Abstract
Segmental pedicle screw fixation is rapidly becoming a popular method of spinal instrumentation. Few studies have investigated the rates of adjacent superior segment facet joint violation. The purpose of our study were to investigate the incidence of superior segment facet joint violation after pedicle screw instrumentation in the lumbar spine and to evaluate technical factors related to the incidence. A prospective study including 96 patients who underwent lumbar and lumbosacral fusion was conducted between March 2006 and December 2007. All patients had bilateral or unilateral posterior pedicle screw-rod instrumentation with either CD-Horizon (top-loading screw) or TSRH (side-connecting screw) implants. Pedicle screws were instrumented according to the methods advocated by Roy-Camille (Group 1, 20 cases) or Weinstein (Group 2, 76 cases). All patients had computed tomography scan at 1 week post operation. CT scans were reviewed blind by an experienced spine research fellow and a consultant radiologist to determine violation of the adjacent superior segment facet joint. Superior segment facet joint violation occurred in all of the 20 patients (100%) and all of the top-level screws (100%) in Group 1. The spinal research fellow noted the incidence of facet joint violation to be present in 23.8% of the screws and 32.9% of the patients in Group 2, whereas the consultant radiologist noted this to be the case in 25.2 and 35.5%, respectively. The incidence of facet joint violation in patients with CD-Horizon screws was far lower than patients with TSRH screws (P < 0.001). In conclusion, it seems that meticulous surgical dissection without injuring the top-level facet joints, proper instrumentation of pedicle screws with the appropriate entry site (Weinstein’s method), trajectory, and use of top-loading screw heads are some ways that surgeons could minimize the risk of top-level facet joint violation.
Keywords: Pedicle screws, Facet joint violation, Lumbar spine
Introduction
The use of pedicle screw internal fixation in treating disease of the lumbar spine is becoming increasingly widespread [3, 11, 16]. Numerous studies have examined the complications from the use of pedicle screws [2, 7], however, few studies have investigated the rates of adjacent superior segment facet joint violation. The main problem at surgery is the possibility of violating superior level facet joint when the screws were inserted. It is most important that the facets between the fused and unfused areas not be injured at surgery, because this can predispose to degeneration and possibly even olisthesis at this level [1].
A thorough review of the literature revealed only 2 articles that studied the rates of superior level facet joint violation following transpedicular instrumentation in the lumbar spine. Shah et al. [13] were the first to study the incidence of adjacent superior segment facet joint violation with a Wiltse muscle-splitting approach. It was noted to be over 20% of involved top-level screws and over 30% of patients. Moshirfar et al. [10] found that superior level facet joint violation occurred in 24% of patients and 15% of screws via a midline approach. These two articles have studied the effect of surgical approach on the incidence. However, they did not study the influence of technical factors on the incidence of facet joint violation.
The purpose of our study were to investigate the incidence of superior segment facet joint violation after pedicle screw instrumentation in the lumbar spine and to evaluate technical factors related to the incidence, including: entry site selected to place the screw in the pedicle and screw used (top-loading screw or side-connecting screw).
Materials and methods
Between March 2006 and December 2007, this prospective study included 96 patients who underwent lumbar and lumbosacral fusion. The average age of the 44 males and 52 females patients was 49 years (range 19–78). There were 58 cases of degenerative disc disease, 11 cases of degenerative spondylolisthesis, 6 cases of lytic spondylolisthesis, 19 cases of degenerative stenosis with claudication, and 2 cases of degenerative scoliosis. There were 70 cases of single-level fusion (9 cases had unilateral pedicle screws), 19 cases of two-level, 5 cases of three-level, and 2 case of four-level fusion. Overall, there were 16 patients with L5 top-level screws (potential for impingement of L4–L5 facet), 53 with L4 top-level screws, 15 with L3 top-level screws, 7 with L2 top-level screws, and 5 cases with L1 top-level screws. Therefore, there were a total of 183 top-level screws (96 patients, 9 patients had unilateral pedicle screws) available for evaluation.
Instrumentation
All patients had bilateral or unilateral posterior pedicle screw-rod instrumentation with either CD-Horizon or TSRH (Medtronic Sofamor Danek, Memphis, TN, USA) titanium implants. Interbody fusion was performed with laminectomy bone and Telamon interbody cage (Medtronic Sofamor Danek, Memphis, TN, USA). All of the pedicle screws were instrumented by the senior author (J. Zhao) who routinely use these techniques for screw placement.
Surgical techniques
Bilateral dissection is extended to the transverse process through a midline posterior approach. Exposure for the superior facet joint required detachment of muscular insertions from the facet capsule, but care was taken to preserve the capsule itself. Each patient underwent decompression and discectomy as indicated, followed by interbody fusion using Telamon cage. Pedicle screws were instrumented by using anatomic landmarks according to the method advocated by Roy-Camille et al. [12] or Weinstein et al. [14]. Appropriate length rods were selected and properly contoured to avoid rods impingement on the adjacent facet joints. The method of Roy-Camille’s (Group 1) was used in the first 20 cases and Weinstein’s (Group 2) was adopted in the following consecutive 76 cases. Two types of screws were used in the top-level; top-loading screw (CD-Horizon) or side-connecting screw (TSRH). In the group 1, there were 24 top-loading screws and 16 side-connecting screws used in the top-level, and in the group 2, 114 top-loading screws (61 cases) and 29 side-connecting screws (15 cases) were used in the top-level.
Computed tomography (CT) evaluation
All patients had computed tomography scan at 1-week post operation. CT was performed with a Somatom Plus. With the use of a standard algorithm, 2-mm slices of the pedicles were made. CT scans were reviewed blindly by an experienced spine research fellow (observer 1, A. G. Liu) and a consultant radiologist (observer 2, J. D. Yuan) to determine violation of the adjacent superior segment facet joint. The facet joint violation was defined as the presence of either the screw, screw head/connector or the connecting rod being in line as well as abutting on or into the corresponding facet joint (Figs. 1, 2, 3, 4).
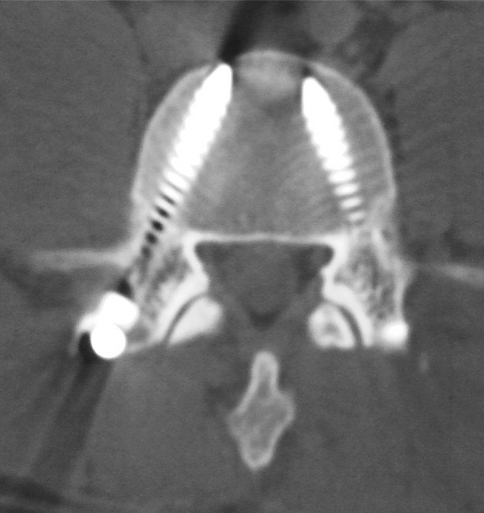
Fig. 1.
Axial CT scan showing no facet joint violation
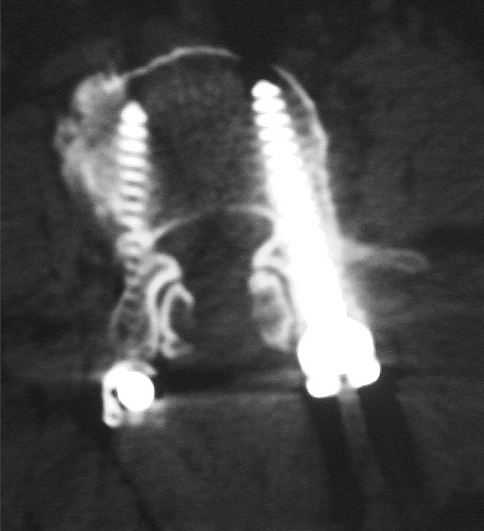
Fig. 2.
CT scan clearly shows bilateral pedicle screws within the facet joint
Fig. 3.
CT scan clearly shows the left pedicle screw head abutting the facet joint
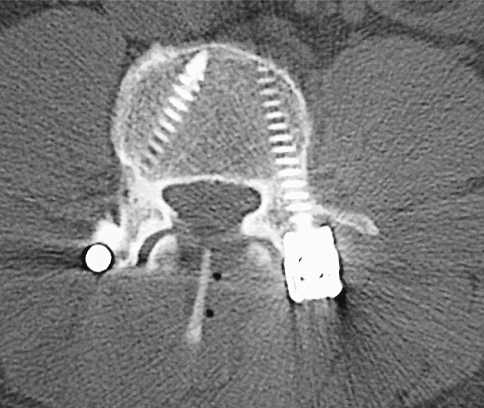
Fig. 4.
CT scan shows the connector of right pedicle screw abutting the facet joint. There was no facet joint violation on the left side because the connector was placed lateral to the screw
Statistical methods
Chi-squared analysis was carried out to determine the association between superior facet joint violation and technical factors (P < 0.05).
Results
In the group 1, 5 of the 40 screws showed penetration of the medial cortex of the pedicle (12.5%) on the CT scan. Of these, the length of penetration was in 4 screws between 0 and 2 mm, in one screw 2 and 4 mm. No penetration of the lateral cortex was seen. No neurological deficits were seen. Both observers noted that there was facet joint violation in all of the 40 (100%) top-level screws.
In the group 2, two screws showed penetration of the medial cortex of the pedicle (2.1%). The length of penetration was between 0 and 2 mm in the two screws. On the CT scan, observer 1 noted that there was facet joint violation in relation to 34 of 143 (24%) top-level screws, whereas observer 2 noted this to be the case in 36 of 143 (25%) (Table 1). The incidence of right- and left-sided screws was 18 of 72 (25%) and 16 of 71 (23%), respectively, which was not statistically significant (P = 0.7292). When TSRH screws were used in top-level, both observers noted the incidence of facet joint violation was 55% (16/29). When CD-Horizon screws were used, observer 1 noted the incidence of facet joint violation was 16% (18/114), whereas observer 2 noted this to be 18% (20/114). Taking the findings of the radiologist into consideration, There was statistical difference (P = 0.0001) in the incidence between CD-Horizon screws and TSRH screws.
Table 1.
Incidence of facet joint violation in relation to cephalad screws in Group 2
| Cephalad screws | No. violations (%) | |
|---|---|---|
| Observer 1 | Observer 2 | |
| Overall cephalad screws (n = 143) | 34 (24%) | 36 (25%) |
| CD-Horizon screws used (n = 114) | 18 (16%) | 20 (18%) |
| Most cephalad screw level | ||
| L1 (n = 5) | 0 | 0 |
| L2 (n = 5) | 0 | 1 (20%) |
| L3 (n = 16) | 2 (13%) | 2 (13%) |
| L4 (n = 70) | 9 (13%) | 9 (13%) |
| L5 (n = 18) | 7 (39%) | 8 (44%) |
| TSRH screws used (n = 29) | 16 (55%) | 16 (55%) |
| Most cephalad screw level | ||
| L1 (n = 4) | 3 (75%) | 3 (75%) |
| L2 (n = 3) | 2 (67%) | 2 (67%) |
| L3 (n = 6) | 3 (50%) | 3 (50%) |
| L4 (n = 14) | 6 (43%) | 6 (43%) |
| L5 (n = 2) | 2 (100%) | 2 (100%) |
In terms of the number of patients in group 2, observer 1 noted that there was facet joint violation in 25 of 76 cases (33%), whereas observer 2 noted the incidence to be 36% (Table 2). Evaluating patients with CD-Horizon screws in group 2, observer 1 and observer 2 noted the incidence of facet joint violation was 23% (14/61) and 26% (16/61), respectively. Both observers noted the incidence was 73% (11/15) in patients with TSRH screws The statistical difference in the incidence between CD-Horizon screws and TSRH screws was also significant (P = 0.0006) .
Table 2.
Incidence of facet joint violation in terms of the number of patients in Group 2
| Patients | No. violations (%) | |
|---|---|---|
| Observer 1 | Observer 2 | |
| Overall cases (n = 76) | 25 (33%) | 27 (36%) |
| CD-Horizon screws used (n = 61) | 14 (23%) | 16 (26%) |
| Most cephalad screw level | ||
| L1 (n = 3) | 0 | 0 |
| L2 (n = 3) | 0 | 1 (33%) |
| L3 (n = 8) | 2 (25%) | 2 (25%) |
| L4 (n = 38) | 8 (21%) | 8 (21%) |
| L5 (n = 9) | 4 (44%) | 5 (56%) |
| TSRH screws used (n = 15) | 11 (73%) | 11 (73%) |
| Most cephalad screw level | ||
| L1 (n = 2) | 2 (100%) | 2 (100%) |
| L2 (n = 2) | 2 (100%) | 2 (100%) |
| L3 (n = 3) | 2 (67%) | 2 (67%) |
| L4 (n = 7) | 4 (57%) | 4 (57%) |
| L5 (n = 1) | 1 (100%) | 1 (100%) |
Discussion
Segmental pedicle screw fixation is rapidly becoming a popular method of spinal instrumentation. Pedicle screw fixation can be very rigid and could result in increased stress transfer and accelerated degenerative change at unfused adjacent levels [4, 5, 9]. Others have disputed this, arguing that interference with adjacent facet joints by the hardware is a more likely cause for the observed effect [6]. Therefore, sufficient attention must be paid to preserve adjacent facet joints.
One risk factor related to instrumentation involves placement of the superior pedicle screw which, depending on the entry site selected, can damage the inferior facet of the adjacent segment [1, 15]. Numerous techniques for placing pedicle screw based solely on anatomic landmarks have been published. According to the method advocated by Roy-Camille [12], before insertion of screws, resection of the tip of inferior articular process was inevitable. The screw is then inserted straight ahead, parallel to the vertebral endplates. Whether it was used top-loading screw or side-connecting screw, superior facet joint violation is unavoidable. In our series, the incidence of superior facet joint violation in the group 1 (Roy-Camille group) was 100%. The facet joints are responsible for a significant amount of load-bearing role in extension [8]. Therefore, the sacrifice of the inferior tip of the facet and the violation of superior facet joint probably do produce some mechanical instability during extension.
The preferred entrance point advocated by Weinstein is at the lateral and inferior corner of the superior articular facet. The screw is then angled lateral to medial. Because the screws are positioned more laterally and their heads are further away from the adjoining facet joints, the Weinstein method is thought to preclude the instrumentation from interfering with the motion of the uninvolved segment cephalad to the arthrodesis [14]. The incidence of facet joint violation in the group 2 was far lower than group 1 in our study. But the incidence was still over 20%, it has shown that despite taking specific intraoperative precautions in terms of pedicle entry point to avoid facet joint violation, it was not possible to completely avoid it.
We also found the incidence of superior facet joint violation in side-connecting screws was much higher than top-loading screws used in top-level. Because side-connecting screws often need eyebolt or connector to connect the screw and rod, when it was placed medial to the screw, the violation of superior facet joint by connectors or rods was unavoidable. In our study, if the eyebolt was placed lateral to the screw, the violation of superior facet joint could be decreased. But this made nut tightening difficult, especially at L5. However, the head of top-loading screw (especially polyaxial screw) can position more laterally and the rods were placed superiorly to inferiorly. It can decrease the risk of impingement of pedicle screws and rods on the adjacent superior facet joint. In view of this, the screw entrance point and the type of screw used in top-level are thought to be important.
Conclusions
The incidence of superior segment facet joint violation was 100% in the patients whose pedicle screws were instrumented according to the method advocated by Roy-Camille. It was noted to be over 20% of involved top-level screws and over 30% of patients in the group that the pedicle screws were inserted by the Weinstein’s method. It showed that the incidence of top-level facet joint violation was significantly decreased by the use of top-loading screw heads.
Footnotes
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1.Aota Y, Kumano K, Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 1995;8:464–473. doi: 10.1097/00002517-199512000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Davne SH, Myers DL. Complications of lumbar spinal fusion with transpedicular instrumentation. Spine. 1992;17(suppl):184–189. doi: 10.1097/00007632-199206001-00021. [DOI] [PubMed] [Google Scholar]
- 3.Glaser J, Stanley M, Sayre H, et al. A 10-year follow-up evaluation of lumbar spine fusion with pedicle screw fixation. Spine. 2003;28:1390–1395. doi: 10.1097/00007632-200307010-00008. [DOI] [PubMed] [Google Scholar]
- 4.Guigui P, Wodecki P, Bizot P, et al. Long term influence of associated arthrodesis on adjacent segments in the treatment of lumbar stenosis: a series of 127 cases with 9-year follow-up. Rev Chir Orthop Repar Appar Mot. 2000;86:546–557. [PubMed] [Google Scholar]
- 5.Hambly MF, Wiltse LL, Raghavan N, et al. The transition zone above a lumbosacral fusion. Spine. 1998;23:1785–1792. doi: 10.1097/00007632-199808150-00012. [DOI] [PubMed] [Google Scholar]
- 6.Krag MH. Biomechanics of the thoracolumbar spinal fixation: a review. Spine. 1991;16:S84–S99. doi: 10.1097/00007632-199103001-00014. [DOI] [PubMed] [Google Scholar]
- 7.Lonstein JE, Denis F, Perra JH, et al. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81:1519–1528. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Lorenz M, Patwardhan A, Vanderby R. Load-bearing characteristics of lumbar facets in normal and surgically altered spinal segments. Spine. 1983;8:122–130. doi: 10.1097/00007632-198303000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Miyakoshi N, Abe E, Shimada Y, et al. Outcome of one-level posterior lumbar interbody fusion for spondylolisthesis and postoperative intervertebral disc degeneration adjacent to the fusion. Spine. 2000;25:1837–1842. doi: 10.1097/00007632-200007150-00016. [DOI] [PubMed] [Google Scholar]
- 10.Moshirfar A, Jenis LG, Spector LR, et al. Computed tomography evaluation of superior-segment facet-joint violation after pedicle instrumentation of the lumbar spine with a midline surgical approach. Spine. 2006;31:2624–2629. doi: 10.1097/01.brs.0000240691.35707.e8. [DOI] [PubMed] [Google Scholar]
- 11.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;203:7–17. [PubMed] [Google Scholar]
- 12.Roy-Camille R, Saillant G, Mazel C. Plating of thoracic, thoracolumbar, and lumbar injuries with pedicle screw plates. Orthop Clin North Am. 1986;17:147–159. [PubMed] [Google Scholar]
- 13.Shah RR, Mohammed S, Saifuddin A, et al. Radiologic evaluation of adjacent superior segment facet joint violation following transpedicular instrumentation of the lumbar spine. Spine. 2003;28:272–275. doi: 10.1097/00007632-200302010-00013. [DOI] [PubMed] [Google Scholar]
- 14.Weinstein JN, Spratt KF, Spengler D, et al. Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine. 1988;13:1012–1018. doi: 10.1097/00007632-198809000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Wiltse LL, Radecki SE, Biel HM, et al. Comparative study of the incidence and severity of degenerative change in the transition zones after instrumented versus noninstrumented fusions of the lumbar spine. J Spinal Disord. 1999;12:27–33. doi: 10.1097/00002517-199902000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Yahiro MA. Comprehensive literature review: pedicle screw fixation devices. Spine. 1994;19(suppl):2274–2278. doi: 10.1097/00007632-199410151-00004. [DOI] [PubMed] [Google Scholar]