Abstract
The association between the epsilon-4 type allele of apolipoprotein E (APOE ε4) and depression was investigated in 323 AD patients. Patients were divided into two groups based on the presence (n=61) or absence (n=262) of depression as assessed by the DSM-based Diagnostic Interview Schedule. Both subgroups were demographically comparable with regard to age, education, gender, and severity of cognitive impairment. Analysis of the frequency of APOE ε4 alleles between the groups revealed a significantly higher prevalence rate of the APOE ε4 genotype in the depressed group (72% of depressed AD patients carried at least one copy of the ε4 allele) compared to the non-depressed AD patients (58%). This effect was primarily accounted for by women. Specifically, an interaction was revealed wherein women who possessed the APOE ε4 allele were almost 4 times more likely to be depressed in comparison to those who did not carry the allele, and APOE ε4 status did not predict depression among men in our sample. These results are consistent with recent suggestions that the APOE ε4 genotype may be over-represented among women with AD and depression and highlight a need for additional research investigating the links between APOE genotype, mood, and gender.
Alzheimer’s disease (AD) is a devastating neurodegenerative disorder characterized by progressive neuropsychological, functional, and behavioral decline. Currently, there are 4.5 million people with AD in the United States and the prevalence is expected to increase to 11 – 16 million by 2050 (Alzheimer’s Association, 2004). Psychiatric disturbance is frequently seen in AD and, although prevalence rates vary considerably across studies (e.g., 1 – 90%), average rates of coexisting AD and depression appear to hover around 20 to 40% (Wragg & Jeste, 1989; Cummings, Ross, Absher, Gornbein & Hadjiaghai, 1995; Tractenberg, Weiner, Patterson, Teri, & Thal, 2003; Green et al., 2003). Lyketsos and Olin (2002) reported that behavioral disturbances among AD patients are 3 to 4 times higher than that seen in normal aging.
Adverse consequences of depression in patients with AD are numerous, including greater impairment in activities of daily living (Lyketsos et al., 1997b), poorer quality of life (Gonzales-Salvador et al., 2000), earlier institutionalization (Magni, Bionetti, Bianchetti, & Trabucchi, 1996), greater caregiver depression and level of burden (Gonzales-Salvador et al., 1999), more rapid declines in cognition (Stern et al., 1997), and higher mortality rates (Ganguli, Hodge, & Mulsant, 2002; Hoch et al., 1993). In addition, neuropsychiatric symptoms significantly increase direct annual costs of care among AD patients, even after adjusting for the severity of cognitive impairment and other medical comorbidities (Murman et al, 2002).
Neuropathologically, depressive symptoms appear to be associated with a selective loss of noradrenergic and serotonergic nuclei in the brainstem (Zubenko, 2000) and these losses may be related to genetic risk factors for AD (Craig, Hart, McIlroy, & Passmore, 2005). Although it is now clear that the ε4 allele of the apolipoprotein E gene (APOE-ε4), a plasma protein involved in the transport of cholesterol and lipids throughout the body, is an important risk factor for AD (Saunders et al., 1993; Corder et al., 1993; Farrer et al.,1997; Aggarwal et al., 2005), inconsistencies exist across studies investigating whether this susceptibility gene modifies the risk for depression in AD. Early studies examining this relationship showed a positive association between depression and the APOE ε4 allele in patients with AD (Murphy, Taylor, Tinklenberg, & Yesavage, 1997; Ramachandran et al., 1996), and other investigators have demonstrated combined risks of developing AD among those with late-onset depression and APOE ε4 genotypes in nondemented geriatric populations (Krishnan et al., 1996; Steffens et al., 1997; Wilson et al., 2002; Rigaud et al., 2001). A recent study suggested that depression and APOE ε4 genotype may be higher in women with AD but not in men (Muller-Thomsen et al., 2002). Despite these findings supporting an association between APOE and depression, several other published studies have not supported the notion that APOE ε4 genotype influences depression in AD (Liu et al., 2002; Scarmeas, et al., 2002; Craig et al., 2005).
Discrepant findings may be due to a number of factors including small sample sizes, differences in sample compositions (e.g., general “dementia” groups versus strictly diagnosed patients with “probable AD”), and the use of very brief, wide-ranging, or unstructured psychopathology inventories. In addition, others have shown trends toward association between APOE genotype and depression but have rendered conclusions of no relationship. For example, Forsell et al. (1997) found that “the odds for depression tended to be elevated in those who carried an ε4 allele (vs. ε3/ε3 allele)” though this did not reach statistical significance. The authors concluded there was no association and did not report any accompanying power or effect size estimates. Moreover, they reported a somewhat low prevalence rate (11%) for depression in their AD sample, causing some speculation about the representativeness of their sample or the diagnostic methodology used to assess depression. Other studies have also used varying schemes for diagnosing depression in AD. For example, Scarmeas et al. (2002) employed a psychiatric inventory that measured only three depression-related symptoms (i.e., depressed mood, change in appetite and sleep problems), two of which are vegetative symptoms and thus problematic for use in older adult samples that frequently have somatic symptoms secondary to physical comorbidity. Similarly, Levy et al. (1999) and Craig et al. (2005) utilized the Neuropsychiatric Inventory (NPI) which contains few items pertaining to depressive symptoms. Thus, the bulk of published studies reporting a lack of association between APOE ε4 genotype and depression in AD have suffered from small sample sizes, low reported prevalence rates for depression, very brief inventories of depressive symptoms, and/or low diagnostic rigor in the determination of the presence or absence of a DSM-based diagnosis of depression.
Given that negative findings in the literature may relate to measurement issues (i.e., insensitive instruments), the current study was designed to address these limitations by employing the Diagnostic Interview Schedule (DIS), a standardized DSM-based interview for depression (i.e., Diagnostic Interview Schedule for the DSM-III-R) in a large sample of AD patients. Thus, the present study examined a sample of well-characterized probable AD patients to investigate whether an association between APOE genotype and depression exists. Although there is considerable debate regarding the relationship between APOE genotype and depression in AD, we hypothesized that the APOE ε4 allele would significantly predict depression in our sample of rigorously diagnosed AD patients. This relationship was posited given previous findings as well as the observation that the APOE ε4 allele is associated with an increased density of neurotoxic beta-amyloid plaques in brain regions thought to be important in emotion regulation (i.e., limbic structures) (Roses, 1994; Shearman, 1998). Furthermore, a secondary aim of this study was to assess possible gender differences within the sample given recent suggestions that depression may be more prevalent in women with the APOE ε4 genotype (i.e., Muller-Thomsen et al., 2002).
Methods
Participants and Procedure
Data from 323 consecutive patients diagnosed with probable AD were retrospectively drawn from a larger cohort participating at the University of California, San Diego Alzheimer’s Disease Research Center (ADRC). All the participants were selected without regard to ethnicity or race. A written informed consent was obtained from all participants (or their caregivers) after full explanation of the study protocol which had been approved by the UCSD Human Research Protection Program.
All participants were independently diagnosed with probable AD by two staff neurologists according to the NINCDS-ADRDA criteria (McKhann et al., 1984) and received (a) annual neurological, medical, and psychiatric examinations; (b) global cognitive screening (i.e., Mattis Dementia Rating Scale; DRS; Mattis, 1988; and the Mini-Mental Status Examination; MMSE; Folstein, Folstein, & McHugh, 1975); (c) a neuropsychological battery of tests that assess basic cognitive domains such as attention, memory, language, visuospatial skill, problem solving and abstraction, and motor coordination. Included in this battery were verbal memory tests consisting of the Wechsler Memory Scale-Revised, Logical Memory subtest (WMS-R; Wechsler, 1987) and the California Verbal Learning Test (CVLT; Delis, Kramer, Kaplan, & Ober, 1987). See Salmon and Butters (1992) for a detailed description of all tests that comprise this battery.
Individuals were excluded from this study if an alternate cause of dementia was determined (i.e., hypothyroidism, vitamin B12 deficiency, electrolyte imbalance), or if they had a history of severe head injury, recent alcohol dependence or abuse, or serious psychiatric disturbance (i.e., schizophrenia). Finally, to ensure that no participants in the study had a dementia with a significant vascular component, participants with modified Hachinski Ischaemia scores (Hachinski et al., 1975) greater than four were excluded.
Concurrent with the dementia diagnosis, all participants were evaluated for psychopathology according to the DIS, which was administered by trained nurse practitioners, and the diagnosis of depression or other psychiatric disorders was made by two board-certified psychiatrists. For this analysis, patients were divided into two groups on the basis of the presence (n = 61) or absence (n = 262) of a current diagnosis of co-occurring depression. Specific categories of affective diagnoses included Dementia with Depression (n = 39), Adjustment Disorder with Depressed Mood (n = 11), Major Depressive Disorder (n = 8), Dysthymic Disorder (n = 2), and Atypical Depression (n = 2).
Participants were genotyped for APOE using a method based on polymerase chain reaction identical to that of Saunders et al. (1993), and were divided into two groups on the basis of the presence (n = 196) or absence (n = 127) of the APOE-ε4 allele (overall percentage = 61%). This allelic frequency is highly consistent with prior published percentages (e.g., Corder et al., 1993; Saunders et al., 1993).
Statistical Analyses
Univariate level associations between different demographic and clinical variables and depression status were made with t-tests, Chi-Square tests, or Fisher’s Exact test, as appropriate. Logistic regression was used to determine the relationship of APOE ε4 status to depression, while controlling for confounders. Variables significantly related at the p<0.10 level to depression status at the univariate level were selected for inclusion into the multivariate model. An interaction term for gender and APOE ε4 status was selected for inclusion in the model, a priori, to address differences in the APOE ε4 relationship to depression by gender, and any confounders significantly related at the p<0.10 level to gender were selected for inclusion in the model. All analyses were run in SPSS (Version 13.0) and confirmed with STATA (version 8.2; College Station, TX).
Results
The sample included a total of 323 participants who were diagnosed with probable AD. Overall, there were 163 men and 160 women, with a mean age of 73 (SD = 9), and a mean education of 13 years (SD = 4). The proportion of patients diagnosed with a depressive disorder was approximately 19 percent and, as shown in Table 1, there were no statistical differences between the depressed and non-depressed AD groups with respect to demographic variables (i.e., age, education, and gender), cognitive status (i.e., DRS total score, MMSE, and verbal memory on the CVLT), or disease duration. For subjects with verbal memory scores, there was no difference between depressed and non-depressed patients on the delayed portion of the Logical Memory subtest of the WMS-R (LM-II) (mean raw score: 2.7 [SD 5.6] vs. 2.1 [SD 3.3]; p = 0.44) or the CVLT (Long Delay Free Recall; LD FR) (mean raw score: 1.2 [SD 1.9] vs. 1.0 [SD 1.8]; p = 0.63). However, results are not generalizable to the entire sample as a large portion of all participants were missing these scores (n = 171 and n = 127, respectively); MMSE values were significantly lower in those subjects who were missing these measures than in those who had them due to the discontinuation rules for administration of these memory tests in severe AD: mean MMSE for those with WMS-R LM II raw = 22.8 (SD 3.6) vs. 16.7 (SD 5.8) for those without, p < 0.001; and mean MMSE for those with CVLT LD FR raw 22.6 (SD 5.9) vs. 17.1 (SD = 17.1) for those without, p < 0.001. When the demographic measures were also compared by gender, only education differed, with women averaging nearly two years less education than men. There was no difference in APOE ε4 status by gender.
Table 1.
Demographic, Cognitive, and Apolipoprotein-E (APOE) ε4 Comparisons by Depression Status and Gender
| AD Groups by Depression Status | AD Groups by Gender | |||||
|---|---|---|---|---|---|---|
| Clinically Depressed(N=61) | Not Depressed (N=262) | p-value* | Women (N=160) | Men (N=163) | p-value | |
| Demographics | ||||||
| Age, mean (SD) | 72.1 (7.0) | 72.7 (9.7) | 0.657 | 72.9 (10.8) | 72.3 (7.5) | 0.586 |
| Female, % | 54.1 | 48.5 | 0.429 | - | - | - |
| Education, mean (SD) | 12.8 (4.1) | 13.2 (4.1) | 0.445 | 12.2 (3.8) | 14.0 (4.2) | <0.001 |
| Clinical Features | ||||||
| Depressed, % | - | - | 20.6 | 17.2 | 0.429 | |
| Years of AD, mean (SD) | 4.3 (2.5) | 3.7 (2.4) | 0.087 | 3.7 (2.3) | 4.0 (2.6) | 0.198 |
| DRS, mean (SD) | 102.1 (25.7) | 103.0 (21.1) | 0.765 | 102.5 (22.0) | 103.2 (22.2) | 0.783 |
| MMSE, mean (SD) | 20.9 (5.7) | 20.3 (5.4) | 0.484 | 20.0 (5.4) | 20.8 (5.6) | 0.185 |
| APOE Status | ||||||
| APOE ε4 Positive, % | 77.0 | 58.0 | 0.042 | 64.4 | 57.1 | 0.178 |
As depicted in Table 1, the frequency of the ε4 allele in depressed patients was approximately 77% (47/61) versus 58% (152/262) in the non-depressed patients. This finding indicates that the depressed AD patients were significantly more likely to possess an APOE ε4 allele than were those without depression (chi-square [df=1, N=323] = 4.13, p = .04). When stratified by gender, the relationship between APOE genotype and depression was significant: of the 33 women who were depressed, 28 were APOE ε4 positive (85%) versus only 75 of the 127 women who were not depressed (59%) [Fisher’s exact chi-square (df=1, N=160) = 7.60, p = .007]. Among men, there was no relationship between APOE ε4 status and depression, with 16 of the 28 men with depression (57%) and 77 of the 135 men without depression (57%) being APOE ε4 positive [Fisher’s exact chi-square (df=1, N=163) = 0.01, p = .99].
The relationship of APOE ε4 status on depression was further investigated using multivariate regression analyses (Table 2). When controlled for education and years of AD duration (see Methods), there is a significant interaction between APOE ε4 status and gender on depression: women who were APOE ε4 positive had increased odds of being depressed of 1.75 compared to APOE ε4 positive men, and women who are APOE ε4 negative had decreased odds of 0.46 over APOE ε4 negative men. This relates to a 3.83-fold increased risk of depression by APOE status among women. APOE ε4 status did not appear to increase the odds of depression among men (OR 1.00).
Table 2.
Multivariate Regression: Depressed versus Non-Depressed by Apolipoprotein-E (APOE) ε4 Status
| OR (95% CI) | Coefficent* | p-value | |
|---|---|---|---|
| APOE ε4 Positive | 1.00 (0.44, 2.31) | 0.004 | 0.992 |
| Female Gender | 0.46 (0.15, 1.42) | −0.787 | 0.176 |
| APOE ε4 Positive x Female Gender | 3.83 (1.02, 14.4) | 1.342 | 0.047 |
| Years of AD Duration | 1.10 (1.0, 1.3) | 0.095 | 0.088 |
| Education (years) | 0.95 (0.87, 1.03) | −0.054 | 0.185 |
Coefficient estimate for linear model, not yet converted to odds ratios. For example, the odds of depression for a female subject who is APOE ε4 positive is exp (0.004− 0.787+1.342)=1.75. Coefficient for model intercept = −1.204.
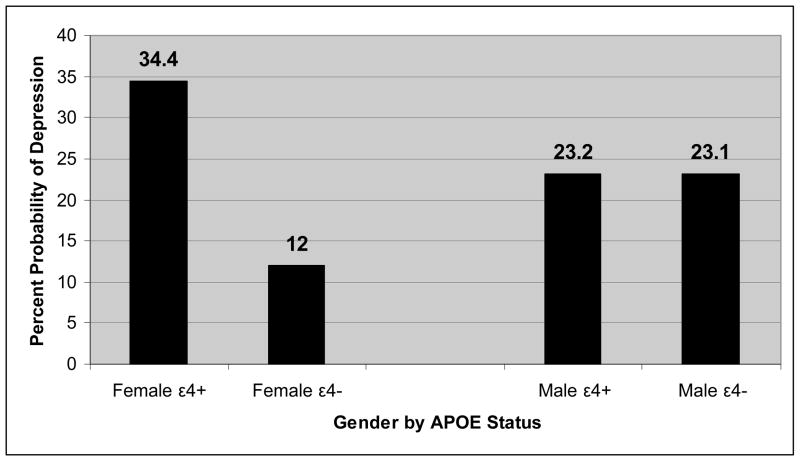
Overall, results indicate that the interaction of APOE genotype and gender significantly impacted whether individuals were classified as depressed or not depressed. Figure 1 depicts the APOE by gender interaction in terms of the predicted probability of depression. Results show that the APOE ε4 allele seems to impact the probability of being depressed for women but not for men and that women with AD who are positive for the APOE ε4 allele have nearly a four-fold increase in risk for depression compared to everyone else as a group.
Figure 1.
Plot of Apolipoprotein-E (APOE) status X Gender interaction on probability of depression for AD sample
*Controlled for Education and Years of AD Duration
Discussion
Consistent with some of the previous studies demonstrating a relationship between APOE genotype and depression in AD (Murphy et al., 1997; Ramachandran et al., 1996; Muller-Thomsen et al., 2002), we found that depressed AD patients had a significantly higher frequency of APOE ε4 genotype than non-depressed AD patients. This relationship was evident despite the groups’ comparability on demographic characteristics and cognitive status. Although the depressed AD group demonstrated a slightly longer duration of dementia (approximately 8 months longer), the difference was not statistically significant. Moreover, when duration of illness was statistically controlled for in the group analysis, the higher frequency of the APOE ε4 allele in the depressed group remained. Thus, it did not appear that the increased likelihood of depression in AD patients with a copy of the APOE ε4 allele was due specifically to disease severity or duration.
Our findings stand in contrast to a number of other studies that demonstrated a lack of association between depression and APOE genotype in AD. One possible explanation for our positive finding and its absence in prior studies may be that we obtained a relatively large sample of depressed AD patients and thus had a greater power to detect group differences. Several recent studies (i.e., Forsell et al., 1997; Liu et al., 2002; Gabryelewicz et al., 2002) included between 21 and 39 depressed individuals, whereas the current study included approximately twice those sample sizes (i.e., 61 depressed AD patients) and many more non-depressed patients. Another factor may be that the use of limited screening measures for determining depression could be leading to poorer diagnostic accuracies and thus different prevalence rates of depression in AD. In contrast to the current study in which 19% of the sample was diagnosed as depressed, Forsell et al. (1997) reported depression rates of 11% and Levy et al. (1999) reported more than double the prevalence we observed (40–50% prevalence of depression in their group of AD patients). These highly variable findings may represent significant heterogeneity within depressed groups. For example, Liu et al. (2002) included a large proportion of patients with Dysthymic Disorder in their sample (52%) whereas our study contained only 3% with Dysthymia. It appears that greater specification of diagnostic categories is clearly needed to inspect for important subgroup differences.
In contrast to standardized psychiatric interviews such as the DIS used in the current study, studies employing the use of very brief inventories for depression or multi-symptom profile inventories add further variability and likely diminish diagnostic accuracy. Determining whether individuals are depressed on the basis of a brief screening measure limited to but a few questions may reduce reliability and diagnostic accuracy rates.
To date, existing studies investigating associations between APOE ε4 genotype and depression in older adults with AD remain mixed and thus the relationship is not well understood. However, recent evidence has been accumulating to suggest that APOE, a low density protein, may be linked to vascular risk factors in late life and, in turn, may be associated with depression (Lavretsky et al., 2000). Indeed, apolipoprotein E is known to play a role in lipid metabolism, cholesterol transport, and neuronal repair (Zubenko et al., 1996), and it has been posited that the ε4 allele may be a predisposing genetic marker for ischemic cerebrovascular disease (Hoffman, Ott, & Breteler et al., 1997; McCarron, Delong, & Alberts, 1999) given its association with hyperlipidemia (Sawada et al., 2000), atherosclerosis (Davignon, Cohn, Mabile, & Bernier, 1999), myocardial infarction (Brscic, 2000), and subcortical white matter lesion pathology (de Leeuw et al., 2004). Moreover, vascular risk factors have been closely linked with depression in late-life and it has been suggested that they may predispose or give rise to depressive symptoms (“vascular depression hypothesis;” Alexopoulos et al., 1997). Furthermore, the APOE ε4 allele appears to be less efficient than other isoforms at inducing cholesterol transport (Michikawa et al., 2000), which may have an important role in maintaining the integrity of membranes, and in synaptic plasticity. Thus, it appears that the APOE ε4 allele is associated with impaired response to cerebral damage and diminished capacity for neuronal repair (Arendt et al., 1997; Crawford et al., 2002), and that this poorer neuronal reparative capacity may be implicated in the development of cognitive decline and depression in older adults with the APOE ε4 genotype. Finally, it has been proposed that, for those carrying a copy of the allele, the destructive effect of subtle, underlying vascular risk factors may be enhanced (de Leeuw et al., 2004). Our findings were limited to those AD patients without significant cerebrovascular disease risk. However, future studies should examine a broader range of patients to determine the relative contributions of cerebrovascular disease risk to depression in AD.
Our results also demonstrated that the association between APOE genotype and depression in AD was primarily seen in women and not men. These findings are consistent with those of Müller-Thomsen (2002) who indicated that the APOE ε4 genotype may be more highly associated with depression in AD for women but not men. Our finding is also supported by a study showing an increased rate of the APOE ε4 genotype in late-onset depressed women with AD relative to men (Steffens et al., 1997) as well as a finding that family history of depression may be a risk factor for depression in AD, but only in women (Lyketsos, Tune, Pearlson, Steele, 1996). Recent research has shown that women demonstrate higher rates of vascular risk factors (i.e., hyperlipidemia) compared to men (Hippisley-Coz, Pringle, Crown, Meal, & Wynn, 2001; de Leeuw et al., 2004) and depressed women have been shown to be overly represented in diffuse neurological disease such as Alzheimer’s disease (Okiishi et al., 2001). Thus, our findings suggest that it may be important to consider potential sex differences in the risk for depression for AD patients possessing the APOE ε4 allele. Indeed, sex effects have not been taken into account in many of the previous studies that have demonstrated negative findings. For example, many studies have not distinguished between men and women across APOE genotypes (Weiner et al., 1998; Cantillon et al., 1997; Harwood, Barker, Ownby, St. George-Hyslop, & Duara, 1999; Scarmeas et al., 2002; Craig et al., 2005), have not directly assessed sex differences within their samples (Levy, Cummings, Fairbanks, Sultzer, & Small, 1999; Harwood et al., 1999; Weiner et al., 1999; Scarmeas et al., 2002; Craig et al., 2005), or have not provided sex distributions for their samples (Cantillon et al., 1997). Thus, it is unclear to what extent the lack of measurement for sex differences may have contributed to a lack of association reported in previous studies.
There has also been an interest in the relationship between the effects of estrogen on mood and cognition in aging women. For example, Steffens et al. (1999) examined postmenopausal estrogen use in a population of 2, 388 nondemented older women aged 65 and older. It was found that depression and the APOE ε4 allele both independently predicted depression and that current and past estrogen users demonstrated significantly higher scores on the Modified Mini-Mental State Examination (3MSE). The effect of estrogen replacement therapy (ERT) on cognitive functioning remained after controlling for age, education, and possession of the APOE ε4 allele. When those study participants were followed longitudinally (Carlson et al., 2001), the effect remained and the oldest-old (aged 75 and older) appeared to benefit the most from lifetime ERT. Finally, in a retrospective study which focused on the effects of estrogen on depression, Morrison and Tweedy (2000) reported that estrogen appeared to improve response to antidepressant treatment in postmenopausal women.
To better understand the relationship between ERT and depression in our sample, we completed a post-hoc analysis using retrospective hormonal self-report data. We found a decreased risk of depression among women who underwent ERT (15%) versus those who did not undergo ERT (28.6%). Although the relationship was not statistically significant (possibly due to the low sample size (n = 59)), the trend that was demonstrated warrants further consideration. Overall, there is a paucity of studies that have concurrently investigated the links between estrogen, mood, and APOE genotype, and increased focus and attention in this area is greatly needed.
There are a few limitations of the current study that should be noted. Specifically, although we assessed a broad range of depressive disorders, it is difficult to ascertain the specific causes of depression within the sample. For example, several factors can contribute to depression in later life (i.e., bereavement, polypharmacy, vascular risk factors) and disentangling the potential etiologies is particularly challenging. In addition, a diagnosis of current depression was necessary for inclusion in the depressed group, and we did not assess the lifetime chronicity or time course of depression for each participant. Such information would be preferable in order to track other potential contributors or predisposing factors. Moreover, it is widely known that depression is often one of the first symptoms of AD, although the natural history of depression in AD is poorly understood (Lyketsos & Olin, 2002). Nevertheless, the results of the current study favor a rigorous diagnostic approach in assessing the impact of genetic and other risk factors on depression in AD.
At present, the effect of APOE ε4 genotype on depression in AD is equivocal and there is a need for additional studies to better elucidate this relationship. Future studies may wish to include examination of the various psychiatric assessment instruments employed for diagnosing depression in older adults given the wide-ranging reported rates of depression reported across studies. Also, close examination of the diagnostic criteria utilized in studies to diagnose participants with depression and with AD is critically needed, given the varying reports of APOE ε4 genotypic influences on depression in AD. Including sufficiently large samples of depressed individuals is crucial because of the possible subtle influence of APOE genotype on psychiatric symptomatology. Finally, in addition to our observed gender differences, future efforts should include greater emphasis on links between the APOE ε4 allele and subtle vascular risk (i.e., hypertension, hyperlipidemia, white matter lesion abnormalities) as well as hormonal factors (i.e., estrogen).
Acknowledgments
This work was supported by National Institute on Aging grants RO1 AG12674 and P50 AG05131, and by National Institute of Mental Health grant P30 MH66248. The authors gratefully acknowledge the assistance of staff, patients, and volunteers of the UCSD Alzheimer’s Disease Research Center.
References
- Aggarwal NT, Wilson RS, Beck TL, Bienias JL, Berry-Kravis E, Bennett DA. The apolipoprotein E4 allele and incident Alzheimer’s disease in persons with mild cognitive impairment. Neurocase. 2005;11(1):3–7. doi: 10.1080/13554790490903038. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M. ‘Vascular depression’ hypothesis. J Neuroscience. 1997;17(2):516–529. doi: 10.1001/archpsyc.1997.01830220033006. [DOI] [PubMed] [Google Scholar]
- Alzheimer’s Association. About Alzheimer’s: Statistics about Alzheimer’s disease. [Retrieved December 20 2005];2004 from http://wwwalzorg/AboutAD/statisticsasp.
- Arendt T, Schindler C, Bruckner MK, Eschrich K, Bigl V, Zedlick D, et al. Plastic neuronal remodeling is impaired in patients with Alzheimer’s disease carrying apolipoprotein epsilon 4 allele. J Neuroscience. 1997;17(2):516–529. doi: 10.1523/JNEUROSCI.17-02-00516.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brscic E, Bergerone S, Gagnor A, Colajanni E, Matullo G, Scaglione L, et al. Acute myocardial infarction in young adults: prognostic role of angiotensin-converting enzyme angiotensin II type I receptor apolipoprotein E endothelial constitutive nitric oxide synthase and glycoprotein IIIa genetic polymorphisms at medium-term follow-up. Am Heart J. 2000;139:979–984. doi: 10.1067/mhj.2000.106165. [DOI] [PubMed] [Google Scholar]
- Cantillon M, Harwood D, Barker W, St George-Hyslop P, Tsuda T, Ekatarina R, et al. No association between apolipoprotein E genotype and late-onset depression in Alzheimer’s disease. Biol Psychiatry. 1997;41:246–248. doi: 10.1016/s0006-3223(96)00422-2. [DOI] [PubMed] [Google Scholar]
- Carlson MC, Zandi PP, Plassman BL, Tschanz JT, Welsh-Bohmer KA, Steffens DC, et al. Hormone replacement therapy and reduced cognitive decline in older women. Neurology. 2001;57(12):1–11. doi: 10.1212/wnl.57.12.2210. [DOI] [PubMed] [Google Scholar]
- Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, et al. Gene dose of apolipoprotein E type 4 allele and risk of Alzheimer’s disease in late onset families. Science. 1993;261:921–3. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- Craig D, Hart DJ, McIlroy SP, Passmore AP. Association analysis of apolipoprotein E genotype and risk of depressive symptoms in Alzheimer’s disease. Dementia Geriatric Cognitive Disorders. 2005;19(2–3):154–157. doi: 10.1159/000082887. [DOI] [PubMed] [Google Scholar]
- Crawford FC, Vanderploeg RD, Freeman MJ, Singh S, Waisman M, Michaels L. APOE genotype influences acquisition and recall following traumatic brain injury. Neurology. 2002;58:1115–1118. doi: 10.1212/wnl.58.7.1115. [DOI] [PubMed] [Google Scholar]
- Cummings JL, Ross W, Absher J, Gornbein J, Hadjiaghai L. Depressive symptoms in Alzheimer’s disease: assessment and determinants. Alz Dis Ass Dis. 1995;9:87–93. doi: 10.1097/00002093-199509020-00005. [DOI] [PubMed] [Google Scholar]
- Davignon J, Cohn JS, Mabile L, Bernier L. Apolipoprotein E and atherosclerosis: insight from animal and human studies. Clin Chim Acta. 1999;286:115–143. doi: 10.1016/s0009-8981(99)00097-2. [DOI] [PubMed] [Google Scholar]
- De Leeuw FE, Richard F, de Groot JC, van Duijn CM, Hofman A, Van Gjin J, et al. Interaction between hypertension apoE and cerebral white matter lesions. Stroke. 2004;35(5):1057–1060. doi: 10.1161/01.STR.0000125859.71051.83. [DOI] [PubMed] [Google Scholar]
- Delis DC, Kramer JH, Kaplan E, Ober BA. The California Verbal Learning Test. New York: Psychological Corporation; 1987. [Google Scholar]
- Farrer LA, Cupples JL, Haines B, Hyman WA, Kukull R, Mayeux RH, et al. Effects of age sex and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease: A meta-analysis APOE and Alzheimer Disease Meta Analysis Consortium. JAMA. 1997;278(16):1349–1356. [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: A practical method for grading the cognitive state of patients for the clinician. J Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Forsell Y, Corder EH, Basun H, Lannfelt L, Viitanen M, Winblad B. Depression and dementia in relation to apolipoprotein E polymorphism in a population sample age 75+ Biol Psychiatry. 1997;42:898–903. doi: 10.1016/S0006-3223(96)00468-4. [DOI] [PubMed] [Google Scholar]
- Ganguli M, Dodge HH, Mulsant BH. Rates and predictors of mortaility in an aging rural community-based cohort: the role of depression. Arch Gen Psychiatry. 2002;59(11):1046–1052. doi: 10.1001/archpsyc.59.11.1046. [DOI] [PubMed] [Google Scholar]
- Gabryelewicz T, Religa D, Styczynska M, Peplonska B, Pfeffer A, Wasiak B, et al. Behavioural pathology in Alzheimer’s disease with special reference to apolipoprotein e genotype. Dementia and Geriatric Cognitive Disorders. 2002;14:208–212. doi: 10.1159/000066020. [DOI] [PubMed] [Google Scholar]
- Gonzales-Salvador T, Aragano C, Lyketsos CG, Barba AC. The stress and psychological morbidity of the Alzheimer patient caregiver. Int J Geriatric Psychiatry. 1999;14:701–710. doi: 10.1002/(sici)1099-1166(199909)14:9<701::aid-gps5>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Gonzales-Salvador T, Lyketsos CG, Baker AS, Hovanec L, Roques C, Brandt J, et al. Quality of life of patients with dementia in long-term care. Int J Geriatric Psychiatry. 2000;15(2):181–189. doi: 10.1002/(sici)1099-1166(200002)15:2<181::aid-gps96>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Green RC, Cupples LA, Kurz A, Auerbach S, Go R, Sadovnick D, et al. Depression as a risk factor for Alzheimer disease: the MIRAGE Study. Arch Neurology. 2003;60(5):753–759. doi: 10.1001/archneur.60.5.753. [DOI] [PubMed] [Google Scholar]
- Harwood DG, Barker WW, Ownby RL, St George-Hyslop P, Duara R. Apolipoprotein-E (APO-E) genotype and symptoms of psychosis in Alzheimer’s disease. Am J Geriatric Psychiatry. 1999;7(2):119–123. [PubMed] [Google Scholar]
- Hippisley-Cox J, Pringle M, Crown N, Meal A, Wynn A. Sex inequalities in ischaemic heart disease in general practice: cross sectional survey. Brit Med J. 2001;322(7290):832–835. doi: 10.1136/bmj.322.7290.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hachinski VC, Ilif LD, Zilcha IE, Du Boulay GH, McAllister VL, Marshall J, et al. Cerebral blood flow in dementia. Arch Neurology. 1975;32(9):632–637. doi: 10.1001/archneur.1975.00490510088009. [DOI] [PubMed] [Google Scholar]
- Hoch CC, Reynolds CF, Buysse DJ, Fasiczka AL, Houck AL, Mazumdar S, et al. Two-year survival in patients with mixed symptoms of depression and cognitive impairment: Comparison with major depression and primary degenerative dementia. Am J Geriatric Psychiatry. 1993;1(1):59–66. doi: 10.1097/00019442-199300110-00008. [DOI] [PubMed] [Google Scholar]
- Hofman A, Ott A, Breteler MM, Bots ML, Slooter AJ, van Harskamp F, et al. Atherosclerosis apolipoprotein E and prevalence of dementia and Alzheimer disease in the Rotterdam Study. Lancet. 1997;349(9046):151–154. doi: 10.1016/S0140-6736(96)09328-2. [DOI] [PubMed] [Google Scholar]
- Krishnan KRR, Tupler LA, Ritchie JC, McDonald WM, Knight DL, Nemeroff CB, Carroll BJ. Apolipoprotein E-ε4 frequency in geriatric depression. Biol Psychiatry. 1996;40:69–71. doi: 10.1016/0006-3223(95)00424-6. [DOI] [PubMed] [Google Scholar]
- Lavretsky H, Lesser IM, Wohl M, Miller BL, Mehringer M, Vinters HV. Apolipoprotein-E and white-matter hyperintensities in late-life depression. Am J Geriatric Psychiatry. 2000;8:257–261. [PubMed] [Google Scholar]
- Levy ML, Cummings JL, Fairbanks LA, Sultzer DL, Small GW. Apolipoprotein E genotype and noncognitive symptoms in Alzheimer’s disease. Biol Psychiatry. 1999;45:422–425. doi: 10.1016/s0006-3223(98)00041-9. [DOI] [PubMed] [Google Scholar]
- Liu CY, Hong CJ, Liu TY, Lin KN, Wang PN, Chi CW, Chuang YY, Liu HC. Lack of association between the ApoE genotype and depression in Alzheimer’s disease. J Ger Psychiatry Neurology. 2002;15(1):20–23. doi: 10.1177/089198870201500105. [DOI] [PubMed] [Google Scholar]
- Lyketsos CG, Tune LE, Pearlson G, Steele C. Major depression in Alzheimer’s disease: An interaction between gender and family history. Psychosomatics. 1996;37(4):380–384. doi: 10.1016/S0033-3182(96)71552-9. [DOI] [PubMed] [Google Scholar]
- Lyketsos CG, Steele C, Baker L, Galik E, Kopunek S, Steinberg M, et al. Major and minor depression in Alzheimer’s disease: prevalence and impact. J Neuropsychiatry Clinical Neuroscience. 1997b;9:556–561. doi: 10.1176/jnp.9.4.556. [DOI] [PubMed] [Google Scholar]
- Lyketsos CG, Olin J. Depression in Alzheimer’s Disease: Overview and Treatment. Biol Psychiatry. 2002;52:243–252. doi: 10.1016/s0006-3223(02)01348-3. [DOI] [PubMed] [Google Scholar]
- Magni E, Binetti G, Bianchetti A, Trabucchi M. Risk of mortality and institutionalization in demented patients with delusions. J Geriatric Psychiatry Neurology. 1996;9(3):123–126. doi: 10.1177/089198879600900303. [DOI] [PubMed] [Google Scholar]
- Mattis S. Dementia Rating Scale. Odessa FL: Psychological Assessment Resources; 1988. [Google Scholar]
- McCarron MO, Delong D, Alberts MJ. APOE genotype as a risk factor for ischemic cerebrovascular disease. Neurology. 1999;53(6):1308–1311. doi: 10.1212/wnl.53.6.1308. [DOI] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlin EM. Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA work group under the auspices of the Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- Michikawa M, Fan QW, Isobe I, Yanagisawa K. Apolipoprotein E exhibits isoform-specific promotion of lipid efflux from astrocytes and neurons in culture. J Neurochemistry. 2000;74:1008–1016. doi: 10.1046/j.1471-4159.2000.0741008.x. [DOI] [PubMed] [Google Scholar]
- Morrison MF, Tweedy K. Effects of estrogen on mood and cognition in aging women. Psychiatric Annals. 2000;30(2):113–119. [Google Scholar]
- Müller-Thomsen T, Arlt S, Ganzer S, Mann U, Mass R, Naber D, et al. Depression in Alzheimer’s disease might be associated with apolipoprotein E e4 allele: Frequency in women but not in men. Dementia and Geriatric Cognitive Disorders. 2002;14:59–63. doi: 10.1159/000064926. [DOI] [PubMed] [Google Scholar]
- Murman DL, Chen MS, Powell MC, Kuo SB, Bradley CJ, Colenda CC. The incremental direct costs associated with behavioral symptoms in AD. Neurology. 2002;59:1721–1729. doi: 10.1212/01.wnl.0000036904.73393.e4. [DOI] [PubMed] [Google Scholar]
- Murphy GM, Taylor J, Tinklenberg JR, Yesavage JA. The apolipoprotein E epsilon 4 allele is associated with increased behavioral disturbance in Alzheimer’s disease. Am J Geriatric Psychiatry. 1997;5(1):88–89. doi: 10.1097/00019442-199700510-00012. [DOI] [PubMed] [Google Scholar]
- Okiishi CG, Paradiso S, Robinson RG. Gender differences in depression associated with neurologic illness: clinical correlates and pharmacological response. J Gender Specific Med. 2001;4(2):65–72. [PubMed] [Google Scholar]
- Ramachandran G, Marder K, Tang M, Schofield PW, Chun MR, Devanand DP, et al. A preliminary study of apolipoprotein E genotype and psychiatric manifestations of Alzheimer’s disease. Neurology. 1996;47:256–259. doi: 10.1212/wnl.47.1.256. [DOI] [PubMed] [Google Scholar]
- Rigaud A, Traykov L, Caputo L, Coste J, Latour F, Couderc R, et al. Association of the apolipoprotein E 4 allele with late-onset depression. Neuroepidemiology. 2001;20(4):268–272. doi: 10.1159/000054801. [DOI] [PubMed] [Google Scholar]
- Roses AD. Apolipoprotein E affects the rate of Alzheimer disease expression: beta-amyloid burden is a secondary consequence dependent on APOE genotype and duration of disease. J Neuropathol Exp Neurol. 1994;53:429–437. doi: 10.1097/00005072-199409000-00002. [DOI] [PubMed] [Google Scholar]
- Salmon DP, Butters N. Neuropsychological assessment of dementia in the elderly. In: Katzman R, Rowe JW, editors. Principles of geriatric neurology. Philadelphia: F A Davis; 1992. pp. 144–5163. [Google Scholar]
- Saunders AM, Strittmatter WJ, Schmechel D, St George-Hyslop PH, Perick-Vance MA, Joo SH, et al. Association of apolipoprotein E allele e4 with late-onset familial and sporadic Alzheimer’s disease. Neurology. 1993;43:1467–1472. doi: 10.1212/wnl.43.8.1467. [DOI] [PubMed] [Google Scholar]
- Sawada H, Udaka F, Izumi Y, Nishinaka K, Kawakami H, Nakamura S, Kameyama M. Cerebral white matter lesions are not associated with apoE genotype but with age and female sex in Alzheimer’s disease. J Neurology Neurosurgery Psychiatry. 2000;68:653–656. doi: 10.1136/jnnp.68.5.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarmeas N, Brandt J, Albert M, Devanand DP, Marder K, Bell K, et al. Association between the APOE genotype and psychopathologic symptoms in Alzheimer’s disease. Neurology. 2002;58:1182–1188. doi: 10.1212/wnl.58.8.1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shearman MS. Amyloid-β hypothesis of Alzheimer’s disease. In: Fisher A, Hanin I, Yoshida M, editors. Progress in Alzheimer’s and Parkinson’s Diseases. Plenum Press; New York: 1998. pp. 187–190. [Google Scholar]
- Steffens DC, Plassman BL, Helms MJ, Welsh-Bohmer KA, Saunders AM, Breithner JC. A twin study of late-onset depression and apolipoprotein E epsilon 4 as risk factors for Alzheimer’s disease. Biol Psychiatry. 1997;41:851–856. doi: 10.1016/S0006-3223(96)00247-8. [DOI] [PubMed] [Google Scholar]
- Steffens DC, Norton MC, Plassman BL, Tschanz JT, Wyse BW, Welsh-Bohmer KA, et al. Enhanced cognitive performance with estrogen use in nondemented community-dwelling older women. J Am Geriatrics Society. 1999;47(10):1171–1175. doi: 10.1111/j.1532-5415.1999.tb05195.x. [DOI] [PubMed] [Google Scholar]
- Stern Y, Tang MX, Albert MS, Brandt J, Jacobs DM, Bell K, et al. Predicting time to nursing home care and death in individuals with Alzheimer disease. JAMA. 1997;277(10):806–812. [PubMed] [Google Scholar]
- Tractenberg RE, Weiner MF, Patterson MB, Teri L, Thal LJ. Comorbidity of psychopathological domains in community-dwelling persons with Alzheimer’s disease. J Geriatric Psychiatry Neurology. 2003;16(2):94–99. doi: 10.1177/0891988703016002006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler memory scale-revised. San Antonio TX: The Psychological Corporation; 1987. [Google Scholar]
- Weiner MF, Vega G, Risser RC, Honig LS, Cullum CM, Crumpacker D, et al. Apolipoprotein Eε4, other risk factors, and course of Alzhiemer’s disease. Soc Biol Psychiatry. 1999;45:633–638. doi: 10.1016/s0006-3223(98)00222-4. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Barnes LL, Mendez de Leon CF, Aggarwal NT, Schneider JS, Bach J, et al. Depressive symptoms cognitive decline and risk of AD in older persons. Neurology. 2002;59:364–370. doi: 10.1212/wnl.59.3.364. [DOI] [PubMed] [Google Scholar]
- Wragg R, Jeste DV. Overview of depression and psychosis in Alzheimer’s disease. Am J Psychiatry. 1989;146(5):577–587. doi: 10.1176/ajp.146.5.577. [DOI] [PubMed] [Google Scholar]
- Zubenko GS. Neurobiology of major depression in Alzheimer’s disease. Int Psychogeriatrics. 2000;12(Suppl 1):217–230. [Google Scholar]
- Zubenko GS, Henderson R, Stiffler JS, Stabler S, Rosen J, Kaplan BB. Association of the APOE 4 allele with clinical subtypes of late life depression. Biol Psychiatry. 1996;40(10):1008–1016. doi: 10.1016/s0006-3223(96)00046-7. [DOI] [PubMed] [Google Scholar]