Abstract
The case report presented herein aims at promoting the awareness in medical, notably cardiological, practice of the importance of, first, collecting at least a week-long record of around-the-clock measurements of blood pressure (BP) and heart rate (HR) (and a much longer record if the 7 day record so indicates) and, second, of analysing the data chronobiologically in the light of reference values specified as a function of time, gender and age as a minimum. In addition to diagnosing deviations in a chronome (time structure)-adjusted mean value, a chronobiological approach identifies abnormalities in the variability of BP and/or HR, gauged by the circadian characteristics (double amplitude and acrophase, measures of the extent and timing of predictable change within a cycle) and by the standard deviation. A woman in presumably good health was 60 years of age at the start of intermittent monitoring over a 7 year span. The case report illustrates the extent to which a decision based on single BP readings and even on 24 hour averages may be misleading. Treatment based on an initial week-long monitoring may benefit from continued long-term monitoring.
Keywords: Blood pressure monitoring lasting 7-year, Case report, Diagnosis of hypertension
INTRODUCTION
In addition to following the hygienic steps of exercise and diet, active surveillance for health care can include the monitoring of vital signs and other physiological variables for pre-habilitation (1, 2). Because BP abnormalities are often asymptomatic until there is target organ damage, and because BP is highly variable, from moment to moment, within a day, as well as from one day to another, single measurements can lead to over 40 % misdiagnoses (3–6). Moreover, abnormalities in BP and/or HR variability can be associated with a large increase in cardiovascular disease risk, larger than that of MESOR-hypertension (2, 6–8).
A chronobiological diagnosis is preferably based, as a start only, on 7-day/24 hour automatic monitoring, complemented by the parametric and non-parametric analysis of the data. Circadian rhythm characteristics are interpreted in the light of reference values consisting of 90% prediction limits derived from records of clinically healthy people of the same gender and a similar age. BP and/or HR excess and/or deficit are also assessed non-parametrically by comparing the BP/HR profile with time-specified prediction limits further qualified in terms of gender and age (6–8).
MATERIALS AND METHODS
At the start of monitoring, CH, a woman in presumably good health, was 60 years of age. She measured her BP and HR around the clock, mostly at 30-min intervals for 7 days or longer at intervals of weeks or months during an about 7-year span, using an ambulatory monitor (TM-2421) from the A&D Company (Tokyo, Japan). The reliability of this monitor had been previously demonstrated (9). The oscillometric readings were used for analysis.
CH kept a thorough diary during monitoring sessions, allowing the association of spans when her BP was found to be deviant with the presence of strong emotions such as grief, conflict, and concern (10, 11). Irrespective of the duration of a given monitoring session, analyses were carried out in repeated scans of the same data for separate subspans of about a day, about a week or longer spans, including an overall analysis of the complete record.
RESULTS
As described elsewhere (2, 10, 11), results from the first two profiles revealed the presence of MESOR-hypertension during the first 5 days of monitoring but not for the ensuing 16 days, and not during another 11-day span obtained a couple of months later. CHAT (brief for Circadian Hyper-Amplitude Tension, a condition characterized by an excessive circadian BP amplitude) was diagnosed at a time when there was trouble at work, grief, and conflict.
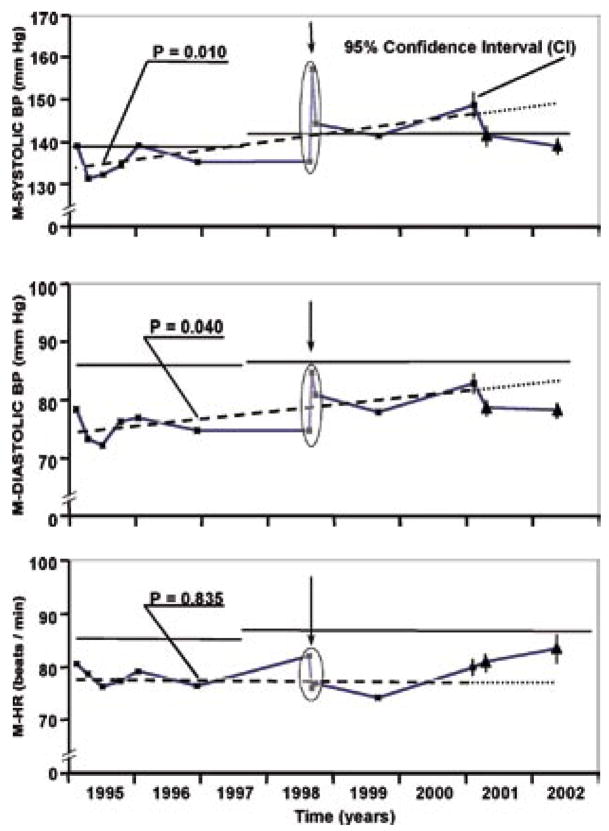
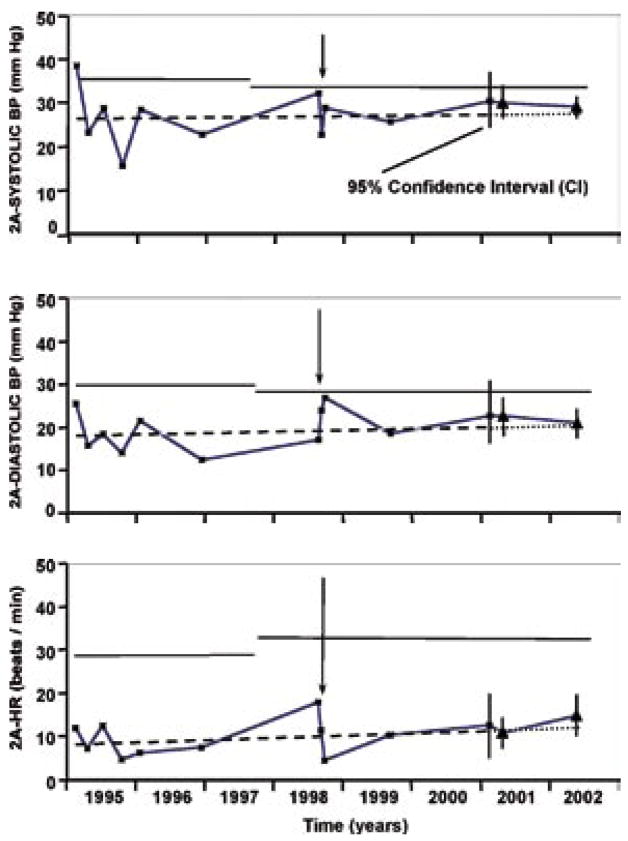
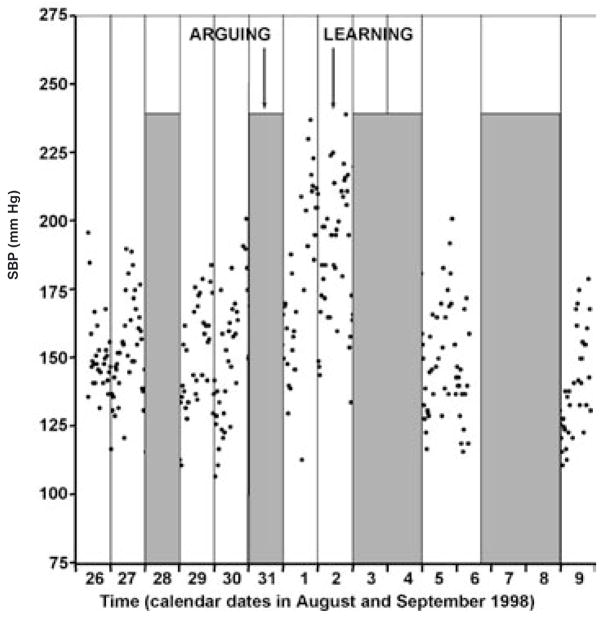
Several profiles were obtained over the next 6 years. The time course of the ME-SOR and circadian amplitude of BP and HR is shown in Figs. 1 and 2, respectively. The results indicate an increase in the MESOR of systolic BP over time, which may reflect no more than expected changes as a function of age. They also show an episode of greatly elevated BP values in 1998. The increase is found to be statistically significant by a cumulative sum (CUSUM) control chart (12, 13). The circadian amplitudes, by contrast, did not change to the same extent. The sharp elevation in BP in 1998 is shown in further detail in Fig. 3. This elevation coincides with a traumatic event in CH’s life, when she learned about her daughter’s diagnosis of ovarian cancer and consequently about some uncertainties about it.
Fig. 1.
*60 years of age at start. Each dot represents a profile of measurements of blood pressure (BP) and heart rate (HR) at 30-minute intervals for least a week (N = 340 to 855/profile [□ or △], total N = 7985). Arrow: learning about health problem. Linear trend (- - - -) over first 6 years (computed without outliers in oval) is statistically significant for systolic (P = 0.010) and diastolic (P = 0.040) BP. Observations during following 1.5 years (△) have 95% CI not overlapping trend predicted (....) from first years’ results (—). Horizontal lines: upper 95% prediction limits adjusted for gender and age.
Fig. 2.
*CHAT ( Circadian Hyper-Amplitude-Tension. Eight-year course of circadian double amplitude (2A) * of blood pressure (BP) and heart rate (HR). CH, 60 years of age at start. Each dot represents a profile of measurements of blood pressure (BP) and heart rate (HR) at 30-minute intervals forat least a week (N = 340 to 855/profile [□ or △], total N = 7985). Arrow: learning about health problem. Linear trend (- - - -) over first 6 years (computed without outliers in ovla) is statistically significant. Excerpt for first dot there is no further “profile-CHAT”, despote frequent but not lasting “~24-h-CHAT”, shown elsewhere. The findings of frequent “~24-h-CHAT” but of “profile-CHAT” only once (at start), suggest that at lest week long monitoring should by repeated, when it reveals abnormality. Observations during last 1.5 years (△) have 95% CI not overlapping trend predicted (___) from first 6 years’ results (—). Horizontal lines: upper 95% prediction limit adjusted for gender and age.
Fig. 3.
*CH, 64 years of age. Vertical lines on the plot divide spans for which circadian rhythm was tested. Shaded areas show the spans for which tero-amplitude test of circadian rhythm is not statistically significant, while in spans shown elsewhere, the,, non circadian rhythm” assumption could be nearly invariably rejected. N of measurements 34 to 48/day (total: 258).
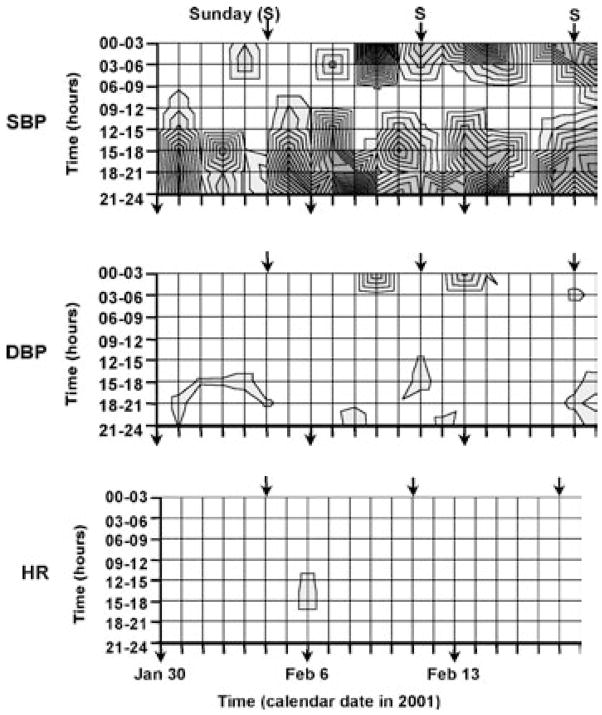
The contour map of Fig. 4 shows that the BP excess of CH tends to occur either during the night or in the afternoon. The span from awakening to noon is relatively free of any excess. This is the time, however, considered for everybody by current “chronotherapy” (14), carried out without marker rhythmometry, aiming at reducing the morning rise in BP by peak drug concentration at that time, a time when CH does not need treatment, if any, another illustration of the need for individualizing the timing of treatment administration.
Fig. 4.
* CH, F, 66 years of age, monitored at 30 minute intervals for 21 consecutive days; S = systolic; D = diastolic; excess: numerically integrated area between the data when they exceed the upper 95% prediction limit and this limit itself, expressed in mm Hg (BP) or beats/min (HR) x hours during 3 hours. The darker the shading the more excess; note least BP excess between 06:00 and 12:00 in CH, i.e., little or no shading during the time span at which generalized “chronotherapy” is aimed, ignoring the individual’s pattern.
DISCUSSION AND CONCLUSION
Other influences may have affected CH’s BP, including a circannual variation found on a population basis with relatively higher values in the winter than in the summer (15). A circaseptan variation in BP, with usually higher values around midweek than during weekends (16), should also be considered.
Whereas there is a tendency for the MESOR of systolic BP of CH to be elevated toward the end of the record, it may still be necessary to obtain additional data on CH before making the final recommendation about the use of anti-hypertensive medication. Exercise, dietary measures, and relaxation techniques may be a preferred initial approach. In some cases such as CH, there is no alternative but continued monitoring, even if it is implemented at intervals, as done during the about 7-year span examined herein. A rigorous study comparing “flying blind” (7) in current practice with monitoring what treatment does with short-term (e.g., assessment of the left ventricular mass index) and long-term (e.g., morbidity and/or mortality incidence) outcomes is overdue.
Acknowledgments
US Public Health Service (GM-13981; FH), Dr hc hc Earl Bakken Fund (FH, GC), University of Minnesota Supercomputing Institute (FH, GC), MSM 0021622402 Ministry of Education, CZ.
References
- 1.Cornélissen G, Halberg F, Schwartzkopff O, et al. Chronomes, time structures, for chronobioengi-neering for “a full life”. Biomed Instrumentation Technology. 1999;33:152–187. [PubMed] [Google Scholar]
- 2.Halberg F, Cornélissen G, Otsuka K, et al. Chronomics detects altered vascular variabilities constituting risks greater than hypertension: with an illustrative case report. In: Mitro P, Pella D, Ry-bar R, Valocik G, editors. Proceedings, 2nd Congress on Cardiovascular Diseases; Kosice, Slovakia. 25 27 April 2002; Bologna: Monduzzi Editore; 2002. pp. 223–258. [Google Scholar]
- 3.Management Committee, Australian National Blood Pressure Study: The Australian therapeutic trial in mild hypertension. Lancet. 1980 June 14;i(8181):1261–1267. [Google Scholar]
- 4.Kumagai Y, Kuwajima I, Suzuki Y, et al. Untenable acceptance of casual systolic/diastolic blood pressure readings below 140/90 mm Hg. Chronobiologia. 1993;20:255–260. [PubMed] [Google Scholar]
- 5.Cornélissen G, Halberg F. Impeachment of casual blood pressure measurements and the fixed limits for their interpretation and chronobiological recommendations. Ann NY Acad Sci. 1996;783:24–46. doi: 10.1111/j.1749-6632.1996.tb26705.x. [DOI] [PubMed] [Google Scholar]
- 6.Cornélissen G, Halberg F, Bakken EE, et al. 100 or 30 years after Janeway or Bartter, Healthwatch helps avoid “flying blind”. Biomedicine Pharmacotherapy. 2004;58(Suppl 1):S69–S86. doi: 10.1016/s0753-3322(04)80012-x. [DOI] [PubMed] [Google Scholar]
- 7.Halberg F, Cornélissen G, Halberg J, et al. Circadian hyper-amplitude-tension, CHAT: a disease risk syndrome of anti-aging medicine. J Anti-Aging Med. 1998;1:239–259. (see also editorial by M Fossel on p 239) [Google Scholar]
- 8.Cornélissen G, Schwartzkopff O, Halberg F, Otsuka K, Watanabe Y. 7 day ambulatory monitoring for adults with hypertension and diabetes. Am J Kidney Diseases. 2001;37:878. doi: 10.1016/s0272-6386(01)80145-1. [DOI] [PubMed] [Google Scholar]
- 9.Imai Y, Sasaki S, Minami N, et al. The accuracy and performance of the A&D TM-2421, a new ambulatory blood pressure monitoring device based on the cuff-oscillometric method and the Korotkoff sound technique. Am J Hypertens. 1992;5:719–726. doi: 10.1093/ajh/5.10.719. [DOI] [PubMed] [Google Scholar]
- 10.Halberg F, Cornélissen G, Halpin C, et al. Fleeting “monitor-”, “conflict-” or “grief-associated” blood pressure disorders: MESOR-hypertension and circadian hyperamplitude tension (CHAT) Eu-roRehab. 1996;6:225–240. [Google Scholar]
- 11.Halberg F, Cornélissen G. International Womb-to-Tomb Chronome Initiative Group: Resolution from a meeting of the International Society for Research on Civilization Diseases and the Environment (New SIRMCE Confederation) Brussels, Belgium: March 17 18, 1995. Fairy tale or reality ? Medtronic Chronobiology Seminar #8, April 1995, 12 pp. text, 18 figures. http://www.msi.umn.edu/~halberg. [Google Scholar]
- 12.Hawkins DM. Self-starting CUSUM charts for location and scale. Statistician. 1987;36:299–315. [Google Scholar]
- 13.Cornélissen G, Halberg F, Hawkins D, Otsuka K, Henke W. Individual assessment of antihyperten-sive response by self-starting cumulative sums. J Med Engineering Technology. 1997;21:111–120. doi: 10.3109/03091909709031156. [DOI] [PubMed] [Google Scholar]
- 14.American Medical Association. A patient guide to chronotherapy. 1997. Chicago: American Medical Association; 1996. Taking your medication: a question of timing; p. 16. [Google Scholar]
- 15.Halberg F, Cornélissen G, Haus E, et al. Clinical relevance of about-yearly changes in blood pressure and the environment. Int J Biometeorol. 1996;39:161–175. doi: 10.1007/BF01221387. [DOI] [PubMed] [Google Scholar]
- 16.Siegelova J, Cornélissen G, Fiser B, et al. Blood pressure and heart rate monitoring in humans: the circaseptan and circadian rhythms. Abstract, 3rd International Workshop on The Human Circulation: Noninvasive Haemodynamic, Autonomic and Vascular Monitoring, Graz, Austria, 9 11 May 2003. Clin Autonom Res. 2003;13:60–61. [Google Scholar]