Abstract
Aims
Modern imaging technology allows us the visualization of coronary artery calcification (CAC), a marker of subclinical coronary atherosclerosis. The prevalence, quantity, and risk factors for CAC were compared between two studies with similar imaging protocols but different source populations: the Multi-Ethnic Study of Atherosclerosis (MESA) and the Heinz Nixdorf Recall Study (HNR).
Methods and results
The measured CAC in 2220 MESA participants were compared with those in 3126 HNR participants with the inclusion criteria such as age 45–75 years, Caucasian race, and free of baseline cardiovascular disease. Despite similar mean levels of CAC of 244.6 among participants in MESA and of 240.3 in HNR (P = 0.91), the prevalence of CAC > 0 was lower in MESA (52.6%) compared with HNR (67.0%) with a prevalence rate ratio of CAC > 0 of 0.78 [95% confidence interval (CI): 0.72–0.85] after adjustment for known risk factors. Consequently, among participants with CAC > 0, the participants in MESA tended to have higher levels of CAC than those in HNR (ratio of CAC levels: 1.39; 95% CI: 1.19–1.63), since many HNR participants have small (near zero) CAC values.
Conclusions
The CAC prevalence was lower in the United States (MESA) cohort than in the German (HNR) cohort, which may be explained by more favourable risk factor levels among the MESA participants. The predictors for increased levels of CAC were, however, similar in both cohorts with the exception that male gender, blood pressure, and body mass index were more strongly associated in the HNR cohort.
Keywords: Epidemiology, Atherosclerosis, Coronary artery calcium, Risk factors, Screening
Introduction
First serious cardiac events are often fatal, and half of all coronary heart disease (CHD) deaths are sudden coronary deaths and occur out of the hospital.1–3 A continued emphasis on primary and secondary prevention programmes may be a key step in reducing mortality due to CHD.1–4
Individual risk prediction algorithms are currently based on cohorts of different countries.4–9 In low-risk subjects (<10% risk of a hard cardiac event within 10 years), life style changes are recommended with a repeat check-up after 3–5 years. However, it is recommended that high-risk subjects (>20% risk of hard events, myocardial infarction, or CHD death within 10 years) should undergo risk factor reduction including drug treatment. In intermediate risk subjects, further tests are suggested for risk stratification.7–9 Calcium screening for the detection of coronary artery calcification (CAC) belongs to the currently available tests.10–12
Two prospective studies have simultaneously been initiated, the MESA (Multi-Ethnic Study of Atherosclerosis)13 and the Heinz Nixdorf Recall Study (HNR) (risk factors, evaluation of coronary calcium and lifestyle study), both of which study the value of CAC levels for risk prediction.14 Their cross-sectional data on the baseline characteristics have previously been published.15–24
The aim of this study is to compare the prevalence of cardiovascular risk factors and their association with CAC between the United States and Germany.
Methods
Study populations
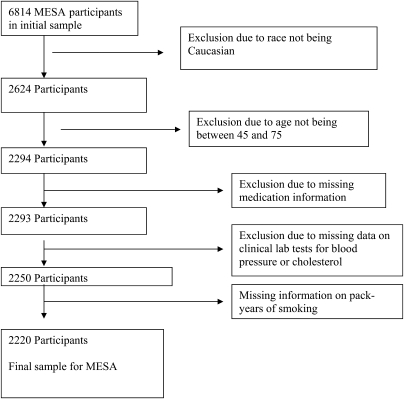
The MESA study recruited 6814 participants between the years 2000 and 2002 across six centres in the United States with participants recruited using locally available resources, including lists of residents, dwellings, telephone exchanges, division of motor vehicle lists, consumer lists, voter registration lists, and census data. Each site recruited an approximately equal number of men and women, according to pre-specified age and race/ethnicity proportions. Participants were between 45 and 84 years of age and identified themselves as one of Caucasian, African-American, Hispanic, or Chinese.13 For this comparison of the two study cohorts, only Caucasians aged 45–75 years with complete information on risk factors, blood pressure and lipid-lowering medication and CAC, and without clinically overt cardiovascular disease were included (Figure 1 and 2).
Figure 1.
Multi-Ethnic Study of Atherosclerosis (MESA) decision tree for inclusion in joint study.
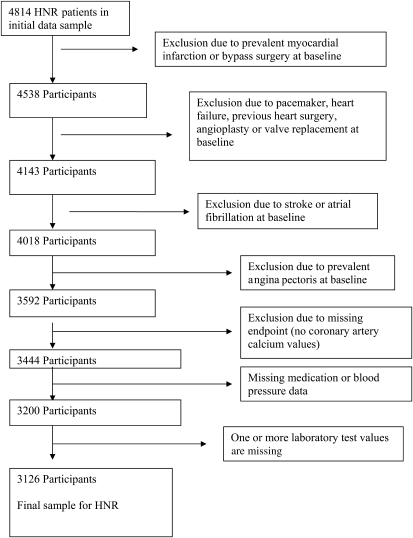
Figure 2.
Heinz Nixdorf Recall Study (HNR) decision tree for inclusion in joint study.
The HNR recruited a total of 4814 Caucasians between 45 and 75 years of age from three neighbouring cities in Germany between the years 2000 and 2003 in a single centre with a response rate of 55.8%.18 Participants were a random sample derived from mandatory citizen registries and provided to the study centre. The study was certified according to DIN EN ISO 9001:2000, and re-certified in 2006.
For both studies, approval was provided by the local institutional review boards.
Clinical data
The traditional cardiovascular risk factors that are part of the Framingham risk scoring algorithm9 were measured in both studies. In addition, body mass index (BMI; kg/m2) was computed on the basis of direct measurements of height and weight. All medication utilization reported was based on participants' self-report.
Standard enzymatic methods were used to measure total cholesterol, high-density lipoprotein (HDL)-cholesterol (HDL-C), and triglycerides.13,14 Low-density lipoprotein (LDL)-cholesterol (LDL-C) was calculated with the Friedewald equation in MESA17,22 and measured directly in HNR.19,20 Blood samples were obtained after a 12 h fasting in MESA. In HNR, participants were fasting 9.7 ± 4.9 h (median 12 h) before blood sampling, with 34.4% having fasted for <6 h.
In both studies, blood pressure was measured using an oscillographic method with two different systems (Dynamap®, J&J, USA and HEM-705CP, Omron, Hoofddrop, NL).13,14,18 The mean values of the second and third of three measurements taken at least 2 min apart were used. Hypertension was defined in both studies as blood pressure >140/90 mmHg or use of antihypertensive medication.18,22
In both studies, participants were considered diabetic if they were taking anti-diabetic medication or had a fasting glucose of >126 mg/dL.19,22 And smoking history was categorized to (i) currently smoking, (ii) former, defined as not smoking within the past 30 days in MESA and as stopped smoking (a) within the past year or (b) more than 1 year ago in the HNR, and (iii) never.17,23
The use of lipid-lowering medication was documented. This included HMG CoA reductase inhibitors (‘statins’), fibrates, bile acid sequestrants, and nicotinic acid derivatives.17,20
Electron beam and multi-slice computed tomography
Participants received the scanning examination first and were then entered into MESA, whereas, in HNR, participants were seen and tested in the study centre before electron beam CT (EBCT) was performed.13,14 Non-enhanced EBCT scans were performed with a C-100 or C-150 scanner (GE Imatron, South San Francisco, USA) in three MESA and the HNR centres. In addition, three other MESA centres used a first-generation multi-slice CT (MSCT).13 The EBCT scanners were operated in the single-slice mode with an image acquisition time of 100 ms and a section thickness of 3 mm. Prospective ECG-triggering was done at 80% of the R–R interval for EBCT. Each participant was scanned twice in MESA and once in HNR.15,16,19
In MESA, scans were read centrally at the Los Angeles Biomedical Research Institute at Harbor–UCLA Medical Center.24 In HNR, the two radiology departments scanned and analysed the CAC score blinded and independently.14,19 In both studies, CAC was defined as a hyper-attenuating foci of at least four contiguous pixels with a CT density of ≥130 Hounsfield Units. The area of each focus was measured and the CAC score was determined using the methods of Agatston et al.25 The CAC score is the product of the area of each focus of detectable CAC and a factor rated one through four dictated by the maximum CT density within that focus. The total (Agatston) CAC score was computed by summing-up the CAC scores of all foci in the epicardial coronary system without phantom adjustment. Agreement with regard to the presence of CAC was high in MESA (κ = 0.90–0.93)24 and interclass correlation coefficient for CAC scoring of 0.99. In the HNR, inter-scan variability was 5–8%, and for inter-institutional readings of the two EBCT centres a κ-value of 0.94 in 250 scans was found.26
Statistical analysis
The MESA and HNR cohorts included in this comparison consisted of 2220 and 3126 Caucasian participants, respectively, between 45 and 75 years of age. Figures 1 and 2 demonstrate both the number of and reason for each exclusion of participants from either study from the current comparison.
The Framingham risk score was calculated for men and women to estimate the 10 year risk of a CHD event.9
Data are given as mean (SD) or frequency (%). Simple unadjusted differences in baseline data between MESA and HNR are statistically evaluated using Student’s t-test for continuous or χ2 test for categorical variables. We compared the prevalence of CAC > 0 between MESA and HNR using relative risk regression with robust standard errors. We used this approach to estimate the prevalence rate ratio (RR) rather than logistic regression because the prevalence of CAC > 0 is high, and hence the odds ratio is a poor estimate of the RR.27 In adjusted models, we controlled for age, sex, blood pressure, BMI, triglycerides, total cholesterol, HDL-C, glucose, current smoking, pack years, and medication use (blood pressure, diabetes, and cholesterol lowering).
Among those with CAC > 0, we modelled the log-transformed amount of CAC as a linear function of study (MESA vs. HNR) and the covariates described above. The exponentiated coefficients from these models are presented, and these are interpreted as a multiplicative increase in average CAC amount. The above analyses were repeated stratifying by sex. In addition, for the pooled models, we tested for interactions between each risk factor and study (MESA vs. HNR) to determine whether the risk factor associations with either presence or level of CAC differed between the study populations.
All analyses were performed with SAS, version 9.1.3. All statistical tests were two sided and at the 5% level of statistical significance.
Results
After all exclusion criteria were applied, the final study population consisted of 2220 subjects from MESA and 3126 from HNR. The baseline demographics and the results of the CAC scoring for men and women are shown in Table 1. The prevalence of most cardiovascular risk factors was lower in MESA than in HNR. In MESA, blood pressure values were lower and antihypertensive medications are more often used than in HNR. Current smoking was much more prevalent in HNR, although due to a higher rate of former smokers in MESA, pack years of smoking were very similar between the two cohorts. For total cholesterol a between-study difference of 35.7 mg/dL and for LDL-C a difference of 29.6 mg/dL were found, with cholesterol values lower in MESA. Average HDL-C was also lower in MESA (7.1 mg/dL estimated difference). Lipid-lowering medication was much more common in MESA than in HNR (17.4 vs. 8.2%). The proportion of treated diabetic participants was similar between the two populations. The 10 year Framingham risk score was slightly lower in the MESA cohort than in the HNR cohort (10 ± 7 vs. 11 ± 8%, P < 0.0001).
Table 1.
Baseline demographics of Multi-Ethnic Study of Atherosclerosis (MESA) and the Heinz Nixdorf Recall Study (HNR) male and female participants
| MESA (n = 2220) |
HNR (n = 3126) |
|||
|---|---|---|---|---|
| Men (n = 1080) | Women (n = 1140) | Men (n = 1466) | Women (n = 1660) | |
| Age, years | 60.6 (8.8) | 59.9 (8.6) | 58.7 (7.5) | 58.9 (7.7) |
| Systolic blood pressure, mmHg | 123.0 (17.8) | 120.6 (21.2) | 137.4 (19.3) | 127.2 (20.8) |
| Diastolic blood pressure, mmHg | 74.2 (9.0) | 67.1 (9.6) | 84.3 (10.5) | 78.8 (10.4) |
| Antihypertensive medication | 31.6 | 29.2 | 27.2 | 27.6 |
| Current smoker, % | 11.9 | 13.1 | 24.6 | 22.8 |
| Former smoker, % | 48.3 | 41.3 | 45.2 | 22.5 |
| Pack years of smokinga, years | 21.0 (29.1) | 9.5 (16.5) | 18.7 (34.7) | 12.2 (19.9) |
| Body mass index, kg/m2 | 28.1 (4.2) | 27.7 (6.0) | 27.9 (3.8) | 27.2 (4.8) |
| Total cholesterol, mg/dL | 189 (33) | 201 (33) | 228 (37) | 234 (39) |
| LDL-C, mg/dL | 118 (29) | 117 (31) | 148 (35) | 146 (37) |
| HDL-C, mg/dL | 45 (12) | 59 (16) | 52 (14) | 66 (17) |
| Triglycerides, mg/dL | 129 (66) | 127 (66) | 161 (115) | 129 (77) |
| Lipid-lowering medication, % | 19.6 | 15.4 | 8.0 | 8.4 |
| Glucose, mg/dL | 101 (24) | 94 (16) | 113 (29) | 106 (22) |
| Treated diabetes mellitus, % | 4.4 | 3.2 | 5.7 | 3.3 |
| Framingham risk score, % in 10 years | 13 (8) | 6 (4) | 15 (9) | 7 (5) |
| Framingham risk score median (Q1–3) | 11 (7.4 and 17.3) | 5 (3.3 and 7.7) | 14 (9 and 18) | 2.6 (3 and 9) |
| Proportion of subjects with CAC (Agatston) score units | ||||
| 0, % | 32.4 | 61.8 | 18.1 | 46.2 |
| 1–10, % | 6.9 | 5.8 | 13.2 | 21.6 |
| 11–100, % | 23.0 | 17.2 | 29.3 | 18.9 |
| 101–400, % | 19.9 | 10.3 | 23.9 | 9.5 |
| 401+, % | 17.9 | 5.0 | 15.4 | 3.7 |
| Median CAC (Agatston) score units (Q1–3) | 30.6 (0–246.9) | 0 (0–24.7) | 52.6 (0– 222.5) | 1.3 (0–31.6) |
| Mean log (CAC + 1) | 3.17 (2.64) | 1.52 (2.33) | 3.58 (2.33) | 1.77 (2.09) |
| Mean log (CAC + 1) where CAC > 0 | 4.69 (1.76) | 3.98 (1.79) | 4.36 (1.79) | 3.31 (1.77) |
Values represent mean ± SD or percentages.
aAmong smokers and past-smokers.
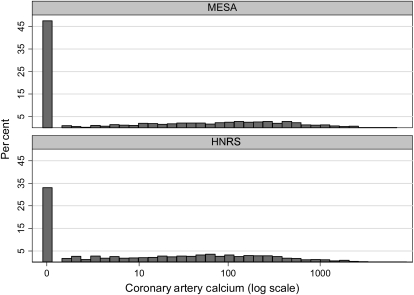
For male and female participants, the prevalence of zero CAC was substantially higher in MESA than those in HNR, while the prevalence of those with small amounts of CAC was much higher in HNR (Figure 3). There was a slightly higher prevalence of CAC > 400 Agatston score units in MESA compared with those in HNR.
Figure 3.
Comparison of the distribution of coronary artery calcium in Multi-Ethnic Study of Atherosclerosis (MESA) (top) with the distribution of coronary artery calcium in Heinz Nixdorf Recall Study (HNR) (bottom) in terms of log(CAC + 1). Data from the MESA and the HNR.
Table 2 provides the RR of CAC > 0 and 95% CI for MESA relative to the HNR cohort. For MESA participants, the rate of prevalent CAC was 22% less (95% CI, 15–28) when adjusted for traditional risk factors. For male participants, the adjusted prevalence of CAC > 0 was 38% lower in the MESA participants than in the HNR participants (95% CI, 27–48) whereas for female participants the adjusted prevalence of CAC > 0 was 18% lower (95% CI, 11–25).
Table 2.
Prevalence rate ratio (RR) of coronary artery calcium greater than zero: Multi-Ethnic Study of Atherosclerosis (MESA) vs. Heinz Nixdorf Recall Study (HNR)
| n | Crude RR (95% CI) | Adjusted RRa (95% CI) | |
|---|---|---|---|
| Overall | |||
| HNR | 3126 | Reference | Reference |
| MESA | 2220 | 0.70 (0.65–0.74) | 0.78 (0.72–0.85) |
| Women | |||
| HNR | 1660 | Reference | Reference |
| MESA | 1140 | 0.75 (0.70–0.80) | 0.82 (0.75–0.89) |
| Men | |||
| HNR | 1466 | Reference | Reference |
| MESA | 1080 | 0.56 (0.49–0.64) | 0.62 (0.52–0.73) |
aAdjusted for age, male, blood pressure, body mass index, triglycerides, total cholesterol, HDL-cholesterol, glucose, current smoker, pack years and medication use (blood pressure, diabetes, and cholesterol lowering).
Table 3 displays the estimated ratio of the average amount of CAC for participants in the MESA and HNR cohorts among those with a measured CAC > 0 at baseline. Among participants with CAC and adjusted for risk factors, MESA participants had an estimated 39% (95% CI, 19–63) higher average level of CAC due to the large number of low CAC values among HNR participants.
Table 3.
Estimated ratio of the amount of coronary artery calcium (CAC) and 95% CI among participants with CAC greater than zero: Multi-Ethnic Study of Atherosclerosis (MESA) vs. Heinz Nixdorf Recall Study (HNR) cohorts
| n | Crude ratio (95% CI) | Adjusted ratioa (95% CI) | |
|---|---|---|---|
| Overall | |||
| HNR | 2093 | Reference | Reference |
| MESA | 1166 | 1.73 (1.51–1.98) | 1.39 (1.19–1.63) |
| Women | |||
| HNR | 893 | Reference | Reference |
| MESA | 436 | 2.09 (1.65–2.58) | 1.68 (1.28–2.20) |
| Men | |||
| HNR | 1200 | Reference | Reference |
| MESA | 730 | 1.40 (1.18–1.66) | 1.24 (1.02–1.52) |
aAdjusted for age, male, blood pressure, body mass index, triglycerides, total cholesterol, HDL-cholesterol, glucose, current smoker, pack years, and medication use (blood pressure, diabetes, and cholesterol lowering).
Table 4 provides the prevalence rate ratio (RR) of CAC being present within the MESA and HNR cohorts. The association of age with CAC presentation was nearly identical between the two cohorts, with each 10 years of age increasing the prevalence of CAC by approximately 47% (for the tested life span from 45 to 75 years). The RR associated with male gender (MESA: RR 1.61 vs. HNR: RR 2.20; P = 0.0063) and BMI (MESA: RR 1.00 vs. HNR: 1.05; P ≤ 0.0001) were significantly lower in MESA than in HNR. As a sensitivity analysis for low CAC values, we performed the calculation using a cut-off value of 10 instead of zero in order to account for possible different measurement protocols. The calculation showed only minor shifts in parameters.
Table 4.
Prevalence rate ratio (RR) and 95% CI of coronary artery calcium greater then zero: Multi-Ethnic Study of Atherosclerosis (MESA; n = 2220) vs. Heinz Nixdorf Recall (HNR) Study (n = 3126)
| MESA (95% CI) | P-value | HNR (95% CI) | P-value | Interaction P-value | |
|---|---|---|---|---|---|
| Age, 10 years | 1.47 (1.38–1.55) | <0.0001 | 1.46 (1.35–1.57) | <0.0001 | 0.9397 |
| Male | 1.61 (1.46–1.79) | <0.0001 | 2.20 (1.93–2.50) | <0.0001 | 0.0063 |
| Systolic blood pressure, 10 mmHg | 1.02 (0.99–1.06) | 0.1933 | 1.04 (0.99–1.08) | 0.1129 | 0.7732 |
| Diastolic blood pressure, 10 mmHg | 1.03 (0.97–1.09) | 0.3436 | 1.03 (0.95–1.10) | 0.5917 | 0.9094 |
| Antihypertensive medication | 1.12 (1.01–1.25) | 0.0358 | 1.18 (1.03–1.34) | 0.0127 | 0.6594 |
| Current smoker | 1.26 (0.98–1.29) | 0.1021 | 1.36 (1.16–1.58) | <0.0001 | 0.1717 |
| Pack years, 10 years | 1.05 (1.01–1.10) | 0.0201 | 1.02 (0.97–1.06) | 0.5557 | 0.1194 |
| Body mass index, kg/m2 | 1.00 (1.00–1.01) | 0.2727 | 1.05 (1.04–1.07) | <0.0001 | <0.0001 |
| Triglycerides, 10 mg/dL | 0.99 (0.98–1.00) | 0.0077 | 1.00 (0.99–1.01) | 0.9532 | 0.2519 |
| Total cholesterol, 10 mg/dL | 1.03 (1.01–1.04) | 0.0001 | 1.12 (1.01–1.04) | <0.0001 | 0.9768 |
| HDL-cholesterol, 5 mg/dL | 0.97 (0.96–0.98) | <0.0001 | 0.99 (0.97–1.01) | 0.2535 | 0.2113 |
| Lipid-lowering medication | 1.53 (1.31–1.78) | <0.0001 | 1.33 (1.05–1.67) | 0.0172 | 0.4365 |
| Glucose, 10 mg/dL | 1.01 (0.98–1.04) | 0.4631 | 1.01 (0.97–1.04) | 0.7184 | 0.8680 |
| Treated diabetes | 1.85 (1.18–2.95) | 0.0085 | 1.55 (1.03–2.33) | 0.0342 | 0.6455 |
Table 5 demonstrates the estimated ratio of the average amount of CAC (among those with CAC > 0) for the MESA and HNR cohorts using log-linear regression analysis. In MESA, age was a stronger predictor for CAC (2.38 in MESA vs. 1.92 in HNR, P = 0.013 for interaction). Blood pressures were not strongly associated with CAC in MESA, whereas in HNR systolic and diastolic blood pressures were strongly positively and negatively associated with CAC respectively. The proportion of the variation explained by these models was nearly identical for the MESA participants (r2 = 21.4%) compared with the HNR participants (r2 = 21.2%).
Table 5.
Estimated ratio of the amount of log(CAC) and 95% CI: Multi-Ethnic Study of Atherosclerosis (MESA; n = 1166) and the Heinz Nixdorf Recall Study (HNR; n = 2093)
| MESA (95% CI) | P-value | HNR (95% CI) | P-value | Interaction P-value | |
|---|---|---|---|---|---|
| Age, 10 years | 2.38 (2.08–2.72) | <0.0001 | 1.92 (1.71–2.17) | <0.0001 | 0.0262 |
| Males | 2.23 (1.76–2.85) | <0.0001 | 3.18 (2.67–3.78) | <0.0001 | 0.0203 |
| Systolic blood pressure, 10 mmHg | 1.04 (0.97–1.12) | 0.2555 | 1.14 (1.07–1.21) | <0.0001 | 0.0609 |
| Diastolic blood pressure, 10 mmHg | 1.11 (0.96–1.28) | 0.1437 | 0.85 (0.77–0.95) | 0.0043 | 0.0054 |
| Antihypertensive medication | 1.32 (1.06–1.64) | 0.0122 | 1.45 (1.22–1.72) | <0.0001 | 0.5281 |
| Current smoker | 1.12 (0.80–1.57) | 0.5062 | 1.21 (1.00–1.48) | 0.0527 | 0.9962 |
| Pack years, 10 years | 1.07 (1.02–1.11) | 0.0022 | 1.08 (1.04–1.12) | <0.0001 | 0.3105 |
| Body mass index | 1.01 (0.99–1.03) | 0.5252 | 1.00 (0.98–1.01) | 0.6705 | 0.6887 |
| Triglycerides, 10 mg/dL | 1.00 (0.98–1.02) | 0.9250 | 1.00 (0.99–1.01) | 0.9503 | 0.5674 |
| Total cholesterol, 10 mg/dL | 1.02 (0.99–1.06) | 0.2229 | 1.04 (1.01–1.06) | 0.0012 | 0.5919 |
| HDL-cholesterol, 5 mg/dL | 1.00 (0.96–1.04) | 0.8672 | 0.99 (0.96–1.02) | 0.5535 | 0.4422 |
| Lipid-lowering medication | 1.20 (0.95–1.53) | 0.1246 | 1.44 (1.09–1.90) | 0.0104 | 0.3470 |
| Glucose, 10 mg/dL | 0.99 (0.95–1.03) | 0.6057 | 1.02 (0.99–1.05) | 0.2760 | 0.5574 |
| Treated diabetes | 1.70 (1.06–2.71) | 0.0266 | 1.21 (0.81–1.79) | 0.3482 | 0.2806 |
| Model fit statistics | |||||
| R2 | 21.4% | 21.2% | 22.6% | ||
Discussion
The main findings of our study were: (i) the prevalence of CAC > 0 was lower in the MESA population than in the HNR population. (ii) Differences in how specific risk factors affected either the prevalence of CAC > 0 or the level of CAC pertained to age, male gender, BMI, and blood pressure. Risk factors in MESA were lower than in HNR. The results for these two studies appear to be representative of the underlying populations and so differences may be due to differences in the distribution of modifiable risk factors between the United States and Germany.
The prevalence of participants with CAC > 0 was lower in the MESA than those in the HNR population, which was surprising. Our study showed not only a lower prevalence but also lower median CAC values in MESA compared with HNR for men and women. The fact that a much higher proportion of HNR participants had low CAC scores (rather than zero scores) could be explained if the HNR scanners were detecting more noise than the MESA scanners. However, we determined that the presence of a small amount of CAC in HNR was associated with the standard risk factors, indicating that these small values are unlikely to be due primarily to noise artefacts.
On the other hand, participants with CAC > 400 were found slightly more often in the MESA cohort than in the HNR cohort. CAC represents the long-term effect of risk factor exposure, and the observed risk factor values in MESA and HNR reflect only the current level. Alternatively, there were selected risk factors that had a worse profile in MESA than in HNR, such as BMI and HDL-C.
With respect to cardiovascular risk, chronological age represents a very strong risk factor in current algorithms.5–9 Measures of CAC seem to be related to survival.11,12,28 The mean age, but not the range, was slightly different between MESA and HNR, but this difference in ages was not sufficient to explain the difference in prevalence of CAC that we observed.16,28,29
Women have much lower values of CAC than men and start to develop CAC later.16,19 Therefore, risk assessment for increased risk of cardiac outcomes should consider both age and sex.30,31 Gender was one of the most important variables when tested for RR of CAC being present. In addition, gender was one of the two variables with a significantly different association with CAC between the two studies. Both in men and women, the prevalence of CAC = 0 is higher in MESA compared with HNR. This may in part be attributable to differences in risk factor control in the United States vs. Germany. This is supported by higher use of antihypertensive and lipid-lowering medication in the United States (see below), which is expected to be similarly effective in men and women. Risk factor control using medication or life-style interventions may also have been initiated earlier in lives of United States compared with German participants.
Blood pressure can be regarded as a strong risk predictor for both cardiac and cardiovascular events.5–9 Blood pressure was lower among MESA participants than among HNR participants. This difference in blood pressure levels may be part of the explanation of the lower degree of CAC in the MESA compared with the HNR cohorts. One factor that might explain some of this observed difference in blood pressure could be the different oscillographic systems that were used, but not being able to explain the total difference.21
More participants in MESA compared with those in HNR received antihypertensive treatment (30 vs. 27%, P < 0.0172), and there was less untreated hypertension (10 vs. 24%, P < 0.0001). Blood pressure control in Germany is far from the optimal that has been reported for other countries.32,33 The poor control of blood pressure and thereby the wider range may be an explanation for the significant association of blood pressure and CAC amount in HNR study but not in MESA. The importance of blood pressure as a risk factor is, however, underlined by the fact that in both studies antihypertensive medication was a highly significant predictor of CAC.
Previous studies have shown that tobacco use is a major avoidable cause of cardiovascular diseases.34 Strong efforts have been made to ban smoking in the United States, but efforts in Europe began later and have been less effective.35 This may explain why the prevalence of current smoking is lower in MESA than in HNR. MESA had much higher rates of former smokers, and roughly equivalent average pack years of smoking, supporting the success of recent anti-smoking efforts in the United States. The interactions between study and the smoking variables were not significant, however, suggesting that the association between smoking and CAC was similar in both studies.
Total cholesterol (TC) and LDL-C are regarded as traditional risk factors.5–9 In the MESA cohort, mean TC was <200 mg/dL, LDL-C <130 mg/dL, and triglycerides <150 mg/dL, which are regarded as desirable, nearly optimal, and normal.9 The results seem to be in line with general trends in the United States.36 LDL-C was selected as the primary target of cholesterol-lowering therapy,9 resulting in an increased use of lipid-lowering medication.36 In HNR, significantly higher concentrations were observed which is representative for Germany.37,38 The association between TC and CAC was not significantly different between the two studies, though was qualitatively stronger in HNR than in MESA. Similarly, HDL was only significantly protective (for the presence of CAC > 0) in MESA, though the interaction was not statistically significant. The prevalence of cholesterol lipid-lowering medication was different between the two studies. The effect of these medications on CAC should be further investigated prospectively in each of these study populations once longitudinal data become available.
In both studies glucose levels were not related to risk of CAC independent of diabetic status, but treated diabetes was significantly associated with CAC. However, in HNR not all subjects were fasting and glucose tolerance tests were not performed in both studies. The RR of prevalent CAC was 55% higher for treated diabetics compared with others in MESA, and 65% higher in HNR. The interaction between study and diabetes was non-significant.
Limitations of the study
It was not possible to compare the full cohorts of either study. To allow for best possible comparability between the two cohorts, identical inclusion criteria were employed to identify all participants without prevalent cardiovascular disease. Thereby, the selection bias could be minimized, which otherwise may have been caused by differences in recruitment strategies.
The prevalence and levels of cardiovascular risk factors are very different in the two cohorts of ostensibly healthy persons but both seem to be representative for each of the two countries. This is a cross-sectional study and so it is not possible to establish the direction of any association between risk factors and CAC.39 In addition, there is a possibility of unmeasured confounders such as lifestyle and dietary history that could explain some of the observed differences between the cohorts. It is possible that differences between the types of scanners used in both studies could explain a small part of the observed population differences in CAC levels. It has to be taken into account that the MESA performed a calculation to estimate the LDL-C concentration whereas it was directly measured in HNR. The assay used met the requirements for accurate testing even from non-fasting individuals.40 However, the differences between MESA and HNR cannot be attributed to these methodological differences because TC also showed the same magnitude of difference in the same direction.
In the present analysis, a socio-economic comparison has not been included, because socio-economic variables such as income—due to differences in services, conversion in income from Euros to Dollars, etc. and education—given the United States cost structure of higher education, are difficult to compare between the two countries.
Conclusions
Coronary artery calcification prevalence was lower in the United States (MESA) cohort than the German (HNR) cohort. This was partially but not fully explained by generally more favourable risk factor levels among the MESA participants. This could be shown for men and women. CAC was significantly associated with age, gender, current smoking, treated diabetes, hypertension, and hypercholesterolaemia. Risk factor associations were comparable across the two studies, with the exception that male gender, blood pressure, and BMI were more strongly associated with CAC in the German cohort. It is possible that the difference in CAC could be attributed to different efforts towards risk factor elimination in the two countries. Germany shows higher rates of hypercholesterolaemia and smoking, but less obesity and use of lipid-lowering medication. In particular, the effect of the higher rates of untreated hypertension in the German population should be further investigated prospectively and could be responsible for an earlier onset of subclinical coronary atherosclerosis.
Funding
The MESA study is funded by the National Heart, Lung and Blood Institute of the National Institutes of Health and supported by contracts N01-HC-95159 through N01-HC-95165 and N01-HC-95169 from the Nationals Heart, Lung, and Blood Institute. The HNR study is funded by a contract with the private Heinz Nixdorf Foundation, Essen, Germany and undergoes continuous monitoring by governmental agencies (DLR) lead by the Bundesministerium für Bildung und Forschung (BMBF). This study is also supported by the German Ministry of Education and Science (DFG).
Funding to pay the Open Access publication charges for this article was provided by the Heinz Nixdorf Recall Study Investigators.
Acknowledgements
We thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org. We also thank the Heinz Nixdorf Foundation (Chairman: Dr. jur. G. Schmidt) for their generous support of this study. We thank Nico Dragano, Johannes Siegrist (Department of Social Medicine of the University Düsseldorf, as well as Rainer Seibel and Dietrich Grönemeyer from the Department of Radiology of the University Witten-Herdecke, Klaus Mann and Martina Bröker from the Department of Clinical Chemistry and Laboratory Medicine, University Duisburg-Essen as well as all members of the investigator group, and the previous member Karl Lauterbach (Dept. of Health Economy and Epidemiology, University of Cologne, Germany) for their valuable contributions to the study. We are indebted to the study personnel of the Heinz Nixdorf Recall Study, in particular D Weimar, and EM Beck, both IMIBE. Funding to pay the Open Access publication charges for this article was provided by the HNR group.
Advisory Board HNR: T. Meinertz, Hamburg (Chair); M. Blettner, Mainz; C. Bode, Freiburg; PJ. de Feyter, Rotterdam, Niederlande; B. Güntert, Hall i.T., Schweiz; F. Gutzwiller, Schweiz; H. Heinen, Bonn; O. Hess, Bern, Schweiz; B. Klein, Essen; H. Löwel, Neuherberg; M. Reiser, München; G. Schmidt, Essen; M. Schwaiger, München; C. Steinmüller, Bonn; T. Theorell, Stockholm, Schweden; SN. Willich, Berlin.
Criteria and Endpoint Committee HNR: C. Bode, Freiburg (Chair), K. Berger, Münster; HR. Figulla, Jena; C. Hamm, Bad Nauheim; P. Hanrath, Aachen; W. Köpcke, Münster; C. Weimar, Essen; A. Zeiher, Frankfurt. http://www.recall-studie.uni-essen.de.
Conflict of interest: A.S. received a research grant by Imatron Inc., South San Francisco.
References
- 1.Fox CS, Evans C, Larson MG, Evans JC, Kannel WB, Levy D. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999. Circulation. 2004;110:522–527. doi: 10.1161/01.CIR.0000136993.34344.41. [DOI] [PubMed] [Google Scholar]
- 2.De Vreede-Swagemakers JJM, Gorgels APM, Dubois-Arbouw WI, van Ree JW, Daemen MJ, Houben LG, Wellens HJ. Out-of-hospital cardiac arrest in the 1990’s: a population-based study in the Maastricht area on incidence, characteristics and survival. J Am Coll Cardiol. 1997;30:1500–1505. doi: 10.1016/s0735-1097(97)00355-0. [DOI] [PubMed] [Google Scholar]
- 3.Löwel H, Meisinger C, Heier M, Hörmann A, von Scheidt W. Herzinfarkt und koronare Sterblichkeit in Süddeutschland. Deutsches Ärzteblatt. 2005;103:A616–A622. [Google Scholar]
- 4.Chambless L, Keil U, Dobson A, Mähönen M, Kuulasmaa K, Rajakangas AM, Löwel H, Tunstall-Pedoe H. Population versus clinical view of case fatality from acute coronary heart disease: results from the WHO MONICA Project 1985–1990. Multinational MONItoring of Trends and Determinants in CArdiovascular Disease. Circulation. 1997;96:3849–3859. doi: 10.1161/01.cir.96.11.3849. [DOI] [PubMed] [Google Scholar]
- 5.Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PW, Wolf PA, Levy D. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 6.Assmann G, Schulte H, Cullen P, Seedorf U. Assessing risk of myocardial infarction and stroke: new data from the Prospective Cardiovascular Münster (PROCAM) study. Eur J Clin Invest. 2007;37:925–932. doi: 10.1111/j.1365-2362.2007.01888.x. [DOI] [PubMed] [Google Scholar]
- 7.Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, Dallongeville J, De Backer G, Ebrahim S, Gjelsvik B, Herrmann-Lingen C, Hoes A, Humphries S, Knapton M, Perk J, Priori SG, Pyorala K, Reiner Z, Ruilope L, Sans-Menendez S, Op Reimer WS, Weissberg P, Wood D, Yarnell J, Zamorano JL. ESC Committee for Practice Guidelines European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Atherosclerosis. 2007;194:1–45. doi: 10.1016/j.atherosclerosis.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 8.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Jr, Stone NJ. Coordinating Committee of the National Cholesterol Education Program. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol. 2004;44:720–732. doi: 10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 9.Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) J Am Med Assoc. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 10.Taylor AJ, Bairey CN, Udelson JE. 34th Bethesda Conference: ‘Can atherosclerosis imaging techniques improve the detection of patients at risk for ischemic heart disease? J Am Coll Cardiol. 2003;41:1855–1917. doi: 10.1016/s0735-1097(03)00363-2. [DOI] [PubMed] [Google Scholar]
- 11.Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, Guerci AD, Lima JA, Rader DJ, Rubin GD, Shaw LJ, Wiegers SE American Heart Association Committee on Cardiovascular Imaging and Intervention; American Heart Association Council on Cardiovascular Radiology and Intervention; American Heart Association Committee on Cardiac Imaging, Council on Clinical Cardiology. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 12.Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, Lauer MS, Post WS, Raggi P, Redberg RF, Rodgers GP, Shaw LJ, Taylor AJ, Weintraub WS, Harrington RA, Abrams J, Anderson JL, Bates ER, Grines CL, Hlatky MA, Lichtenberg RC, Lindner JR, Pohost GM, Schofield RS, Shubrooks SJ, Jr, Stein JH, Tracy CM, Vogel RA, Wesley DJ American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography); Society of Atherosclerosis Imaging and Prevention; Society of Cardiovascular Computed Tomography. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) Circulation. 2007;115:402–426. doi: 10.1161/CIRCULATIONAHA..107.181425. [DOI] [PubMed] [Google Scholar]
- 13.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacobs DR, Kronmal R, Liu K, Nelson JC, ÒLeary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 14.Schmermund A, Möhlenkamp S, Stang A, Grönemeyer D, Seibel R, Hirche H, Mann K, Siffert W, Lauterbach K, Siegrist J, Jöckel KH, Erbel R. Assessment of clinically silent atherosclerotis disease and established and novel risk factors for predicting myocardial infarction and cardiac death in healthy middle-aged subjects: Rationale and design of the Heinz Nixdorf RECALL Study. Am Heart J. 2002;144:212–218. doi: 10.1067/mhj.2002.123579. [DOI] [PubMed] [Google Scholar]
- 15.Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Sahar E, Iuyang P, Jackson S, Saad MF. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclersosis (MESA) Circulation. 2005;111:1313–1320. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 16.McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2006;113:30–37. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]
- 17.Kronmal RA, McClelland RL, Detrano R, Shea S, Lima JA, Cushman M, Bild DE, Burke GL. Risk factors for the progression of coronary artery calcification in asymptomatic subjects: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2007;115:2722–2730. doi: 10.1161/CIRCULATIONAHA.106.674143. [DOI] [PubMed] [Google Scholar]
- 18.Stang A, Moebus S, Dragano N, Beck EM, Möhlenkamp S, Schmermund A, Siegrist J, Erbel R, Jöckel KH on behalf of the Heinz Nixdorf Study Investigative Group. Baseline recruitment and analyses of non-response of the Heinz Nixdorf Recall Study: Identifiability of phone numbers as the major determinant of response. Eur J Epidemiol. 2005;20:489–496. doi: 10.1007/s10654-005-5529-z. [DOI] [PubMed] [Google Scholar]
- 19.Schmermund A, Möhlenkamp S, Berenbein S, Pump H, Moebus S, Roggenbuck U, Stang A, Seibel R, Grönemeyer D, Jöckel KH, Erbel R. Population-based assessment of subclinical coronary atherosclerosis using electron-beam computed tomography. Atherosclerosis. 2006;185:177–182. doi: 10.1016/j.atherosclerosis.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 20.Erbel R, Möhlenkamp S, Lehmann N, Schmermund A, Moebus S, Stang A, Grönemeyer D, Seibel R, Mann K, Volbracht L, Dragano N, Siegrist J, Jöckel KH on behalf of the Heinz Nixdorf Recall Study Investigative Group. Sex related cardiovascular risk stratification based on quantification of atherosclerosis and inflammation. Atherosclerosis. 2008;197:662–672. doi: 10.1016/j.atherosclerosis.2007.02.031. [DOI] [PubMed] [Google Scholar]
- 21.Stang A, Moebus S, Möhlenkamp S, Dragno N, Schmermund A, Beck EM, Siegrist J, Erbel R, Jöckel KH on behalf of the Heinz Nixdorf Recall Study Investigative Group. Algorithms for converting random-zero to automated oscillometric blood pressure values, vice versa. Am J Epidemiol. 2006;164:85–94. doi: 10.1093/aje/kwj160. [DOI] [PubMed] [Google Scholar]
- 22.Nasir K, Budoff MJ, Wong ND, Scheuner M, Herrington D, Arnett DK, Szklo M, Greenland P, Blumenthal RS. Family history of premature coronary heart disease and coronary artery calcification: Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2007;116:619–626. doi: 10.1161/CIRCULATIONAHA.107.688739. [DOI] [PubMed] [Google Scholar]
- 23.Jöckel KH, Lehmann N, Jaeger BR, Moebus S, Möhlenkamp S, Schmermund A, Dragano N, Stang A, Grönemeyer D, Seibel R, Mann K, Volbracht L, Siegrist J, Erbel R on behalf of the Heinz Nixdorf Recall Investigation Group. Smoking behaviour and subclinical atherosclerosis—results from the Heinz Nixdorf Recall Study. Atherosclerosis. 2008 doi: 10.1016/j.atherosclerosis.2008.05.041. (e-pub ahead of print) [DOI] [PubMed] [Google Scholar]
- 24.Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs DR, Jr, Sidney S, Bild DE, Williams OD, Detrano RC. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) Study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 25.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 26.Schmermund A, Pump H, Möhlenkamp S, Stang A, Grönemeyer D, Seibel R, Erbel R für die Heinz Nixdorf Recall Studiengruppe. Nachweis einer exzellenten Befundübereinstimmung (K 0. 94) der Koronarkalkmessung mittels Elektronenstrahltomographie in der Heinz Nixdorf Recall Studie. Z Kardiol. 2003;92:I/385. [Google Scholar]
- 27.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;291:210–215. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 28.Vliegenthart R, Oudkerk M, Hofman A, Oei HH, van Dijck W, van Rooij FJ, Witteman JC. Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation. 2005;112:572–577. doi: 10.1161/CIRCULATIONAHA.104.488916. [DOI] [PubMed] [Google Scholar]
- 29.Schmermund A, Lehmann N, Bielak LF, Yu P, Sheedy PF, 2nd, Cassidy-Bushrow AE, Turner ST, Moebus S, Möhlenkamp S, Stang A, Mann K, Jöckel KH, Erbel R, Peyser PA. Comparison of subclinical coronary atherosclerosis and risk factors in unselected populations in Germany and US-America. Atherosclerosis. 2007;195:e207–e216. doi: 10.1016/j.atherosclerosis.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shaw LJ, Bairey Merz CN, Pepine CJ, Reis SE, Bittner V, Kelsey SF, Olson M, Johnson BD, Mankad S, Sharaf BL, Rogers WJ, Wessel TR, Arant CB, Pohost GM, Lerman A, Quyyumi AA, Sopko G WISE Investigators. Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: Part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J Am Coll Cardiol. 2006;47(Suppl. 3):S4–S20. doi: 10.1016/j.jacc.2005.01.072. [DOI] [PubMed] [Google Scholar]
- 31.Bairey Merz CN, Shaw LJ, Reis SE, Bittner V, Kelsey SF, Olson M, Johnson BD, Pepine CJ, Mankad S, Sharaf BL, Rogers WJ, Pohost GM, Lerman A, Quyyumi AA, Sopko G WISE Investigators. Insights from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: Part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol. 2006;47(Suppl. 3):S21–S29. doi: 10.1016/j.jacc.2004.12.084. [DOI] [PubMed] [Google Scholar]
- 32.Heidemann C, Hoffmann K, Klipstein-Grobusch K, Weikert C, Pischon T, Hense HW, Boeing H. Potentially modifiable classic risk factors and their impact on incident myocardial infarction: results from the EPIC-Potsdam study. Eur J Cardiovasc Prev Rehabil. 2007;14:65–71. doi: 10.1097/01.hjr.0000238392.19847.4c. [DOI] [PubMed] [Google Scholar]
- 33.Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, Joffres M, Kastarinen M, Poulter N, Primatesta P, Rodríguez-Artalejo F, Stegmayr B, Thamm M, Tuomilehto J, Vanuzzo D, Vescio F. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. J Am Med Assoc. 2003;289:2363–2369. doi: 10.1001/jama.289.18.2363. [DOI] [PubMed] [Google Scholar]
- 34.Teo KK, Ounpuu S, Hawken S, Pandey MR, Valentin V, Hunt D, Diaz R, Rashed W, Freeman R, Jiang L, Zhang X, Yusuf S INTERHEART Study Investigators. Tobacco use and risk of myocardial infarction in 52 countries in the INTERHEART study: a case-control study. Lancet. 2006;368:647–658. doi: 10.1016/S0140-6736(06)69249-0. [DOI] [PubMed] [Google Scholar]
- 35.Ashraf H. European tobacco control reaches a critical phase. Lancet. 2002;359:585–586. doi: 10.1016/S0140-6736(02)07767-X. [DOI] [PubMed] [Google Scholar]
- 36.Arnett DK, Jacobs DR, Jr, Luepker RV, Blackburn H, Armstrong C, Claas SA. Twenty-year trends in serum cholesterol, hypercholesterolemia, and cholesterol medication use: the Minnesota Heart Survey, 1980–1982 to 2000–2002. Circulation. 2005;112:3884–3891. doi: 10.1161/CIRCULATIONAHA.105.549857. [DOI] [PubMed] [Google Scholar]
- 37.Koenig W, Khuseyinova N, Baumert J, Meisinger C, Löwel H. Serum concentrations of adiponectin and risk of type 2 diabetes mellitus and coronary heart disease in apparently healthy middle-aged men: results from the 18-year follow-up of a large cohort from southern Germany. J Am Coll Cardiol. 2006;48:1369–1377. doi: 10.1016/j.jacc.2006.06.053. [DOI] [PubMed] [Google Scholar]
- 38.Breckenkamp J, Mielck A, Razum O. Health inequalities in Germany: do regional-level variables explain differentials in cardiovascular risk? BMC Public Health. 2007;7:132. doi: 10.1186/1471-2458-7-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O’Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 40.Nauck M, Warnick GR, Rifai N. Methods for measurement of LDL-cholesterol: a critical assessment of direct measurement by homogeneous assays versus calculation. Clin Chem. 2002;48:236–254. [PubMed] [Google Scholar]