgroups both at baseline and after 12 months (P <.001) improved but were still above average in 58% of all patients (Table 2 ▶).
Table 4.
Sleep (PSQI Scores) at 1 Month After Baseline, for Total Study Population and by Subgroup
| Measure | Total (n=359) | Chronic Course | Fast Recovery | Slow Recovery | Recurrent Fatigue | PValuea |
| PSQI score | ||||||
| Total, mean (SD) | 7.23 (3.55) | 9.17 (3.96) | 4.60 (2.19) | 7.53 (3.23) | 6.48 (3.15) | <.001 |
| No. (%) with score >5 | 229 (62) | 64 (82) | 9 (21) | 63 (70) | 50 (55) | |
| Sleep quality | ||||||
| Reasonably well, % | 63 | 53 | 82 | 57 | 70 | <.001b |
| Very well, % | 5.5 | 3.8 | 11 | 5.6 | 4.4 | |
| Time awake before sleeping | ||||||
| Mean (SD), minutes | 30 (31) | 36 (38) | 18 (14) | 31 (30) | 26 (24) | <.01 |
| >30 minutes, % | 26 | 37 | 9.3 | 27 | 19 | |
| Sleep duration | ||||||
| Mean (SD), hours | 7.10 (1.34) | 6.64 (1.36) | 7.33 (1.03) | 7.15 (1.41) | 7.18 (1.22) | <.05 |
| >6 hours, % | 88 | 75 | 98 | 89 | 90 | |
| Sleep efficiencyc | ||||||
| Mean (SD), % | 84 (16) | 78 (16) | 89 (10) | 84 (16) | 85 (18) | <.01 |
| >85%, % | 53 | 41 | 67 | 48 | 54 | |
| Use sleep medication, % | 20 | 29 | 4.5 | 22 | 19 | <.05 |
PSQI = Pittsburgh Sleep Questionnaire Inventory.
Note: to enable a more straightforward interpretation, component scores are not presented.
a For difference between groups, determined by analysis of variance.
b For well (reasonably well and very well) vs bad.
c Sleep time as a percentage of total bedtime.
DISCUSSION
In this cohort of primary care patients consulting general practitioners because of fatigue, the proportion of patients who were severely fatigued decreased from 90% to 46% over 1 year. Among patients with complete follow-up, we identified 4 subgroups that had distinctly different courses of fatigue. Patterns in these subgroups showed that a reduction in severity of fatigue over time was associated with improvements in functioning, sleep, and psychological symptoms.
Fatigue
The proportion of patients showing improvement during the year is in line with previous studies of smaller cohorts of patients seeking care for fatigue3,18,19 Strikingly, a majority of patients were already chronically or recurrently fatigued when they visited the general practitioner, and most reported severe fatigue. Our study is the first to use the CIS in primary care, and compared with other populations, our patients had mean scores at baseline that were close to those of patients with CFS or multiple sclerosis.10 Because we recruited patients when they were seeking care for their fatigue, the fatigue may have been relatively severe at presentation. The improvement of symptoms after consultation may therefore partly represent regression to the “mean level of fatigue” after the visit or the self-limiting course of fatigue, or may be the result of effective care by the general practitioner.
Functioning
Patients in this study often had impairment due to fatigue, as was evident from both their low levels of role functioning and the substantial proportions who missed work or other daily activities because of their fatigue. Baseline SF-36 scores were comparable to those recently found among primary care patients who had a main symptom of unexplained fatigue.20 The impact of fatigue on perceived health and functioning was not as strong as that reported for patients with CFS; scores for pain, general health, and physical functioning were closer to those for the general population than those for CFS patients.17,21 In the group with persistent fatigue, most SF-36 scores were in between those of the total population and those of CFS patients.
Psychological Symptoms
The co-occurrence of fatigue and psychological symptoms has been reported extensively in various populations including primary care patients, the general population, and employees.22–28 In our cohort study, all 4 subgroups had a similar pattern of psychological symptom scores, with more patients reporting symptoms of distress and somatization and fewer scoring above the threshold for depression or anxiety. Patients with a chronic course of fatigue had mean 4DSQ scores that were comparable to those of primary care patients seeking care for psychosocial problems, although our population had somewhat lower anxiety scores. This finding demonstrates the severity of psychological problems in patients with chronic fatigue. In the total population, mean scores after 1 year were similar to those in a random sample of general practitioner consulters.14 The association between the number of experienced somatic symptoms and psychiatric comorbidity has been reported before.27,29 Our findings could reflect several processes, such as physical expression of psychological symptoms, or a heightened awareness of physical symptoms.30–32 These processes are difficult to measure in large, epidemiologic studies. It should be noted that existing somatization scales, such as the one we used, represent only the number of experienced symptoms; therefore, we cannot ascertain the origin of these symptoms or patients’ perceptions of the symptoms.
Sleep
To our knowledge, this is the first time that sleep quality has been measured in fatigued primary care patients. The different patterns we found in our subgroups indicate that sleep quality deserves attention in patients visiting the general practitioner for fatigue. Sleep scores in the chronic fatigue subgroup were generally similar to those reported for depressed patients.16,33,34 In our fatigued population, sleep quality was more of a problem than sleep duration. This finding corresponds to observed PSQI patterns in patients with CFS35 and to the results of a population-based study, in which fatigue was predicted by sleep quality and psychological symptoms rather than by amount of sleep.5 Both in populations reporting vital exhaustion and in populations reporting major stress or depression, a poorer quality of sleep has been reported by patients who show a reduction of slow wave sleep, which represents the stages of deep sleep and is thought to mark a restorative process.36–38
From our descriptive study, we cannot infer causal relationships, nor can we disentangle temporal associations. Our findings might nevertheless indicate that the experience of physical and psychological symptoms, including fatigue, and poorer sleep, perceived health, and functioning, may interact and reinforce one another, adding to the continuation of symptoms and impaired functioning.
Strengths and Weaknesses
To our knowledge, this is the first time that a large primary care cohort of fatigued patients has been followed up with repeated measurements over a period of 12 months. Because of our large sample size and use of repeated measurements of multiple outcomes, we were able to distinguish between patients with different patterns of fatigue and associated variables over time. We aimed to describe trajectories of fatigue. Longitudinal analyses assessing individual associations over time are needed to give more insight into the temporal relationships between variables.
The completion rates of 82% to 88% during follow-up were high, and there was no selective dropout in terms of severity of fatigue. Participants and completers were somewhat older than nonparticipants and noncompleters, and this difference may have slightly influenced our findings, as older patients may more often report chronic fatigue. We did not find any differences in mean age between the 4 subgroups with a different course of fatigue, however. Participants were more often female than nonparticipants, and women more often had a chronic or recurrent course of fatigue compared with men (60% vs 48%), while women were less likely to have a fast recovery (14% vs 28%). The generalizability of our results might not be optimal for younger and male patients; however, it is unlikely that the associations we found between different outcomes were influenced by this selective nonparticipation.
Implications for General Practice and Further Research
Our findings indicate that among patients consulting their general practitioner because of fatigue, most of the improvement in both fatigue and functional impairment occurred 1 to 4 months after baseline; however, only 17% of patients showed a fast recovery. More than half of the patients (58%) had a course of recurrent or chronic fatigue with minimal changes over the year. To identify these patients, general practitioners should pay attention to patients’ functioning, psychological symptoms, and sleep quality, especially in patients who are already chronically fatigued at presentation. Additionally, future research is needed to analyze the predictive value of these and other characteristics, which may provide handholds for more targeted treatment of fatigue in primary care.
Acknowledgments
We thank all patients and general practitioners who participated in this study, and the reviewers of the manuscript for their useful comments.
Annals Journal Club selection—see inside back cover or http://www.annfammed.org/AJC/.
Conflicts of interest: none reported
REFERENCES
- 1.Cullen W, Kearney Y, Bury G. Prevalence of fatigue in general practice. Ir J Med Sci. 2002;171(1):10–12. [DOI] [PubMed] [Google Scholar]
- 2.Kenter EG, Okkes IM, Oskam SK, Lamberts H. Tiredness in Dutch family practice. Data on patients complaining of and/or diagnosed with “tiredness.” Fam Pract. 2003;20(4):434–440. [DOI] [PubMed] [Google Scholar]
- 3.Nelson E, Kirk J, McHugo G, et al. Chief complaint fatigue: a longitudinal study from the patient’s perspective. Fam Pract Res J. 1987; 6(4):175–188. [PubMed] [Google Scholar]
- 4.Sharpe M, Wilks D. Fatigue. BMJ. 2002;325(7362):480–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lavidor M, Weller A, Babkoff H. How sleep is related to fatigue. Br J Health Psychol. 2003;8(Pt 1):95–105. [DOI] [PubMed] [Google Scholar]
- 6.Russo J, Katon W, Clark M, Kith P, Sintay M, Buchwald D. Longitudinal changes associated with improvement in chronic fatigue patients. J Psychosom Res. 1998; 45(1 Spec No):67–76. [DOI] [PubMed] [Google Scholar]
- 7.Skapinakis P, Lewis G, Mavreas V. One-year outcome of unexplained fatigue syndromes in primary care: results from an international study. Psychol Med. 2003;33(5):857–866. [DOI] [PubMed] [Google Scholar]
- 8.Solomon L, Nisenbaum R, Reyes M, Papanicolaou DA, Reeves WC. Functional status of persons with chronic fatigue syndrome in the Wichita, Kansas, population. Health Qual Life Outcomes. 2003;1(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nijrolder I, Van der Horst HE, Van der Windt DAWM. Prognosis of fatigue. A systematic review. J Psychosom Res. 2008;64(4):335–349. [DOI] [PubMed] [Google Scholar]
- 10.Vercoulen JHMM, Alberts M, Bleijenberg G. De checklist individual strength (CIS). Gedragstherapie. 1999;32(2):131–136. [Google Scholar]
- 11.Huibers MJ, Bultmann U, Kasl SV, et al. Predicting the two-year course of unexplained fatigue and the onset of long-term sickness absence in fatigued employees: results from the Maastricht Cohort Study. J Occup Environ Med. 2004;46(10):1041–1047. [DOI] [PubMed] [Google Scholar]
- 12.Servaes P, van der WS, Prins J, Verhagen S, Bleijenberg G. Fatigue in disease-free cancer patients compared with fatigue in patients with chronic fatigue syndrome. Support Care Cancer. 2001;9(1):11–17. [DOI] [PubMed] [Google Scholar]
- 13.Van der Zee K, Sanderman R, Heyink J. De psychometrische kwaliteiten van de MOS-36-item Short Form health Survey [SF-36] in een Nederlandse populatie. T Soc Gezondheidsz. 1993;71:183–191. [Google Scholar]
- 14.Terluin B, van Marwijk HW, Ader HJ, et al. The Four-Dimensional Symptom Questionnaire (4DSQ): a validation study of a multidimensional self-report questionnaire to assess distress, depression, anxiety and somatization. BMC Psychiatry. 2006;6:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arrindell WAEJ. SCL-90: Handleiding bij een Multidimensionele Psychopathologie-Indicator. Lisse, the Netherlands: Swets Test Services; 1986.
- 16.Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 17.Aaronson NK, Muller M, Cohen PD, et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 1998;51(11):1055–1068. [DOI] [PubMed] [Google Scholar]
- 18.Cathebras PJ, Robbins JM, Kirmayer LJ, Hayton BC. Fatigue in primary care: prevalence, psychiatric comorbidity, illness behavior, and outcome. J Gen Intern Med. 1992;7(3):276–286. [DOI] [PubMed] [Google Scholar]
- 19.Ridsdale L, Evans A, Jerrett W, Mandalia S, Osler K, Vora H. Patients with fatigue in general practice: a prospective study. BMJ. 1993;307(6896):103–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koch H, van Bokhoven MA, Riet GT, van der WT, Dinant GJ, Bindels PJ. Demographic characteristics and quality of life of patients with unexplained complaints: a descriptive study in general practice. Qual Life Res. 2007;16(9):1483–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Komaroff AL, Fagioli LR, Doolittle TH, et al. Health status in patients with chronic fatigue syndrome and in general population and disease comparison groups. Am J Med. 1996;101(3):281–290. [DOI] [PubMed] [Google Scholar]
- 22.Bultmann U, Kant I, Kasl SV, Beurskens AJ, Van den Brandt PA. Fatigue and psychological distress in the working population: psychometrics, prevalence, and correlates. J Psychosom Res. 2002;52(6):445–452. [DOI] [PubMed] [Google Scholar]
- 23.De Waal MWM, Arnold IA, Spinhoven P, Eekhof JAH, Van Hemert AM. The reporting of specific physical symptoms for mental distress in general practice. J Psychosom Res. 2005;59(2):89–95. [DOI] [PubMed] [Google Scholar]
- 24.Hickie IB, Hooker AW, Hadzi-Pavlovic D, Bennett BK, Wilson AJ, Lloyd AR. Fatigue in selected primary care settings: sociodemographic and psychiatric correlates. Med J Aust. 1996;164(10):585–588. [DOI] [PubMed] [Google Scholar]
- 25.Pawlikowska T, Chalder T, Hirsch SR, Wallace P, Wright DJ, Wessely SC. Population based study of fatigue and psychological distress. BMJ. 1994;308(6931):763–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ridsdale L, Evans A, Jerrett W, Mandalia S, Osler K, Vora H. Patients who consult with tiredness: frequency of consultation, perceived causes of tiredness and its association with psychological distress. Br J Gen Pract. 1994;44(386):413–416. [PMC free article] [PubMed] [Google Scholar]
- 27.Skapinakis P, Lewis G, Mavreas V. Unexplained fatigue syndromes in a multinational primary care sample: specificity of definition and prevalence and distinctiveness from depression and generalized anxiety. Am J Psychiatry. 2003;160(4):785–787. [DOI] [PubMed] [Google Scholar]
- 28.Wijeratne C, Hickie I, Brodaty H. The characteristics of fatigue in an older primary care sample. J Psychosom Res. 2007;62(2):153–158. [DOI] [PubMed] [Google Scholar]
- 29.Simon G, Gater R, Kisely S, Piccinelli M. Somatic symptoms of distress: an international primary care study. Psychosom Med. 1996;58(5):481–488. [DOI] [PubMed] [Google Scholar]
- 30.Lipowski ZJ. Somatization: the concept and its clinical application. Am J Psychiatry. 1988;145(11):1358–1368. [DOI] [PubMed] [Google Scholar]
- 31.Nakao M, Barsky AJ. Clinical application of somatosensory amplification in psychosomatic medicine. Biopsychosoc Med. 2007;1(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rief W, Broadbent E. Explaining medically unexplained symptoms—models and mechanisms. Clin Psychol Rev. 2007;27(7):821–841. [DOI] [PubMed] [Google Scholar]
- 33.Doi Y, Minowa M, Uchiyama M, et al. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000;97(2–3):165–172. [DOI] [PubMed] [Google Scholar]
- 34.Germain A, Caroff K, Buysse DJ, Shear MK. Sleep quality in complicated grief. J Trauma Stress. 2005;18(4):343–346. [DOI] [PubMed] [Google Scholar]
- 35.Neu D, Mairesse O, Hoffmann G, et al. Sleep quality perception in the chronic fatigue syndrome: correlations with sleep efficiency, affective symptoms and intensity of fatigue. Neuropsychobiology. 2007;56(1):40–46. [DOI] [PubMed] [Google Scholar]
- 36.Cartwright RD, Wood E. Adjustment disorders of sleep: the sleep effects of a major stressful event and its resolution. Psychiatry Res. 1991;39(3):199–209. [DOI] [PubMed] [Google Scholar]
- 37.Riemann D, Berger M, Voderholzer U. Sleep and depression—results from psychobiological studies: an overview. Biol Psychol. 2001;57(1–3):67–103. [DOI] [PubMed] [Google Scholar]
- 38.van Diest R, Appels WP. Sleep physiological characteristics of exhausted men. Psychosom Med. 1994;56(1):28–35. [DOI] [PubMed] [Google Scholar]