Abstract
We examined age-related differences in frontal plane stability during performance of narrow base (NB) walking relative to usual gait. A cross-sectional analysis of participants from the Baltimore Longitudinal Study of Aging (BLSA) was performed on data from the BLSA Motion Analysis Laboratory. Participants were thirty-four adults aged 54 to 92 without history of falls. We measured step error rates during NB gait and spatial-temporal parameters, frontal plane stability, and gait variability during usual and NB gait. There was a non-significant age-associated linear increase in step error rate (P = 0.12) during NB gait. With increasing age, step width increased (P=0.002) and step length and stride velocity decreased (P<0.001), especially during NB gait. Age-associated increases in medio-lateral (M-L) center of mass (COM) peak velocity (P<0.001) and displacement (P=0.005) were also greater during NB compared to usual gait. With increasing age there was greater variability in stride velocity (P=0.001) and step length (P<0.001) under both conditions. Age-associated differences related to M-L COM stability suggest that the quantification of COM control during NB gait may improve identification of older persons at increased falls risk.
Keywords: Mobility, aging, tandem walk, postural control, frontal plane stability
INTRODUCTION
Mobility, defined as the ability to move from place to place in one’s environment, is crucial to maintaining independence and quality of life in older persons. Diminished mobility leads to increased risk for morbidity, disability, and mortality [1]. Poor balance is a major factor in age-related declines in mobility and increased risk for falls in older adults [2]. Furthermore, falls in older adults occur most commonly during walking [3]. Therefore, an improved understanding of factors that contribute to functional walking limitations is critical in order to postpone or prevent functional declines in mobility and reduce fall risk in older adults.
Instability during walking is primarily in the medio-lateral (M-L) direction [4, 5], and loss of M-L stability has a particularly profound effect on walking function. Declines in M-L stability during stance and gait have been shown to be a major risk factor for falls in older adults [5]. In addition, balance-impaired older adults demonstrate greater and faster lateral motion of the center of mass (COM) during obstacle crossing than young adults [6]. Thus, changes in M-L COM motion during unobstructed level walking compared to an adaptive gait task such as obstacle crossing may be useful as indicators of fall risk. Similarly, narrow base and tandem walking are adaptive walking tasks that are often used to evaluate stability [7] because of the increased demands on frontal plane stability. Performance on the tandem walk test has been shown to predict falls [8] among community-dwelling older women. However, age-related changes in M-L COM motion during narrow versus usual base walking are not well understood.
The purpose of this study was to examine age-related changes in frontal plane stability during performance of a narrow base (NB) walking task compared to unobstructed level walking (i.e. usual gait). We also examined factors that potentially predict changes in M-L COM motion during performance of NB walking, such as step width, gait velocity, step length, and variability in each of these parameters. We hypothesized that M-L COM motion would increase with age, indicating an inefficient control of frontal plane stability when walking within a narrowed base of support.
METHODS
Participants
Participants were community-dwelling volunteers between 54 and 92 years of age who were enrolled in the Baltimore Longitudinal Study of Aging (BLSA) (Table 1), an ongoing observational study of normal aging initiated in 1958 [9]. As part of the BLSA visit, all participants in the present study received a complete medical history and physical examination visit, including history of falls, and ADL/IADL disability. Exclusion criteria for the gait evaluation included an inability to walk without assistance (from an assistive device or another person), legal blindness, an inability to follow instructions due to cognitive impairment, and the report of one or more fall in the previous 12 months. In the previous 12 months, three participants reported ADL disability and nine reported IADL disability. The number of comorbidities was determined based on a simple count of affirmative responses to questions addressing several clinical conditions, such as hypertension, cancer, acute myocardial infarction, stroke, diabetes mellitus, arthritis, or other neurological disease. Compared with previous work [10], participants in the current study had relatively few comorbidities (1.6 ± 1.3 and 1.4 ± 1.1 for men and women, respectively). An independent institutional review board approved the BLSA study protocol (IRB number: Medstar 2003-076), and participants provided informed consent for all gait testing procedures.
Table 1.
Subject Characteristics
| Men (n = 18) | Women (n = 16) | |
|---|---|---|
| Age, yr | 74.7 ± 12.9 | 68.3 ± 10.5 |
| Height, cm | 172.2 ± 0.06 | 162.3 ± 0.06 |
| Weight, kg | 79.8 ± 10.8 | 85.9 ± 16.6 |
| BMI, kg/m2 | 26.9 ± 3.3 | 26.7 ± 4.0 |
| Number of medications | 2.8 ± 2.3 | 4.9 ± 3.2 |
| Number of comorbidities | 1.6 ± 1.3 | 1.4 ± 1.1 |
Values are means ± SD for all measures.
Experimental Protocol
Participants were asked to perform 3–4 trials of both usual and narrow base of support (NB) walking along a 6-m walkway. Usual gait trials were performed first, followed by NB gait trials. In all gait trials, participants were asked to walk at a comfortable pace. For the NB trials, participants were asked to walk within a narrow path outlined by tape on the walking surface. The width of the narrow path was standardized to 50% of the distance between the subject’s anterior superior iliac spines. For familiarization with the NB task, participants were given 2 practice trials. Retro-reflective markers were used to visualize the narrow path in the motion capture and analysis software and to detect step errors.
A set of 37 retro-reflective markers was placed on bony landmarks of the arms, legs, trunk, and head, and a six-camera VICON motion analysis system (VICON Motion Systems, Inc., Lake Forest, CA) was used to collect 3-dimensional marker trajectory data at 60 Hz. Visual 3-D software (C-Motion, Rockville, MD) was used to create a 13-segment biomechanical model, and the location of the whole body COM was calculated as the weighted sum of each body segment’s COM. This model included six links for the lower extremities, four links for the upper extremities, one for the pelvis, one for the trunk, and one for the head. The trajectory of the COM during each trial was then computed using Visual 3-D software.
Custom software (RP, University of Washington) was then used to calculate step and stride characteristics, including spatial-temporal and center of mass variables. Stride velocity was calculated as the velocity from the heel strike of one foot to the next heel strike of that same foot. Step width and step length were calculated as the distance (width and length) between heel strike of one foot to heel strike of the opposite foot. For the NB gait trials, a step error was defined as any step in which the ankle marker was detected outside the narrow path at foot strike, and error rates were calculated for each subject in the NB condition. The M-L COM displacement was defined as the maximum minus the minimum value of the COM in the medio-lateral direction during a single stride. Peak M-L COM velocity was defined as the maximum M-L velocity of the COM during a single stride.
Statistical Analysis
For each subject, the mean and standard deviation (SD) for each variable were calculated using all valid steps or strides within a given walking condition. Variability for all parameters was calculated as the coefficient of variation (CV). The mean (SD) number of strides for each subject was 8.2 (0.6) in the usual gait condition and 10.6 (1.2) in the NB gait condition. Linear regression models for repeated measures [11] were used to analyze the potential associations between age and spatial-temporal parameters; age and COM parameters; and age and stride velocity-adjusted COM parameters. We also evaluated expected main effects of trial condition (usual vs. NB gait) on these parameters. To do so, a dichotomous term for trial condition (usual vs. NB gait) was included in the linear regression models, which allowed for the simultaneous analysis of both trial conditions. Potential 2-way interactions were evaluated. Whether a significant ‘age × condition’ interaction term existed was of particular interest because such an interaction could indicate that age-associated changes in performance may be more or less apparent with NB compared to usual gait. The analysis of stride velocity-adjusted data was based on recent findings suggesting that gait velocity affects not only anterior-posterior [12, 13] but also lateral gait parameters [14]. Results shown include both accurate and inaccurate steps, but similar results were found when only accurate steps were analyzed.
The compound symmetry correlation structure applied in this study fit the data best according to the Akaike's information criterion [11], and the repeated measures design of the analyses allowed for inclusion of all of the individual step and stride data collected. For the purposes of graphical presentation, however, mean subject data were used (Figure 1–Figure 3). All analyses were performed using the SAS statistical software version 8.2 (SAS Institute, Cary, NC).
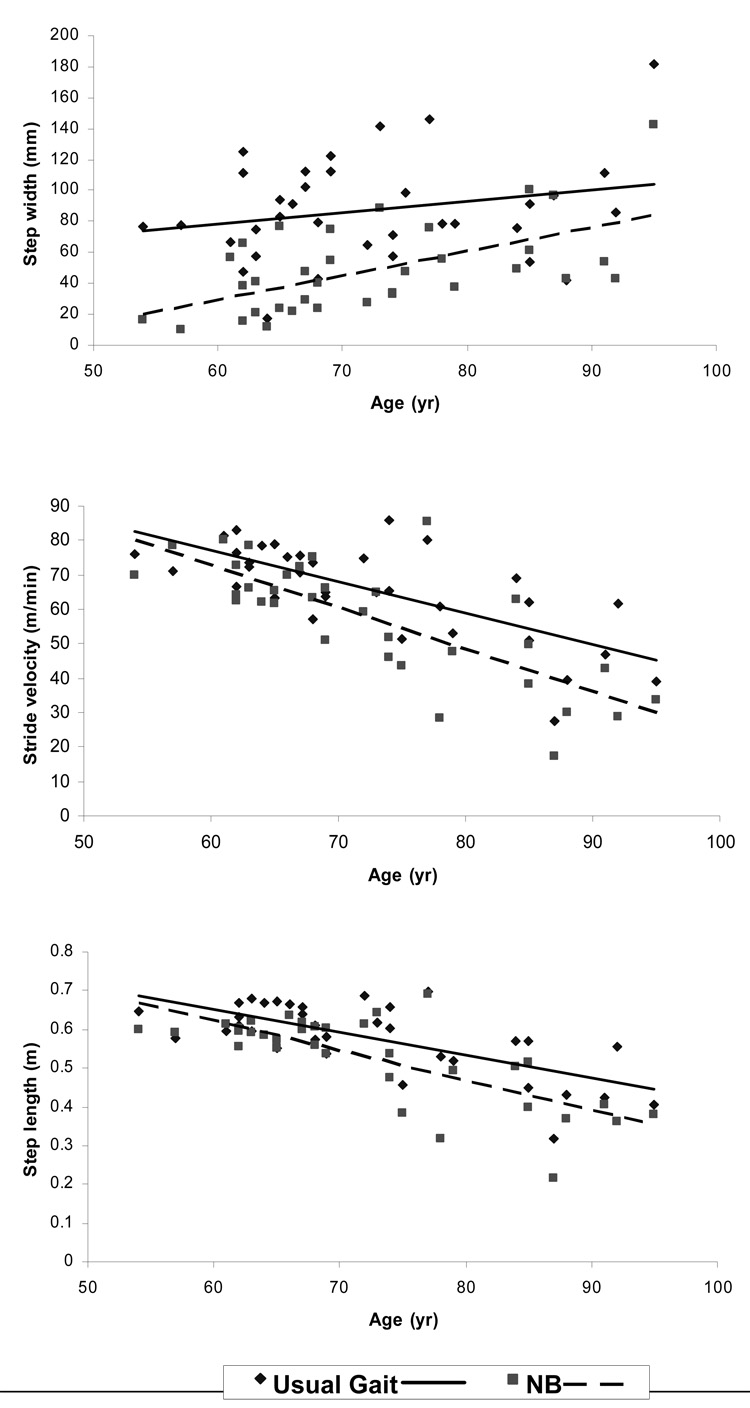
Figure 1.
Relationships between age and spatial-temporal parameters under usual and narrow base (NB) gait conditions.
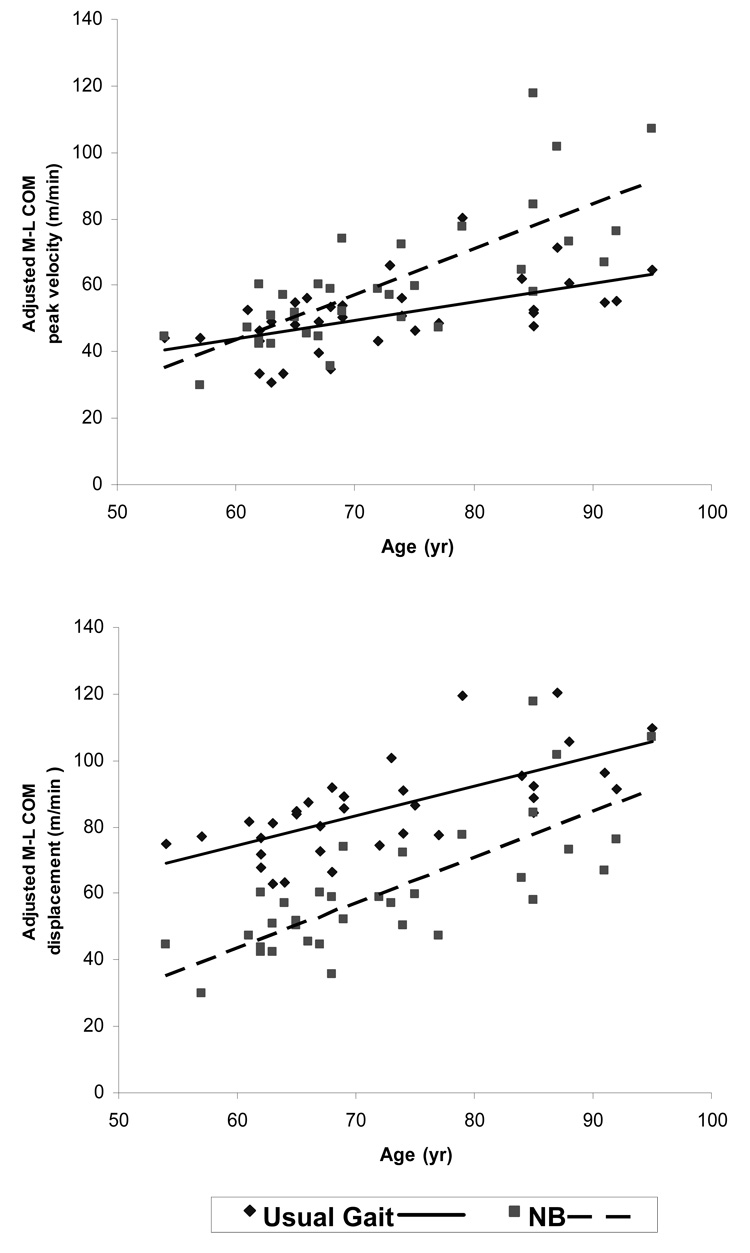
Figure 3.
Relationships between age and stride velocity-adjusted COM parameters under usual and narrow base (NB) gait conditions.
RESULTS
Performance of Narrow Base Gait Task
There was a non-significant age-associated linear increase in step error rate (P = 0.12) during NB gait. During the NB compared to the usual gait condition, participants walked with a narrower step width, shorter step length, slower velocity, and reduced M-L COM peak velocity and displacement (all P < 0.001).
Spatial-Temporal Characteristics During Usual and NB Gait
Figure 1 shows the significant age-associated declines in stride velocity (P < 0.001) and step length (P < 0.001) under both usual and NB gait conditions. The significant ‘age × condition’ interactions for the 3 spatial-temporal parameters (Table 2) indicated that age-associated changes in all 3 spatial-temporal variables were more marked in the NB condition than in usual gait.
Table 2.
Linear regression model on the relationship between spatiotemporal, COM, and stride velocity-adjusted COM parameters and age and test condition
| Age | Condition | Age × Condition | |
|---|---|---|---|
| Spatial-Temporal Variable | |||
| Step Width | |||
| β ± SE | 0.78 ± 0.43 | −90.3 ± 16.8 | 0.71 ± 0.22 |
| P | 0.081 | <0.001 | 0.002 |
| Step Length | |||
| β ± SE | −0.006 ± 0.001 | 0.11 ± 0.03 | −0.002 ± 0.0004 |
| P | <0.001 | <0.001 | <0.001 |
| Stride Velocity | |||
| β ± SE | −0.88 ± 0.15 | 20.7 ± 3.8 | −0.40 ± 0.05 |
| P | <0.001 | <0.001 | <0.001 |
| COM Variable | |||
| M-L Peak Velocity | |||
| β ± SE | 0.05 ± 0.02 | −8.05 ± 0.93 | 0.060 ± 0.01 |
| P | 0.020 | <0.001 | <0.001 |
| M-L Displacement | |||
| β ± SE | 0.55 ± 0.14 | −30.8 ± 7.7 | 0.25 ± 0.10 |
| P | <0.001 | <0.001 | 0.016 |
| Stride velocity−adjusted COM Variable | |||
| M-L Peak Velocity | |||
| β ± SE | 0.57 ± 0.14 | −37.7 ± 7.7 | 0.29 ± 0.10 |
| P | <0.001 | <0.001 | 0.005 |
| M-L Displacement | |||
| β ± SE | 0.91 ± 0.16 | −60.6 ± 8.2 | 0.48 ± 0.11 |
| P | <0.001 | <0.001 | <0.001 |
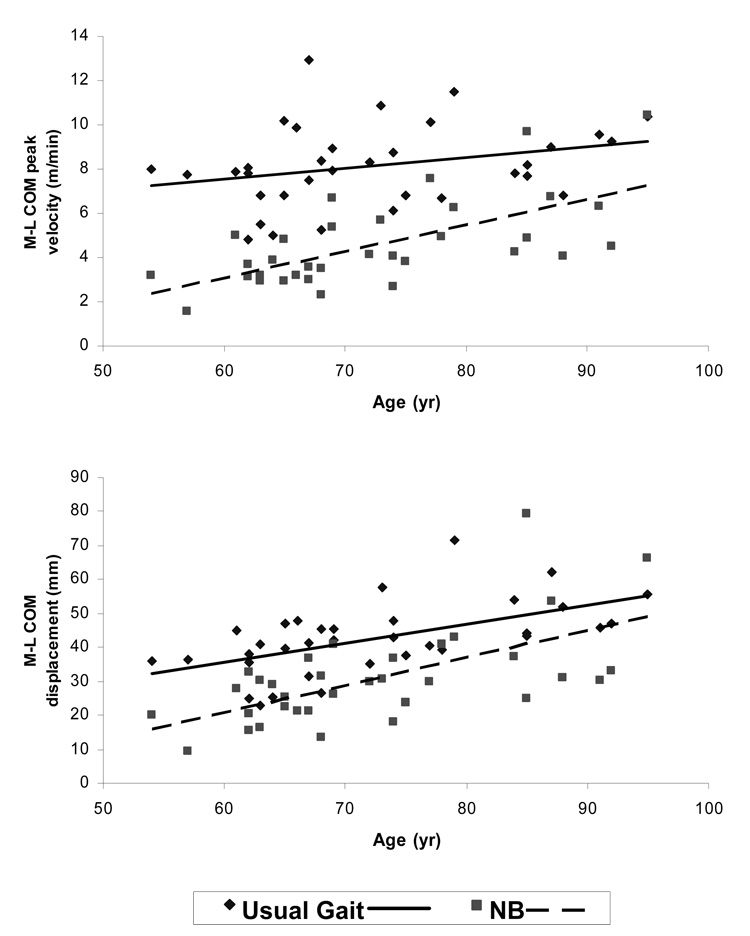
COM Parameters During Usual and NB Gait
Significant age-associated increases in M-L COM peak velocity (P = 0.02) and displacement (P < 0.001) were seen under both usual and NB gait conditions (Figure 2). Significant ‘age × condition’ effects were found with M-L COM peak velocity and displacement (Table 2). These interactions indicate that, relative to usual gait, the NB condition elicited disproportionately higher values in M-L COM peak velocity and displacement with increasing age, consistent with diminished M-L COM control.
Figure 2.
Relationships between age and COM parameters under usual and narrow base (NB) gait conditions.
Stride Velocity-Adjusted COM Parameters During Usual and NB Gait
As shown in Table 2 and Figure 3, after adjusting for potential effects of stride velocity on M-L COM motion, significant effects of age on M-L COM peak velocity (P < 0.001) and M-L COM displacement remained significant (P < 0.001). After adjusting for potential effects of stride velocity on M-L COM motion, the significant ‘age × condition’ interaction effects found in the unadjusted data persisted, indicating greater age-associated increases in M-L COM peak velocity (P = 0.005) and displacement (P < 0.001) in NB gait relative to usual gait that were independent of age-related differences in stride velocity.
Variability in Spatial-temporal and COM Parameters During Usual and NB Gait
Table 3 shows the variability in spatial-temporal and COM parameters during NB gait for all participants. There was no significant age-associated increase in variability of step idth or COM parameters. However, with increasing age there was a greater degree of variability in stride velocity (P = 0.001) and step length (P < 0.001) under both conditions, as indicated by significant age main effects.
Table 3.
Linear regression model on the relationship between variability of spatiotemporal and COM parameters and age and test condition
| Age | Condition | Age × Condition | |
|---|---|---|---|
| Spatial−Temporal Variable | |||
| Step Width | |||
| β ± SE | −0.33 ± 0.39 | −17.6 ± 40.1 | −0.02 ± 0.55 |
| P | 0.22 | <0.66 | 0.98 |
| Stride Velocity | |||
| β ± SE | 0.29 ± 0.09 | 4.5 ± 9.4 | −0.12 ± 0.13 |
| P | 0.001 | 0.63 | 0.33 |
| Step Length | |||
| β ± SE | 0.42 ± 0.07 | 8.5 ± 7.2 | −0.18 ± 0.10 |
| P | <0.001 | 0.24 | 0.067 |
| COM Variable | |||
| M-L Peak Velocity | |||
| β ± SE | −0.03 ± 0.21 | −11.7 ± 21.7 | −0.01 ± 0.30 |
| P | 0.82 | 0.59 | 0.97 |
| M-L Displacement | |||
| β ± SE | −0.22 ± 0.17 | −18.0 ± 17.2 | 0.09 ± 0.23 |
| P | 0.14 | 0.30 | 0.71 |
DISCUSSION
This study evaluated the effects of age on frontal plane stability in individuals walking with a usual and a narrow base of support. These data indicated that an age-related decline in the ability to successfully perform a narrow base task was associated with hanges in spatial-temporal and M-L COM parameters that were more marked in NB versus usual gait. Specifically, age-associated increases in step width and decreases in step length and stride velocity were greater when walking with a narrow base of support compared to a usual base of support. Even when adjusted for stride velocity, the significant age-associated increases in M-L COM velocity and displacement remained greater under NB compared to usual base of support conditions.
These data suggest that in performing the narrow base task, older persons utilized a more conservative strategy marked by greater step width, shorter step length, and lower stride velocity. Despite employing this more conservative strategy, the oldest participants committed more step errors and demonstrated greater M-L COM movement. Adjustment for the known effects of walking speed on M-L COM motion [14] did not eliminate the age effects on either M-L COM parameter, suggesting that other factors such as decreased vestibular function [15] or hip abductor strength [16–18] may have contributed to increased COM motion in the frontal plane.
Stride-to-stride variability, as measured by CV, is considered a dependable marker of gait control [19] and has been used as a clinical index of gait steadiness [20, 21]. The data presented in this study demonstrated an age-associated increase in stride velocity and step length variability, consistent with previous research showing increased variability during usual walking and dual task walking in healthy, community-dwelling older adults [19, 22]. Because increased gait variability is an independent predictor of falling, it may be a useful measure for identifying high-risk individuals in advance of clinical signs and for evaluating fall-prevention interventions [19].
The adaptive gait test evaluated in the current study is similar to a widely used clinical test, the tandem walk test. Because walking with a narrowed base of support requires tight control of the COM in the frontal plane, age-related impairments in M-L COM control may help to explain why the tandem walk test has been shown to be a highly sensitive measure of fall risk in older adults [8, 21, 23].
One limitation of the present study was the sample size. A larger sample may have produced a greater effect of age on step error rate. In addition, the step errors were not separated according to degree, and larger errors may have been committed at a higher rate among the oldest individuals. Nevertheless, our data indicated the presence of age-related changes in the ability to successfully complete an adaptive gait task that required strict control of the COM in the frontal plane.
In conclusion, the quantification of frontal plane stability in addition to spatial-temporal parameters during narrow base walking reveals age-related changes in both the speed and the stability of walking under adaptive gait conditions. Future studies comparing fallers and non-fallers during narrow base walking will enhance our understanding of mechanisms of falls risk in older persons and may improve early identification of older persons at increased risk of falling.
ACKNOWLEDGEMENT
This research was supported (in part) by the Intramural Research Program of the NIH, National Institute on Aging. Data for these analyses were obtained from the Baltimore Longitudinal Study of Aging, a study performed by the National Institute on Aging.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Dunn JE, Rudberg MA, Furner SE, Cassel CK. Mortality, disability, and falls in older persons: the role of underlying disease and disability. Am J Public Health. 1992;82(3):395–400. doi: 10.2105/ajph.82.3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guralnik JM, LaCroix AZ, Abbott RD, Berkman LF, Satterfield S, Evans DA, Wallace RB. Maintaining mobility in late life. I. Demographic characteristics and chronic conditions. Am J Epidemiol. 1993;137(8):845–857. doi: 10.1093/oxfordjournals.aje.a116746. [DOI] [PubMed] [Google Scholar]
- 3.Rubenstein LZ, Josephson KR, Robbins AS. Falls in the nursing home. Ann Intern Med. 1994;121(6):442–451. doi: 10.7326/0003-4819-121-6-199409150-00009. [DOI] [PubMed] [Google Scholar]
- 4.Judge JO, Ounpuu S, Davis RB., 3rd Effects of age on the biomechanics and physiology of gait. Clin Geriatr Med. 1996;12(4):659–678. [PubMed] [Google Scholar]
- 5.Maki BE. Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc. 1997;45(3):313–320. doi: 10.1111/j.1532-5415.1997.tb00946.x. [DOI] [PubMed] [Google Scholar]
- 6.Chou LS, Kaufman KR, Hahn ME, Brey RH. Medio-lateral motion of the center of mass during obstacle crossing distinguishes elderly individuals with imbalance. Gait Posture. 2003;18(3):125–133. doi: 10.1016/s0966-6362(02)00067-x. [DOI] [PubMed] [Google Scholar]
- 7.Brown LA, Gage WH, Polych MA, Sleik RJ, Winder TR. Central set influences on gait. Age-dependent effects of postural threat. Exp Brain Res. 2002;145(3):286–296. doi: 10.1007/s00221-002-1082-0. [DOI] [PubMed] [Google Scholar]
- 8.Cho BL, Scarpace D, Alexander NB. Tests of stepping as indicators of mobility, balance, and fall risk in balance-impaired older adults. J Am Geriatr Soc. 2004;52(7):1168–1173. doi: 10.1111/j.1532-5415.2004.52317.x. [DOI] [PubMed] [Google Scholar]
- 9.Shock NWGR, Andres RA, Arenberg D, Costa PT, Lakatta EG, Tobin JD. Normal Human Aging: The Baltimore Longitudinal Study of Aging. Washington, DC: US Government Printing Office; 1984. [Google Scholar]
- 10.Shumway-Cook A, Ciol MA, Yorkston KM, Hoffman JM, Chan L. Mobility limitations in the Medicare population: prevalence and sociodemographic and clinical correlates. J Am Geriatr Soc. 2005;53(7):1217–1221. doi: 10.1111/j.1532-5415.2005.53372.x. [DOI] [PubMed] [Google Scholar]
- 11.Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. Vol. 458. Springer-Verlag; 2000. [Google Scholar]
- 12.Alexander NB. Gait disorders in older adults. J Am Geriatr Soc. 1996;44(4):434–451. doi: 10.1111/j.1532-5415.1996.tb06417.x. [DOI] [PubMed] [Google Scholar]
- 13.Ostrosky KM, VanSwearingen JM, Burdett RG, Gee Z. A comparison of gait characteristics in young and old subjects. Phys Ther. 1994;74(7):637–644. doi: 10.1093/ptj/74.7.637. discussion 644-6. [DOI] [PubMed] [Google Scholar]
- 14.Helbostad JL, Moe-Nilssen R. The effect of gait speed on lateral balance control during walking in healthy elderly. Gait Posture. 2003;18(2):27–36. doi: 10.1016/s0966-6362(02)00197-2. [DOI] [PubMed] [Google Scholar]
- 15.Kaya BK, Krebs DE, Riley PO. Dynamic stability in elders: momentum control in locomotor ADL. J Gerontol A Biol Sci Med Sci. 1998;53(2):M126–M134. doi: 10.1093/gerona/53a.2.m126. [DOI] [PubMed] [Google Scholar]
- 16.Maki BE, McIlroy WE. Control of rapid limb movements for balance recovery: age-related changes and implications for fall prevention. Age Ageing. 2006;35 Suppl 2:ii12–ii18. doi: 10.1093/ageing/afl078. [DOI] [PubMed] [Google Scholar]
- 17.MacKinnon CD, Winter DA. Control of whole body balance in the frontal plane during human walking. J Biomech. 1993;26(6):633–644. doi: 10.1016/0021-9290(93)90027-c. [DOI] [PubMed] [Google Scholar]
- 18.Chang SH, Mercer VS, Giuliani CA, Sloane PD. Relationship between hip abductor rate of force development and mediolateral stability in older adults. Arch Phys Med Rehabil. 2005;86(9):1843–1850. doi: 10.1016/j.apmr.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 19.Dubost V, Kressig RW, Gonthier R, Herrmann FR, Aminian K, Najafi B, Beauchet O. Relationships between dual-task related changes in stride velocity and stride time variability in healthy older adults. Hum Mov Sci. 2006;25(3):372–382. doi: 10.1016/j.humov.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Hausdorff JM, Edelberg HK, Mitchell SL, Goldberger AL, Wei JY. Increased gait unsteadiness in community-dwelling elderly fallers. Arch Phys Med Rehabil. 1997;78(3):278–283. doi: 10.1016/s0003-9993(97)90034-4. [DOI] [PubMed] [Google Scholar]
- 21.Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. Jama. 1989;261(18):2663–2668. [PubMed] [Google Scholar]
- 22.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050–1056. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- 23.Dargent-Molina P, Favier F, Grandjean H, Baudoin C, Schott AM, Hausherr E, Meunier PJ, Breart G. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet. 1996;348(9021):145–149. doi: 10.1016/s0140-6736(96)01440-7. [DOI] [PubMed] [Google Scholar]