Abstract
Context: One in four hospitalized patients has diagnosed diabetes. The prevalence of unrecognized, or undiagnosed, diabetes among hospitalized patients is not well established.
Objective: Our objective was to determine the prevalence of unrecognized probable diabetes in this patient population determined by elevated hemoglobin A1c (HbA1c) level.
Design: We conducted a prospective observational cohort trial with retrospective follow-up of patients with elevated HbA1c levels and no diagnosis of diabetes. HbA1c levels were obtained for all patients.
Setting: The study was conducted at an acute care general hospital.
Patients: Patients included 695 adult, nonobstetric patients admitted on 11 d in 2006.
Main Outcome Measures: Outcome measures included rate of unrecognized probable diabetes, defined as admission HbA1c of more than 6.1% and no diagnosis of diabetes or treatment with antidiabetic medications before or during their admission and rate of unrecognized diabetes 1 yr after discharge.
Results: Eighteen percent of hospitalized patients had elevated HbA1c levels without a diagnosis of diabetes. Random glucose levels poorly predicted elevated HbA1c levels (area under receiver operating characteristic curve, 0.60). Neither diagnosed diabetes nor HbA1c level was associated with length of stay or costs (P > 0.1 for all comparisons). Only 15% of patients with elevated HbA1c levels who continued to receive care within the system studied had diabetes diagnosed in the year after the index admission.
Conclusions: Nearly one in five adult patients admitted to a large general hospital had unrecognized probable diabetes, based on elevated HbA1c levels. Random glucose levels during the hospital stay were poorly predictive of this condition. Few hospitalized patients with elevated HbA1c levels were diagnosed within the year after admission.
Eighteen percent of patients admitted to a general hospital had undiagnosed diabetes, but only 15% of these patients with follow-up data available had evaluation for, or diagnosis of, diabetes within the year following admission.
Approximately one quarter of patients admitted to the hospital have diabetes (1). In response to both observational studies (2,3,4,5) and randomized trials (6,7) that have shown decreased mortality with tight glycemic control among inpatients in various settings, many physician groups and regulatory agencies have called for improving inpatient diabetes management (8,9,10). Because patients with type 2 diabetes have a high rate of complications at diagnosis (11,12,13), one important component of improved inpatient diabetes management may be screening of high-risk inpatients to prevent diabetes-related morbidity in the years after discharge.
Diabetes in the outpatient setting is typically diagnosed based on blood glucose testing. However, hyperglycemia is common among hospitalized patients even in the absence of diabetes (stress hyperglycemia) (14). The relationship of stress hyperglycemia to unrecognized diabetes and, therefore, the true prevalence of undiagnosed diabetes among hospitalized patients varies by population. Estimates of this condition have ranged from 1.9% in general inpatients based on fasting plasma glucose (15) to 18% of acute myocardial infarction patients based on an oral glucose tolerance test 3 months after discharge (16) in European samples.
In contrast to glucose testing in the acute setting, hemoglobin A1c (HbA1c) testing allows determination of mean levels of glycemia, relatively unperturbed by the acute stress of hospitalization, and therefore represents a useful test for identifying diabetes in the hospital setting. HbA1c has been validated for the diagnosis of diabetes in hospitalized patients with random plasma glucose of at least 126 mg/dl (17). In addition, HbA1c levels greater than 2 sd above the population mean (∼6.1%) have a high sensitivity for diabetes diagnosed by fasting plasma glucose of at least 126 mg/dl in two NHANES cohorts (18,19). Elevation in HbA1c levels at baseline correlates with the likelihood of developing hyperglycemia under stress (20).
The prevalence of unrecognized diabetes is estimated to be 3.3–4.5% of the general outpatient population over 40 yr of age (19,21,22), with an annual incidence of diabetes of 7.8% in subjects with HbA1c of at least 6.1%. We hypothesized that the prevalence of unrecognized diabetes, characterized by elevated HbA1c levels and no diabetes diagnosis, would be higher among patients admitted to the hospital. We sought to determine the prevalence of this condition among an unselected population of patients admitted to a U.S. acute care hospital, to describe characteristics of these patients, and to determine rates of follow-up to target groups for future screening and intervention.
Patients and Methods
Study design, setting, and participants
We performed a cohort study to determine the prevalence of previously unrecognized probable diabetes among inpatients. The cohort was drawn from all adult nonobstetric admissions to Massachusetts General Hospital, a 900-bed acute care general hospital in Boston, MA, during 11 d (weekdays and weekends) of July and August 2006 (n = 945). We included patients who had an available blood sample on which to measure HbA1c level (n = 716) and excluded patients who were admitted for observation only (n = 21), leaving a final sample size of 695 patients. The Partners Healthcare Institutional Review Board approved this study as a quality improvement study; HbA1c levels were determined for research purposes. Patients and providers did not have access to results.
Diagnosis of diabetes
In addition to using billing codes for diabetes excluding gestational diabetes, patients with previously diagnosed diabetes were identified by any mention of diabetes in the text of the full admission note or discharge summary or the presence of any hypoglycemic medications in the admission medications. Type 1 diabetes was identified by chart review notation of type 1 diabetes. We measured HbA1c levels from available admission blood samples to identify patients with undiagnosed diabetes. The HbA1c assay reflects mean glucose levels integrated over the previous 2–3 months and is relatively unaffected by the perturbations in glucose levels associated with acute illness (17,23). HbA1c was measured with a HPLC method that serves as one of the primary reference methods for the National Glycohemoglobin Standardization Program (24), is aligned to the Diabetes Control and Complications Trial standard assay, and has intra- and interassay coefficients of variation less than 2.0%. HbA1c higher than 6.1% (2 sd above the nondiabetic mean) was used as a diagnostic level for diabetes, with HbA1c higher than 6.5% (3 sd above the nondiabetic mean) used for sensitivity analyses. These HbA1c levels have specificity for diabetes in Caucasians, compared with fasting glucose levels of more than 126 mg/dl in outpatients, of 97.4 and 99.6%, respectively (18); similar results were found in a subsequent study (19). In a separate study of hospitalized patients with random glucose levels of at least 126 mg/dl in the emergency department who subsequently underwent fasting glucose or outpatient oral glucose tolerance testing, HbA1c levels greater than 6% were 100% specific for diabetes (17). We classified patients without diabetes as those with HbA1c of 6.1% or less who were not prescribed hypoglycemic medications and did not carry a diagnosis of diabetes in medical records or billing codes.
Demographic and clinical variables
Demographic characteristics including age, sex, race, length of stay, admission service, admission unit [intensive care unit (ICU) (n = 105) or non-ICU], and cost data were obtained from hospital electronic data repositories. The maximum glucose values from laboratory testing during the index admission were obtained from the central laboratory data repository. Comorbidity data for all patients were obtained electronically from discharge billing codes associated with the index admission and were used to calculate Charlson scores (25). A trained nurse reviewer abstracted individual patient records to collect data on comorbidities and medications among patients with HbA1c levels higher than 6.1% and no known diagnosis of diabetes at the time of admission to confirm that diabetes had not been recognized during the admission. Random glucose levels obtained in the course of routine care (with no indication of carbohydrate exposure) were evaluated in relation to HbA1c levels.
A physician reviewer (D.J.W.) reviewed all available records of patients with unrecognized diabetes to determine their clinical course in the year after the index admission. Of the 123 patients with undiagnosed diabetes, 21 could reasonably be considered moribund (life-threatening illness leading to hospice or death within 1 yr) at the time of admission and were excluded from analysis of diabetes-specific follow-up. Seventy-one of the remaining 102 patients (70%) had continuing care within the hospital-affiliated healthcare system, defined as any follow-up office note available for review in the electronic medical record. For these 71 patients, we considered diabetes to have been recognized if HbA1c level was obtained in the routine course of care or if diabetes or a diabetes-specific medication was listed in physician notes within 1 yr of the index admission.
Statistical methods
Prevalence of diabetes and unrecognized probable diabetes was calculated for the overall sample and by service, with sensitivity analyses excluding moribund (n = 21) and steroid-treated patients (n = 18) from the group with elevated HbA1c levels without a diabetes diagnosis. For categorical variables, differences in patient characteristics by diabetes diagnosis group were estimated using χ2 tests in 3 by x contingency tables. For between-group comparisons, 2 by 2 contingency tables were used to determine the χ2 P-value, which was then multiplied by 2. ANOVA was used to determine differences in patient groups for continuous variables, with Tukey adjustment for between-group comparisons. A receiver operating characteristic curve demonstrated the ability of random glucose levels to predict probable diabetes diagnosis, excluding patients with diagnosed diabetes, and using HbA1c of more than 6.1% as the criterion of probable diabetes. Logistic regression modeling was used to determine predictors of elevated HbA1c levels in patients without a diabetes diagnosis. Charlson score was included as a variable in this analysis; patients with previously recognized diabetes, which contributes to the calculation of the Charlson score, were excluded. SAS version 9.1 was used for all analyses.
Role of the funding source
The study was funded by Massachusetts General Hospital, which had no role in the data analysis.
Results
Characteristics of sample
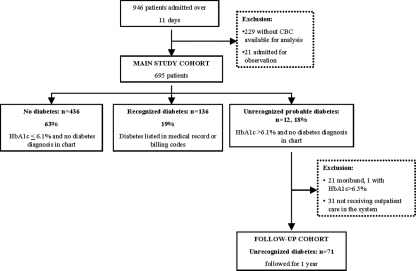
Of 945 patients admitted over the 11 d of observation, 170 patients had known diabetes (18%). Six hundred ninety-five admitted patients, including 136 with previously diagnosed diabetes (19%), had available blood samples for HbA1c measurement and constituted the final study sample (Fig. 1). Patients with available samples were older (61 ± 17 vs. 56 ± 17 yr, P < 0.0001), more likely to be ensured by Medicare (50 vs. 43% private insurance, P = 0.03 for comparison across all insurance categories), and more likely to be admitted to a medical service than patients without available samples but did not differ by sex, race, or rate of known diagnosis of diabetes.
Figure 1.
Study population. CBC, Complete blood count.
Patients with unrecognized probable diabetes
The overall prevalence of elevated HbA1c levels without a diabetes diagnosis in the inpatient population was 18% (123 of 695 patients). Thirty-three of these patients, or 5% of the overall sample, had HbA1c levels higher than 6.5%. Of patients with elevated HbA1c levels and no diabetes diagnosis, 18 (15%) were on glucocorticoids, and 11 of these patients had HbA1c levels higher than 6.5%. Twenty-one (17%) died within the year after admission. Exclusion of steroid-treated or moribund patients from this group only did not change the prevalence of undiagnosed probable diabetes (18% for both calculations).
Patients with elevated HbA1c levels and no diabetes diagnosis were older than patients without diabetes and were more likely to be female than patients without diabetes or with known diabetes but were not significantly different with regard to race (Table 1). Patients with unrecognized probable diabetes were more likely to have heart disease, particularly congestive heart failure, and peripheral vascular disease than patients without diabetes, whereas patients with known diabetes were more likely to have renal disease than patients with unrecognized probable diabetes (Table 1). Thirty-one percent of patients with elevated HbA1c levels and no diabetes diagnosis had a Charlson score greater than or equal to 3, compared with 20% of patients without diabetes (P < 0.0001). Fifty-two percent of patients with diabetes had Charlson scores greater than or equal to 3, but diabetes itself increases the Charlson score.
Table 1.
Characteristics of patients without diabetes (group 1), with unrecognized probable diabetes (group 2), and with known diabetes (group 3) by HbA1c and chart review
| Group 1: no diabetes; n = 436 (63%) | Group 2: unrecognized probable diabetes; n = 123 (18%) | Group 3: recognized diabetes; n = 136 (19%) | P value across groupsa | P value: difference between groups 1 and 2b | P value: difference between groups 2 and 3b | |
|---|---|---|---|---|---|---|
| Age (yr) | 59 ± 18 | 67 ± 15 | 64 ± 15 | <0.0001 | <0.0001 | 0.3 |
| Female sex | 51% | 58% | 35% | 0.0002 | 0.3 | 0.0002 |
| White race | 88% | 86% | 82% | 0.3 | 0.7 | 0.99 |
| HbA1c | 5.57 ± 0.39 | 6.48 ± 0.41 | 7.40 ± 1.66 | <0.0001 | <0.0001 | <0.0001 |
| Comorbidity by billing code | ||||||
| CVD, MI, or CHF | 19% | 29% | 35% | <0.0001 | 0.02 | 0.6 |
| PVD | 8% | 20% | 16% | 0.0003 | 0.0002 | 0.8 |
| COPD | 17% | 27% | 19% | 0.06 | 0.04 | 0.3 |
| Renal disease | 6% | 11% | 23% | <0.0001 | 0.1 | 0.01 |
| Charlson score | 13.3 ± 2.6 | 4.3 ± 2.5 | 5.1 ± 2.5 | <0.0001 | 0.0004 | 0.05 |
| Insurance | ||||||
| Commercial | 49% | 44% | 38% | 0.03 | 0.3 | 0.99 |
| Medicare | 41% | 50% | 56% | |||
| Medicaid | 5% | 6% | 4% | |||
| Free care | 4% | 1% | ||||
| Hospital use | ||||||
| Length of stay | 5.3 ± 5.8 | 5.9 ± 7.4 | 5.4 ± 6.7 | 0.7 | 0.7 | 0.08 |
| Total charges | $51,007 ± 76,202 | $55,008 ± 73,075 | $46,523 ± 40,913 | 0.6 | 0.8 | 0.6 |
Undiagnosed probable diabetes is defined as HbA1c of more than 6.1% with no indication of diabetes in the medical record. CHF, Congestive heart failure; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; MI, myocardial infarction; PVD, peripheral vascular disease.
P value by χ2 for categorical data and ANOVA for continuous data.
Difference between Tukey-Kramer adjusted P value for difference between groups for continuous variables and χ2 P value multiplied by 2 for categorical variables.
Prevalence of diabetes and unrecognized diabetes by service
The prevalence of elevated HbA1c levels without a diabetes diagnosis was very similar across cardiology (19%), medicine (19%), and surgical (18%) services (P = 0.1). By contrast, the prevalence of known diabetes among hospitalized patients differed by service and was highest on dedicated cardiology services (29%), followed by medicine (22%) and surgical (16%) services (P = 0.003 for difference among services). The prevalence of unrecognized probable diabetes (general settings 17% vs. ICU 20%, P = 0.7) and prevalence of known diabetes were similar between non-ICU (or general) and ICU settings (19 vs. 17%, P = 0.7).
Random glucose levels among patients with unrecognized probable diabetes
Of the cohort of 695 patients, 609 had plasma glucose levels drawn as part of routine care while inpatients, allowing some estimation of the relationship of random glucose levels to diabetes diagnosis category. A greater fraction of patients with known diabetes had glucose levels over 200 mg/dl (50%) than patients with unrecognized probable diabetes (18%) or no diabetes (13%, P < 0.0001 for comparison across the three groups), but between-group comparisons showed that patients with undiagnosed probable diabetes were not significantly more likely to have hyperglycemia to this degree than patients without diabetes. The prevalence of glucose levels higher than 200 mg/dl was 4-fold higher among ICU patients than non-ICU patients (56 vs. 14%, P < 0.0001). In the ICU, the prevalence of glucose levels higher than 200 mg/dl did not differ among patients without diabetes, with unrecognized probable diabetes, and with diabetes (P = 0.08).
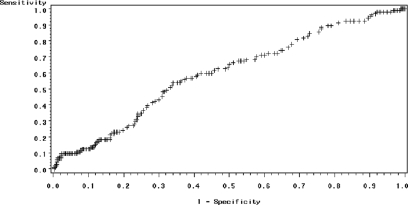
Random glucose levels, accordingly, were insensitive and nonspecific for the diagnosis of diabetes: only 17% of patients with elevated HbA1c levels and no diabetes diagnosis had a random glucose greater than 200 mg/dl, the outpatient diagnostic criterion for diabetes. The sensitivity and specificity of random inpatient serum glucose levels for the diagnosis of diabetes defined by HbA1c level of more than 6.1% (excluding patients with known diabetes) is shown in the receiver operating characteristic curve in Fig. 2 (area under the curve = 0.6). The positive predictive value of random glucose greater than 200 mg/dl for unrecognized probable diabetes was 52%, whereas the negative predictive value was 87%.
Figure 2.
Receiver operating curve: random glucose and undiagnosed diabetes. Area under the curve = 0.60. P value for glucose predicting unrecognized probable diabetes = 0.07.
Logistic regression models predicting unrecognized probable diabetes showed that glucose levels greater than 150 mg/dl and older age were associated with increased risk of unrecognized probable diabetes, controlling for Charlson score as an index of chronic illness that might contribute to stress hyperglycemia (Table 2). Thirty-one percent of patients without diagnosed diabetes had a random glucose level greater than 150 mg/dl while hospitalized.
Table 2.
Model including significant predictors of elevated HbA1c levels among patients without diagnosed diabetes
| Variables in model | Odds ratio | 95% Wald confidence limits |
|---|---|---|
| Female (vs. male as referent) | 1.3 | 0.8–1.9 |
| Age 46–65 yr, vs. <46 yr | 2.5 | 1.1–5.4 |
| Age >65 yr | 3.5 | 1.7–7.4 |
| Glucose >150 mg/dl | 1.8 | 1.2–2.8 |
| Charlson score | 1.1 | 1.0–1.2 |
n = 555; c = 0.65 for model.
Glycemic control, length of stay, and costs
Patients without diabetes had a mean HbA1c of 5.57 ± 0.39%. Patients with unrecognized probable diabetes had mean HbA1c of 6.48 ± 0.41%. Patients with type 1 diabetes (n = 9) had mean HbA1c of 7.78 ± 1.21%, and patients with type 2 diabetes (n = 127) had HbA1c of 7.39 ± 1.68%. Length of stay was not significantly different among patients without diabetes, with unrecognized probable diabetes, and with diabetes. Costs did not differ between patients with diagnosed and unrecognized probable diabetes (Table 1).
Follow-up
Overall, only 11 of the 71 eligible patients with elevated HbA1c levels and no diabetes diagnosis (15%) had diabetes recognized during 1 yr of follow-up, according to chart review or measurement of HbA1c level. Of the 21 patients with HbA1c higher than 6.5%, five (24%) had diabetes recognized within the year after initial admission. Of the 50 patients with HbA1c levels between 6.1 and 6.5%, six (12%) had further diabetes-related evaluation in the year after admission.
Discussion
In this cohort of 695 unselected inpatients admitted to an acute care hospital, 18% of patients had elevated HbA1c levels without a diabetes diagnosis. The prevalence of unrecognized probable diabetes among these inpatients is roughly 5-fold higher than in the general outpatient population, based on recent NHANES data (19,21). Of the 71 subjects with unrecognized probable diabetes who were followed within hospital-affiliated practices, only 15% had any diabetes diagnosis or diabetes-specific follow-up 1 yr after discharge. To our knowledge, this study is the first to estimate the prevalence of unrecognized probable diabetes among a diverse group of hospitalized U.S. patients and estimate rates of recognition at follow-up.
Using the HbA1c level to identify undiagnosed diabetes in inpatients may be controversial. Notably, the sensitivity of this test may be lower in hospitalized patients due to abnormal hemoglobin kinetics or red blood cell transfusion, and false positives may accrue as a result of longstanding stress hyperglycemia in chronically ill patients. We controlled for Charlson score in our multivariable model to attempt to account for chronic illness-related stress hyperglycemia. Nonetheless, although HbA1c is not currently recommended as a screening or diagnostic test in the outpatient setting (26), the HbA1c is an attractive option as an inpatient screening test due to buffering of the effect of acute glycemia on the result. A similar study conducted in an ethnically heterogeneous cohort of U.S. trauma patients, who would not be expected to have preceding stress hyperglycemia (but who may have experienced blood loss, leading to lower mean HbA1c levels), found a similar prevalence of undiagnosed probable diabetes (22%) (27).
One of the reasons it has been hard to determine the prevalence of unrecognized diabetes among inpatients is that random serum glucose level is an insensitive marker for diabetes among inpatients, despite the fact that persistent hyperglycemia is common among inpatients with known diabetes (28) and unrecognized diabetes (14). Considering the stress hyperglycemia that may occur in inpatients and the recognized deleterious effects of fasting on glucose metabolism, diagnosing diabetes in inpatients using glucose levels is problematic. The results of the logistic model identify increased risk elevated HbA1c in older patients and in patients with random plasma glucose level over 150 mg/dl, controlling for level of chronic illness. Still, this plasma glucose level has only 48% sensitivity and 73% specificity for diagnosis of diabetes. In the outpatient setting, screening with a random plasma glucose greater than 130 mg/dl provided a good yield while minimizing false positives and costs (29), but that cutoff would have a sensitivity of 54% and false-positive rate of 44% in this inpatient population.
These data show that hyperglycemia, although a good marker for critical illness, is an insensitive marker for undiagnosed diabetes. It is important to note that although diabetes (30,31) and hyperglycemia (3,32) have been associated with increased mortality among inpatients in observational studies, undiagnosed diabetes has not. In this sample, patients with unrecognized probable diabetes were not likely to be significantly more hyperglycemic than patients without unrecognized diabetes.
Consequently, the utility of diagnosis for inpatients is likely to be low unless patients subsequently receive long-term outpatient care to prevent complications of diabetes. Early identification and treatment can prevent complications, which are present in up to 48% of patients at the time of diagnosis of type 2 diabetes (11,12,13). Patients with HbA1c levels over 6.1% have high rates of progression to worsening glycemia in the absence of treatment (33,34). These patients can benefit from reduction in cardiac risk factors with intensive lifestyle intervention or medication (35) and in reduction in microvascular complications with control of glycemia (36,37). Among patients with unrecognized diabetes who had follow-up data available, we found a low rate of clinical recognition of diabetes in the year after discharge. In general, systems for follow-up of hospitalized patients after discharge are haphazard (38). If inpatient screening for diabetes with HbA1c levels is to be used as a means of targeting a group at high risk for unrecognized diabetes and its complications, any inpatient resources devoted to diabetes screening should be coupled with an effective plan for follow-up after discharge.
The rate of unrecognized probable diabetes in this cohort is necessarily biased by the sample and may not reflect the rate among all patients in acute care hospitals. For example, because patients who were admitted for observation or those who did not have serum samples available for HbA1c levels were excluded, and were likely healthier than the patients in this cohort, we may have overestimated the prevalence of unrecognized diabetes. Conversely, because diabetes and obesity have a lower prevalence in Massachusetts and the availability of health care resources is high relative to other parts of the country, this sample may underestimate the rate of unrecognized diabetes among inpatients elsewhere. Despite these limitations, our estimate of undiagnosed probable diabetes is identical to that obtained in an outpatient setting at an academic medical center located in an area with a higher prevalence of diabetes (Duke University Medical Center) (39) and very similar to that in a trauma cohort (27). Our estimate is much higher than a prevalence of 2.6% obtained in patients presenting to an emergency department in London (40) and in a European study (15) of unselected patients.
Although this study provides a real-world estimate of the prevalence of unrecognized diabetes among inpatients, it is limited by the nature of data obtained in the course of routine care. In addition to the those outlined above, data on inpatient glycemia may be biased because patients in ICUs and those with diabetes may have been more likely to have glucose levels measured and, consequently, may be more likely to have hyperglycemia detected. HbA1c levels may have been affected by prior illness and other factors, as noted above. Data on diabetes-related follow-up are limited by small sample size and provide only a snapshot of real-world behavior.
In summary, this study of 695 adult patients admitted to an acute care hospital revealed a prevalence of unrecognized probable diabetes of 18% based on HbA1c levels higher than 6.1%, with 5% of the sample having HbA1c over 6.5%. These patients did not have significant hyperglycemia during the hospital admission. Patients with undiagnosed probable diabetes are at risk for development and progression of complications of diabetes before clinical recognition of their metabolic abnormalities, yet only 15% of these patients were recognized as having diabetes within 1 yr of follow-up. Screening with HbA1c levels at the time of admission to an acute care hospital may represent an opportunity to identify a high-risk group of patients with unrecognized diabetes and, if coupled with effective follow-up, to promote prevention of subsequent diabetes-related complications.
Acknowledgments
We are grateful to Nancy Wong, M.A., for extensive assistance with data retrieval. D.J.W. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
D.J.W. is supported by a National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Career Development Award (K23 DK 080 228). D.M.N. is supported in part by the Earl Charlton Fund for Innovative Diabetes Research. R.W.G. is supported by an NIDDK Career Development Award (K23 DK067452).
Disclosure Statement: The authors have nothing to disclose.
First Published Online August 12, 2008
Abbreviations: HbA1c, Hemoglobin A1c; ICU, intensive care unit.
References
- Aubert RE, Geiss LS, Ballard DJ, Cocanougher B, Herman WH 1995 Diabetes-related hospitalization and hospital utilization. In: Diabetes in America. 2nd ed. Bethesda, MD: National Institutes of Health; 553–569 [Google Scholar]
- Baker EH, Janaway CH, Philips BJ, Brennan AL, Baines DL, Wood DM, Jones PW 2006 Hyperglycaemia is associated with poor outcomes in patients admitted to hospital with acute exacerbations of chronic obstructive pulmonary disease. Thorax 61:284–289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosiborod M, Rathore SS, Inzucchi SE, Masoudi FA, Wang Y, Havranek EP, Krumholz HM 2005 Admission glucose and mortality in elderly patients hospitalized with acute myocardial infarction: implications for patients with and without recognized diabetes. Circulation 111:3078–3086 [DOI] [PubMed] [Google Scholar]
- Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE 2002 Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 87:978–982 [DOI] [PubMed] [Google Scholar]
- Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein HC 2001 Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke 32:2426–2432 [DOI] [PubMed] [Google Scholar]
- Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R 2001 Intensive insulin therapy in the critically ill patients. N Engl J Med 345:1359–1367 [DOI] [PubMed] [Google Scholar]
- Malmberg K 1997 Prospective randomised study of intensive insulin treatment on long term survival after acute myocardial infarction in patients with diabetes mellitus. DIGAMI (Diabetes Mellitus, Insulin Glucose Infusion in Acute Myocardial Infarction) Study Group. BMJ 314:1512–1515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The ACE/ADA Task Force on Inpatient Diabetes 2006 American College of Endocrinology and American Diabetes Association Consensus Statement on Inpatient Diabetes and Glycemic Control: a call to action. Diabetes Care 29:1955–1962. [DOI] [PubMed] [Google Scholar]
- Society of Hospital Medicine Glycemic Control Task Force, Workbook for improvement: improving glycemic control, preventing hypoglycemia, and optimizing care of the inpatient with hyperglycemia and diabetes. http://www.hospitalmedicineorg/ResourceRoomRedesign/pdf/GC_Workbookpdf, accessed July 16, 2007 [Google Scholar]
- Joint Commission on Accreditation of Healthcare Organizations 2006 American Diabetes Association and Joint Commission collaborate on Joint Commission Inpatient Diabetes Care Certification. http://www.jointcommissionorg/NewsRoom/NewsReleases/jc_nr_072006htm, accessed January 10, 2007 [Google Scholar]
- Kohner EM, Aldington SJ, Stratton IM, Manley SE, Holman RR, Matthews DR, Turner RC 1998 United Kingdom Prospective Diabetes Study, 30: diabetic retinopathy at diagnosis of non-insulin-dependent diabetes mellitus and associated risk factors. Arch Ophthalmol 116:297–303 [DOI] [PubMed] [Google Scholar]
- Spijkerman AM, Dekker JM, Nijpels G, Adriaanse MC, Kostense PJ, Ruwaard D, Stehouwer CD, Bouter LM, Heine RJ 2003 Microvascular complications at time of diagnosis of type 2 diabetes are similar among diabetic patients detected by targeted screening and patients newly diagnosed in general practice: the Hoorn screening study. Diabetes Care 26:2604–2608 [DOI] [PubMed] [Google Scholar]
- Koopman RJ, Mainous 3rd AG, Liszka HA, Colwell JA, Slate EH, Carnemolla MA, Everett CJ 2006 Evidence of nephropathy and peripheral neuropathy in US adults with undiagnosed diabetes. Ann Fam Med 4:427–432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levetan CS, Passaro M, Jablonski K, Kass M, Ratner RE 1998 Unrecognized diabetes among hospitalized patients. Diabetes Care 21:246–249 [DOI] [PubMed] [Google Scholar]
- Carral F, Olveira G, Aguilar M, Ortego J, Gavilan I, Domenech I, Escobar L 2003 Hospital discharge records under-report the prevalence of diabetes in inpatients. Diabetes Res Clin Pract 59:145–151 [DOI] [PubMed] [Google Scholar]
- Lankisch M, Futh R, Gulker H, Lapp H, Bufe A, Haastert B, Martin S, Rathmann W 2008 Screening for undiagnosed diabetes in patients with acute myocardial infarction. Clin Res Cardiol, in press [DOI] [PubMed] [Google Scholar]
- Greci LS, Kailasam M, Malkani S, Katz DL, Hulinsky I, Ahmadi R, Nawaz H 2003 Utility of HbA1c levels for diabetes: case finding in hospitalized patients with hyperglycemia. Diabetes Care 26:1064–1068 [DOI] [PubMed] [Google Scholar]
- Rohlfing CL, Little RR, Wiedmeyer HM, England JD, Madsen R, Harris MI, Flegal KM, Eberhardt MS, Goldstein DE 2000 Use of GHb (HbA1c) in screening for undiagnosed diabetes in the U.S. population. Diabetes Care 23:187–191 [DOI] [PubMed] [Google Scholar]
- Buell C, Kermah D, Davidson MB 2007 Utility of A1C for diabetes screening in the 1999–2004 NHANES population. Diabetes Care 30:2233–2235 [DOI] [PubMed] [Google Scholar]
- Cely CM, Arora P, Quartin AA, Kett DH, Schein RM 2004 Relationship of baseline glucose homeostasis to hyperglycemia during medical critical illness. Chest 126:879–887 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) 2003 Prevalence of diabetes and impaired fasting glucose in adults: United States, 1999–2000. MMWR Morb Mortal Wkly Rep 52:833–837 [PubMed] [Google Scholar]
- Edelman D, Olsen MK, Dudley TK, Harris AC, Oddone EZ 2004 Utility of hemoglobin A1c in predicting diabetes risk. J Gen Intern Med 19:1175–1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein DE, Little RR, Lorenz RA, Malone JI, Nathan D, Peterson CM, Sacks DB 2004 Tests of glycemia in diabetes. Diabetes Care 27:1761–1773 [DOI] [PubMed] [Google Scholar]
- Little RR, Rohlfing CL, Wiedmeyer HM, Myers GL, Sacks DB, Goldstein DE 2001 The national glycohemoglobin standardization program: a five-year progress report. Clin Chem 47:1985–1992 [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR 1987 A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383 [DOI] [PubMed] [Google Scholar]
- American Diabetes Association 2008 Standards of medical care in diabetes: 2008. Diabetes Care 31:S12–S54 [DOI] [PubMed] [Google Scholar]
- Kopelman TR, O'Neill PJ, Kanneganti SR, Davis KM, Drachman DA 2008 The relationship of plasma glucose and glycosylated hemoglobin A1C levels among nondiabetic trauma patients. J Trauma 64:30–33; discussion 33–34 [DOI] [PubMed] [Google Scholar]
- Wexler DJ, Meigs JB, Cagliero E, Nathan DM, Grant RW 2007 Prevalence of hyper- and hypoglycemia among inpatients with diabetes. Diabetes Care 30:367–369 [DOI] [PubMed] [Google Scholar]
- Johnson SL, Tabaei BP, Herman WH 2005 The efficacy and cost of alternative strategies for systematic screening for type 2 diabetes in the U.S. population 45–74 years of age. Diabetes Care 28:307–311 [DOI] [PubMed] [Google Scholar]
- Kornum JB, Thomsen RW, Riis A, Lervang HH, Schonheyder HC, Sorensen HT 2007 Type 2 diabetes and pneumonia outcomes: a population-based cohort study. Diabetes Care 30:2251–2257 [DOI] [PubMed] [Google Scholar]
- Malmberg K, Norhammar A, Wedel H, Ryden L 1999 Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation 99:2626–2632 [DOI] [PubMed] [Google Scholar]
- Krinsley JS 2003 Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc 78:1471–1478 [DOI] [PubMed] [Google Scholar]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM; Diabetes Prevention Program Research Group 2002 Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pani LN, Nathan DM, Grant RW 2007 Clinical predictors of disease progression and medication initiation in untreated patients with type 2 diabetes and A1C less than 7%. Diabetes Care31:386–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratner R, Goldberg R, Haffner S, Marcovina S, Orchard T, Fowler S, Temprosa M; Diabetes Prevention Program Research Group 2005 Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the Diabetes Prevention Program. Diabetes Care 28:888–894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1998 Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet [Erratum (1998) 352:1558] 352:854–865 [PubMed] [Google Scholar]
- 1998 Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet [Erratum (1999) 354:602] 352:837–853 [PubMed] [Google Scholar]
- Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW 2007 Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA 297:831–841 [DOI] [PubMed] [Google Scholar]
- Edelman D 2002 Outpatient diagnostic errors: unrecognized hyperglycemia. Eff Clin Pract 5:11–16 [PubMed] [Google Scholar]
- George PM, Valabhji J, Dawood M, Henry JA 2005 Screening for type 2 diabetes in the accident and emergency department. Diabet Med 22:1766–1769 [DOI] [PubMed] [Google Scholar]