Abstract
The genetic basis for virulence and host switching in influenza A viruses (FLUAV) is largely unknown. Because the hemagglutinin (HA) protein is a determinant of these properties, HA evolution was mapped in an experimental model of mouse lung adaptation. Variants of prototype A/Hong Kong/1/68 (H3N2) (wild-type [wt] HK) human virus were selected in both longitudinal and parallel studies of lung adaptation. Mapping of HA mutations found in 11 independently derived mouse-adapted populations of wt HK identified 27 mutations that clustered within two distinct regions in or near the globular frameworks of the HA1 and HA2 subunits. The adaptive mutations demonstrated multiple instances of convergent evolution involving four amino acid positions (162, 210, and 218 in HA1 and 154 in HA2). By use of reverse genetics, convergent HA mutations were shown to affect cell tropism by enhancing infection and replication in primary mouse tracheal epithelial cells in vitro and mouse lung tissue in vivo. Adaptive HA mutations were multifunctional, affecting both median pH of fusion and receptor specificity. Specific mutations within both adaptive regions were shown to increase virulence in a mouse lung model. The occurrence of mutations in the HA1 and HA2 adaptive regions of natural FLUAV host range and virulent variants of avian and mammalian viruses is discussed. This study has identified adaptive sites and regions within the HA1 and HA2 subunits that may guide future studies of viral adaptation and evolution in nature.
In order to assess the pandemic potential of influenza A virus (FLUAV) strains, there is currently a need to understand the genetic control of host range and virulence. Receptor binding specificity of the hemagglutinin (HA) protein is a determinant of the ability of FLUAV to infect different host species. The HA gene is a genetic determinant of enhanced virulence, as shown for highly pathogenic avian H5N1 (6) strains and the 1918 human pandemic strain (22).
HA binds to receptors possessing terminal N-acetyl neuraminic acid, also termed sialic acid (SA), linked to galactose through either α2-3 or α2-6 bonds (α2,3 SA or α2,6 SA, respectively). Subsequent to binding and internalization within endosomes, the HA protein mediates fusion and uncoating due to low-pH-induced conformational changes (25). HA preferentially binds to the linkages that are abundant in their natural host such that avian strains preferentially bind α2,3 SA and human strains preferentially bind α2,6 SA (15). Human respiratory epithelia have been shown to possess α2,6 SA on ciliated, nonciliated, and goblet cells, with α2,3 SA on ciliated and alveolar epithelia (14, 18). Avian FLUAVs preferentially infect and are restricted to the ciliated epithelium, but human strains have a predilection for the nonciliated epithelium, with subsequent spread to the ciliated epithelium (18). The mouse airway and alveolar receptors are exclusively of the α2,3 SA linkage type, thus demonstrating differences with respect to human tracheal epithelia but similarities to human alveolar epithelia (4, 18).
Adaptation of avian H1, H2, and H3 subtypes to humans involves mutations that increase receptor specificity for SA α2,6 Gal. The primary receptor binding site (RBS) contacts SA via three HA1 secondary structural components: the 190 helix (amino acid [aa] residues 190 to 198), the 130 loop (aa residues 135 to 138), and the 220 loop (aa residues 221 to 228) (25). Mutations in these regions have been shown to increase human receptor binding for the 1918 (H1N1) pandemic virus (mutations E190D and G225D) (16) and human H2 and H3 subtype viruses (mutations Q226L and G228S in both) (16, 28). Human adaptive HA mutations in H5N1 isolates have been observed at multiple sites in the RBS, such as S227N (7), L133V plus A138V (1), and N186K plus Q196R (31) (all H3 numbering).
Experimental evolution of human FLUAV by serial passage in the mouse lung results in the selection of mouse-adapted (MA) variants with enhanced abilities to replicate and cause fatal pneumonia in mice (3). Genomic and reassortant analysis of a virulent MA variant of A/FM/1/47 (H1N1) identified five mutations that all functioned to increase replication and virulence in the mouse lung, including a W472G mutation in the HA2 subunit (superscripts 1 and 2 denote HA1 and HA2, respectively) that increased virulence 102.3-fold (2, 26). Because the mouse lung possesses only avian-like α2,3 SA receptors (14), mouse adaptation of human influenza virus is expected to involve mutations that increase α2,3 SA binding. Other studies have shown that MA variants of human H1N1 and H3N2 viruses also possess altered pH of fusion, indicating that fusion properties are altered during mouse adaptation (12, 27).
In this study, variants were generated on serial passage in the mouse in order to map adaptive regions and sites within the HA protein. Mutations were observed to cluster within two regions, one in HA1 and one in HA2, that were both involved in controlling adaptation and virulence.
MATERIALS AND METHODS
Cells.
Madin-Darby canine kidney (MDCK) cells and 293T human embryonic kidney cells were maintained in minimum essential medium supplemented with l-glutamine (200 mM), penicillin (100 U/ml), streptomycin (100 μg/ml), and fetal bovine serum (10%). Mouse tracheal epithelial cells (mTECs) were cultured and differentiated under the air-liquid interface as previously described by Ibricevic et al. (14).
Viruses.
The prototype clinical isolate A/HK/1/68 (H3N2) (wild-type [wt] HK) was obtained from the Laboratory Center for Disease Control, Health Canada, Ottawa, ON, Canada. Viruses were purified by plaque isolation in MDCK cells, and stocks were prepared in MDCK cells or alternatively by a single passage in the allantoic cavity of 10-day-old specific-antigen-free chicken embryos (Canadian Food Inspection Agency, Ottawa, ON, Canada). Studies were initiated using MA clones that were previously derived from wt HK after 12 and 20 passages in the mouse lung (3). Briefly, virus was passaged in the mouse lung by cycles of intranasal infection under halothane anesthesia for groups of three CD-1 mice for 3 days for a total of 20 passages, with collection of viral clones by plaque isolation at passages 12 and 20. Independent mouse adaptation experiments employed 10 sister clones derived by plaque isolation from wt HK and amplification in 9- to 10-day-old specific-pathogen-free chicken embryos. All sister clone HA genes were sequenced and shown to possess the same coding sequence as the parental wt HK virus. Serial passages were initiated with 106 PFU for passage 1 and subsequently employed 50 μl of 0.22-μm-filtered lung extracts (1 ml of phosphate-buffered saline [PBS]/lung) for subsequent inoculation into CD-1 mice. Because the previously isolated MA variant of HK virus grew to maximal titers in the mouse lung after 1 day postinfection (dpi) instead of 2 for the wt HK virus, we initiated the mouse passages by using 10 passages with 1-day durations in individual mice. However, the resulting populations showed that no mutations were selected in the M1 or NS1 genes after this level of passage (data not shown). Continued passages employed five cycles with two mice each for 2 days, which showed the selection of HA mutations in 1 of 10 passaged populations (the HK5 population). Subsequent passages employed six cycles with two mice each for 3 days before the MA clones were isolated; thus, each isolate was passaged for a total of 21 passages (10 passages [one mouse for 1 day] plus 5 passages [two mice for 2 days] plus 6 passages [two mice for 3 days]). For each of the 10 independent MA passage 21 populations, three clones were isolated by two sequential plaque purifications (designated with “HK,” then the sister clone number, then “MA,” and then the mouse passage number).
Hemolysis.
Hemolysis assays were performed as previously described (27). Briefly, 50-μl aliquots of virus (possessing ≥107 PFU of virus) were adsorbed with 50 μl of 2% washed human red blood cells (less than 48 h old) before sedimentation. Supernatants were decanted, and pellets were suspended in 100 μl of 100 mM citrate buffers covering a pH range of 5 to 6. Samples were incubated at 37°C before sedimentation of blood cells and transfer of supernatant to a plate for spectrophotometric measurement based on optical density at 540 nm. Samples were analyzed in duplicate, and the control values for the virus suspension medium were subtracted from each test sample.
Reverse genetics.
The HA and neuraminidase (NA) genome segments of the parental A/HK/1/68 and the HA genome segments of specific MA variants were inserted into the pHH21A vector by using ligation-independent cloning as described previously (29). Monolayer cultures containing a mixture of 293T and MDCK cells were used to rescue defined HA genes in combination with the wt HK NA gene onto an A/WSN/33 backbone (provided by Y. Kawaoka), using the method described by Neumann et al. (21). Recombinant viruses possessed either the wt HK HA and NA genes or the mutant HK HA genes in combination with the wt HK NA gene. Supernatants were collected at 48 h posttransfection and grown in MDCK cells before sequence verification of each HA gene variant.
Sialylglycopolymers and solid-phase binding assay.
The synthetic ligands used in this study were 6′ sialyl-(N-acetyllactosamine) (6′SLN), 3′ sialyl-(N-acetyllactosamine) (3′SLN), 6′ sialyllactose (6′SL), and 3′ sialyllactose (3′SL). These ligands contained biotin that was attached to a soluble polyacrylamide linker. The binding protocol involved binding SA ligands to viruses immobilized on 96-well plates as previously described by Matrosovich et al. (16).
Infection of mTECs.
Cells grown at the air-liquid interface were washed with PBS and supplemented with medium containing Dulbecco's modified Eagle's medium-Ham's F-12 medium with 30 mM HEPES, 4 mM l-glutamine, 3.5 mM NaHCO3, 100 U/ml penicillin, and 100 μg/ml streptomycin. The apical surfaces of cells containing 2 × 105cells/insert were infected with 6 × 105 PFU of the recombinant viruses for 30 min to achieve a multiplicity of infection (MOI) of 3 and incubated for 20 h before apical medium was collected for titration of infectious virus by a plaque assay.
Immunohistochemistry of mTECs.
mTECs on supported membranes were stained for viral antigen as previously described, using 1/1,000 of the primary antibody, rabbit serum against A/HK/1/68 virus (14). The signal was detected using secondary antibody conjugated with Alexa Fluor 555 (Molecular Probes, Carlsbad, CA). No detectable staining was observed for species-specific control antibodies. The figures were organized using Photoshop software (Adobe Systems, San Jose, CA).
Immunofluorescence staining of BALB/c mice.
BALB/c mice (4- to 6-week-old females from Charles River Laboratories, Montreal, Quebec, Canada) were infected intranasally with 105 PFU of the recombinant viruses, and lungs were collected at 2 dpi. Infected lungs were fixed in 10% buffered formalin for 24 h, and frozen sections were prepared. Viral antigen was detected by incubating the sections with anti-HK primary rabbit antibody diluted (1/1,000) in buffer (10 mM PBS containing 3% bovine serum albumin and 0.3% Triton X-100). After being washed with 10 mM PBS, the slides were incubated with Cy3-conjugated donkey anti-rabbit secondary antibody (Jackson ImmunoResearch laboratories Inc., ME) diluted (1/800) in the antibody buffer. The slides were then washed, and nuclei were stained by incubation with 100 μl of Hoechst (0.2 μg/ml). Images were taken at ×20 magnification by using an Olympus BX50 microscope and organized using Adobe Photoshop 7.0 and Corel Draw 10 software.
LD50.
Five mice were inoculated per group, and mortality was monitored for 10 days. The median lethal dose (LD50) was measured in PFU after intranasal infection of BALB/c mice with various recombinant viruses by use of the Karber-Spearman method (19). The Karber-Spearman method calculates the LD50 by the following equation: negative log of LD50 = negative log10 of highest dose − [−(sum of percent mortality at each dose/100) × log10 of dilution steps].
Growth of the recombinant viruses in the mouse lung.
Groups of three BALB/c mice were infected intranasally with 5 × 103 PFU of the recombinant viruses, and lungs were collected at 3 dpi. The lungs were suspended in 4 volumes (wt/wt) of PBS and sonicated before titration by a MDCK cell plaque assay.
Locations of mutations in the HA trimer structure.
The figures were created with PyMOL software, using a monomer of the A/HK/1/68 H3 HA structure (Protein Data Bank number 1HGD).
Nucleotide sequence accession numbers.
Nucleotide sequences have been deposited in GenBank under accession numbers FU215802 to FU215856.
RESULTS
Sequence analysis of MA strains.
Prior mouse adaptation of the avirulent prototype clinical isolate A/HK/1/68 (LD50 > 107.7) showed that following 12 passages in the mouse lung, the virus population had an LD50 of 103.7 PFU, which after 20 passages decreased to 102.7 PFU (3). To identify HA mutations in variants in the passage 12 population, six clones were sequenced (HKMA-12 to HKMA-12E [3]) (Table 1). All six clones possessed mutant forms of HA, with five possessing two mutations. The G2181W mutation in HA1 was most prevalent and was found in four clones (HKMA-12, -12C, -12D, and -12E), with three of them possessing a second mutation, T1562N in HA2. This pattern suggested that the G2181W mutation (found in isolation in HKMA-12E) preceded the T1562N mutation. The two other double mutants, HKMA-12a and -12b, possessed two mutations in HA1 (D21Y and N2461D) and possessed one mutation in HA1 (P1621L) and one in HA2 (D1582N), respectively.
TABLE 1.
Mutations in the HA proteins of clones of MA A/HK/1/68 obtained after passages 12 (HKMA-12 to HKMA-12E) and 20 (HKMA-20 to HKMA-20E)
| Virus | Mutationa in indicated protein at indicated aa position
|
||||||
|---|---|---|---|---|---|---|---|
| HA1
|
HA2
|
||||||
| 2 | 162 | 218 | 246 | 154 | 156 | 158 | |
| HK wt | D | P | G | N | N | T | D |
| HKMA-12 | − | W | − | − | N | − | |
| HKMA-12A | Y | − | − | D | − | − | − |
| HKMA-12B | − | L | − | − | − | − | N |
| HKMA-12C | − | − | W | − | − | N | − |
| HKMA-12D | − | − | W | − | − | N | − |
| HKMA-12E | − | − | W | − | − | − | − |
| HKMA-20 | − | − | W | − | − | N | − |
| HKMA-20A | − | − | W | − | − | N | − |
| HKMA-20B | − | − | W | − | − | N | − |
| HKMA-20C | − | − | W | − | − | N | − |
| HKMA-20D | − | − | W | − | S | − | − |
| HKMA-20E | − | − | W | − | − | N | − |
− indicates identity with the parental sequence.
Sequence analysis of six clones from the passage 20 MA population (HKMA-20 to HKMA-20E) confirmed that the G2181W mutation was the most common adaptive mutation, as it was selected in all the passage 20 clones, along with a mutation in HA2 at position 154 or 156 (Table 1). The HA2 N1542S and T1562N mutations demonstrated convergent evolution since both of these mutations remove the same N-linked glycosylation site (1542NGT1562 mutated to SGT and NGN, respectively) (3).
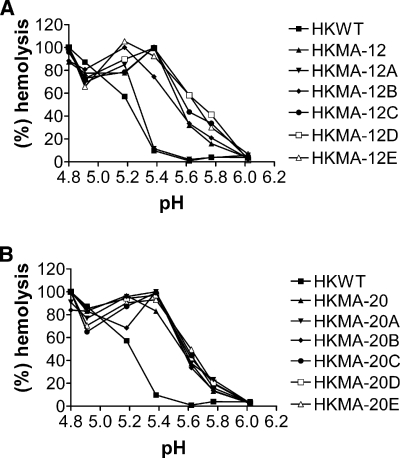
Role of HA mutations in pH of fusion.
Because previous analysis had demonstrated an increased pH of fusion for some of the HKMA clones (3), hemolysis assays were performed to measure the optimal pH of fusion for each of the variants after passages 12 and 20 of A/HK/1/68. In comparison to the HK parent, most of the passage 12 clones and all of the passage 20 clones showed an increased median pH of fusion, from pH 5.2 to 5.6, which represented an increase of 0.4 pH units (Fig. 1A and B). The only exception was isolate HKMA-12A, which demonstrated a minor increase in pH of fusion of approximately 0.05 pH units (Fig. 1A). These results indicated that mutations that increase the pH of fusion are under positive selection on mouse adaptation. Previous studies in our laboratory have also demonstrated that mouse adaptation of A/FM/1/47 results in a virus that fuses at pH 5.6, indicating that this level might be optimal for replication within the mouse lung (27).
FIG. 1.
pH dependence of hemolysis by wt HK and the MA isolates. The extent of hemolysis was measured at 0.2-pH increments, and the assays were performed using human blood. Hemolysis was monitored by measuring released hemoglobin spectrophotometrically at 540 nm for passage 12 MA isolates (HKMA-12 to HKMA-12E) (A) and passage 20 MA isolates (HKMA-20 to HKMA-20E) (B).
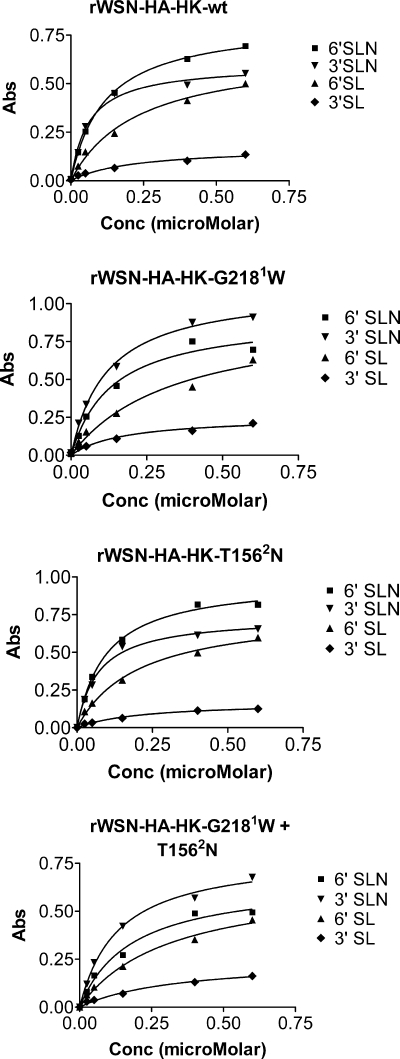
Receptor binding specificity of the recombinant viruses.
To study the HA mutations in isolation, recombinant viruses were generated using the 12-plasmid rescue system (21). All the synthetic viruses contained the HA and NA genes of A/HK/1/68 virus on the A/WSN/33 backbone to generate viruses with H3N2 surface genes. Viruses that contained the most common adaptive mutations that were acquired after passages 12 and 20 were generated, possessing either the G2181W or the T1562N mutation alone or a combination of both. The binding specificity of these viruses was investigated using biotin-labeled synthetic ligands containing either Neu5Acα2,6 lactose or Neu5Acα2,6 lactosamine (6′SL or 6′SLN, respectively) or Neu5Acα2,3 lactose or Neu5Acα2,3 lactosamine (3′SL or 3′SLN, respectively), thus representing human or avian/mouse-type linkages, respectively. The recombinant WSN (rWSN)-HA-HK wt and mutant viruses were indistinguishable in binding to the respective SL ligands in that all bound 6′SL to a much greater extent than 3′SL, which was consistent with previous demonstrations of A/HK/1/68 SA binding (17) and indicated that the G2181W and T1562N mutations did not significantly change the pattern of binding to this pair of ligands (Fig. 2).
FIG. 2.
Receptor binding specificities of recombinant viruses. The binding affinities of the recombinant viruses for different biotin-labeled trisaccharides (3′SL, 6′SL, 3′SLN, and 6′SLN) were measured using horseradish peroxide-labeled streptavidin. The graphs plot the amounts of bound SA ligand assayed by absorbance at 450 nM relative to ligand concentrations. Abs, absorbance.
Binding studies have shown that production of 6′SLN by N-acetyl modification of the third sugar significantly enhances binding in comparison to levels for 6′SL (8, 20). When this ligand was used along with 3′SLN, both rWSN-HA-HK wt and the rWSN-HA-HK T1562N mutant bound both ligands well but maintained binding preferences for 6′SLN relative to 3′SLN. This binding pattern was reversed for recombinant viruses containing the G2181W mutation alone or in combination with T1562N (rWSN-HA-HK G2181W or rWSN-HA-HK G2181W+T1562N, respectively), each of which demonstrated a change in binding specificity to a preference for 3′SLN over 6′SLN (Fig. 2). The binding data indicated that the G2181W mutation enhances binding to 3′SLN while maintaining binding to the N-acetyl 6′SLN ligands and had thus changed the binding preference from α2,6 to α2,3 linkage-type ligands. This change in binding was evident with the ligands possessing the amino-modified glucose at the third position (6′ and 3′SLN) but not the SL ligands, suggesting that the G2181W mutation may affect binding to the ligand side chains of α2,3-type SA receptors.
Parallel mouse adaptation of A/HK/1/68.
To further identify HA mutations that mediate mouse-adaptive variation, 10 clones of the parental HK/1/68 virus (sister clones) were independently adapted to the mouse lung by 21 mouse-to-mouse passages. Serial passage was similar to the preceding serial passage except that fewer mice were infected for shorter times (from 1 to 3 days; see Materials and Methods). Three clones were isolated from each passage 21 population, and the HA genes were sequenced (Table 2). All passaged populations were composed primarily of HA mutants (two of three or three of three) and in addition possessed multiple mutant types, with a single population (HK6MA21) being composed of one mutant type (Table 2). The mutant-type HA genes were mainly single (15 of 25) and double (11 of 25) mutants, with a single triple mutant (HK9MA21 clone 3) (Table 2). Comparison of mutations among independent populations showed that a number of identical mutations were independently selected to demonstrate convergent evolution. Convergent evolution was demonstrated both by parallel mutations, where identical mutations are observed in independently adapted variants, and by directional mutations, where the same site was mutated but with different amino acids (3). The most dominant mutation was the G2181E mutation, which was selected in 4 of the 10 populations (HK4MA21, HK5MA21, HK6MA21, and HK8MA21), and the Q210R mutation, selected in 3 populations (HK2MA21, HK10MA21, and HK12MA21). Multiple mutations were seen at positions 218 (G2181W and G2181E) and 162 (P1621L and P1621S) of HA1 and positions 154 (N1542K and N1542S) and 156 (T1562N) of HA2, which all remove the same glycosylation site (Tables 1 and 2). The original, plaque-purified stock of A/HK/1/68 used to perform these studies consisted of a mixture of viruses that differed due to a silent mutation at nucleotide 669 (A669 or G669) and thus differed among the 10 sister clones. This mutation was used as a reference marker for discriminating independently passaged viruses and for excluding cross-contamination as an explanation for convergent evolution (Table 2).
TABLE 2.
Mutations detected in the HA proteins of 10 sister clones of A/HK/1/68 derived by independent mouse adaptations
| Virusa | Clone no. | Mutationb in indicated protein at indicated aa position
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| nt
|
HA1
|
HA2
|
||||||||||||||||||||
| 669 | 124 | 162 | 165 | 192 | 210 | 218 | 220 | 223 | 231 | 238 | 242 | 244 | 262 | 268 | 29 | 117 | 124 | 154 | 160 | 175 | ||
| A/HK/1/68 | G/A | G | P | N | T | Q | G | R | V | S | K | V | V | T | M | S | K | R | N | D | G | |
| HK1MA21 | 1 | G | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | R | − | − | − | − |
| HK1MA21 | 2 | G | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK1MA21 | 3 | G | − | − | − | − | − | − | S | − | − | − | − | − | − | − | Y | − | − | − | − | − |
| HK2MA21 | 1 | A | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK2MA21 | 2 | A | − | − | − | − | R | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK2MA21 | 3 | A | − | S | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK4MA21 | 1 | G | − | − | − | − | − | E | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK4MA21 | 2 | G | − | − | − | − | − | E | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK4MA21 | 3 | G | − | − | − | − | − | − | − | − | − | − | E | − | − | − | − | − | − | − | − | − |
| HK5MA21 | 1 | A | − | − | − | − | − | E | − | − | − | − | − | − | − | − | − | − | − | − | − | D |
| HK5MA21 | 2 | A | − | − | − | − | − | E | − | − | − | − | − | − | − | V | − | − | − | − | − | − |
| HK5MA21 | 3 | A | − | − | − | − | − | E | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK6MA21 | 1 | A | − | − | − | − | − | E | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK6MA21 | 2 | A | − | − | − | − | − | E | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK6MA21 | 3 | A | − | − | − | − | − | E | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK8MA21 | 1 | G | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK8MA21 | 2 | G | − | − | − | − | − | E | − | − | − | − | − | − | − | − | − | − | − | K | − | − |
| HK8MA21 | 3 | G | − | − | − | − | − | E | − | − | − | N | − | − | − | − | − | − | − | − | − | − |
| HK9MA21 | 1 | A | − | − | − | − | − | − | − | − | N | − | − | − | N | − | − | − | − | − | − | − |
| HK9MA21 | 2 | A | − | − | − | − | − | − | − | − | − | − | − | − | N | − | − | − | − | − | − | − |
| HK9MA21 | 3 | A | − | − | − | − | − | − | − | I | N | − | − | − | N | − | − | − | − | − | − | − |
| HK10MA21 | 1 | G | − | − | − | A | R | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK10MA21 | 2 | G | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | K | − | − | − |
| HK10MA21 | 3 | G | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK11MA21 | 1 | G | D | − | D | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK11MA21 | 2 | G | D | − | D | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − |
| HK11MA21 | 3 | G | − | − | − | − | − | − | − | − | − | − | − | E | − | − | − | − | − | − | − | − |
| HK12MA21 | 1 | G | − | − | − | − | R | − | − | − | − | − | − | − | − | − | − | − | − | − | N | − |
| HK12MA21 | 2 | G | − | − | − | − | R | − | − | − | − | − | − | − | − | − | − | − | − | − | N | − |
| HK12MA21 | 3 | G | − | − | − | − | R | − | − | − | − | − | − | − | − | − | − | − | − | − | N | − |
Each passage series is designated with “HK,” then the sister clone number, then “MA,” and then the mouse passage number.
Bold font indicates convergent mutations. − indicates identity with the parental virus sequence. nt, nucleotide.
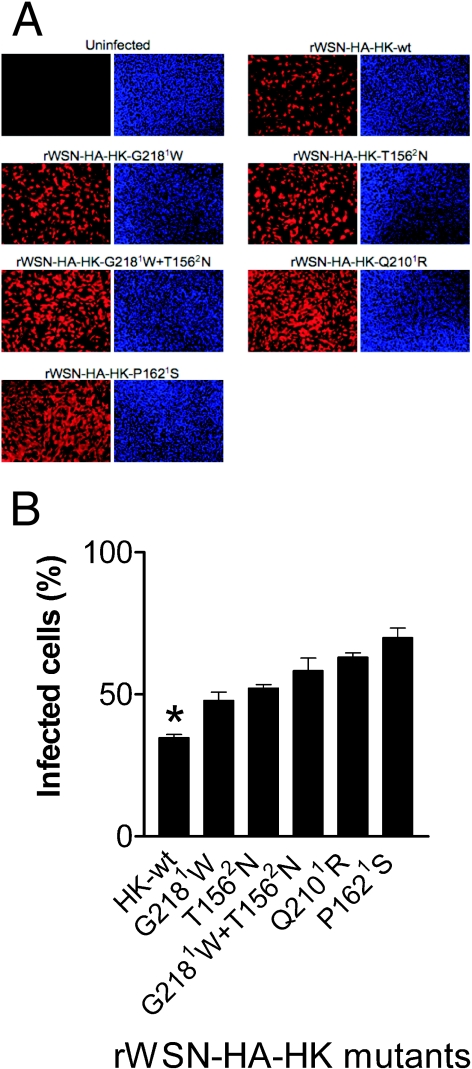
Infection of mTECs with recombinant HA mutants.
To determine the adaptive nature of a subset of mouse-selected mutations occurring at sites of convergent evolution, infection and viral replication of recombinant HA mutants in primary mTECs were assessed. mTECs were cultured and differentiated under air-liquid interface conditions, infected with five recombinant viruses (possessing the mutations G2181W, T1562N, G2181W+T1562N, P1621S, and Q2101R) at an MOI of 3, and assayed at 20 h postinfection. The extent of infection was measured by assessing protein expression in infected cells as detected both by immunofluorescent staining with anti-HK antibody and by titration of infectivity of released virus.
Immunofluorescence of infected cultures showed that all of the recombinant mutants demonstrated significantly greater abilities to infect mTECs, as assessed by the proportions of cells expressing detectable viral protein, than rWSN-HA-HK wt (P < 0.0001; t test) (Fig. 3A and B). The P1621S and Q2101R mutants demonstrated the greatest increases in ability to infect mTECs. The G2181W and T1562N mutations in combination were more infectious than either mutation alone, indicating that their effects were cumulative.
FIG. 3.
Increased infection of mTECs with recombinant HA mutant viruses. The cells were cultured under air-liquid interface conditions and infected with the indicated recombinant viruses at an MOI of 3 for 20 h. (A) Viral expression was detected by staining with anti-HK antibody (red). The nuclei were stained with DAPI (4′,6-diamidino-2-phenylindole) (blue). (B) Percentages of infected cells were counted for multiple microscopic fields (n = 4 to 8) from duplicate infections for each sample and are shown as averages ± standard deviations. All the mutants infected significantly more cells than the wt (P < 0.0001) (*).
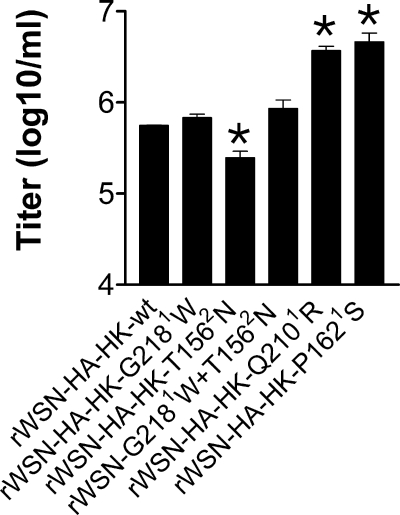
Titration of infectious virus released from the mTEC infections showed that all of the recombinant viruses yielded amounts of virus greater than or comparable to the amount for rWSN-HA-HK wt, with the exception of the HK T1562N mutant, which was significantly reduced in titer by 40% (Fig. 4). Relative yield corresponded with extent of infection for the P1621S and Q2101R mutants (P < 0.05). The significantly reduced yield of the recombinant T1562N mutant in mTECs relative to that in wt HK cells (P < 0.05) was complemented by the G2181W mutation (Fig. 4).
FIG. 4.
Yield of infectious virus from mTECs. Medium was collected following infection of mTECs with the recombinant viruses shown in Fig. 3. The infections were performed in duplicate, and titrations were performed in duplicate to derive average values ± standard deviations, which were calculated per ml of supernatant. The samples that showed significant differences compared to the wt are indicated with an asterisk (P < 0.05).
Differences in mouse lung replication, pH of fusion, and virulence of HA mutations.
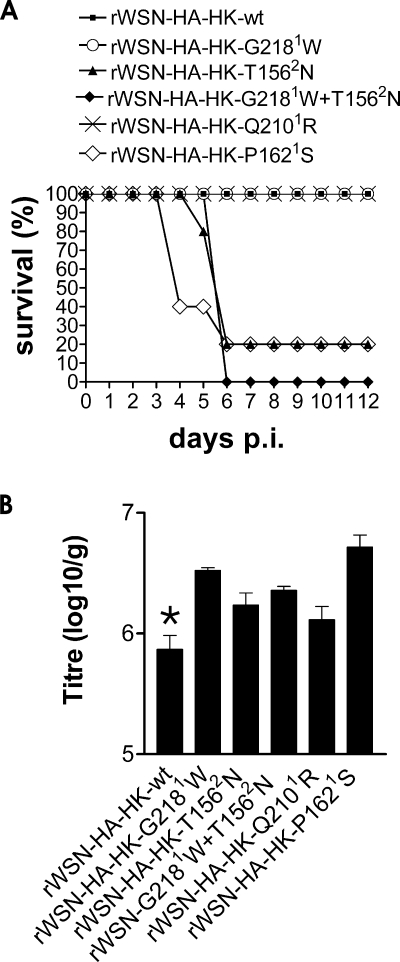
The same set of recombinant HA mutants were used to infect BALB/c mice to assess possible differences in virulence associated with these mutations. Infection of groups of five mice with 106 PFU of wt HK did not result in mortality, nor did infection with the recombinants possessing mutations G2181W and Q2101R, indicating that the lethal dose for these viruses was >106.5 PFU (Fig. 5A). In contrast, the recombinant viruses possessing the T1562N and P1621S mutations were both significantly increased in virulence, causing 80% mortality, and the G2181W+T1562N double mutant caused 100% mortality. The P1621S mutant demonstrated the shortest time to death, 4 days, relative to 6 days for both of the T1562N-containing mutants. The rWSN-HA-HK P1621S and G2181W+T1562N mutants did not kill at a 10-fold-reduced dose (not shown), and thus, these viruses possessed LD50s of 105.7 and 105.5 PFU, respectively. This indicated that the P1621S and T1562N mutations that reside in the HA1 and HA2 subunits increased virulence by >100.8- and >101.0-fold, respectively.
FIG. 5.
Lethal response and growth of recombinant viruses in mouse lungs. (A) Groups of five BALB/c mice were infected intranasally with 106 PFU each of the indicated recombinant viruses, and survival was monitored for 12 days. (B) Groups of three BALB/c mice were intranasally infected with 5 × 103 PFU of the recombinant viruses, and lungs were collected at 3 dpi for titration of infectious virus by a plaque assay. Values are shown as means with standard deviations, calculated per gram of lung tissue. All the mutants grew to significantly higher levels than the wt (indicated with an asterisk) (P < 0.05; t test).
The yields of infectious virus were measured on day 3 for groups of three mice infected intranasally with a low dose of 5 × 103 PFU of each of the recombinant viruses (Fig. 5B). All mutations demonstrated increased replication in the lung relative to rWSN-HK wt (P < 0.05; t test), further indicating the lung-adaptive nature of these mutations. Higher yields were associated with the most-virulent viruses that possessed the G2181W+T1562N and P1621S mutations as well as the G2181W mutant, which was not seen to detectably increase virulence on the HK-(HA+NA)/WSN backbone.
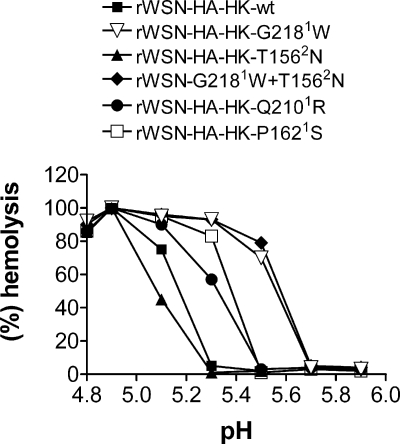
In addition to the role of HA mutations in mouse lung replication and virulence, we also demonstrated that the changes in optimal pH of fusion were a direct consequence of these HA mutations. Using the hemolysis assay, we showed that G2181W and G2181W+T1562N both possessed median pH-of-fusion values that were 0.4 units greater than those for wt HK, as previously seen for the MA viruses that possessed these mutations (Fig. 6). The recombinant Q2101R and P1621S mutants were also elevated in pH of fusion, by 0.15 and 0.2 pH units, respectively. However, the T1562N mutant was slightly reduced in pH of fusion, with a pH of 0.1. These data demonstrate that the mutations observed in MA mutants were associated with an elevated pH of fusion; however, the T1562N mutation did not increase fusion but did function to increase virulence, indicating that increased virulence does not require an increased pH of fusion. However the increased pHs of fusion of the Q2101R, P1621S, G2181W, and G2181W+T1562N mutants may contribute to the associated properties of increased virulence and/or replication.
FIG. 6.
pH dependence of fusion of recombinant viruses possessing mutant HA genes. The extent of hemolysis was measured at 0.2-pH increments for recombinant viruses possessing the mutations indicated in Fig. 5. The assays were performed in duplicate to obtain mean values.
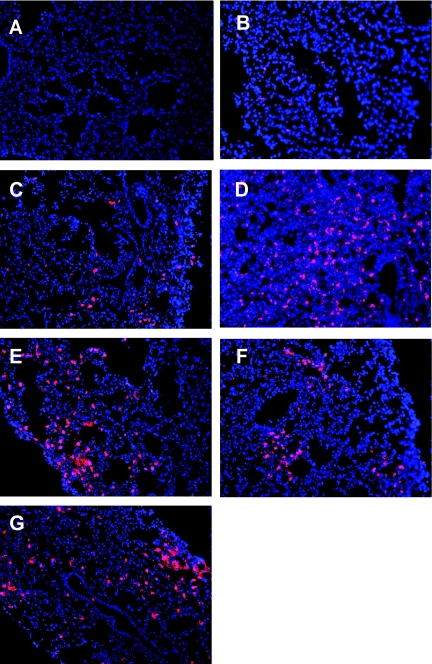
Immunofluorescent staining of mouse lungs.
The recombinant viruses were also used to infect BALB/c mice at 105 PFU for a qualitative assessment of lung infection at 2 dpi by florescent microscopy of frozen lung sections with anti-HK primary antibody (Fig. 7). Staining of the lung parenchyma showed that all the MA mutants increased the extent of infection of alveolar regions, where more and/or larger foci of infection were seen for all mutants than for the wt HK strain, which showed scattered infection of small foci of alveolar cells. Cross sections taken near the first major branch of the bronchus showed that whereas WSN-HA-HK wt infection resulted in small foci of infection in bronchiolar epithelia, all the rWSN-HA-HK mutant viruses (G2181W, T1562N, G2181W+T1562N, and P1621S) except Q2101R showed abilities to more extensively infect bronchiolar epithelia (data not shown). Both the HK T1562N and the HK P1621S mutations, which increased virulence, were also associated with the greatest extents of both bronchiolar and alveolar staining (Fig. 7 and data not shown).
FIG. 7.
Mouse-adaptive mutations increase immunofluorescent staining of alveoli in mouse lungs. BALB/c mice were infected with 105 PFU of the recombinant viruses containing mutations acquired after mouse passages. Viral antigen was detected by staining frozen lung sections with anti-HK primary antibody followed by Cy3-conjugated secondary antibody (red). Nuclei were stained with Hoechst (blue), and images were obtained using a 20× objective. Representative alveolar regions are shown for each sample. (A) PBS control. (B) rWSN-HA-HK wt. (C) rWSN-HA-HK G2181W. (D) rWSN-HA-HK T1562N. (E) rWSN-HA-HK G2181W+T1562N. (F) rWSN-HA-HK Q2101R. (G) rWSN-HA-HK P1621S.
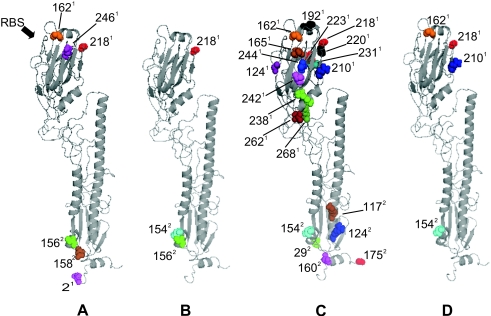
Location of mutations in the HA trimer after passages 12, 20, and 21.
Positioning of the human H3 mouse-adaptive mutations on the three-dimensional HA structure shows that they cluster in two regions that primarily involve sites of intersubunit contact on the left side relative to the exposed face of the HA monomer (shown in Fig. 8). The mutations observed in the initial longitudinal study of passage 12 and 20 populations were mapped separately (Fig. 8A and B, respectively) from those obtained in the subsequent series of 10 independent mouse passages (Fig. 8C), and in both cases, the same two HA subregions were identified. The convergent mutations seen among all mouse adaptation series at positions 162, 210, and 218 of HA1 and position 154 of HA2 identify the most-prevalent adaptive HA sites, which are shown in Fig. 8D.
FIG. 8.
Locations of the passage 12, 20, and 21 mutations within the HA trimer. The images were created with PyMOL software, using a monomer of the 1HGD H3 HA structure. The numbered locations of individual mutations are shown in space-filling models. (A) MA passage 12 mutations (from Table 1). (B) MA passage 20 mutations (from Table 1). (C) Total passage 21 mutations from 10 parallel studies (from Table 2). (D) Convergent mutations detected among independent studies (from Tables 1 and 2).
DISCUSSION
Mouse lung adaptive map.
The experimental mouse lung model of adaptation identified 27 mutations that were used to derive a functional genetic map of human H3 HA gene evolution in a novel host. The patterns of H3 gene variation were similar for longitudinal and parallel studies, both of which showed the selection of HA variants with mutations in two regions of the HA, one in HA1 and one in HA2. Most mutations in HA1 clustered around and behind the RBS and did not involve substitutions of amino acids in direct contact with SA. Functional mapping of a subset of convergent mutations by using reverse genetics demonstrated examples of increased ability to bind α2,3 SA and infect mouse tracheal and lung tissue types as well as increased virulence. These results indicated that multiple and different HA mutations were mouse adaptive, including the repeated selection of convergent mutations at HA1 positions 210, 218, and 162 as well as those affecting the HA2 154 glycosylation site, indicating that specific mutations were functionally dominant. Convergent mutations were observed in 8 of 11 independent mouse adaptation experiments, with the most prevalent mutations being observed at HA1 positions 210 and 218.
HA1 adaptive domain.
In general, mouse-selected mutations occurred in or near folds of the globular domains in each of the HA1 and HA2 subunits. The HA1 mutations primarily resided in the turns and loops of the globular, eight-stranded antiparallel beta barrel that supports the RBS and interfaces with adjacent subunits. Mutations most often involved the fifth beta strand at the innermost edge of the globular domain, which is packed at the central threefold axis within the strand (i.e., position 210) as well as the extending loop region (i.e., position 218), which interacts with adjacent subunits (30). As these mutations do not directly contact the SA in the RBS (30), it is proposed that these internal adaptive mutations affect the shape of the binding site by affecting the positions and/or orientations of the amino acids in the binding pocket to affect receptor specificity. Studies of the crystal structures of human A/HK/1/68 H3 and the possible avian precursor A/Duck/Ukraine/63 (H3N8) bound to receptors show that α2,3 SA avian-type RBSs are narrower than those that bind α2,6 SA (11). Mutational changes in the 1918 H1N1 influenza HA that function to increase α2,6 SA binding do not involve substitutions of amino acids in direct contact with SA but instead result in reorientations that allow binding to the larger α2,6 SA group (9). Substitutions of bulky or charged amino acids at internal positions of subunit contact, such as G2181W, G2181E, and Q2101R, may move the top of the HA1 subunit outward, buckling and thus narrowing the RBS cleft and increasing α2,3 SA binding. Contortion of HA structure would concomitantly decrease the pH stability, resulting in an increased pH threshold for fusion. This model is supported by studies of the G2181E H3 monoclonal antibody escape mutant that show altered antigenicity, increased pH of fusion, and increased α2,3 SA receptor binding, thus demonstrating effects on protein structure and function caused by this mutation (5). An elevated pH of fusion could increase the rate of uncoating and thus more rapidly establish infections, resulting in higher yields of virus. N-Acetyl modification of glucose at the third sugar of SLN is an important determinant of binding, and the mutations seen on mouse adaptation enhanced α2,3 SA binding, in part through contact with the adjacent sugars (8, 20).
HA2 adaptive domain.
The HA2 adaptive domain most often involved mutations in a short, outer-exposed, partially helical strand that lies across the five-stranded antiparallel beta barrel as well as mutations around the globular domain (30). Three mutations removed the NGT glycosylation site at position 154 (N1542S, N1542K, and T1562N), which could affect the structure, flexibility, and solvent exposure of this region. An additional two mutations of identical chemistry were located at positions D1582N and D1602N, further encompassing the HA2 helix loop region at positions 154 to 160 and thus defining an adaptive focus within the HA2 domain. Although the HA2 globular domain is primarily composed of HA2 beta strands, the central strand of the five-stranded barrel is composed of the amino-terminal region of HA1, which acquired a mutation at position 2 (D21Y), extending toward the membrane from this strand. Two other HA2 mutations were also observed to be near the membrane-proximal region below the HA2 globular domain (positions S292Y and G1752D) as well as above this domain (positions K1172R and R1242K). The removal of the HA2 glycosylation site at position 154 could possibly affect protease accessibility; however, neither HA cleavage (3) nor plaquing in the absence of trypsin (data not shown) was observed for the MA variants.
Cell tropism and pathogenicity.
There were different patterns of respiratory infection with respect to infection of tracheal and lung epithelia. The Q2101R and P1621S mutations showed the greatest effects in mTEC infection, with the G2181W, P1621S, and T1562N mutations demonstrating the most-enhanced lung infection. Whereas all four mutations increased the ability to infect or replicate in mTECs and lungs, only the P1621S and T1562N mutations demonstrated extensive alveolar and bronchiolar infection, which was associated with increased virulence. The rWSN backbone possessing the HK HA and NA genes was not sensitive enough to detect the influence on virulence of the other mouse-adaptive mutations.
The different patterns of infection among HA variants suggest that respiratory tropism and disease were the result of differences in ability to infect the distinct cell types that comprise the respiratory tract and furthermore suggest that the receptors on tracheal, bronchial, and alveolar epithelia are distinct. The data are consistent with increased lung replication due to a greater ability to infect more cells or a greater ability to yield infectious virus and the observation that mutants that combine both properties became dominant in the mouse lung. Virulence appears to be the function of relative abilities to replicate in alveolar and possibly bronchiolar tissues.
Although most of the MA variants had elevated pHs of fusion, the role of this property in virulence was not clear. The observation of increased virulence due to the T1562N mutation, which did not alter the pH of fusion, indicated that an increased pH of fusion was not required for increased virulence. Although it was possible that an increased pH of fusion contributes to virulence, it was not possible to ascertain the contribution of the increased pH of fusion relative to changes in other properties, such as receptor binding, for the increased replication in the mouse trachea and lung due to mutations Q2101R, P1621S, G2181W, and G2181W+T1562N. Future studies will analyze the role in virulence of HA mutations that affect the properties of either pH of fusion or receptor binding specificity but not both.
Mouse-adaptive regions are similar in avian and mammalian viruses.
Genetic studies of mutations that enhance the virulence of avian and mammalian H2, H3, and H5 viruses have implicated changes in the mouse-adaptive regions defined in this study. Comparison of human H3 with the closely related A/Duck/Ukraine/63 (H3N8) strain reveals mutations near mouse-adaptive changes in HA1 in the 190 helix (N193S) as well as in the HA2 adaptive region (D1322E, I1612V, and L1962F in HA2) that may contribute to human adaptation of avian H3 virus (Table 2) (11). The recent adaptation of equine H3N8 virus to dogs is associated with five HA mutations, which include the N1542T mutation in HA2 and the W2221L in HA1, and one of the five canine strains possessed a G2181E mutation (23). Thus, evolution of canine-adapted viruses was found to include mutations that were identical to or located at the same positions as mouse-adaptive mutations in both the HA1 and the HA2 mouse-adaptive regions.
In avian studies of the role of highly pathogenic avian H5N1 HA mutations in the control of virulence, mutations at positions E2161K and P2211S (H3 numbering) that were within or near the loop at positions 210 to 220 identified on mouse adaptation conferred higher virulence for chickens (13). The same E2161K mutation was also selected on mouse adaptation of H2 avian influenza and functioned to increase virulence (10). These observations suggest that the adaptive regions, identified here in the mouse, are shared among different HA subtypes, modulating the biological properties associated with changes in host range among different hosts.
Veracity of mouse-selected mutations.
The observed MA mutations were not the result of laboratory culture, because 10 subclones cultured from wt HK did not possess any HA-coding mutations. Nor were any of the 27 MA mutations (this study) seen in a panel of 19 H3 pH-of-fusion mutants (4). Nor were any of the mouse-selected mutations seen in a panel of H3 mutations selected by chicken allantoic cavity adaptation which included some mutations in similar locations (E1561K, S1591R, and N1931K) (Tables 1 and 2) (24). The distinctiveness of the egg-adapted map demonstrates that, whereas both chicken embryo and mouse lungs possess exclusively α2,3 SA receptors, there are differences in receptors between these hosts.
Conclusion.
Mouse-adaptive mutations selected under serial passage were multifunctional, changing the pH of fusion as well as the receptor specificity associated with enhanced tropism for mouse respiratory tissues. Our findings of adaptive regions in both the HA1 and the HA2 subunits, which enhance tropism and virulence, indicates that HA can modulate virulence in a manner that is receptor dependent as well as receptor independent. This study suggests that similar adaptive studies of human cells or other animal models with various influenza strains may provide further understanding of the evolutionary control of receptor binding and tissue tropism in different species.
Acknowledgments
The rWSN reverse genetics system was provided by Y. Kawaoka.
E.G.B. was funded by CIHR MOP 74526.
Footnotes
Published ahead of print on 1 October 2008.
REFERENCES
- 1.Auewarakul, P., O. Suptawiwat, A. Kongchanagul, C. Sangma, Y. Suzuki, K. Ungchusak, S. Louisirirotchanakul, H. Lerdsamran, P. Pooruk, A. Thitithanyanont, C. Pittayawonganon, C. T. Guo, H. Hiramatsu, W. Jampangern, S. Chunsutthiwat, and P. Puthavathana. 2007. An avian influenza H5N1 virus that binds to a human-type receptor. J. Virol. 819950-9955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown, E. G. 1990. Increased virulence of a mouse-adapted variant of influenza A/FM/1/47 virus is controlled by mutations in genome segments 4, 5, 7, and 8. J. Virol. 644523-4533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown, E. G., H. Liu, L. C. Kit, S. Baird, and M. Nesrallah. 2001. Pattern of mutation in the genome of influenza A virus on adaptation to increased virulence in the mouse lung: identification of functional themes. Proc. Natl. Acad. Sci. USA 986883-6888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daniels, R. S., J. C. Downie, A. J. Hay, M. Knossow, J. J. Skehel, M. L. Wang, and D. C. Wiley. 1985. Fusion mutants of the influenza-virus hemagglutinin glycoprotein. Cell 40431-439. [DOI] [PubMed] [Google Scholar]
- 5.Daniels, R. S., S. Jeffries, P. Yates, G. C. Schild, G. N. Rogers, J. C. Paulson, S. A. Wharton, A. R. Douglas, J. J. Skehel, and D. C. Wiley. 1987. The receptor-binding and membrane-fusion properties of influenza-virus variants selected using anti-hemagglutinin monoclonal-antibodies. EMBO J. 61459-1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Wit, E., and R. A. M. Fouchier. 2008. Emerging influenza. J. Clin. Virol. 411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gambaryan, A., A. Tuzikov, G. Pazynina, N. Bovin, A. Balish, and A. Klimov. 2006. Evolution of the receptor binding phenotype of influenza A (H5) viruses. Virology 344432-438. [DOI] [PubMed] [Google Scholar]
- 8.Gambaryan, A. S., A. B. Tuzikov, V. E. Piskarev, S. S. Yamnikova, D. K. Lvov, J. S. Robertson, N. V. Bovin, and M. N. Matrosovich. 1997. Specification of receptor-binding phenotypes of influenza virus isolates from different hosts using synthetic sialylglycopolymers: non-egg-adapted human H1 and H3 influenza A and influenza B viruses share a common high binding affinity for 6′-sialyl(N-acetyllactosamine). Virology 232345-350. [DOI] [PubMed] [Google Scholar]
- 9.Gamblin, S. J., L. F. Haire, R. J. Russell, D. J. Stevens, B. Xiao, Y. Ha, N. Vasisht, D. A. Steinhauer, R. S. Daniels, A. Elliot, D. C. Wiley, and J. J. Skehel. 2004. The structure and receptor binding properties of the 1918 influenza hemagglutinin. Science 3031838-1842. [DOI] [PubMed] [Google Scholar]
- 10.Govorkova, E. A., A. S. Gambaryan, E. C. J. Claas, and Y. A. Smirnov. 2000. Amino acid changes in the hemagglutinin and matrix proteins of influenza A (H2) viruses adapted to mice. Acta Virologica 44241-248. [PubMed] [Google Scholar]
- 11.Ha, Y., D. J. Stevens, J. J. Skehel, and D. C. Wiley. 2003. X-ray structure of the hemagglutinin of a potential H3 avian progenitor of the 1968 Hong Kong pandemic influenza virus. Virology 309209-218. [DOI] [PubMed] [Google Scholar]
- 12.Hartley, C. A., P. C. Reading, A. C. Ward, and E. M. Anders. 1997. Changes in the hemagglutinin molecule of influenza type A (H3N2) virus associated with increased virulence for mice. Arch. Virol. 14275-88. [DOI] [PubMed] [Google Scholar]
- 13.Hulse, D. J., R. G. Webster, R. J. Russell, and D. R. Perez. 2004. Molecular determinants within the surface proteins involved in the pathogenicity of H5N1 influenza viruses in chickens. J. Virol. 789954-9964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ibricevic, A., A. Pekosz, M. J. Walter, C. Newby, J. T. Battaile, E. G. Brown, M. J. Holtzman, and S. L. Brody. 2006. Influenza virus receptor specificity and cell tropism in mouse and human airway epithelial cells. J. Virol. 807469-7480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ito, T., J. N. Couceiro, S. Kelm, L. G. Baum, S. Krauss, M. R. Castrucci, I. Donatelli, H. Kida, J. C. Paulson, R. G. Webster, and Y. Kawaoka. 1998. Molecular basis for the generation in pigs of influenza A viruses with pandemic potential. J. Virol. 727367-7373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matrosovich, M., A. Tuzikov, N. Bovin, A. Gambaryan, A. Klimov, M. R. Castrucci, I. Donatelli, and Y. Kawaoka. 2000. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J. Virol. 748502-8512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matrosovich, M. N., A. S. Gambaryan, A. B. Tuzikov, N. E. Byramova, L. V. Mochalova, A. A. Golbraikh, M. D. Shenderovich, J. Finne, and N. V. Bovin. 1993. Probing of the receptor-binding sites of the H1 and H3 influenza A and influenza B virus hemagglutinins by synthetic and natural sialosides. Virology 196111-121. [DOI] [PubMed] [Google Scholar]
- 18.Matrosovich, M. N., T. Y. Matrosovich, T. Gray, N. A. Roberts, and H. D. Klenk. 2004. Human and avian influenza viruses target different cell types in cultures of human airway epithelium. Proc. Natl. Acad. Sci. USA 1014620-4624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller, J., and R. Ulrich. 2004. A computer program for Spearman-Karber and probit analysis of psychometric function data. Behav. Res. Methods Instrum. Comput. 3611-16. [DOI] [PubMed] [Google Scholar]
- 20.Mochalova, L., A. Gambaryan, J. Romanova, A. Tuzikov, A. Chinarev, D. Katinger, H. Katinger, A. Egorov, and N. Bovin. 2003. Receptor-binding properties of modern human influenza viruses primarily isolated in Vero and MDCK cells and chicken embryonated eggs. Virology 313473-480. [DOI] [PubMed] [Google Scholar]
- 21.Neumann, G., T. Watanabe, H. Ito, S. Watanabe, H. Goto, P. Gao, M. Hughes, D. R. Perez, R. Donis, E. Hoffmann, G. Hobom, and Y. Kawaoka. 1999. Generation of influenza A viruses entirely from cloned cDNAs. Proc. Natl. Acad. Sci. USA 969345-9350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pappas, C., P. V. Aguilar, C. F. Basler, A. Solorzano, H. Zeng, L. A. Perrone, P. Palese, A. Garcia-Sastre, J. M. Katz, and T. M. Tumpey. 2008. Single gene reassortants identify a critical role for PB1, HA, and NA in the high virulence of the 1918 pandemic influenza virus. Proc. Natl. Acad. Sci. USA 1053064-3069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Payungporn, S., P. C. Crawford, T. S. Kouo, L. M. Chen, J. Pompey, W. L. Castleman, E. J. Dubovi, J. M. Katz, and R. O. Donis. 2008. Influenza A virus (H3N8) in dogs with respiratory disease, Florida. Emerg. Infect. Dis. 14902-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robertson, J. S. 1993. Clinical influenza-virus and the embryonated hens egg. Rev. Med. Virol. 397-106. [Google Scholar]
- 25.Skehel, J. J., and D. C. Wiley. 2000. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu. Rev. Biochem. 69531-569. [DOI] [PubMed] [Google Scholar]
- 26.Smeenk, C. A., and E. G. Brown. 1994. The influenza virus variant A/FM/1/47-MA possesses single amino acid replacements in the hemagglutinin, controlling virulence, and in the matrix protein, controlling virulence as well as growth. J. Virol. 68530-534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smeenk, C. A., K. E. Wright, B. F. Burns, A. J. Thaker, and E. G. Brown. 1996. Mutations in the hemagglutinin and matrix genes of a virulent influenza virus variant, A/FM/1/47-MA, control different stages in pathogenesis. Virus Res. 4479-95. [DOI] [PubMed] [Google Scholar]
- 28.Vines, A., K. Wells, M. Matrosovich, M. R. Castrucci, T. Ito, and Y. Kawaoka. 1998. The role of influenza A virus hemagglutinin residues 226 and 228 in receptor specificity and host range restriction. J. Virol. 727626-7631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang, S., Q. Liu, J. Pu, Y. Li, L. Keleta, Y. W. Hu, J. Liu, and E. G. Brown. 2008. Simplified recombinational approach for influenza A virus reverse genetics. J. Virol. Methods 15174-78. [DOI] [PubMed] [Google Scholar]
- 30.Wiley, D. C., I. A. Wilson, and J. J. Skehel. 1981. Structural identification of the antibody-binding sites of Hong Kong influenza haemagglutinin and their involvement in antigenic variation. Nature 289373-378. [DOI] [PubMed] [Google Scholar]
- 31.Yamada, S., Y. Suzuki, T. Suzuki, M. Q. Le, C. A. Nidom, Y. Sakai-Tagawa, Y. Muramoto, M. Ito, M. Kiso, T. Horimoto, K. Shinya, T. Sawada, M. Kiso, T. Usui, T. Murata, Y. Lin, A. Hay, L. F. Haire, D. J. Stevens, R. J. Russell, S. J. Gamblin, J. J. Skehel, and Y. Kawaoka. 2006. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature 444378-382. [DOI] [PubMed] [Google Scholar]