Abstract
Objective:
To present recommendations for the prevention, recognition, and treatment of environmental cold injuries.
Background:
Individuals engaged in sport-related or work-related physical activity in cold, wet, or windy conditions are at risk for environmental cold injuries. An understanding of the physiology and pathophysiology, risk management, recognition, and immediate care of environmental cold injuries is an essential skill for certified athletic trainers and other health care providers working with individuals at risk.
Recommendations:
These recommendations are intended to provide certified athletic trainers and others participating in athletic health care with the specific knowledge and problem-solving skills needed to address environmental cold injuries. Each recommendation has been graded (A, B, or C) according to the Strength of Recommendation Taxonomy criterion scale.
Keywords: environmental physiology, hypothermia, frostbite, frostnip, chilblain, pernio, immersion foot, trench foot
Cold injuries are a common result of exposure to cold environments during physical activity or occupational pursuits. Many individuals engage in fitness pursuits and physical activity year-round in environments with cold, wet, or windy conditions (or a combination of these), thereby placing themselves at risk of cold injuries. The occurrence of these injuries depends on the combination of 2 factors: low air or water temperatures (or both) and the influence of wind on the body's ability to maintain a normothermic core temperature, due to localized exposure of the extremities to cold air or surfaces. Cold injuries and illnesses occur in a wide range of physically active individuals, including military personnel, traditional winter-sport athletes, and outdoor-sport athletes, such as those involved in running, cycling, mountaineering, and swimming. Traditional team sports such as football, baseball, softball, soccer, lacrosse, and track and field have seasons that extend into late fall or early winter or begin in early spring, when weather conditions can increase susceptibility to cold injury. Reported rates of hypothermia and frostbite include 3% to 5% of all injuries in mountaineers and 20% of all injuries in Nordic skiers.1 Cold injury frequency in military personnel is reported to range from 0.2 to 366 per 1000 exposures.1–6
As the scope of physical activity participation broadens (eg, extreme sports, adventure racing) and environments with the potential for extreme weather conditions become more accessible, a review of cold injury physiology, prevention, recognition, treatment, and management is warranted. Clinicians practicing in settings or geographic regions that predispose individuals to cold injury must be aware of these risks and implement strategies to prevent cold injuries and to minimize them when they occur.
Purposes
This position statement includes a review of available literature, definitions of cold injuries, and a set of recommendations that will allow certified athletic trainers (ATs) and other allied health and medical providers to
Identify and employ prevention strategies to reduce cold-related injuries and illnesses in the physically active.
Describe factors associated with cold-related injuries and illnesses.
Provide on-site first aid and immediate care of cold-related injuries and illnesses.
Understand the thermoregulatory and physiologic responses to cold.
Identify groups with unique concerns related to cold exposure.
Definitions of Cold Injuries
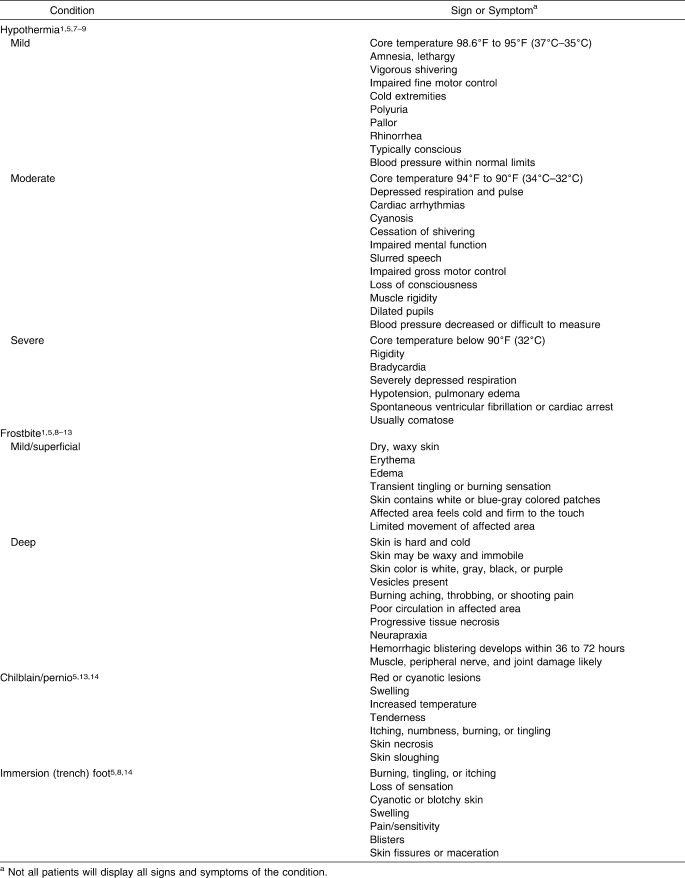
Cold injuries are classified into 3 categories: decreased core temperature (hypothermia), freezing injuries of the extremities, and nonfreezing injuries of the extremities. Each scenario and its characteristic condition(s) will be described. A summary of the signs and symptoms of these injuries and illnesses is found in Table 1, with images of the skin conditions displayed in Figures 1 through 3.
Table 1.
Signs and Symptoms of Cold-Related Injuries
Figure 1. Frostbite.

Figure 2. Chilblain. Photograph reprinted with permission: ©Christoph U. Lehmann, MD, Dermatlas; http://www.dermatlas.org.

Figure 3. Immersion (trench) foot.

Hypothermia
Traditionally, hypothermia is defined as a decrease in core body temperature below 95°F (35°C). Hypothermia is classified as mild, moderate, or severe, depending upon measured core temperature. Information in the literature varies slightly as to which core temperatures are assigned to which degree of hypothermia, but in this paper, we will use the following definitions. Mild hypothermia is a core temperature of 95°F (35°C) to 98.6°F (37°C). Moderate hypothermia is a core temperature of 90°F (32°C) to 94°F (34°C). Severe hypothermia is a core temperature below 90°F (32°C).1,7–9 Each level of hypothermia has characteristic signs and symptoms, although individuals respond differently, and not every hypothermic person exhibits all signs and symptoms. Therefore, a detailed assessment is appropriate in all cases of potential cold injury. Hypothermia is most likely to occur with prolonged exposure to cold, wet, or windy conditions (or a combination of these) experienced during endurance events, outdoor team sports (eg, soccer, football), mountaineering, hiking, and military maneuvers and in occupations that require long periods outdoors or in unheated spaces (eg, public safety, building trades, transportation).
Frostbite and Frostnip
Frostbite is actual freezing of body tissues. It is a localized response to a cold, dry environment, yet moisture from sweating may exacerbate frostbite due to increased tissue cooling. Similar to hypothermia, frostbite has stages, delineated by the depth of tissue freezing and resulting in frostnip, mild frostbite, or severe frostbite.1,8–13 Frostbite develops as a function of the body's protective mechanisms to maintain core temperature. Warm blood is shunted from cold peripheral tissues to the core by vasoconstriction of arterioles, which supply capillary beds and venules to the extremities and face, especially the nose and ears. Frostbite progresses from distal to proximal and from superficial to deep. As the temperature of these areas continues to decrease, cells begin to freeze. Damage to the frostbitten tissue is due to electrolyte concentration changes within the cells, resulting in water crystallization within the tissue. For cells to freeze, the tissue temperature must be below 28°F (−2°C).8–13
Frostnip, the mildest form of cold injury to the skin, is a precursor to frostbite. It can occur with exposure of the skin to very cold temperatures, often in combination with windy conditions. It can also occur from skin contact with cold surfaces (eg, metal, equipment, liquid). With frostnip, only the superficial skin is frozen; the tissues are not permanently damaged, although they may be more sensitive to cold and more likely, with repeated exposures, to develop frostnip or frostbite.8–13 Mild frostbite involves freezing of the skin and adjacent subcutaneous tissues; extracellular water freezes first, followed by cell freezing. Severe frostbite is freezing of the tissues below the skin and the adjacent tissues, which can include muscle, tendon, and bone.8–13
Chilblain (pernio)
Chilblain, also known as pernio, is an injury associated with extended exposure (1–5 hours) to cold, wet conditions. Chilblain is an exaggerated or uncharacteristic inflammatory response to cold exposure. Prolonged constriction of the skin blood vessels results in hypoxemia and vessel wall inflammation; edema in the dermis may also be present. Chilblain can occur with or without freezing of the tissue. The hands and feet are most commonly affected, but chilblain of the thighs has also been reported.14 Situations in which this can happen include alpine sports, mountaineering, hiking, endurance sports, and team sports in which footwear and clothing remain wet for prolonged periods due to water exposure or sweating.
Chilblain severity is time and temperature related. The higher the temperature of the water (generally ranging from 32°F [0°C] to 60°F [16°C]), the longer the duration of exposure required to develop chilblain. Time of exposure is usually measured in hours or even days, rather than the minutes or hours associated with frostbite. Chilblain and immersion foot (see below) occur in similar environments, but the former is a more superficial injury and can develop in a shorter time period than the latter.13,14
Immersion (trench) Foot
Immersion foot typically occurs with prolonged exposure (12 hours to 4 days) to cold, wet conditions, usually in temperatures ranging from 32°F to 65°F (0°C–18°C). This condition affects primarily the soft tissues, including nerves and blood vessels, due to an inflammatory response that results in high levels of extracellular fluid. The most common mechanism for developing immersion foot is the continued wearing of wet socks or footwear (or both).8,14
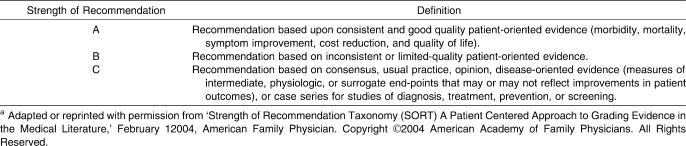
Evidence Classification
In this position statement, we present recommendations using an evidence-based review and the Strength of Recommendation Taxonomy (SORT) criterion scale (Table 2) proposed by the American Academy of Family Physicians.15 The recommendations are given a grade of A, B, or C based upon evidence using patient or disease-oriented outcomes (treatments or practices). Little outcomes-based research using randomized clinical trials on cold injury has been performed due to ethical constraints regarding standards of care and difficulties procuring large sample groups. These limitations should be weighed when assessing specific recommendations.
Table 2.
Strength of Recommendation Taxonomy (SORT)a
Recommendations
Recommendations are presented to help ATs and other health care providers minimize risks to the health and safety of physically active individuals exposed to cold environments and provide effective immediate care when needed. Individual responses to cold vary physiologically with combinations of cold, wet, and windy conditions as well as clothing insulation, exposure time, and other nonenvironmental factors. Therefore, these recommendations do not guarantee complete elimination of cold-related injuries but may decrease risk. The National Athletic Trainers' Association (NATA) promotes the following approaches for prevention, recognition, and treatment of cold-related injuries.
Prevention
Perform a comprehensive, physician-supervised, preparticipation medical screening to identify athletes with a previous history of cold injury and athletes predisposed to cold injury based upon known risk factors (Table 3). This preparticipation examination should include questions pertaining to a history of cold injury and problems with cold exposure16 and should be performed before planned exposures to conditions that may lead to cold injury. Evidence Category: C
Identify participants who present with known risk factors (Table 3) for cold injury and provide increased monitoring of these individuals for signs and symptoms.5 Evidence Category: C
Ensure that appropriately trained personnel are available on-site at the event and are familiar with cold injury prevention, recognition, and treatment approaches.5 Evidence Category: C
Educate athletes and coaches concerning the prevention, recognition, and treatment of cold injury and the risks associated with activity in cold environments.5 Evidence Category: C
Educate and encourage athletes to maintain proper hydration and eat a well-balanced diet. These guidelines are especially imperative for activities exceeding 2 hours.17–19 Consistent fluid intake during low-intensity exercise is necessary to maintain hydration in the presence of typical cold-induced diuresis.20–22 Athletes should be encouraged to hydrate even if they are not thirsty, as evidence suggests the normal thirst mechanism is blunted with cold exposure.23 Evidence Category: C
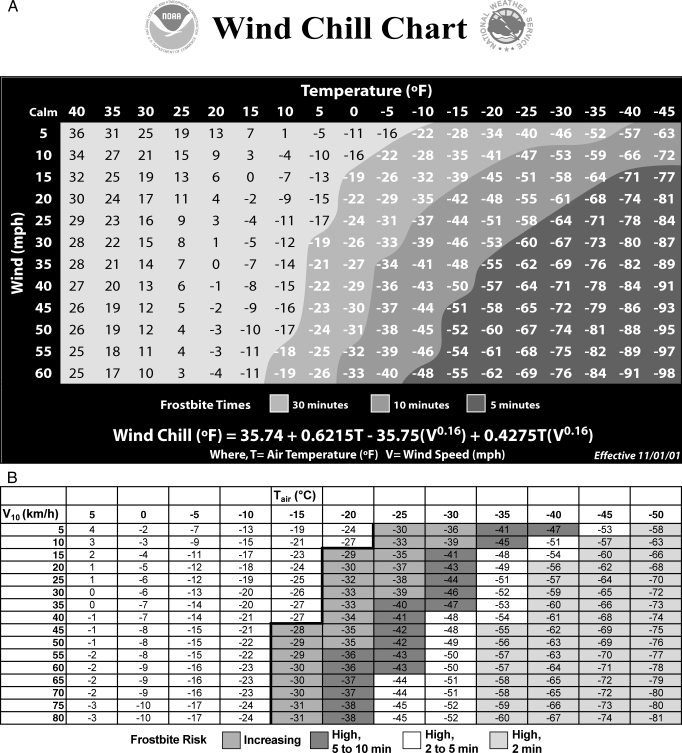
Develop event and practice guidelines that include recommendations for managing athletes participating in cold, windy, and wet conditions.24,25 The influence of air temperature and wind speed conditions should be taken into account by using wind-chill guidelines.26,27 Risk management guidelines (Table 3, Figure 4) can be used to make participation decisions based upon the prevailing conditions. Participation decisions depend upon the length of anticipated exposure and availability of facilities and interventions for rewarming if needed. Modify activity in high-risk conditions to prevent cold injury. Monitor athletes for signs and symptoms and be prepared to intervene with basic treatment. Also monitor environmental conditions before and during the activity and adjust activities if weather conditions change or degenerate.28,29 Evidence Category: C
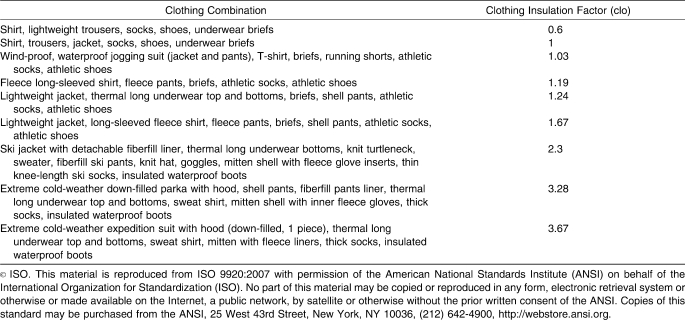
Clothing should provide an internal layer that allows evaporation of sweat with minimal absorption, a middle layer that provides insulation, and a removable external layer that is wind and water resistant and allows for evaporation of moisture. Examples of various clothing ensembles are found in Table 4. Toes, fingers, ears, and skin should be protected when wind-chill temperatures are in the range at which frostbite is possible in 30 minutes or less. Remove wet clothing as soon as practical and replace with dry, clean items.30–32 Evidence Category: C
Provide the opportunity for athletes to rewarm, as needed, during and after activity using external heaters, a warm indoor environment, or the addition of clothing. After water immersion, rewarming should begin quickly and the athlete should be monitored for afterdrop, in which the core temperature actually decreases during rewarming.33–35 Evidence Category: C
-
Include the following supplies on the field, in the locker room, or at convenient aid stations for rewarming purposes:
A supply of water or sports drinks for rehydration purposes as well as warm fluids for possible rewarming purposes. Fluids that may freeze during events in subfreezing temperatures may need to be placed in insulated containers or replaced intermittently.
Heat packs, blankets, additional clothing, and external heaters, if feasible, for active rewarming.
Flexible rectal thermometer probe to assess core body temperature. Rectal temperature has been identified as the best combination of practicality and accuracy for assessing core temperature in the field.36 Other measurements (tympanic, aural, and esophageal) are problematic or difficult to obtain. The rectal thermometer used should be a low-reading thermometer (ie, capable of measuring temperatures below 95°F [35°C]).
Telephone or 2-way radio to communicate with additional medical personnel and to summon emergency medical transportation.
Tub, wading pool, or whirlpool for immersion warming treatments (including a thermometer and additional warm water to maintain required temperatures). Evidence Category: C
Notify area hospital and emergency personnel before large events to inform them of the potential for cold-related injuries. Evidence Category: C
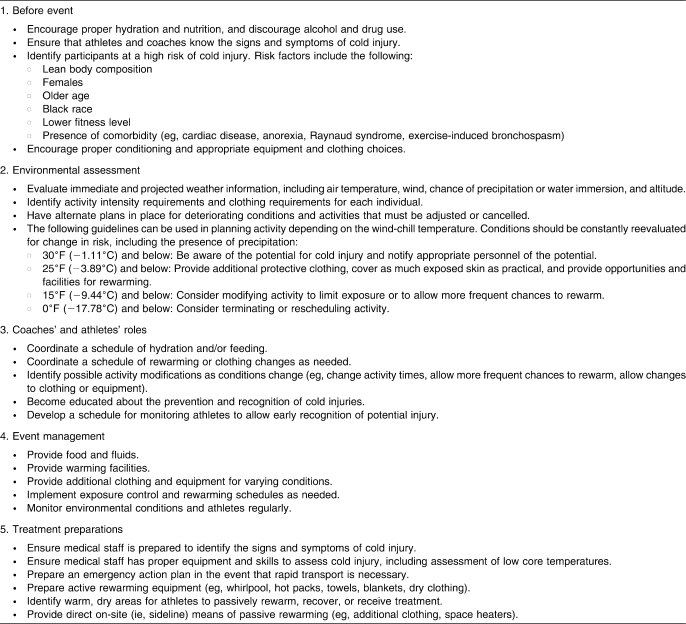
Table 3.
Prevention and Risk Management Process for the Certified Athletic Trainer
Figure 4. A, United States National Weather Service Wind Chill Chart (figure reproduced from http://www.weather.gov/os/windchill/images/windchillchart3.pdf). B, Meteorological Society of Canada/EnvironmentCanada Wind-Chill Calculation Chart (figure adapted from http://www.msc.ec.gc.ca/education/windchill/windchill_chart_e.cfm). Tair = Actual air temperature in °C; V10 = wind speed at 10 m in km/h (as reported in weather observations). Temperatures to the left of the bold line are a low risk of frostbite for most people. Increasing indicates within 30 min, increasing risk of frostbite for most people within 30 minutes of exposure; High, 5 to 10 min, high risk for most people in 5 to 10 minutes of exposure; High, 2 to 5 min, high risk for most people in 2 to 5 minutes of exposure; and High, ≤2 min, high risk for most people in ≤2 minutes of exposure. Conversions: °F = (°C × 9/5) + 32; mile = km × 0.6214.
Table 4.
Approximate Clothing Insulation of Various Clothing Combinations for Cold Weather Exposure96
Recognition and Treatment
Hypothermia (Mild)
-
11.
Be aware of the signs and symptoms of hypothermia, which include vigorous shivering, increased blood pressure, rectal temperature less than 98.6°F (37°C) but greater than 95°F (35°C), fine motor skill impairment, lethargy, apathy, and mild amnesia (Table 1). Evidence Category: A
-
12.
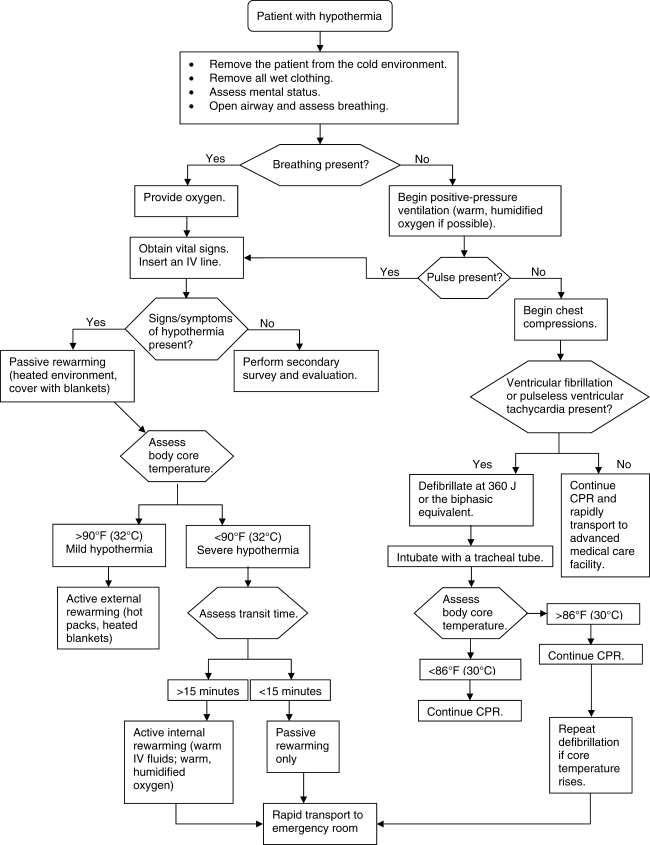
Rectal temperature obtained using a thermometer (digital or mercury) that can read below 94°F (34°C) is the preferred method for assessing core temperature in persons suspected of being hypothermic, even though procuring rectal temperature in the field can be a challenge. Using tympanic, axillary, or oral temperatures instead of rectal temperature is faulty due to environmental concerns, such as exposure to air temperatures; however, if either axillary or oral temperature is above 95°F (35°C), the person is not hypothermic.1,7–9 Figure 5 provides a treatment algorithm for hypothermia. Evidence Category: B
-
13.
Begin by removing wet or damp clothing; insulating the athlete with warm, dry clothing or blankets (including covering the head); and moving the athlete to a warm environment with shelter from the wind and rain. Evidence Category: C
-
14.
When rewarming, apply heat only to the trunk and other areas of heat transfer, including the axilla, chest wall, and groin.37–39 Rewarming the extremities can produce afterdrop, which is caused by dilation of peripheral vessels in the arms and legs when warmed. This dilation sends cold blood, often with a high level of acidity and metabolic byproducts, from the periphery to the core. This blood cools the core, leading to a drop in core temperature, and may result in cardiac arrhythmias and death.40,41 Evidence Category: C
-
15.
Provide warm, nonalcoholic fluids and foods containing 6% to 8% carbohydrates to help sustain shivering and maintain metabolic heat production. Evidence Category: C
-
16.
Avoid applying friction massage to tissues, as this may increase damage if frostbite is present.10 Evidence Category: A
Figure 5. Algorithm for patient with hypothermia.
Hypothermia (Moderate/Severe)
-
17.
Be aware of the signs and symptoms of moderate and severe hypothermia, which may include cessation of shivering, very cold skin upon palpation, depressed vital signs, rectal temperature between 90°F (32°C) and 95°F (35°C) for moderate hypothermia or below 90°F (32°C) for severe hypothermia, impaired mental function, slurred speech, unconsciousness, and gross motor skill impairment (Table 1).1,7–9 Evidence Category: A
-
18.
If an athlete with suspected hypothermia presents with signs of cardiac arrhythmia, he or she should be moved very gently to avoid causing paroxysmal ventricular fibrillation.7–9 Evidence Category: B
-
19.
Begin with a primary survey to determine the necessity of cardiopulmonary resuscitation (CPR) and activation of the emergency medical system. Remove wet or damp clothing; insulate the athlete with warm, dry clothing or blankets (including covering the head); and move the athlete to a warm environment with shelter from the wind and rain. Evidence Category: C
-
20.
When rewarming, apply heat only to the trunk and other areas of heat transfer, including the axilla, chest wall, and groin.37–39 Evidence Category: C
-
21.
If a physician is not present during the treatment phase, initiate rewarming strategies immediately and continue rewarming during transport and at the hospital. Evidence Category: C
-
22.
During the treatment and/or transport, continually monitor vital signs and be prepared for airway management. A physician may order more aggressive rewarming procedures, including inhalation rewarming, heated intravenous fluids, peritoneal lavage, blood rewarming, and use of antiarrhythmia drugs.41–46 Evidence Category: C
-
23.
When immediate management is complete, monitor for postrewarming complications, including infection and renal failure.47 Evidence Category: A<1?tpb=18pt?>
Frostbite (Superficial)
-
24.
Be aware of signs and symptoms of superficial frostbite, which include edema, redness or mottled gray skin appearance, stiffness, and transient tingling or burning (Table 1, Figure 1). Evidence Category: A
-
25.
Rule out the presence of hypothermia by evaluating observable signs and symptoms and measuring core temperature. Evidence Category: C
-
26.
The decision to rewarm an athlete is contingent upon resources available and likelihood of refreezing. Rewarming can occur at room temperature or by placing the affected tissue against another person's warm skin. Rewarming should be performed slowly, and water temperatures greater than 98°F to 104°F (37°C–40°C) should be avoided. Evidence Category: C
-
27.
If rewarming is not undertaken, protect the affected area from additional damage and further tissue temperature decreases and consult with a physician or transport to a medical facility.48–50 Evidence Category: C
-
28.
Avoid applying friction massage to tissues and leave any vesicles (fluid-filled blisters) intact.48–50 Evidence Category: C
-
29.
Once rewarming has begun, it is imperative that affected tissue not be allowed to refreeze, as tissue necrosis usually results.48–50 Evidence Category: C
-
30.
Athletes should avoid consuming alcohol and using nicotine.5 Evidence Category: B
Frostbite (Deep)
-
31.
Be aware of signs and symptoms of deep frostbite, which include edema, mottled or gray skin appearance, tissue that feels hard and does not rebound, vesicles, and numbness or anesthesia (Table 1).10–12 Evidence Category: A
-
32.
Rule out the presence of hypothermia by assessing observable signs and symptoms and measuring core temperature.10–12,48–50 Evidence Category: C
-
33.
To rewarm, the affected tissue should be immersed in a warm (98°F–104°F [37°C–40°C]) water bath. Water temperature should be monitored and maintained. Remove any constrictive clothing and submerge the entire affected area. The water will need to be gently circulated, and the area should be immersed for 15 to 30 minutes. Thawing is complete when the tissue is pliable and color and sensation have returned. Rewarming can result in significant pain, so a physician may prescribe appropriate analgesic medication. Evidence Category: C
-
34.
If rewarming is not undertaken, the affected area should be protected from additional damage and further tissue temperature decreases. Consult with a physician or transport the athlete to a medical facility.48–50 Evidence Category: C
-
35.
Tissue plasminogen activators (tPA) may be administered to improve tissue perfusion. These agents have been shown to limit the need for subsequent amputation due to tissue death.51 Evidence Category: B
-
36.
Do not use dry heat or steam to rewarm affected tissue.48–50 Evidence Category: C
-
37.
Avoid friction massage or vigorous rubbing to the affected tissues and leave any vesicles or fluid-filled blisters intact. If vesicles rupture, they should be treated to prevent infection.48–50 Evidence Category: C
-
38.
Once rewarming has begun, it is imperative that the affected tissue not be allowed to refreeze, as tissue necrosis usually results. Also, weight bearing should be avoided when feet are affected. If the possibility of refreezing exists, rewarming should be delayed until advanced medical care can be obtained.48–50 Evidence Category: C
-
39.
Athletes should avoid using alcohol and nicotine.48–50 Evidence Category: B
-
40.
If tissue necrosis occurs and tissue sloughs off, debridement and infection control measures are appropriate.48–50 Evidence Category: B
Chilblain
-
41.
Be aware of the signs and symptoms of chilblain, which include exposure to cold, wet conditions for more than 60 minutes at temperatures less than 50°F (16°C) and the presence of small erythematous papules, with edema, tenderness, itching, and pain (Table 1, Figure 2). Upon rewarming, the skin may exhibit inflammation, redness, swelling, itching, or burning and increased temperature.14 Evidence Category: A
-
42.
Remove wet or constrictive clothing, wash and dry the area gently, elevate the area, and cover with warm, loose, dry clothing or blankets.14 Evidence Category: C
-
43.
Do not disturb blisters, apply friction massage, apply creams or lotions, use high levels of heat, or allow weight bearing on the affected area.14 Evidence Category: C
-
44.
During treatment, continually monitor the affected area for return of circulation and sensation.14 Evidence Category: C
Immersion (Trench) Foot
-
45.
Be aware of the signs and symptoms of immersion (trench) foot, which include exposure to cold, wet environments for 12 hours to 3 or 4 days, burning, tingling or itching, loss of sensation, cyanotic or blotchy skin, swelling, pain or sensitivity, blisters, and skin fissures or maceration (Table 1, Figure 3).8,14 Evidence Category: A
-
46.
To prevent immersion foot, encourage athletes to maintain a dry environment within the footwear, which includes frequent changes of socks or footwear (or both), the use of moisture-wicking sock material, controlling excessive foot perspiration, and allowing the feet to dry if wearing footwear that does not allow moisture evaporation (eg, vinyl, rubber, vapor-barrier shoes or boots).5,8,14 Evidence Category: C
-
47.
For treatment, thoroughly clean and dry the feet, and then treat the affected area by applying warm packs or soaking in warm water (102°F–110°F [39°C–43°C]) for approximately 5 minutes. Replace wet socks with a clean, dry pair, and rotate footwear or allow footwear to dry before reusing.8,14 Evidence Category: C
-
48.
Use a risk management process that includes strategies for preventing, recognizing, and treating cold injuries during events. These strategies can then be used for preparing and devising risk management protocols and plans when cold injuries may be a possibility. An example of a risk management process is found in Table 3. Evidence Category: C
Background and Literature Review
Thermoregulation
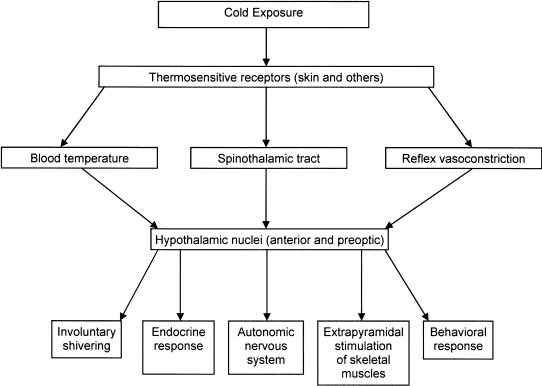
During cold stress, a normal body temperature is maintained through a complex regulatory system. A summary of the interactions among various physiologic influences and controls is found in Figure 6. Maintaining a normothermic body temperature depends on a dynamic balance between heat gained from metabolic heat production and heat lost to the environment.52–58 The body's basic responses to cold stress in order to maintain normothermia are an increase in metabolic heat production, or thermogenesis, and peripheral vasoconstriction at the skin surface to prevent heat loss to the environment.
Figure 6. Physiologic responses to cold exposure.
An increase in metabolic heat production can be accomplished in 2 ways: nonshivering thermogenesis and shivering thermogenesis. Nonshivering thermogenesis is defined as an increase in metabolic heat production from sources other than muscle contraction and is not considered a major source of metabolic heat in adult humans.52–58 Shivering thermogenesis is defined as an increase in heat production due to involuntary muscle contraction.52–60 The onset and intensity of shivering are mitigated by the duration and intensity of the cold exposure. The large muscle groups of the trunk are typically the first muscles to begin contracting, and the contractions then spread to the extremities.60 These alterations in body metabolism are mediated by the efferent output leaving the thermoregulatory center of the hypothalamus. This efferent output is determined by the integration of afferent input from the skin and the deep body receptors at the great vessels and by the local temperature of the hypothalamic thermoregulatory center itself.58,61
A decrease in peripheral blood flow due to blood vessel constriction prevents loss of heat to the environment by reducing the thermal gradient (ie, the temperature difference between the skin and the environment). The reduction in peripheral blood flow is highly specific and most pronounced in the extremities. Neural control of peripheral blood flow is under the influence of skin temperature, core temperature, and baroreflexes.53–57,61 The vasoconstriction response typically begins at a skin temperature of less than 93.2°F to 95.0°F (34°C–35°C)62 and is maximized at skin temperatures of 87.8°F (31°C) and below.63 The magnitude and duration of the vasoconstriction is modulated by a cold-induced vasodilation (CIVD). The CIVD appears to limit the duration of the vasoconstriction and protect the affected area from local cold injury. Periodic fluctuations in blood flow create fluctuations in skin temperature after the initial drop in skin blood flow and temperature with cold exposure. This fluctuation between minimal and greater-than-normal flow continues throughout the cold exposure. The CIVD appears to be mediated by the cessation of norepinephrine release after initial release. It may also occur due to decreases in tissue temperature, which diminish sympathetic nerve conduction and stop the release of norepinephrine. The resulting blood flow increase rewarms the tissue, nerve activity is reestablished, norepinephrine is released, and vasoconstriction is reinitiated. When the CIVD is absent (which can result from certain drugs; see “Nonenvironmental Risk Factors”) and fails to provide protection, the risk of nonfreezing cold injury may increase.14,64
Heat Loss Mechanisms
The human body loses heat to the environment through 4 mechanisms: radiation, convection, conduction, and evaporation. By manipulating environment or clothing (microenvironment) or both, humans can minimize heat losses. However, with inappropriate choices or when proper choices are unavailable, heat losses are exacerbated, with potentially fatal consequences.
Radiation is heat lost directly to the environment by long-wave (infrared) radiation. Wind, wetness, and other factors do not affect it. Radiative heat loss is greatest at night, especially with the absence of the moon or cloud cover. Uncovered surfaces of the body, especially the head, face, neck, and hands, also increase radiative heat loss. Heat lost through uncovered skin is perceived to be greater because skin temperature is lower and can account for 50% to 65% of all heat losses from the human body in a resting state.52
Convection is heat lost through the movement of air or water across the skin. The human body maintains a thin layer of warm air adjacent to the skin, called the boundary layer. Convection enhances the rate of evaporative heat loss. Air moving across the skin removes this warm layer, replacing it with a cold layer of air that must then be warmed. Air movement may be from wind or a person moving through the air, as in running, skiing, cycling, etc. Depending upon the speed of the air moving across the skin, convective heat losses may be small or large. An estimate of convective heat loss is the wind-chill factor. The amount and insulative properties of clothing worn may reduce or intensify convective heat losses.52
Conduction is heat lost by direct contact with a cold surface. It is exacerbated by moisture, either in the environment (rain, snow, or water immersion) or in wet clothing. Conduction can increase heat loss by up to 5 times with wet clothing and up to 25 times with water immersion. Proper selection of clothing, footwear, layering, and activity level can drastically reduce conductive heat losses. Subcutaneous fat stores also help to reduce conductive heat loss. Conductive and convective heat losses usually account for approximately 15% of all heat losses; however, high air speed, inadequate amounts of dry clothing, wet clothing, and water immersion all drastically increase conductive and convective heat losses.52
Evaporative heat losses account for 15% to 25% of the total and occur through respiration and exposed skin. Little can be done to reduce evaporative heat losses from respiration, because ambient air must be warmed to core temperature and humidified to 100% as it moves into the respiratory tract. However, like conductive heat losses, losses from the skin and sweating can be controlled through proper selection of clothing and activity level.52
The amount of heat lost from the body can be calculated using the classical heat balance equation. The equation refers to the balancing of heat being produced by metabolism (thermogenesis) and the rate at which it is being lost to the environment via radiation, convection, conduction, and evaporation (thermolysis). This equation provides a conceptual understanding of the interplay between the production of heat within the body and the loss of heat to the environment. When an imbalance develops between the rates of heat production and heat loss, total body heat content changes.52 For example, when an athlete ceases exercise, the level of heat production diminishes, while the level of heat loss remains unchanged. This leads to an imbalance between the rates of heat production and heat loss.
S = M-R-C-K-E
S = heat gain/loss
M = metabolic heat production
R = radiative heat loss
C = convective heat loss
K = conductive heat loss
E = evaporative heat loss
Pathophysiology of Cold Injury
Hypothermia
Hypothermia (defined as a decrease in core body temperature below 95°F [35°C]) can develop in cold and dry or cold and wet conditions and can arise either slowly over many hours or quite suddenly. Generally, slow-onset hypothermia occurs on land, whereas sudden hypothermia results from cold-water immersion or exposure to cold rain.1,7–9 The body loses heat faster than it can generate heat and core temperature begins to drop. Although we associate hypothermia with temperatures below freezing, it also occurs at temperatures as high as 50°F to 60°F (10°C–16°C).3 For example, at the 1983 Bostonfest Marathon, 20% of the runners presenting for treatment at the finish-line medical tent were diagnosed with hypothermia3 despite an ambient temperature of approximately 50°F (10°C). During the 1985 Boston Marathon, 75 runners (1.3% of entrants) were treated for hypothermia, even though the ambient temperature was 76°F (24°C).1
Hypothermia is caused by the body's inability to maintain a normal core temperature, with resulting changes in the function of the nervous system, cardiovascular system, respiratory system, and renal system.62 The central nervous system is susceptible to depression during cold exposure. This depressed activity is typically manifested as changes in motor function (eg, clumsiness, loss of finger dexterity, slurred speech), cognition (eg, confusion, poor decision making, memory loss) and level of consciousness. Significant changes in central nervous system function occur as core temperature drops below 95°F (35°C), and show a linear decrease as core temperature continues to drop. Brain function becomes measurably abnormal below 92.3°F (34°C) and ceases at 66°F to 68°F (19°C–20°C).7,62
Cardiovascular system functional change is manifested as an initial tachycardia and then a progressive bradycardia that decreases the resting heart rate by 50%. This drop in heart rate is due to decreased depolarization of the heart pacemaker cells. Other changes include increased myocardial oxygen demand and decreased arterial pressure and cardiac output. The conduction system changes are apparent during an electrocardiogram as prolonged PR, QRS, and QT intervals. Additional arrhythmias may include ventricular fibrillation and asystole, which can occur when the core temperature is below 77°F (25°C), and atrial fibrillation, which is common at core temperatures below 89.6°F (32°C).7,62
The renal system responds to cold exposure by excreting large amounts of glomerular filtrate. This cold-induced diuresis appears to be due to a large increase in central volume secondary to peripheral vasoconstriction. Diuresis may occur to balance fluid levels as the central circulation becomes overloaded. The urine produced is very dilute, regardless of hydration status. Cold-water immersion can further increase urine output by 3.5 times normal. These renal responses occur during rest and light activity.7,62
The respiratory system reacts to cold exposure by initially producing a hyperventilation response. After the initial response, however, the ventilation rate progressively decreases as core temperature drops, reaching 5 to 10 breaths per minute below a core temperature of 86°F (30°C). Carbon dioxide production also decreases by up to 50%, which can lead to respiratory acidosis. These respiratory responses occur during rest and light activity.7,62
Frostbite
The pathophysiology of deep frostbite (defined as actual freezing of body tissues) typically consists of 3 distinct phases: frostnip, mild frostbite, and deep frostbite. The frostnip, or prefreeze, phase occurs with superficial skin cooling below 50°F (10°C), resulting in loss of sensation, constriction of the microvasculature, plasma leakage, and increased viscosity of vascular contents.65
Mild frostbite, or freeze-thaw phase, begins as skin temperature drops below 28°F (−2°C) and extracellular ice crystals form. The location and rate of crystal formation depends on the severity of the cold stress (combination of air temperature, moisture presence, and wind). Water migrates across the cell membrane, resulting in intracellular dehydration and increased intracellular electrolyte concentrations. As the cell volume decreases, the cell eventually collapses, the membrane ruptures, and cell death occurs. As crystallization progresses, surrounding cells and vascular structures are compressed.65–67
The third phase, or severe frostbite, results in microvascular collapse at the arteriole and venule levels. As microvascular tissue fails, blood viscosity increases, resulting in microthrombi, plasma leakage, increased tissue pressure, ischemia, and tissue death. Nerve and muscle tissue may also be affected. As edema resolves over approximately 72 hours from onset, the most noticeable sign of frostbite is gangrenous tissue.65–67
Blood flow to the skin of the extremities (acral skin) (eg, fingers, toes, tip of nose) is under much stronger local control of vasoconstriction and vasodilation than nonacral skin and is very sensitive to local changes in temperature. This local control is independent of the central nervous system and produces significant changes in blood flow to skin that is cooled, regardless of changes in core temperature. Nonacral skin blood flow is controlled by the central nervous system, and changes in flow are likely due to changes in core temperature. These differences in control of blood flow produce the scenario of potential freezing injury to acral skin without a significant drop in core body temperature.68
Chilblain (pernio) and Immersion (trench) Foot
Nonfreezing cold injuries, such as chilblain and immersion foot, appear to share a common pathophysiology and generally result in cellular damage without ice crystal formation.67 The abnormal inflammatory response typically leads to intracellular and then extracellular fluid build-up. Increased extracellular fluid results in damage to neurologic and vascular tissue. Classic symptoms of swelling, numbness, and itching, followed by hypersensitivity to cold after rewarming, appear related to a dermal edema, migration of lymph fluid, microvascular damage, and vascular and neurologic hypersensitivity to cold exposure.67
Nonenvironmental Risk Factors
Health care providers should be aware of the following nonenvironmental risk factors, which may make athletes more susceptible to cold injury and may affect normal physiologic responses to cold exposure.
Previous Cold Injuries
Having sustained a previous cold injury increases the chance of subsequent cold injuries by 2 to 4 times, even if prior injuries were not debilitating or resolved with no or minimal medical care.3,6,69 For example, an athlete who sustained frostnip or frostbite is 2 to 4 times more likely to develop frostbite in the same area again, given similar environmental conditions.
Low Caloric Intake, Dehydration, and Fatigue
Low caloric intake (less than 1200 to 1500 kcal/day) or hypoglycemia (or both) directly decreases metabolism and concomitant heat production,5 contributing to the inability to maintain body temperature balance through physical activity. Dehydration does not negatively affect peripheral vasoconstriction or shivering and, therefore, does not appear to increase susceptibility to cold injury.5,70–80 Fatigue associated with hypoglycemia is linked to impaired peripheral vasoconstriction and shivering responses and can lead to faulty decision making and inadequate preparations, indirectly resulting in cold injuries.
Race
Black individuals have been shown to be 2 to 4 times more likely than individuals from other racial groups to sustain cold injuries. These differences may be due to cold weather experience, but are likely due to anthropometric and body composition differences, including less-pronounced CIVD, increased sympathetic response to cold exposure, and thinner, longer digits.3,6
Nicotine, Alcohol, and Drug Use
Nicotine inhaled through smoking causes a reflex peripheral vasoconstriction, possibly negating the CIVD and later enhancing the cold-induced vasoconstriction to maintain core temperature. Alcohol reduces the glucose concentration in the blood, which tends to decrease the shivering response. Alcohol also may lead to faulty decision making due to its effects on the central nervous system. Drugs with a depressive effect may impair the thermoregulatory system and so inhibit the body's reaction to cold by blunting the peripheral vasoconstriction and shivering responses. As with alcohol, they may also lead to faulty decision making.77,81,82
Body Size and Composition
Body fat and muscle mass appear to be instrumental in providing protection for maintaining core body temperature with exposure to cold air and water. This effect appears in both males and females regardless of the amount of clothing worn. Strong evidence suggests that percentage of body fat (>25%, approximately) and amount of muscle mass are reliable predictors of the ability to maintain and protect core body temperature during prolonged exposure to a wide range of cold air and water temperatures. The greater the level of body fat and muscle mass, the better the ability to protect core body temperature through passive (eg, insulative properties of fat) and active (eg, shivering thermogenesis) mechanisms.83–86
Aerobic Fitness Level and Training
Overall, physical training and fitness level appear to have only minor influence on thermoregulatory responses to cold. Most cross-sectional comparisons of aerobically fit and less-fit persons show no relationship between maximal aerobic exercise capability and temperature regulation in the cold. In those studies purportedly demonstrating a relationship,87,89 differences in thermoregulation appear more likely attributable to anthropometric (body size and composition) differences between aerobically fit and less-fit participants, rather than an effect of maximal aerobic exercise capabilities per se. The primary thermoregulatory advantage provided by increased endurance resulting from physical training is that a fitter individual can sustain higher-intensity, longer-duration voluntary activity than a less-fit person and, thus, maintain higher sustained rates of metabolic heat production, keeping the former warmer. In addition, exercise training has been suggested to enhance the peripheral vasoconstriction response, which would conserve body heat but possibly increase peripheral cold injury risks.87–91
Sex
The hypothermia injury rate for females is 2 times higher than for males. Sex differences in thermoregulatory responses during cold exposure are influenced by interactions among total body fat content, subcutaneous fat thickness, amount of muscle mass, and surface area-to-mass ratio. For example, among men and women with equivalent total body mass and surface areas, women's greater fat content enhances insulation and reduces the fall in core temperature. In women and men of equivalent subcutaneous fat thickness, women typically have a greater surface area but smaller total body mass and smaller muscle mass (thus, lower total body heat content) than men and lose heat at a greater rate. Women's thermogenic response to cold exposure also appears less able to generate metabolic heat than men of similar body composition due to less total muscle mass. Therefore, total heat loss is greater in women due to the larger surface area for convective heat loss, and body temperature tends to fall more rapidly for any given cold stress.91–94 As a result, the prevention and recognition recommendations in this position statement should be interpreted and used more conservatively for female athletes than male athletes.
Clothing
The role of clothing in preventing cold injuries lies in its ability to reduce heat loss to the environment by trapping warm air. Cold-weather clothing typically has an internal layer that allows evaporation of sweat without absorption, a middle layer that provides insulation, and an external layer that is wind and water resistant and allows evaporation of moisture. The internal layer is in direct contact with the skin and uses a moisture-wicking material such as polyester or polypropylene. This layer should not retain moisture but should transfer the moisture to other layers, from which it can evaporate. The middle layer provides the primary insulation against heat loss and can be a fleece or wool material. The outer layer should have venting abilities (eg, zippers or mesh in the armpits or low back area) to allow moisture transfer to the environment.95
Clothing requirements for cold environment exercise depend on ambient temperature; presence of wind, rain, and water; and activity intensity. Generally speaking, as exercise intensity increases at any given air temperature, the amount of clothing insulation needed to maintain body temperature equilibrium decreases. The insulative protection offered by different clothing combinations is represented in units of clo. One clo of insulation is the clothing needed to permit a person to rest comfortably when the air temperature is 70°F (21°C).96 See Table 4 for a list of the clo values of common clothing combinations. Interactions between exercise intensity and ambient conditions dictate the selection of clothing based upon clo values. For example, if the ambient temperature is 20°F (−7°C) and the person is at rest (1 metabolic equivalent of exercise intensity), then clothing with a clo value of approximately 5 is needed to maintain core temperature. If activity is increased to an exercise intensity of 4 metabolic equivalents, then clothing with a clo value of approximately 2 would be adequate.5 However, imposing a standard clothing requirement for a group of individuals could result in overheating in some and inadequate protection in others. Individuals should be able to adjust clothing according to their specific responses and comfort levels while following general guidelines.
Other clothing considerations include the ability to adapt when weather conditions change, especially if rain, snow, or water immersion is a possibility. In these instances, waterproof or water-resistant clothing should be available, and the athlete should be able to change into dry clothing as needed. Socks should not constrict blood flow, should allow the evaporation of moisture, and should be changed frequently after sweating or water immersion. Another consideration is the heat lost from an uncovered head. Even if the remainder of the body is well insulated in ambient temperatures of 25°F (−4°C),97 fleece, knit caps, or other complete head coverings can significantly reduce heat loss.
Predisposing Medical Conditions
The following medical conditions add to the risk of cold injury or are exacerbated by exposure to cold environments.
Exercise-Induced Bronchospasm
Exercise-induced bronchospasm (EIB), also called exercise-induced asthma or airway hyperresponsiveness, is a narrowing of the respiratory tract airways. It is exacerbated by exposure to cold, dry air. Predisposing factors include asthma and allergies. However, not all individuals with EIB have asthma or allergies, and not all individuals with asthma or allergies have EIB. This condition can affect any individual, from a small child at play to an elite athlete.98–101 Authors102 have noted a high prevalence of EIB in cold-weather athletes, in women, and in athletes training and competing in indoor ice facilities. Two possible mechanisms have been suggested to explain EIB. The osmotic theory postulates that excessive airway drying due to increased breathing rates enhances the secretion of vasoconstrictor mediators in the breathing passageways. This increased vasoconstrictor response then limits air flow.103 A second theory suggests that the combination of cold air and increased breathing rate cools airways; after airways rewarm, increased blood flow leads to edema formation and airway flow reductions.103 The reduction of airway flow reduces maximal ventilation and, subsequently, maximal performance.
Raynaud Syndrome
As with EIB, Raynaud syndrome is caused by cold exposure and characterized by intermittent vasospasm of the digital vessels. This vasospasm significantly reduces blood flow to the extremities. The affected area may present with tingling, swelling, or a throbbing pain. The skin may turn a shade of white, then possibly blue, and then becomes red upon rewarming. Raynaud syndrome describes a spectrum of disorders whose causes are usually idiopathic, although infrequently, autonomic dysfunction or an underlying condition such as thoracic outlet syndrome or collagen vascular disease may be responsible.67
Anorexia Nervosa
Anorexia nervosa results in a deficiency of body fat stores, potential malnutrition, decreased metabolic rate, and peripheral vasoconstriction. These changes limit the ability to maintain a normal core temperature.104–106
Cold Urticaria
Cold urticaria may be the most common form of urticaria.5,107 The condition has a rapid onset, presenting with wheals (hives) that may be local or generalized, redness, itching, and edema. Other symptoms may include fatigue, headache, dyspnea, and in rare cases, anaphylactic shock. Two forms of the condition, primary acquired and secondary acquired (hereditary), have been identified and differ in speed of onset: within minutes or 24 to 48 hours after cold exposure, respectively.107
Cardiovascular Disease
Individuals with cardiovascular disease are sensitive to increased demands on the myocardium and increases in blood pressure, as well as having potentially decreased flow to cutaneous and subcutaneous tissues. Cold exposure coupled with exercise increases the demand on the cardiovascular system by increased sympathetic nervous system activity, peripheral resistance, blood pressure, and myocardial oxygen demands. This increased stress is in contrast to the demands of rest and exercise in warm environments.108,109 Therefore, individuals with diminished cardiovascular system function should be cautious when exercising in the cold and should be monitored closely for symptoms associated with a myocardial infarction.
Environmental Risk Factors
Environmental cold stress results from a combination of low air temperature; humidity, rain, or immersion; and little thermal radiation and air movement. An index of cold stress is the wind-chill temperature index (WCT) (Figure 4). This index gives an indication of how cold a person feels when exposed to a combination of cold air and wind. This index estimates the danger of extreme cooling of exposed skin (ie, the risk of frostbite) while walking at 3 mph (1.3 m·s−1) in various combinations of conditions. When the WCT is below −18°F (−27°C), the risk of developing frostbite in exposed skin in less than 30 minutes increases, warranting closer observation. However, the environmental wind speed in the WCT does not account for wind produced during movement. Biking or running produce wind across the body at the same rate as body movement and should be taken into account when estimating risk. For example, if a light wind is present (less than 5 mph [2.24 m·s−1]) with cold temperatures (25°F [−4°C]), the risk of frostbite for most people is low. Yet if the athlete is cycling at 15 mph (16.71 m·s−1), the relative risk of developing frostbite increases. Therefore, the effect of air movement produced by the body should be taken into account when using the wind-chill recommendations. The WCT is calculated using the following formula27:
Wind chill (°F) = 35.74 + 0.6215T − 35.75V0.16 + 0.4275T(V0.16)
Where T = Air temperature (°F), and V = Wind speed (mph)
This index is a useful tool to monitor the potential thermal stress athletes must deal with when exposed to cold temperatures.
Influence of Wind, Rain, and Immersion
Exercise during windy or rainy conditions or water immersion poses several unique challenges to the body's ability to maintain a normal body temperature. The transfer of body heat in water may be 70 times greater than in air.52 This transfer can lead to a significant loss of body heat for those exercising in rainy conditions or in the water. Maintaining normal body temperature in those conditions depends on several factors, including exercise intensity, exercise mode, anthropometric factors, insulative properties of clothing and equipment, and the magnitude of heat loss caused by wind speed, amount of rain, or water temperature.52
During exercise in cold and wet conditions, the ability to generate adequate metabolic heat to maintain body temperature depends on exercise intensity and mode.51 More heat is lost from the arms and legs due to smaller diameter and shorter distance from the limb center to the surface, which allows rapid heat conduction compared with the trunk. This increased conduction is outweighed when exercise intensity is greater than 75% of maximal oxygen uptake (V̇o2 max).53,54 Exercise mode also affects the ability to generate metabolic heat. The more muscle mass involved in performing the exercise, the greater the heat generated. Therefore, exercise involving only the lower body generates more heat than exercise involving only the upper body, and whole-body exercise generates more heat than lower or upper body exercise alone.
The combination of windy and wet conditions can also affect body temperature maintenance. Light to moderate exercise in the rain leads to decreases in core temperature compared with resting conditions.79 When air temperature is −15.0°F (5°C) and clothes are wet, heat losses may double those observed in dry conditions.55 Decreases in core temperature have been observed with the addition of wind during light-intensity exercise. With high-intensity exercise (greater than 60% of peak oxygen consumption), body temperature can be maintained in cold, windy, and wet conditions.56
The influence of water temperature and amount of wet or immersed skin also influences heat loss. The lower the water temperature and the larger the surface area of the body immersed in or in contact with water, the greater the heat loss and the more rapid the decreases in core temperature.57
The best survival strategy for an individual exposed to accidental, prolonged cold-water immersion (eg, boating or water craft accident) has been debated: try to swim for safety, move vigorously in place to generate body heat, or remain quiet and move very little to conserve body heat. Recent researchers110 suggested the following strategies:
Stay calm. Unless you're wearing an immersion suit, you'll experience cold shock when you go into cold water due to rapid cooling of the skin. You won't be able to control your breathing, and you won't get far if you try to swim at this point. Your breathing will return to normal in 2 to 3 minutes.
Make a plan. While you're waiting for the cold shock to subside, consider your situation and decide whether to swim or stay in the present location.
If you decide to swim, look for the shore and decide if you can make it. Most people studied could swim between 800 and 1500 m (874.9 and 1640.4 y) in cold water, or for 45 minutes, before their arms and leg muscles cooled to the point that they could no longer swim.
If you decide to stay in place, try to get out of the water as much as possible. Complete any tasks that require the use of your hands, such as tying knots or turning on flares, as soon as possible. As your hands cool, they lose dexterity.
Stick to your decision; don't change your mind midway. After 30 minutes in cold water, you may become hypothermic, and you won't make the best decisions.
After immersion in cold water, athletes should be monitored for the phenomenon of afterdrop. Once physical activity concludes, the body still dissipates significant amounts of heat but no longer generates metabolic heat through activity. This imbalance between heat loss and heat production could lead to drops in core temperature during the rewarming process. Afterdrop is commonly found in individuals after prolonged water immersion in which core temperature has already decreased.30–32
Role of Cold Acclimatization
Cold acclimatization may play a role in tolerance of cold exposure, but observed adjustments are modest and rely upon the severity of previous exposure. Adjustments found in persons with recurring exposure to cold are habituation, metabolic acclimatization, and insulative acclimatization.111
Cold-induced habituation manifests itself as a decreased shivering and vasoconstriction response during cold exposure compared with nonacclimatized exposures. Some individuals may also have a greater decrease in core temperature than nonacclimatized persons; this is known as hypothermic habituation. Short, intense exposures that occur a few times per week appear to elicit habituation. Hypothermic habituation, however, occurs with longer exposures in moderate temperatures during consecutive days over a period greater than 2 weeks.111
Metabolic acclimatization is characterized by a more pronounced shivering response to cold and typically occurs after long-term exposures. Insulative acclimatization is produced by greater conservation of heat during exposure to cold. This includes a larger and more rapid decline in skin temperature, resulting in less heat conduction at the skin. Another response may be improved convective heat loss due to a circulatory countercurrent heat exchange mechanism.111
In comparison with the acclimatization observed with repeated environmental heat exposure, adjustment to the physiologic response during cold exposure appears to be more difficult to acquire, varies more from individual to individual, develops more slowly, and has less of a preventive effect.
Special Concerns
Children (prepubescents)
Exposure to cold environments poses unique challenges for young athletes due to their higher surface area-to-mass ratios and smaller adipose tissue deposits. These factors result in a faster cooling rate than for adults in water and similar cooling rates as adults in cold air. These rates appear to be a function of a higher level of metabolic heat production and a stronger peripheral vasoconstriction response.112,113 Therefore, children should take similar preventive measures as those suggested for adults, but they should be encouraged to take more frequent breaks from a cold environment, especially water immersion.
Older Individuals (more Than 50 Years Old)
As one ages, the ability to tolerate cold decreases and risk of hypothermia increases.5,6 This increased risk for hypothermia appears to be due to diminished sympathetic nervous system-mediated reflex vasoconstriction, which allows greater heat loss.114 Additionally, an older individual is more likely to have health concerns such as diabetes, hypothyroidism, hypopituitarism, or hypertension, which increase the likelihood of cold injury. As older individuals continue an active lifestyle and as advances in medical and surgical treatments extend life, more persons with histories of myocardial infarction and stroke are becoming active in outdoor environments.6,55,62,64,115,116 Thus, ATs working with older athletes should apply prevention and recognition recommendations more conservatively in this population.
Spinal Cord Injuries
The presence of a spinal cord injury (SCI) resulting in some form of paralysis is associated with an increased risk for hypothermia during cold exposure.117,118 Athletes with SCI tend to be less sensitive to the sensation of cold on the skin surface and have a diminished perception of skin temperature change.119,120 Overall, individuals with SCI have a diminished capability to stabilize core temperature121; specifically, they have a diminished autonomic response to cold, which results in a decreased vasoconstriction response117,122 and a decreased effector response to the muscle to generate metabolic heat.122 Those with SCI also have abnormal blood pressure responses to cold exposure,123 as well as increased complaints of muscle spasticity, pain, and numbness.124–127 Consequently, athletes with SCI should be monitored closely for both core temperature changes and skin changes associated with nonfreezing cold injury.
Conclusions
Certified athletic trainers and other health care providers must be able to identify the signs and symptoms of hypothermia, frostbite, chilblains, and immersion (trench) foot in athletes. This position statement outlines the current recommendations to prevent the occurrence and improve the recognition and treatment of cold injury in athletes.
Acknowledgments
We gratefully acknowledge the efforts of Timothy S. Doane, MA, ATC; Michael G. Dolan, MA, ATC; Ernie Hallbach, MA, ATC; W. Larry Kenney, PhD; Glen P. Kenny, PhD; Roger Kruse, MD; and the Pronouncements Committee in the preparation of this document.
DISCLAIMER
The NATA publishes its position statements as a service to promote the awareness of certain issues to its members. The information contained in the position statement is neither exhaustive not exclusive to all circumstances or individuals. Variables such as institutional human resource guidelines, state or federal statutes, rules, or regulations, as well as regional environmental conditions, may impact the relevance and implementation of these recommendations. The NATA advises its members and others to carefully and independently consider each of the recommendations (including the applicability of same to any particular circumstance or individual). The position statement should not be relied upon as an independent basis for care but rather as a resource available to NATA members or others. Moreover, no opinion is expressed herein regarding the quality of care that adheres to or differs from NATA's position statements. The NATA reserves the right to rescind or modify its position statements at any time.
Footnotes
Thomas A. Cappaert, PhD, ATC, CSCS, CES, contributed to conception and design; analysis and interpretation of the data; and drafting, critical review, and final approval of the article. Jennifer A. Stone, MS, ATC, CSCS, contributed to conception and design; analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. John W. Castellani, PhD, FACSM, contributed to conception and design; analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. Bentley Andrew Krause, PhD, ATC, contributed to conception and design; analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. Daniel Smith, ATC, CSTS, ART, contributed to conception and design and critical revision and final approval of the article. Bradford A. Stephens, MD, PC, contributed to conception and design and critical revision and final approval of the article.
References
- 1.Sallis R, Chassay C.M. Recognizing and treating common cold-induced injury in outdoor sports. Med Sci Sports Exerc. 1999;31(10):1367–1373. doi: 10.1097/00005768-199910000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Rav-Acha M, Heled Y, Moran D.S. Cold injuries among Israeli soldiers operating and training in a semiarid zone: a 10-year review. Mil Med. 2004;169(9):702–706. doi: 10.7205/milmed.169.9.702. [DOI] [PubMed] [Google Scholar]
- 3.Reynolds K, Williams J, Miller C, Mathis A, Dettori J. Injuries and risk factors in an 18-day Marine winter mountain training exercise. Mil Med. 2000;165(12):905–910. [PubMed] [Google Scholar]
- 4.Jones B.H, Rock P.B, Smith L.S, et al. Medical complaints after a marathon run in cool weather. Physician Sportsmed. 1985;13(10):103–110. doi: 10.1080/00913847.1985.11708904. [DOI] [PubMed] [Google Scholar]
- 5.Castellani J.W, Young A.J, Ducharme M.B, Giesbrecht G.G, Glickman E, Sallis R.E. American College of Sports Medicine position stand: prevention of cold injuries during exercise. Med Sci Sports Exerc. 2006;38(11):2012–2029. doi: 10.1249/01.mss.0000241641.75101.64. [DOI] [PubMed] [Google Scholar]
- 6.DeGroot D.W, Castellani J.W, Williams J.O, Amoroso P.J. Epidemiology of U.S. Army cold weather injuries, 1980–1999. Aviat Space Environ Med. 2003;74(5):564–570. [PubMed] [Google Scholar]
- 7.Danzl D.F. Accidental hypothermia. In: Marx J.A, editor. Rosen's Emergency Medicine: Concepts and Clinical Practice. St Louis, MO: Mosby; 2006. pp. 2236–2254. Vol 3. [Google Scholar]
- 8.Hamlet M.P. Human cold injuries. In: Pandolf K.B, Sawka M.N, Gonzalez R.R, editors. Human Performance Physiology and Environmental Medicine at Terrestrial Extremes. Indianapolis, IN: Benchmark Press; 1988. pp. 435–466. [Google Scholar]
- 9.Ulrich A.S, Rathlev N.K. Hypothermia and localized cold injuries. Emerg Med Clin North Am. 2004;22(2):281–298. doi: 10.1016/j.emc.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Murphy J.V, Banwell P.E, Roberts A.H.N, McGrouther D.A. Frostbite: pathogenesis and treatment. J Trauma. 2000;48(1):171–178. doi: 10.1097/00005373-200001000-00036. [DOI] [PubMed] [Google Scholar]
- 11.Hamlet M.P. Prevention and treatment of cold injury. Int J Circumpolar Health. 2000;59(2):108–113. [PubMed] [Google Scholar]
- 12.Hassi J. Frostbite, a common cold injury: challenges in treatment and prevention. Int J Circumpolar Health. 2000;59(2):90–91. [PubMed] [Google Scholar]
- 13.Mills W.J. Clinical aspects of freezing cold injury. In: Pandolf K.B, Burr R.E, editors. Textbooks of Military Medicine: Medical Aspects of Harsh Environments. Falls Church, VA: Office of The Surgeon General, US Army; 2002. pp. 429–466. Vol 1. [Google Scholar]
- 14.Thomas J.R, Oakley E.H.N. Nonfreezing cold injury. In: Pandolf K.B, Burr R.E, editors. Textbooks of Military Medicine: Medical Aspects of Harsh Environments. Falls Church, VA: Office of The Surgeon General, US Army; 2002. pp. 467–490. Vol 1. [Google Scholar]
- 15.Strength of Recommendation Taxonomy (SORT) American Academy of Family Physicians. http://www.aafp.org/afp/20040201/548.html. Accessed July 2, 2008.
- 16.Hassi J, Raatikka V.P, Huurre M. Health-check questionnaire for subjects exposed to cold. Int J Circumpolar Health. 2003;62(4):436–443. doi: 10.3402/ijch.v62i4.17587. [DOI] [PubMed] [Google Scholar]
- 17.Askew E.W. Environmental and physical stress and nutrient requirements. Am J Clinic Nutr. 61(3 suppl):631S–637S. doi: 10.1093/ajcn/61.3.631S. 1995; [DOI] [PubMed] [Google Scholar]
- 18.Casa D.J, Armstrong L.E, Hillman S.K, et al. National Athletic Trainers' Association position statement: fluid replacement for athletes. J Athl Train. 2000;35(2):212–224. [PMC free article] [PubMed] [Google Scholar]
- 19.United States Department of Agriculture. MyPyramid.gov. www.mypyramid.gov. Accessed February 1, 2006.
- 20.Knight D.R, Horvath S.M. Urinary responses to cold temperature during water immersion. Am J Physiol. 1985;248(5, pt 2):R560–R566. doi: 10.1152/ajpregu.1985.248.5.R560. [DOI] [PubMed] [Google Scholar]
- 21.Allen D.E, Gellai M. Mechanisms for the diuresis of acute cold exposure: role for vasopressin. Am J Physiol. 1993;264(3, pt 2):R524–R532. doi: 10.1152/ajpregu.1993.264.3.R524. [DOI] [PubMed] [Google Scholar]
- 22.Sramek P, Simeckova M, Jansky L, Savlikova J, Vybiral S. Human physiological responses to immersion into water of different temperatures. Eur J Appl Physiol. 2000;81(5):436–442. doi: 10.1007/s004210050065. [DOI] [PubMed] [Google Scholar]
- 23.Kenefick R.W, Hazzard M.P, Mahood N.V, Castellani J.W. Thirst sensations and AVP responses at rest and during exercise-cold exposure. Med Sci Sports Exerc. 2004;36(9):1528–1534. doi: 10.1249/01.mss.0000139901.63911.75. [DOI] [PubMed] [Google Scholar]
- 24.Kuehn L.A. Sports Science Periodical on Research and Technology in Sport. Ottawa, ON, Canada: The Coaching Association of Canada; 1985. Managing and monitoring cold stress in sport; pp. 51–62. [Google Scholar]
- 25.Priest S, Dixon T, Strong M. Preventing cold injuries. J Phys Educ Rec Dance. 1989;60(8):45–50. [Google Scholar]
- 26.Danielsson U. Windchill and the risk of tissue freezing. J Appl Physiol. 1996;81(6):2666–2673. doi: 10.1152/jappl.1996.81.6.2666. [DOI] [PubMed] [Google Scholar]
- 27.National Weather Service. Windchill terms and definition. http://www.nws.noaa.gov/om/windchill/windchillglossary.shtml. Accessed February 15, 2006.
- 28.Moran D.S. Current opinion: potential applications of heat and cold stress indices to sporting events. Sports Med. 2001;31(13):909–917. doi: 10.2165/00007256-200131130-00002. [DOI] [PubMed] [Google Scholar]
- 29.Holmer I. Work in the cold: review of methods for assessment of cold exposure. Int Arch Occup Environ Health. 1993;65(3):147–155. doi: 10.1007/BF00381150. [DOI] [PubMed] [Google Scholar]
- 30.Rissanen S, Rintamaki H. Thermal responses and physiological strain in men wearing impermeable and semipermeable protective clothing in the cold. Ergonomics. 1997;40(2):141–150. doi: 10.1080/001401397188260. [DOI] [PubMed] [Google Scholar]
- 31.Smolander J, Louhevaara V, Ahonen M. Clothing, hypothermia, and long-distance skiing. Lancet. 1986;2(8500):226–227. doi: 10.1016/s0140-6736(86)92529-8. [DOI] [PubMed] [Google Scholar]
- 32.Tanaka M, Tochihara Y, Yamazaki S, Ohnaka T, Yoshida K. Thermal reaction and manual performance during cold exposure while wearing cold-protective clothing. Ergonomics. 1983;26(2):141–149. doi: 10.1080/00140138308963325. [DOI] [PubMed] [Google Scholar]
- 33.Nuckton T.J, Claman D.M, Goldreich D, Wendt F.C, Nuckton J.G. Hypothermia and afterdrop following open water swimming; the Alcatraz/San Francisco swim study. Am J Emerg Med. 2000;18(6):703–707. doi: 10.1053/ajem.2000.16313. [DOI] [PubMed] [Google Scholar]
- 34.Romet T.T. Mechanism of afterdrop after cold water immersion. J Appl Physiol. 1988;65(4):1535–1538. doi: 10.1152/jappl.1988.65.4.1535. [DOI] [PubMed] [Google Scholar]
- 35.Giesbrecht G.G, Goheen M.S, Johnston C.E, Kenny G.P, Bristow G.K, Hayward J.S. Inhibition of shivering increases core temperature afterdrop and attenuates rewarming in hypothermic humans. J Appl Physiol. 1997;83(5):1630–1634. doi: 10.1152/jappl.1997.83.5.1630. [DOI] [PubMed] [Google Scholar]
- 36.Moran D.S, Mendal L. Core temperature measurement: methods and current insights. Sports Med. 2002;32(14):879–885. doi: 10.2165/00007256-200232140-00001. [DOI] [PubMed] [Google Scholar]
- 37.Danzl D.F, Lloyd E.L. Treatment of accidental hypothermia. In: Pandolf K.B, Burr R.E, editors. Textbooks of Military Medicine: Medical Aspects of Harsh Environments. Falls Church, VA: Office of The Surgeon General, US Army; 2002. pp. 491–529. Vol 1. [Google Scholar]
- 38.Petrone P. Kuncir EJ. Asensio JA. Surgical management and strategies in the treatment of hypothermia and cold injury. Emerg Med Clinic North Am. 2003;21(4):1165–1178. doi: 10.1016/s0733-8627(03)00074-9. [DOI] [PubMed] [Google Scholar]
- 39.Kempainen R.R, Brunette D.D. The evaluation and management of accidental hypothermia. Respir Care. 2004;49(2):192–205. [PubMed] [Google Scholar]
- 40.Delaney K.A, Howland M.A, Vassallo S, Goldfrank L.R. Assessment of acid-base disturbances in hypothermia and their physiologic consequences. Ann Emerg Med. 1989;18(1):72–82. doi: 10.1016/s0196-0644(89)80319-1. [DOI] [PubMed] [Google Scholar]
- 41.Giesbrecht G.G, Bristow G.K, Uin A, Ready A.E, Jones R.A. Effectiveness of three field treatments for induced mild (33.0 degrees C) hypothermia. J Appl Physiol. 1987;63(6):2375–2379. doi: 10.1152/jappl.1987.63.6.2375. [DOI] [PubMed] [Google Scholar]
- 42.Daanen H.A, Van de Linde F.J. Comparison of four noninvasive rewarming methods for mild hypothermia. Aviat Space Environ Med. 1992;63(12):1070–1076. [PubMed] [Google Scholar]
- 43.Kornberger E, Schwarz B, Lindner K.H, Mair P. Forced air surface rewarming in patients with severe accidental hypothermia. Resuscitation. 1999;41(2):105–111. doi: 10.1016/s0300-9572(99)00069-6. [DOI] [PubMed] [Google Scholar]
- 44.Walpoth B.H, Walpoth-Aslan B.N, Mattle H.P, et al. Outcome of survivors of accidental deep hypothermia and circulatory arrest treated with extracorporeal blood warming. New Engl J Med. 1997;337(21):1500–1505. doi: 10.1056/NEJM199711203372103. [DOI] [PubMed] [Google Scholar]
- 45.Visetti E, Pastorelli M, Bruno M. Severe accidental hypothermia successfully treated by warmed peritoneal lavage. Minerva Anestesiol. 1998;64(10):471–475. [PubMed] [Google Scholar]
- 46.Aslam A.F, Aslam A.K, Vasavada B.C, Khan I.A. Hypothermia: evaluation, electrocardiographic manifestations, and management. Am J Med. 2006;119(4):297–301. doi: 10.1016/j.amjmed.2005.09.062. [DOI] [PubMed] [Google Scholar]
- 47.Collins A.M, Danzl D.F. Hypothermia with profound anemia and pancreatitis. Wilderness Environ Med. 2006;17(1):31–35. doi: 10.1580/pr34-04.1. [DOI] [PubMed] [Google Scholar]
- 48.Biem J, Koehncke N, Classen D, Dosman J. Out of the cold: management of hypothermia and frostbite. CMAJ. 2003;168(3):305–311. [PMC free article] [PubMed] [Google Scholar]
- 49.Bird D. Identification and management of frostbite injuries. Emerg Nurse. 2000;7(8):17–19. doi: 10.7748/en1999.12.7.8.17.c1305. [DOI] [PubMed] [Google Scholar]
- 50.Murphy J.V, Banwell P.E, Roberts A.H.N, McGrouther D.A. Frostbite: pathogenesis and treatment. J Trauma. 2000;48(1):171–178. doi: 10.1097/00005373-200001000-00036. [DOI] [PubMed] [Google Scholar]
- 51.Bruen K.J, Ballard J.R, Morris S.E, Cochran A, Edelman L.S, Saffle J.R. Reduction of the incidence of amputation in frostbite injury with thrombolytic therapy. Arch Surg. 2007;142(6):546–551. doi: 10.1001/archsurg.142.6.546. [DOI] [PubMed] [Google Scholar]
- 52.Toner M.M, McArdle W.D. Human thermoregulatory responses to acute cold stress with special reference to water immersion. In: Fregly M.J, Blatteis C.M, editors. Handbook of Physiology: Environmental. New York, NY: Oxford Press; 1996. pp. 379–397. Vol 1. [Google Scholar]
- 53.Ferretti G, Veicsteinas A, Rennie D.W. Conductive and convective heat flows of exercising humans in cold water. J Appl Phsyiol. 1989;67(6):2473–2480. doi: 10.1152/jappl.1989.67.6.2473. [DOI] [PubMed] [Google Scholar]
- 54.Toner M.M, Sawka M.N, Pandolf K.B. Thermal responses during arm and leg and combined arm-leg exercise in water. J Appl Physiol. 1984;56(5):1355–1360. doi: 10.1152/jappl.1984.56.5.1355. [DOI] [PubMed] [Google Scholar]
- 55.Kaufman W.C, Bothe D.J. Wind chill reconsidered, Siple revisited. Aviat Space Environ Med. 1986;57(1):23–26. [PubMed] [Google Scholar]
- 56.Weller A.S, Millard C.E, Stroud M.A, Greenhaff P.L, Macdonald I.A. Physiological responses to cold stress during prolonged intermittent low- and high-intensity walking. Am J Physiol. 1997;272(6, pt 2):R2025–R2033. doi: 10.1152/ajpregu.1997.272.6.R2025. [DOI] [PubMed] [Google Scholar]
- 57.Lee D.T, Toner M.M, McArdle W.D, Vrabas J.S, Pandolf K.B. Thermal and metabolic responses to cold-water immersion at knee, hip, and shoulder levels. J Appl Physiol. 1997;82(5):1523–1530. doi: 10.1152/jappl.1997.82.5.1523. [DOI] [PubMed] [Google Scholar]
- 58.Young A.J, Castellani J.W, Sawka M.N. Human physiological responses to cold exposure. In: Nose H, Nadel E.R, Morimoto T, editors. Proceedings of 1997 Nagano Symposium on Sports Science. Carmel, IN: Cooper Publishing Group; 1998. pp. 273–286. [Google Scholar]
- 59.Jacobs I, Martineau L, Vallerand A.L. Thermoregulatory thermogenesis in humans during cold stress. Exerc Sports Sci Rev. 1994;22:221–250. [PubMed] [Google Scholar]
- 60.Tikuisis P, Bell D.G, Jacobs I. Shivering onset, metabolic response, and convective heat transfer during cold air exposure. J Appl Physiol. 1991;70(5):1996–2002. doi: 10.1152/jappl.1991.70.5.1996. [DOI] [PubMed] [Google Scholar]
- 61.Rothwell N.J. CNS regulation of thermogenesis. Crit Rev Neurobiol. 1994;8(1–2):1–10. [PubMed] [Google Scholar]
- 62.Savage M.V, Brengelmann G.L. Control of skin blood flow in the neutral zone of human body temperature regulation. J Appl Physiol. 1996;80(4):1249–1257. doi: 10.1152/jappl.1996.80.4.1249. [DOI] [PubMed] [Google Scholar]
- 63.Veicsteinas A, Ferretti G, Rennie D.W. Superficial shell insulation in resting and exercising men in cold water. J Appl Physiol. 1982;52(6):1557–1564. doi: 10.1152/jappl.1982.52.6.1557. [DOI] [PubMed] [Google Scholar]
- 64.O'Brien C. Reproducibility of the cold-induced vasodilation response in the human finger. J Appl Physiol. 2005;98(4):1334–1340. doi: 10.1152/japplphysiol.00859.2004. [DOI] [PubMed] [Google Scholar]
- 65.Danzl D.F, Pozos R.S, Hamlet M.P. Accidental hypothermia. In: Auerbach P.A, editor. Wilderness Medicine: Management of Wilderness and Environmental Emergencies. St Louis, MO: Mosby; 1995. pp. 51–103. 3rd ed. [Google Scholar]
- 66.Danzl D.F. Frostbite. In: Marx J.A, editor. Rosen's Emergency Medicine: Concepts and Clinical Practice. St Louis, MO: Mosby; 2006. pp. 2228–2236. Vol 3. [Google Scholar]
- 67.McCauley R.L, Smith D.J, Jr, Robson M.C, Heggers J.P. Frostbite and other cold-induced injuries. In: Auerbach P.A, editor. Wilderness Medicine: Management of Wilderness and Environmental Emergencies. St Louis, MO: Mosby; 1995. pp. 129–145. 3rd ed. [Google Scholar]
- 68.Charkoudian N. Skin blood flow in adult human thermoregulation: how it works, when it does not, and why. Mayo Clin Proc. 2003;78(5):603–612. doi: 10.4065/78.5.603. [DOI] [PubMed] [Google Scholar]
- 69.Healy J.D. Excess winter mortality in Europe: a cross country analysis identifying key risk factors. J Epidemiol Community Health. 2003;57(10):784–789. doi: 10.1136/jech.57.10.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Freund B.J, Sawka M.N. Influence of cold stress on human fluid balance. In: Marriot B.M, Carlson S.J, editors. Nutritional Needs in Cold and High-Altitude Environments: Applications for Military Personnel in Field Operations. Washington, DC: National Academy Press; 1996. pp. 161–180. [PubMed] [Google Scholar]
- 71.O'Brien C, Young A.J, Sawka M.N. Hypohydration and thermoregulation in cold air. J Appl Physiol. 1998;84(1):185–189. doi: 10.1152/jappl.1998.84.1.185. [DOI] [PubMed] [Google Scholar]
- 72.Layden J.D, Patterson M.J, Nimmo M.A. Effects of reduced ambient temperature on fat utilization during submaximal exercise. Med Sci Sports Exerc. 2002;34(5):774–779. doi: 10.1097/00005768-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 73.Makinen T.T, Gavhed D, Holmer I, Rintamaki H. Effects of metabolic rate on thermal responses at different air velocities in −10°C. Comp Biochem Physiol A Mol Integr Physiol. 2001;128(4):759–768. doi: 10.1016/s1095-6433(01)00281-1. [DOI] [PubMed] [Google Scholar]
- 74.Fellows I.W, Macdonald I.A, Bennett T, Allison S.P. The effect of undernutrition on thermoregulation in the elderly. Clin Sci (Lond) 1985;69(5):525–532. doi: 10.1042/cs0690525. [DOI] [PubMed] [Google Scholar]
- 75.Ainslie P.N, Campbell I.T, Lambert J.P, MacLaren D.P.M, Reilly R. Physiological and metabolic aspects of very prolonged exercise with particular reference to hill walking. Sports Med. 2005;35(7):619–647. doi: 10.2165/00007256-200535070-00006. [DOI] [PubMed] [Google Scholar]
- 76.Tikuisis P, Ducharme M.B, Moroz D, Jacobs I. Physiological responses of exercised-fatigued individuals exposed to wet-cold conditions. J Appl Physiol. 1999;86(4):1319–1328. doi: 10.1152/jappl.1999.86.4.1319. [DOI] [PubMed] [Google Scholar]
- 77.Castellani J.W, Young A.J, Sawka M.N, Pandolf K.B. Human thermoregulatory responses during serial cold water immersions. J Appl Physiol. 1998;85(1):204–209. doi: 10.1152/jappl.1998.85.1.204. [DOI] [PubMed] [Google Scholar]
- 78.Young A.J, Castellani J.W, O'Brien C, et al. Exertional fatigue, sleep loss, and negative energy balance increase susceptibility to hypothermia. J Appl Physiol. 1998;85(4):1210–1217. doi: 10.1152/jappl.1998.85.4.1210. [DOI] [PubMed] [Google Scholar]
- 79.Castellani J.W, Young A.J, Degroot D.W, et al. Thermoregulation during cold exposure after several days of exhaustive exercise. J Appl Physiol. 2001;90(3):939–946. doi: 10.1152/jappl.2001.90.3.939. [DOI] [PubMed] [Google Scholar]
- 80.Castellani J.W, Stulz D.A, Degroot D.W, et al. Eighty-four hours of sustained operations alter thermoregulation during cold exposure. Med Sci Sports Exerc. 2003;35(1):175–181. doi: 10.1097/00005768-200301000-00026. [DOI] [PubMed] [Google Scholar]
- 81.Fox G.R, Hayward J.S, Hobson G.N. Effect of alcohol on thermal balance of man in cold water. Can J Physiol Pharmacol. 1979;57(8):860–865. doi: 10.1139/y79-131. [DOI] [PubMed] [Google Scholar]
- 82.Centers for Disease Control and Prevention (CDC) Hypothermia-related deaths, United States, 2003–2004. MMWR Morb Mortal Wkly Rep. 2005;54(7):173–175. [PubMed] [Google Scholar]
- 83.Glickman-Weiss E.L, Nelson A.G, Hearon C.M, Goss F.L, Robertson R.J, Cassinelli D.A. Effects of body morphology and mass on thermal responses to cold water: revisited. Eur J Appl Physiol Occup Physiol. 1993;66(4):299–303. doi: 10.1007/BF00237772. [DOI] [PubMed] [Google Scholar]
- 84.Glickman-Weiss E.L, Nelson A.G, Hearon C.M, Prisby R, Caine N. Thermal and metabolic responses of women with high fat versus low fat body composition during exposure to 5 and 27°C for 120 minutes. Aviat Space Environ Med. 1999;70(3, pt 1):284–288. [PubMed] [Google Scholar]
- 85.Prisby R, Glickman-Weiss E.L, Nelson A.G, Caine N. Thermal and metabolic responses of high and low fat women to cold water immersion. Aviat Space Environ Med. 1999;70(9):887–891. [PubMed] [Google Scholar]
- 86.Tikuisis P, Gonzalez R.R, Oster R.A, Pandolf K.B. Role of body fat in the prediction of the metabolic response for immersion in cold water. Undersea Biomed Res. 1988;15(2):123–134. [PubMed] [Google Scholar]
- 87.Moriya K, Suda T, Hattori M, Yokoyama S. The correlation of thermoregulatory reactions in young men exposure to cold air with their physical fitness. Jpn J Biometeorol. 1993;30:77–84. [Google Scholar]
- 88.Savourey G, Bittel J. Thermoregulatory changes in the cold induced by physical training in humans. Eur J Appl Physiol Occup Physiol. 1998;78(5):379–384. doi: 10.1007/s004210050434. [DOI] [PubMed] [Google Scholar]
- 89.Sugahara M, Taimura A. Relationship between thermoregulation and cold induced vasodilation during cold exposure with regard to maximal oxygen uptake. Jpn J Phys Fitness Sports Med. 1996;46(1):101–110. [Google Scholar]
- 90.Jacobs I, Romet T, Frim J, Hynes A. Effects of endurance fitness on responses to cold water immersion. Aviat Space Environ Med. 1984;55(8):715–720. [PubMed] [Google Scholar]
- 91.Bittel J.H.M, Nonotte-Varly C, Livecchi-Gonnot G.H, Savourey G.L.M.J, Hanniquet A.M. Physical fitness and thermoregulatory reactions in a cold environment in men. J Appl Physiol. 1988;65(5):1984–1989. doi: 10.1152/jappl.1988.65.5.1984. [DOI] [PubMed] [Google Scholar]
- 92.McArdle W.D, Magel J.R, Gergley T.J, Spina R.J, Toner M.M. Thermal adjustment to cold-water exposure in resting men and women. J Appl Physiol. 1984;56(6):1565–1571. doi: 10.1152/jappl.1984.56.6.1565. [DOI] [PubMed] [Google Scholar]
- 93.McArdle W.D, Magel J.R, Spina R.J, Gergley T.J, Toner M.M. Thermal adjustment to cold-water exposure in exercising men and women. J Appl Physiol. 1984;56(6):1572–1577. doi: 10.1152/jappl.1984.56.6.1572. [DOI] [PubMed] [Google Scholar]
- 94.Graham T.E. Thermal, metabolic and cardiovascular changes in men and women during cold stress. Med Sci Sports Exerc. 1998;20(5 suppl):S185–S192. doi: 10.1249/00005768-198810001-00017. [DOI] [PubMed] [Google Scholar]
- 95.Holmer I. Assessment of cold stress in terms of required clothing insulation-IREQ. Int J Indust Ergon. 1988;3(2):159–166. [Google Scholar]
- 96.International Organization for Standardization. Ergonomics of the Thermal Environment: Estimation of the Thermal Insulation and Evaporative Resistance of A Clothing Ensemble. Geneva, Switzerland: International Organization for Standardization; 1993. ISO 9920. [Google Scholar]
- 97.Froese G, Burton A.C. Heat losses from the human head. J Appl Physiol. 1957;10(2):235–241. doi: 10.1152/jappl.1957.10.2.235. [DOI] [PubMed] [Google Scholar]
- 98.Langdeau J.B, Boulet L.P. Prevalence and mechanisms of development of asthma and airway hyperresponsiveness in athletes. Sports Med. 2001;31(8):601–616. doi: 10.2165/00007256-200131080-00005. [DOI] [PubMed] [Google Scholar]
- 99.Storms W.W. Review of exercise-induced asthma. Med Sci Sports Exerc. 2003;35(9):1464–1470. doi: 10.1249/01.MSS.0000084533.75912.B4. [DOI] [PubMed] [Google Scholar]
- 100.Helenius I.J, Tikkanen H.O, Haahtela T. Occurrence of exercise induced bronchospasm in elite runners: dependence on atopy and exposure to cold air and pollen. Br J Sports Med. 1998;32(2):125–129. doi: 10.1136/bjsm.32.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zeitoun M, Wilk B, Matsuzaka A, Knopfli B.H, Wilson B.A, Bar-Or O. Facial cooling enhances exercise-induced bronchoconstriction in asthmatic children. Med Sci Sports Exerc. 2004;36(5):767–771. doi: 10.1249/01.mss.0000126466.67458.5b. [DOI] [PubMed] [Google Scholar]
- 102.Wilber R.L, Rundell K.W, Szmedra L, Jenkinson D.M, Im J, Drake S.D. Incidence of exercise-induced bronchospasm in Olympic winter sport athletes. Med Sci Sports Exerc. 2000;32(4):732–737. doi: 10.1097/00005768-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 103.Evans T.M, Rundell K.W, Beck K.C, Levine A.M, Baumann J.M. Cold air inhalation does not affect the severity of EIB after exercise or eucapnic voluntary hyperventilation. Med Sci Sports Exerc. 2005;37(4):544–549. doi: 10.1249/01.mss.0000158186.32450.ec. [DOI] [PubMed] [Google Scholar]
- 104.Davies C.T.M, Fohlin L, Thoren C. Temperature regulation in anorexia nervosa [proceedings] J Physiol (Lond) 1977;268(1):8P–9P. [PubMed] [Google Scholar]
- 105.Luck P, Wakeling A. Increased cutaneous vasoreactivity to cold in anorexia nervosa. Clin Sci (Colch) 1981;61(5):559–567. doi: 10.1042/cs0610559. [DOI] [PubMed] [Google Scholar]
- 106.Beard J.L, Borel M.J, Derr J. Impaired thermoregulation and thyroid function in iron-deficiency anemia. Am J Clin Nutr. 1990;52(5):813–819. doi: 10.1093/ajcn/52.5.813. [DOI] [PubMed] [Google Scholar]
- 107.Neittaanmaki H. Cold urticaria: clinical findings in 200 patients. J Am Acad Dermatol. 1985;13(4):636–644. doi: 10.1016/s0190-9622(85)70208-3. [DOI] [PubMed] [Google Scholar]
- 108.Epstein S.E, Stampfer M, Beiser G.D, Goldstein R.E, Braunwald E. Effects of a reduction in environmental temperature on the circulatory response to exercise in man: implications concerning angina pectoris. New Engl J Med. 1969;280(1):7–11. doi: 10.1056/NEJM196901022800102. [DOI] [PubMed] [Google Scholar]
- 109.Neill W.A, Duncan D.A, Kloster F, Mahler D.J. Response of coronary circulation to cutaneous cold. Am J Med. 1974;56(4):471–476. doi: 10.1016/0002-9343(74)90478-1. [DOI] [PubMed] [Google Scholar]
- 110.Ducharme M.B, Lounsbury D.S. Self-rescue swimming in cold water: the latest advice. J Appl Physiol Nutr Metab. 2007;32(4):799–807. doi: 10.1139/H07-042. [DOI] [PubMed] [Google Scholar]
- 111.Young A.J. Homeostatic responses to prolonged cold exposure: human cold acclimatization. In: Fregly M.J, Blatteis C.M, editors. Handbook of Physiology: Environmental. New York, NY: Oxford Press; 1996. pp. 419–438. Vol. 1. [Google Scholar]
- 112.Sloan R.E.G, Keatinge W.R. Cooling rates of young people swimming in cold water. J Appl Physiol. 1973;35(3):371–375. doi: 10.1152/jappl.1973.35.3.371. [DOI] [PubMed] [Google Scholar]
- 113.Smolander J, Bar-Or O, Korhonen O, Ilmarinen J. Thermoregulation during rest and exercise in the cold in pre- and early pubescent boys and young men. J Appl Physiol. 1992;72(4):1589–1594. doi: 10.1152/jappl.1992.72.4.1589. [DOI] [PubMed] [Google Scholar]
- 114.Thompson-Torgerson C.S, Holowatz S.A, Kenney W.L. Altered mechanisms of thermoregulatory vasoconstriction in aged human skin. Exerc Sports Science Rev. 2008;36(3):122–127. doi: 10.1097/JES.0b013e31817bfd47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Holmer I. Strategies for prevention of cold stress in the elderly. Int J Circumpolar Health. 2000;59(3–4):267–272. [PubMed] [Google Scholar]
- 116.Potkanowicz E.S, Caine-Bish N, Otterstetter R, Glickman E.L. Age effects on thermal, metabolic, and perceptual responses to acute cold exposure. Aviat Space Environ Med. 2003;74(11):1157–1162. [PubMed] [Google Scholar]
- 117.Ferrara M.S, Buckley W.E, Peterson C.L. Epidemiology of sport related injuries for athletes with disability. Athl Ther Today. 1997;2(1):28–33. [Google Scholar]
- 118.Colachis S.C., III Hypothermia associated with autonomic dysreflexia after traumatic spinal cord injury. Am J Phys Med Rehabil. 2002;81(3):232–235. doi: 10.1097/00002060-200203000-00013. [DOI] [PubMed] [Google Scholar]
- 119.Aguilera E.J, Glenn A.M, Lynch W.J, Molinari C.J, Jr, Nguyen C.H. Exposure hypothermia and the winter SCI participant. J Am Paraplegia Soc. 1987;10(1):14–17. doi: 10.1080/01952307.1987.11719629. [DOI] [PubMed] [Google Scholar]
- 120.Dykes R.W, Saddiki-Traki F, Tremblay N, Boureau F, Morel-Fatio X. Differences in the sensations of cold on the anterior torso of control and spinal-cord-transected individuals. Behav Neurosci. 2006;120(2):463–473. doi: 10.1037/0735-7044.120.2.463. [DOI] [PubMed] [Google Scholar]
- 121.Krassioukov A, Wolfe D.L, Hsieh J.T, Hayes K.C, Durham C.E. Quantitative sensory testing in patients with incomplete spinal cord injury. Arch Phys Med Rehabil. 1999;80(10):1258–1263. doi: 10.1016/s0003-9993(99)90026-6. [DOI] [PubMed] [Google Scholar]
- 122.Claus-Walker J, Halstead L.S. Metabolic and endocrine changes in spinal cord injury, II (section 1): consequences of partial decentralization of the autonomic nervous system. Arch Phys Med Rehabil. 1982;63(11):569–575. [PubMed] [Google Scholar]
- 123.Sawka M.N, Latzka W.A, Pandolf K.B. Temperature regulation during upper body exercise: able-bodied and spinal cord injured. Med Sci Sports Exerc. 1989;21(5 suppl):S132–S140. [PubMed] [Google Scholar]
- 124.Nicotra A, Young T.M, Asahina M, Mathias C.J. The effect of different physiological stimuli on skin vasomotor reflexes above and below the lesion in human chronic spinal cord injury. Neurorehabil Neural Repair. 2005;19(4):325–331. doi: 10.1177/1545968305281210. [DOI] [PubMed] [Google Scholar]
- 125.Mizushima T, Tajima F, Okawa H, Umezu Y, Furusawa K, Ogata H. Cardiovascular and endocrine responses during the cold pressor test in subjects with cervical spinal cold injuries. Arch Phys Med Rehabil. 2003;84(1):112–118. doi: 10.1053/apmr.2003.50072. [DOI] [PubMed] [Google Scholar]
- 126.Shirado O, Shundo M, Kaneda K, Strax T.E. Outdoor winter activities of spinal-cord injured patients: with special reference to outdoor mobility. Am J Phys Med Rehabil. 1995;74(6):408–414. doi: 10.1097/00002060-199511000-00002. [DOI] [PubMed] [Google Scholar]
- 127.Finnerup N.B, Gyldensted C, Fuglsang-Frederiksen A, Bach F.W, Jensen T.S. Sensory perception in complete spinal cord injury. Acta Neurol Scand. 2004;109(3):194–199. doi: 10.1034/j.1600-0404.2003.00219.x. [DOI] [PubMed] [Google Scholar]