Abstract
Introduction
Luminal pressure may injure the gut mucosa in obstruction, ileus, or IBD.
Methods
We formed Roux-en-Y anastomoses in 19 mice, creating proximal and defunctionalized partially obstructed limbs and a distal limb to vary luminal pressure and flow. We induced mucosal ulcers by serosal acetic acid, and assessed proliferation (PCNA) and ERK (immunoblotting). Parallel studies compared Caco-2 enterocyte migration and proliferation after pressure and/or ERK blockade.
Results
At 3 days, anastomoses were probe-patent, proximal and distal limbs contained chyme, and defunctionalized limbs were empty. The proximal and defunctionalized limbs exhibited increased pressure and slower healing despite increased proliferation, ERK protein and ERK activation. In vitro, pressure decreased Caco-2 migration across collagen or fibronectin, stimulated proliferation, and activated ERK. However, ERK blockade did not prevent pressure effects.
Conclusions
Luminal pressure during obstruction or ileus may impair mucosal healing independently of luminal flow despite increased mitosis and ERK activation.
Keywords: Force, mechanotransduction, migration, pressure, proliferation, Roux-en-y
Introduction
The intestinal mucosa experiences diverse forces in normal and diseased states. The small intestine mixes and propels the chyme by peristaltic and segmental contractions, pendular movements (1), and villous motility (2). The liquid luminal contents are largely non-compressible (3) and interact repetitively with the gut mucosa in complex ways as they pass along the villi (4). These forces all alter intra-luminal pressure, which along with other physiologic forces may support the normal gut mucosal cytoarchitecture (5).
However, supraphysiologic forces, such as elevated pressure, caused by diet or illness, may adversely impact gut physiology and mucosal healing (6). Luminal jejunal pressure reaches 50 mm Hg in irritable bowel syndrome (7). Intra-abdominal pressure may also increase after surgery due to tissue edema (8). Inflammation and injury increase luminal pressure in chronic inflammatory states such as Crohn’s disease or ulcerative colitis (9–11). Such increases in pressure could affect wound healing (5, 12).
The gut mucosa is constantly subjected to injuries that it must heal to maintain normal function (13) Biophysical forces in the gut stimulate intestinal epithelial proliferation and modulate intestinal epithelial differentiation in vitro (14), and activate mucosal tyrosine kinases in vivo (15) Mucosal repair is required for recovery from pathologic injury such as chronic ulceration and inflammation in inflammatory bowel disease, and is likely deficient when the mucosal barrier deteriorates in sepsis. (16, 17) Mucosal healing is affected in many pathophysiologic states that exhibit altered luminal pressure. Sepsis, ileus, fasting, and inflammatory bowel disease may be associated with altered contractile rhythms, villous motility, and mucosal deformation from luminal contents with consequent changes in luminal pressure. Ulcerative colitis, for example, exhibits decreased contractility, increased low-amplitude propagating contractions, and variable transit times (18). Anastomoses rupture at lower pressures in a rat inflammatory bowel disease model, suggesting impaired healing (19).
In vitro, repetitive deformation promotes intestinal epithelial proliferation and differentiation when the enterocytes are cultured on collagen or laminin substrates (20), but inhibits proliferation and promotes epithelial sheet migration on fibronectin substrates (21). However, the effects of physical forces on the biology of the intestinal mucosa in vivo are less clear, although repetitive deformation stimulates mucosal tyrosine kinase activity in anesthetized rats (15). Moreover, pressure may affect intestinal epithelial cells differently than repetitive deformation (12). It therefore becomes important to understand how increased pressure might modulate mucosal healing during altered intestinal homeostasis. We created a murine model of partial bowel obstruction in a defunctionalized jejunal Roux-en-Y limb in which the effects of luminal pressure were dissociated from luminal contents, and compared mucosal healing, proliferation, and ERK signaling among the proximal partially obstructed bowel, the defunctionalized partially obstructed bowel, and the bowel distal to the partial obstruction. We studied ERK because it critically mediates the effects of repetitive deformation on intestinal epithelial cells in vitro. (21) We validated our observations in vitro by studying the effects of extracellular pressure on human Caco-2 intestinal epithelial migration, proliferation, and ERK activation, and blocked ERK with the MEK inhibitor PD98059. Caco-2 cells are a common model for human intestinal epithelial biology. (22)
MATERIALS AND METHODS
In Vivo Studies
Roux-en-Y anastomosis
We created defunctionalized Roux limbs in C57 Black mice by an approved protocol. We divided the jejunum 1 cm from the ligament of Treitz with 5-0 silk, anastomosed the proximal jejunum side to side to the distal gut 2 cm distal to the original transection with 9-0 vicryl, and closed the abdomen with running 5-0 silk.
Pressure Determination within the murine small bowel
We assessed luminal pressures with a Stryker 295-1 Pressure Monitor (Kalamazoo, MI) before and three days after defunctionalized limb creation. The pressures measured in the animal model using the Stryker needle were on the order of 0–6 mmHg. Preliminary calibration demonstrated the accuracy of the needle and pressure monitor, measured against a clinical ICU pressure transducer (not shown). These pressures were reproducible, but notably lower than those reported in human unobstructed or obstructed bowel. (9–11) These differences may reflect species differences or the use of the Stryker needle technique in which the fluid is injected and the pressure peaks briefly before the fluid runs away into the measured space. However, the constraints generated by the closed and intact abdominal wall may also contribute substantially to measurements of bowel pressures in intact humans, and were absent when we measured bowel pressure in the mouse at necropsy. We therefore chose to apply a pressure of 80 mmHg to the human Caco-2 intestinal epithelial cells based upon literature reports of such pressures within the lumen of obstructed human bowel.
Mucosal ulcers
Paper disks pretreated with 70% acetic acid were applied to the small bowel serosa for 15 seconds to create circumscribed ischemic mucosal ulcers of predictable size, by a modification of a method for gastric ulcers (23). Ulcers were photographed and measured on a Kodak Image Station (Perkin Elmer, Boston, MA). Initial studies showed that this routinely produces jejunal mucosal ulcers of 3.1+/−0.3 mm2 in normal jejunum at ulcer induction.
Immunohistochemical studies of proliferation
Tissue from the proximal, distal and Roux limbs was fixed in 10 % formalin for 24 hours and embedded in paraffin. Five micron sections were stained for Proliferating Cell Nuclear Antigen (PCNA) (Zymed, CA), haematoxylin-counterstained for orientation, and visualized and photographed on a Nikon Microphot-FXA. These results were confirmed utilizing antibody against KI 67 (not shown).
Western Blotting
Samples were immediately immersed in 4oC lysis buffer, agitated by a Tissue Tearor (Biospec Products, Bartlesville, OK) at 10,000–15,000g, centrifuged at 12,000g for 30 min at 2°C, assayed for protein, subjected to Western blot for phospho-ERK Thr 202, Tyr204 or total ERK, and visualized using enhanced chemiluminescence as previously described (21). Membranes were re-probed for GAPDH and appropriate secondary antibody as a loading controls. All exposures were within the linear range.
In Vitro Studies
Cell culture
We studied Caco-2BBE intestinal epithelial cells, a subclone of the original Caco-2 cell line selected for its ability to differentiate in culture (24). Caco-2 cells were cultured as previously described.(25)
Pressure regulation
Pressure was controlled using a prewarmed airtight box with an inlet valve for gassing and an outlet connected to a manometer (5). Temperature was maintained within 2°C, and pressure within 1.5 mmHg.
Matrix and medium modulation
6-well dishes were pre-coated with 12.5 ug/mL collagen I or tissue fibronectin (Sigma, St Louis, MO) at saturating concentrations. Cells were seeded 50,000/well for proliferation studies and serum-starved for 24 hours. Cells seeded at 500,000/well were grown to confluence for migration assays. ERK was blocked by 20 mM MEK antagonist PD98059 (Calbiochem, La Jolla, CA) for 30 minutes before application of pressure to assess wound closure with inhibited ERK. Control cells were treated with a 0.1% DMSO vehicle control.
Motility measurement
Caco-2 monolayers on 6 well matrix-coated dishes were subjected to 0–80 mmHg increased pressure for 24 hours after induction of small uniform circular wounds as described. (26) We measured wound areas at 0 and 24 hours on a Kodak Image Station (Perkin Elmer, Boston, MA), and calculated percent closure.
Proliferation
Subconfluent (30–40%) cells were serum-starved for 24 hours. We reserved one 6-well plate for a time 0 measurement, and incubated the remaining serum-starved cells in normal growth medium under ambient or pressure conditions for 24 hours before counting cells by a crystal violet absorbance assay over the linear assay range, with interpolation against a standard curve, as described (27).
Western blotting
Following pressure, Caco-2 cells were lysed in buffer with protease inhibitors, centrifuged at 10,000g for 15 minutes at 4°C, and resolved by SDS-PAGE as described (21). Membranes were blotted for phospho-ERK Thr 202, Tyr204 or total ERK, re-probed with antibodies specific for GAPDH and appropriate secondary antibody as a loading control, and detected by enhanced chemiluminescence as described (28).. All exposures used for densitometric analysis were within the linear range.
Data analysis
All data are expressed as mean±SE. Statistical analysis was performed using paired or unpaired t tests or analysis of variance as appropriate. A P value less than 0.05 was considered significant.
Results
Murine Roux limb formation affects pressure within small bowel lumen, as well as mucosal healing and proliferation
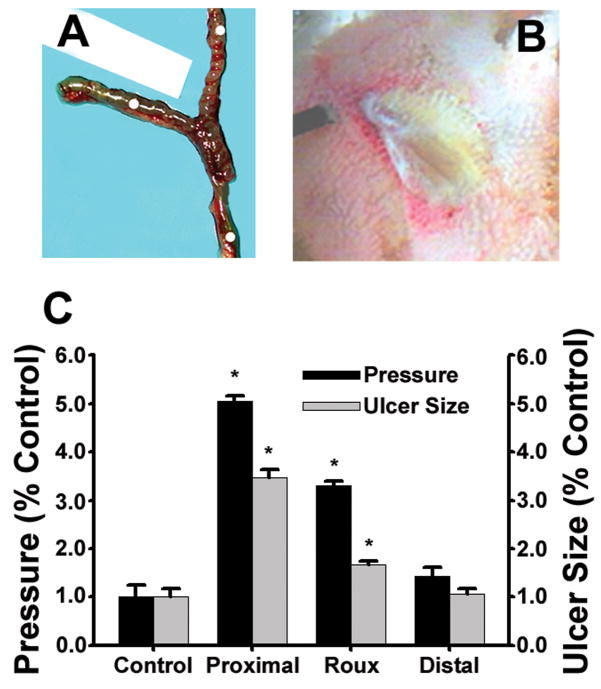
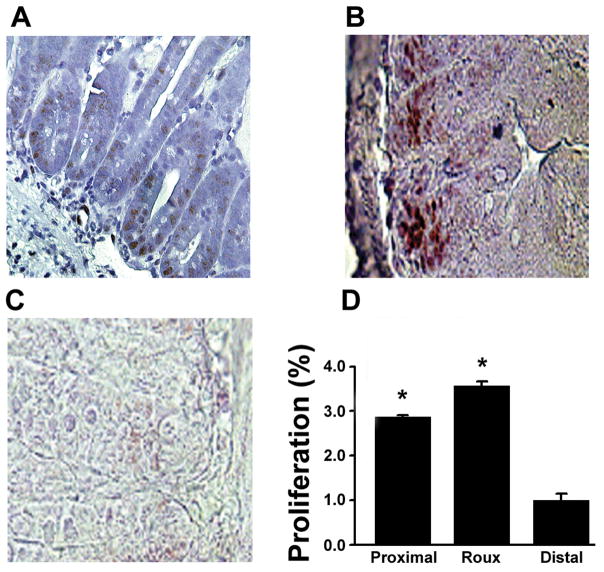
Creation of a defunctionalized roux limb in mice (Figure 1a) yielded probe-patent but partially obstructed small bowel. We induced ulcers on the roux, proximal and distal gut (Figure 1b). At 72 hours, the roux and proximal limb pressures were 3.3+/−0.1 and 5.0+/−0.1 fold normal respectively (n=10,p<0.0001). Ulcer size was measured after 72 hours, at necropsy. Ulcers in proximal and defunctionalized limbs were 224+/−14.9% and 55.7+/−7.8% larger than those in the distal limbs respectively (Figure 1c, n=15,p<0.0001 each). Proliferation was assessed using a PCNA stain for proliferating cells (Figure 2a). PCNA immunoreactivity within the mucosa of the proximal and defunctionalized limbs was 186+/−15.8% and 256 +/−9.9% greater than in the distal limb respectively (n=4,p<0.05 each, Figure 2b). We obtained similar results using Ki67 staining (not shown).
Figure 1.
The Roux limb ex-vivo is shown in (A) with the defunctionalized Roux limb to the left, the proximal limb at the top, and the distal limb at the bottom. (B) illustrates the gross appearance of an acetic acid induced jejunal mucosal ulcer after 3 days. At 3 days (C), the proximal limb exhibits the highest luminal pressure and the slowest ulcer healing (n=10 and 15 respectively, P<0.05 for each), compared to the distal limb. The Roux limb also exhibits higher pressure and slower healing (n=10 and 15 respectively, P<0.05 for each) than the distal limb.
Figure 2.
Mucosal PCNA staining. Typical images are shown of PCNA staining of the mucosa from the proximal limb (A), Roux limb (B), and distal limb (C). Areas of brown stain indicate proliferating cells. (D) The proliferative index is increased in Roux and proximal limb mucosa compared to the distal limb (n=4, p<0.001 for each).
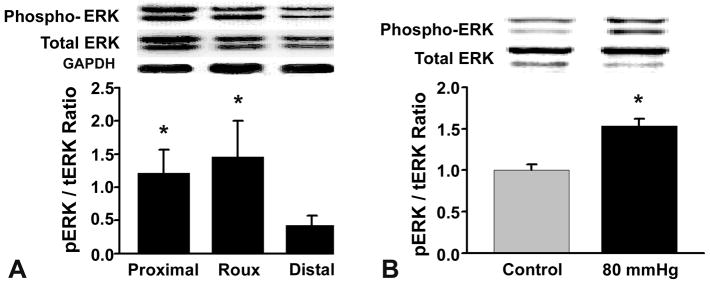
Pressure increases phosphorylated and total ERK in vivo
Phosphorylated ERK was increased in the proximal and Roux limbs compared to the distal limb (Figure 3, top blot, 171.0+/−37.5% and 140.6+/−39%, n=19, p<0.05). Total ERK was also increased in the Roux and proximal limbs compared to the distal limb (Figure 3, middle blot, 97.9+/−33.7% and 60.9+/−30.9%, n=19, p<0.05). To ensure that the increase in phosphorylated ERK was not an artifact of the increase in total ERK, we calculated the phosphorylated to total ERK ratio (Figure 3a). The ratio of activated to total ERK in the proximal and Roux limb was also increased in the proximal and defunctionalized limbs by 184.6+/−83.6% and 243.3+/−127.5% respectively compared to the distal limb (n=19, p<0.05).
Figure 3.
(A) Phosphorylated and total ERK are each increased significantly in the proximal and Roux limbs compared to the distal limbs of the anastomoses. The phospho ERK/total ERK ratio demonstrates a true increase in the proportion of activated ERK in both proximal and Roux limbs compared to the distal gut (n=19, p<0.05 for each comparison of phosphorylated and total ERK and for the ratio) (B) Phosphorylated ERK is increased in pressurized Caco-2 cells compared to controls. (n=18, p<0.05)
Pressure activates ERK in Caco-2 cells
ERK is activated in Caco-2 cells by repetitive strain (22). We asked whether pressure also activates ERK in vitro in parallel to ERK activation in the partially obstructed mucosa in vivo. When confluent Caco-2 cells on collagen substrates were subjected to 30 minutes of 80 mm Hg increased pressure on collagen, pressure increased ERK activation by 35.5+/−6.6% (Figure 3b, n=18, p<0.05).
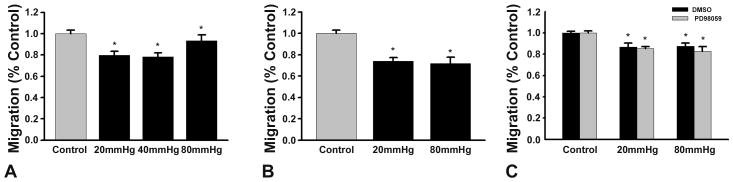
Pressure inhibits Caco-2 epithelial sheet migration
Basal migration was more rapid on collagen I than on fibronectin, consistent with previous findings (25). On collagen substrates, migration was reduced at 20–80 mmHg increased pressure (n=18, p<0.001 each). (Figure 4a ). Caco-2 motility was similarly inhibited by 20 and 80 mHg pressures across fibronectin (n=12, p<0.001 each) (Figure 4b). It was thought that Caco-2 migration may be influenced by ERK (21). However, blocking ERK with the MEK inhibitor PD98059 did not prevent the inhibition of migration by pressure at either 20 or 80 mm Hg (n=6 each, p<0.05 each) (Figure 4c). Additional studies conducted in parallel confirmed that pressure inhibits IEC-6 cell motility similarly to its effects on Caco-2 cells (not shown).
Figure 4.
(A) Wound closure on a collagen substrate is reduced when cells are exposed to 20–80 mmHg increased pressure vs. ambient pressure control (n=36 each, P<0.005 for each comparision). (B) 20 and 80 mm Hg pressures reduce migration across fibronectin vs. ambient pressure control (n=24 each, P<0.005 each). (C) Pressure decreases wound closure on a collagen substrate similarly after treatment with a DMSO vehicle control or after ERK blockade by the upstream MEK inhibitor PD 98059 vs. ambient pressure control (n=36 each, P<0.005 each).
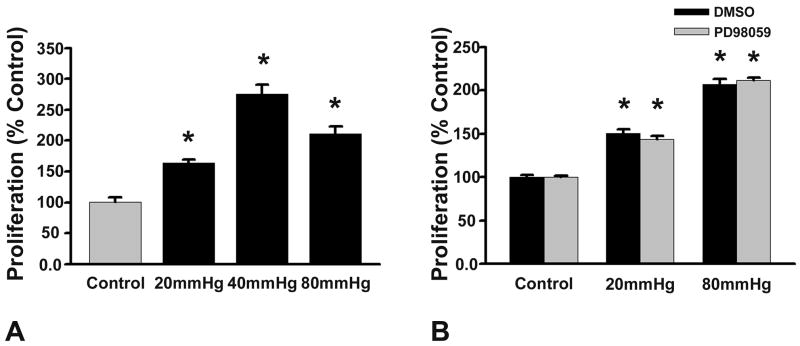
Pressure stimulates Caco-2 cell proliferation
Caco-2 cells exposed to pressure at 20–80 mm Hg, over 24 hours, exhibited increased cell numbers compared with control cells at ambient pressures. Blocking ERK with PD98059 did not prevent the mitogenic effect of increased pressure. (Fig. 5, n=32, p<0.05 for all)
Figure 5.
Proliferation is increased on collagen by a 20 or 80 mm Hg increase in pressure (black bars). This effect is not prevented by ERK blockade by PD98059 (grey bars) compared to ambient controls (n=22, p<0.05 for each)
Discussion
Peristalsis and the interactions of the luminal contents with the mucosa expose the small intestinal epithelium to a wide range of luminal pressures. Nocturnal luminal pressure manometry in healthy volunteers (29) demonstrated a mean average pressure of 15–20 mm Hg during phase II of the migrating motor complex (MMC). Luminal pressures fall to almost zero during phase I of the MMC, before phase II restarts. Thus, the gut mucosa normally experiences changes in luminal pressure ranging from 0–30 mm Hg over 85–110 minutes with average pressure of 15–21 mm Hg. We studied 0–80 mm Hg pressures to approximate the normal variance of the intra-luminal pressure and the high supra-physiologic pressures in pathologic states. Our results suggest that supraphysiologic pressure inhibits mucosal wound healing in vivo and in vitro independently of both extracellular matrix regulation and intracellular ERK activation. The effects on wound healing are likely to reflect true motility rather than effects on proliferation, because proliferation is actually stimulated by pressure, an effect that was also ERK-independent.
In vivo wound healing was significantly decreased in the defunctionalized and proximal bowel as compared to the distal gut. Ulcer healing was slowest in the proximal limb. The magnitude of inhibition of restitution correlated with luminal pressure. The presence or absence of luminal chyme and its own chemical and physical interactions with the mucosa is an additional variable in vivo. However, luminal chyme was present within the proximal limb while the roux limb was empty and had no significant intra-luminal contents at necropsy, being distended only by gas. Since both limbs generally exhibited the same tendencies to decreased wound healing, increased proliferation, and ERK activation, and since the in vitro model reproduced this effect simply by manipulating extracellular pressure, our results suggest that the effects of pathologic luminal pressure dominates any effect of the chyme itself. The murine ulcers were created simultaneously with the Roux-en-Y preparation. It is conceivable that the edema of the anastomosis contributed to the proximal and Roux obstruction. If the anastomosis had been allowed to heal for a period of weeks, it is possible that the obstruction would have cleared, intraluminal pressure would have normalized, and the epithelial migration and mucosal healing in the defunctionalized and proximal limbs would no longer have demonstrated a pressure effect. However, this awaits further study beyond the scope of the current manuscript.
The magnitude of wound closure in these studies appears modest, but is highly statistically significant. We (14, 30) and others (31–34) have described similar magnitude changes in intestinal epithelial migration, proliferation, or signaling due to other stimuli. For instance, strain induces an average 22% change in proliferation in Caco-2 cells plated on various matrices (14). However, the effects of physiologic repetitive strain on intestinal epithelial cells are matrix-dependent while those of pathologic pressures seem to escape regulation by the extracellular matrix just as they are independent of luminal chyme. Repetitive strain accelerates Caco-2 or IEC-6 monolayer wound closure but inhibits proliferation on fibronectin while deformation inhibits wound closure but stimulates proliferation on collagen (14, 21). In contrast, increased pressure inhibited wound closure in vitro on either collagen or fibronectin.
ERK stimulates proliferation and migration in the absence of physical forces (35, 36) and mediates the mitogenic effects of repetitive deformation in intestinal epithelial cells on collagen and the motogenic effects of repetitive deformation in intestinal epithelial cells on fibronectin (21, 22). It was therefore somewhat surprising that pressure activates ERK while inhibiting motility in vivo and that blocking ERK did not prevent inhibition of motility by pressure in vitro. However, not all physical force effects on intestinal epithelial cells involve ERK. Repetitive deformation inhibits intestinal epithelial cell motility across collagen substrates independently of ERK (21). Moreover, extracellular pressure stimulates colon cancer cell adhesion independently of ERK (12). We hypothesize that pressure may inhibit intestinal epithelial motility by an ERK-independent signal mechanism similar to that responsible for the inhibition of intestinal epithelial migration across collagen. The precise signals that mediate these effects await further study. Moreover, it seems likely that the activation of intestinal epithelial ERK by pressure in vivo and in vitro reflects some other yet to be identified ERK-mediated effect of pressure on the gut mucosa.
Intestinal mucosal healing is a complex process involving lamellipodial extension of epithelial cells, migration, and proliferation. Physical forces due to intestinal contraction as in peristalsis, villous motility, and interactions with luminal contents likely interact with the effects of cell-matrix interactions and soluble factor signaling to influence these processes. These effects are interesting because the intestinal lumen experiences greatly increased pressure during diverse pathologic states, including the exacerbation of inflammatory bowel disease, post-operative ileus, and partial or complete bowel obstruction (37–39). In some pathologic situations that increase pressure within the bowel, this pressure may itself have a deleterious effect that further worsens the patient’s condition. When the normal homeostasis of the small bowel is disturbed by disease, the normal physical forces of the gut are altered and the response to these forces also changes. In particular, increased pressures within the gut may impair mucosal healing in intestinal disease or injury.
Acknowledgments
Supported in part by a VA Merit Research Award (MDB), NIH RO1 DK067257 (MDB) and NIH 2 T32 GM008420 (MDB, CG, TF)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sarna SK, Otterson MF. Small intestinal physiology and pathophysiology. Gastroenterol Clin North Am. 1989;18(2):375–404. [PubMed] [Google Scholar]
- 2.Mailman D, Womack WA, Kvietys PR, Granger DN. Villous motility and unstirred water layers in canine intestine. Am J Physiol. 1990;258(2 Pt 1):G238–46. doi: 10.1152/ajpgi.1990.258.2.G238. [DOI] [PubMed] [Google Scholar]
- 3.Miftakhov R, Wingate D. Numerical simulation of the peristaltic reflex of the small bowel. Biorheology. 1994;31(4):309–25. doi: 10.3233/bir-1994-31402. [DOI] [PubMed] [Google Scholar]
- 4.McNeil PL, Ito S. Gastrointestinal cell plasma membrane wounding and resealing in vivo. Gastroenterology. 1989;96(5 Pt 1):1238–48. doi: 10.1016/s0016-5085(89)80010-1. [DOI] [PubMed] [Google Scholar]
- 5.Basson MD, Yu CF, Herden-Kirchoff O, et al. Effects of increased ambient pressure on colon cancer cell adhesion. J Cell Biochem. 2000;78(1):47–61. doi: 10.1002/(sici)1097-4644(20000701)78:1<47::aid-jcb5>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 6.Brodribb AJ, Condon RE, Cowles V, DeCosse JJ. Effect of dietary fiber on intraluminal pressure and myoelectrical activity of left colon in monkeys. Gastroenterology. 1979;77(1):70–4. [PubMed] [Google Scholar]
- 7.Kellow JE, Phillips SF. Altered small bowel motility in irritable bowel syndrome is correlated with symptoms. Gastroenterology. 1987;92(6):1885–93. doi: 10.1016/0016-5085(87)90620-2. [DOI] [PubMed] [Google Scholar]
- 8.Granger DN, Barrowman JA. Microcirculation of the alimentary tract I. Physiology of transcapillary fluid and solute exchange. Gastroenterology. 1983;84(4):846–68. [PubMed] [Google Scholar]
- 9.Allan A, Wyke J, Allan RN, et al. Plasma fibronectin in Crohn’s disease. Gut. 1989;30(5):627–33. doi: 10.1136/gut.30.5.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fallingborg J, Nielsen D, Pedersen JO. Decreased gelatin-binding fibronectin in patients with chronic inflammatory bowel diseases. Scand J Gastroenterol. 1985;20(9):1062–4. doi: 10.3109/00365528509088872. [DOI] [PubMed] [Google Scholar]
- 11.Verspaget HW, Biemond I, Allaart CF, et al. Assessment of plasma fibronectin in Crohn’s disease. Hepatogastroenterology. 1991;38(3):231–4. [PubMed] [Google Scholar]
- 12.Thamilselvan V, Basson MD. Pressure activates colon cancer cell adhesion by inside-out focal adhesion complex and actin cytoskeletal signaling. Gastroenterology. 2004;126(1):8–18. doi: 10.1053/j.gastro.2003.10.078. [DOI] [PubMed] [Google Scholar]
- 13.McNeil PL, Ito S. Molecular traffic through plasma membrane disruptions of cells in vivo. J Cell Sci. 1990;96 ( Pt 3):549–56. doi: 10.1242/jcs.96.3.549. [DOI] [PubMed] [Google Scholar]
- 14.Zhang J, Li W, Sanders MA, Sumpio BE, Panja A, Basson MD. Regulation of the intestinal epithelial response to cyclic strain by extracellular matrix proteins. FASEB J. 2003;17(8):926–8. doi: 10.1096/fj.02-0663fje. [DOI] [PubMed] [Google Scholar]
- 15.Basson MD, Coppola CP. Repetitive deformation and pressure activate small bowel and colonic mucosal tyrosine kinase activity in vivo. Metabolism. 2002;51(12):1525–7. doi: 10.1053/meta.2002.36303. [DOI] [PubMed] [Google Scholar]
- 16.Kirsner JB, Shorter RG. Recent developments in nonspecific inflammatory bowel disease (second of two parts) N Engl J Med. 1982;306(14):837–48. doi: 10.1056/NEJM198204083061404. [DOI] [PubMed] [Google Scholar]
- 17.Kirsner JB, Shorter RG. Recent developments in “nonspecific” inflammatory bowel disease (first of two parts) N Engl J Med. 1982;306(13):775–85. doi: 10.1056/NEJM198204013061304. [DOI] [PubMed] [Google Scholar]
- 18.Reddy SN, Bazzocchi G, Chan S, et al. Colonic motility and transit in health and ulcerative colitis. Gastroenterology. 1991;101(5):1289–97. doi: 10.1016/0016-5085(91)90079-z. [DOI] [PubMed] [Google Scholar]
- 19.Rabau M, Eyal A, Kluger Y, Dayan D. Bursting pressure in anastomotic healing in experimentally induced colitis in rats. Dis Colon Rectum. 1998;41(4):468–72. doi: 10.1007/BF02235761. [DOI] [PubMed] [Google Scholar]
- 20.Basson MD, Li GD, Hong F, Han O, Sumpio BE. Amplitude-dependent modulation of brush border enzymes and proliferation by cyclic strain in human intestinal Caco-2 monolayers. J Cell Physiol. 1996;168(2):476–88. doi: 10.1002/(SICI)1097-4652(199608)168:2<476::AID-JCP26>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 21.Zhang J, Owen CR, Sanders MA, Turner JR, Basson MD. The motogenic effects of cyclic mechanical strain on intestinal epithelial monolayer wound closure are matrix dependent. Gastroenterology. 2006;131(4):1179–89. doi: 10.1053/j.gastro.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Chaturvedi LS, Marsh HM, Shang X, Zheng Y, Basson MD. Repetitive deformation activates focal adhesion kinase and ERK mitogenic signals in human Caco-2 intestinal epithelial cells through Src and Rac1. J Biol Chem. 2007;282(1):14–28. doi: 10.1074/jbc.M605817200. [DOI] [PubMed] [Google Scholar]
- 23.Araki H, Komoike Y, Matsumoto M, Tanaka A, Takeuchi K. Healing of duodenal ulcers is not impaired by indomethacin or rofecoxib, the selective COX-2 inhibitor, in rats. Digestion. 2002;66(3):145–53. doi: 10.1159/000066759. [DOI] [PubMed] [Google Scholar]
- 24.Peterson MD, Mooseker MS. Characterization of the enterocyte-like brush border cytoskeleton of the C2BBe clones of the human intestinal cell line, Caco-2. J Cell Sci. 1992;102 ( Pt 3):581–600. doi: 10.1242/jcs.102.3.581. [DOI] [PubMed] [Google Scholar]
- 25.Basson MD, Modlin IM, Madri JA. Human enterocyte (Caco-2) migration is modulated in vitro by extracellular matrix composition and epidermal growth factor. J Clin Invest. 1992;90(1):15–23. doi: 10.1172/JCI115828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Providence KM, White LA, Tang J, Gonclaves J, Staiano-Coico L, Higgins PJ. Epithelial monolayer wounding stimulates binding of USF-1 to an E-box motif in the plasminogen activator inhibitor type 1 gene. J Cell Sci. 2002;115(Pt 19):3767–77. doi: 10.1242/jcs.00051. [DOI] [PubMed] [Google Scholar]
- 27.Chaturvedi LS, Marsh HM, Basson MD. Src and focal adhesion kinase mediate mechanical strain-induced proliferation and ERK1/2 phosphorylation in human H441 pulmonary epithelial cells. Am J Physiol Cell Physiol. 2007;292(5):C1701–13. doi: 10.1152/ajpcell.00529.2006. [DOI] [PubMed] [Google Scholar]
- 28.Craig DH, Zhang J, Basson MD. Cytoskeletal signaling by way of alpha-actinin-1 mediates ERK1/2 activation by repetitive deformation in human Caco2 intestinal epithelial cells. Am J Surg. 2007;194(5):618–22. doi: 10.1016/j.amjsurg.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scott SM, Knowles CH, Wang D, et al. The nocturnal jejunal migrating motor complex: defining normal ranges by study of 51 healthy adult volunteers and meta-analysis. Neurogastroenterol Motil. 2006;18(10):927–35. doi: 10.1111/j.1365-2982.2006.00824.x. [DOI] [PubMed] [Google Scholar]
- 30.Han O, Sumpio BE, Basson MD. Mechanical strain rapidly redistributes tyrosine phosphorylated proteins in human intestinal Caco-2 cells. Biochem Biophys Res Commun. 1998;250(3):668–73. doi: 10.1006/bbrc.1998.9372. [DOI] [PubMed] [Google Scholar]
- 31.Zhong J, Gencay MM, Bubendorf L, et al. ERK1/2 and p38 MAP kinase control MMP-2, MT1-MMP, and TIMP action and affect cell migration: a comparison between mesothelioma and mesothelial cells. J Cell Physiol. 2006;207(2):540–52. doi: 10.1002/jcp.20605. [DOI] [PubMed] [Google Scholar]
- 32.Von Offenberg Sweeney N, Cummins PM, Cotter EJ, et al. Cyclic strain-mediated regulation of vascular endothelial cell migration and tube formation. Biochem Biophys Res Commun. 2005;329(2):573–82. doi: 10.1016/j.bbrc.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 33.Kobayashi M, Nishita M, Mishima T, Ohashi K, Mizuno K. MAPKAPK-2-mediated LIM-kinase activation is critical for VEGF-induced actin remodeling and cell migration. Embo J. 2006;25(4):713–26. doi: 10.1038/sj.emboj.7600973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Antico G, Lingen MW, Sassano A, et al. Recombinant human uteroglobin/CC10 inhibits the adhesion and migration of primary human endothelial cells via specific and saturable binding to fibronectin. J Cell Physiol. 2006;207(2):553–61. doi: 10.1002/jcp.20604. [DOI] [PubMed] [Google Scholar]
- 35.Gu J, Chen L, Shatos MA, et al. Presence of EGF growth factor ligands and their effects on cultured rat conjunctival goblet cell proliferation. Exp Eye Res. 2008;86(2):322–34. doi: 10.1016/j.exer.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buffin-Meyer B, Crassous PA, Delage C, Denis C, Schaak S, Paris H. EGF receptor transactivation and PI3-kinase mediate stimulation of ERK by alpha(2A)-adrenoreceptor in intestinal epithelial cells: a role in wound healing. Eur J Pharmacol. 2007;574(2–3):85–93. doi: 10.1016/j.ejphar.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 37.Summers RW, Anuras S, Green J. Jejunal manometry patterns in health, partial intestinal obstruction, and pseudoobstruction. Gastroenterology. 1983;85(6):1290–300. [PubMed] [Google Scholar]
- 38.Dabareiner RM, White NA, Donaldson LL. Effects of intraluminal distention and decompression on microvascular permeability and hemodynamics of the equine jejunum. Am J Vet Res. 2001;62(2):225–36. doi: 10.2460/ajvr.2001.62.225. [DOI] [PubMed] [Google Scholar]
- 39.Camilleri M. Jejunal manometry in distal subacute mechanical obstruction: significance of prolonged simultaneous contractions. Gut. 1989;30(4):468–75. doi: 10.1136/gut.30.4.468. [DOI] [PMC free article] [PubMed] [Google Scholar]