Abstract
OBJECTIVE—Insulin resistance has been reported in up to 70% of women with polycystic ovary syndrome (PCOS). Physiologic and genetic data currently implicate post–insulin receptor signaling defects in substrates such as glycogen synthase kinase 3β (GSK3β). The AKT2 gene was chosen as a candidate for PCOS because its product affects glucose metabolism and mitogenic signaling, interacts with GSK3β, and mediates cell survival in the ovary.
RESEARCH DESIGN AND METHODS—Subjects were recruited from the reproductive endocrinology clinic at the University of Alabama at Birmingham, and control subjects were recruited from the surrounding community; 287 white women with PCOS and 187 white control subjects were genotyped for four single nucleotide polymorphisms (SNPs) in AKT2. Genotyping took place at Cedars-Sinai Medical Center in Los Angeles. SNPs and haplotypes were tested for association with PCOS risk and phenotypic markers of PCOS.
RESULTS—Minor allele carriers of SNPs rs3730051 and rs8100018 had increased odds of PCOS (odds ratio [OR] 2.2, P = 0.004, and 2.4, P = 0.001, respectively). The haplotype T-G-C-T was significantly associated with PCOS (OR 2.0, P = 0.01). Carriers of the risk haplotypes for both AKT2 and GSK3B had a further increased odds of PCOS (OR 3.1, P = 0.005).
CONCLUSIONS—These data suggest that polymorphisms in two components of the insulin signaling pathway, AKT2 and GSK3B, are associated with PCOS. The presence of multiple lesions in a single pathway may confer increased risk.
Polycystic ovary syndrome (PCOS), characterized by hyperandrogenism, oligo-ovulation, and polycystic ovarian morphology, affects 7% of women (1). Inherent in PCOS is a profound peripheral insulin resistance, observed in up to 70% of women with PCOS (2). The molecular basis of this intrinsic resistance remains unknown, but postinsulin receptor defects appear to contribute to the pathophysiology of both insulin resistance and hyperandrogenemia (2).
The insulin signaling pathway includes two main pathways: a metabolic arm through the activation of phosphatidylinositol 3-kinase (PI3K) and a mitogenic arm acting via mitogen-activated protein kinase (3). The expression and activity of downstream targets of PI3K have been investigated in PCOS tissues, with distinct molecular defects in post–insulin receptor signaling identified in fibroblasts and adipose tissues of women with PCOS (4).
Akt, also known as protein kinase B, participates in insulin signaling via activation by 3′-phosphoinositide–dependent kinase, which is activated by the product of PI3K, phosphatidylinositol 3,4,5-trisphosphate (5). Three highly conserved genes encode the forms of Akt, Akt1, Akt2, and Akt3 (5). Akt2 is the major form involved in insulin signaling in adipose tissue and is required for net gain in surface GLUT4 in response to insulin signaling (6).
Akt2 is widely expressed and participates in insulin metabolism, mitogenic signaling, and apoptosis (5). Activation of Akt by insulin in adipocytes is reduced in type 2 diabetes (5), and experimental reduction of Akt2 leads to decreased insulin sensitivity and reduced glucose disposal (3), both of which are features of PCOS. Insulin-stimulated Akt phosphorylation is reduced by 40–60% in PCOS skeletal muscle compared with matched control muscle (7).
In response to insulin signaling, Akt2 phosphorylates and inhibits glycogen synthase kinase 3β (GSK3β), which facilitates glycogen synthesis (8). Physiological data indicate that insulin-stimulated glycogen synthesis is impaired in PCOS fibroblasts (9) and cultured ovarian granulosa cells (10). In PCOS adipocytes, GSK3β tyrosine phosphorylation is increased and insulin-stimulated serine phosphorylation is decreased (11), which could result in an overactive GSK3β that is less able to be suppressed by insulin, possibly explaining impaired insulin-stimulated glycogen synthesis. Aberrant GSK3β expression and activity has also been reported in PCOS ovarian theca, with overexpression of GSK3β stimulating 17α-hydroxylase activity of P450c17 (12). Based on these physiological data, we previously genotyped GSK3B for association between polymorphisms in the gene and PCOS and identified a risk haplotype (13).
In the current study, we continued this line of investigation by examining whether variants in AKT2 were associated with susceptibility to PCOS or the biochemical features of PCOS. Analysis revealed associations between the minor allele of two single nucleotide polymorphisms (SNPs) from AKT2 and PCOS susceptibility. The presence of these alleles in a haplotype spanning the AKT2 gene region was also associated with PCOS.
RESEARCH DESIGN AND METHODS
Subjects and phenotyping
A total of 287 consecutive unrelated white patients with PCOS and 187 unrelated white control women were recruited from the Birmingham, Alabama, area. Case patients were recruited from the reproductive endocrine practice of one of the investigators (R.A.) at the University of Alabama at Birmingham. Participation in research was offered to patients meeting the inclusion criteria (being premenopausal and nonpregnant, having undergone no hormonal therapy [including oral contraceptives] for at least 3 months, and meeting the 1990 National Institutes of Health criteria for PCOS [14]). The comprehensive physical examination and hormonal evaluation used in our research have been described in detail previously (15).
Control subjects were healthy women, with regular menstrual cycles and no family history of hirsutism. These women had no hirsutism, acne, alopecia, or endocrine dysfunction and had not undergone hormonal therapy (including oral contraceptives) for at least 3 months before testing. Control subjects were recruited by word of mouth and advertisements in the Birmingham, Alabama, area through a call for “healthy women” without detailing the nature of the studies.
All subjects gave written informed consent. The study was performed according to the guidelines of the institutional review boards of the University of Alabama at Birmingham and Cedars-Sinai Medical Center.
SNP genotyping and haplotype determination
We selected four SNPs (rs11671439, rs8100018, rs3730051, and rs2304188) that span the 51.5-kb genomic length of AKT2 at chromosome 19q13.1–13.2. These were selected because they are predicted to tag the haplotypes (across the entire gene, plus 10 kb upstream and 10 kb downstream) occurring at >1% frequency in the Caucasian population of the HapMap database (16). The four SNPs were genotyped using the 5′-exonuclease assay (TaqMan MGB; Applied Biosystems, Foster City, CA) (17); duplicate genotyping of 96 samples for one SNP yielded 100% concordance. The genotyping success rate was 92.5%.
Haploview 3 (18) was used to determine haplotypes as well as haplotype blocks, with an accelerated expectation maximization algorithm. Haploview was also used to calculate linkage disequilibrium (LD) (the D′ statistic) between each pairwise combination of all the SNPs. Haplotypes were assigned to individual subjects only when the assignment could be made with >95% certainty.
Statistical analysis
Unpaired t tests and χ2 tests were used to compare clinical characteristics between women with and without PCOS; quantitative trait values were log- or square root–transformed as appropriate to reduce non-normality.
Association of SNPs or haplotypes with presence or absence of PCOS was evaluated using logistic regression, with adjustment for BMI and age in every analysis. ANCOVA was used for association between genotype and quantitative traits, again with adjustment for age and BMI. Significance was taken at P < 0.017 to account for the effects of multiple testing, considering that we analyzed one LD group of SNPs against three families of traits (PCOS diagnosis, androgens, and metabolic traits), yielding a correction factor of 3 (i.e., three independent comparisons).
In exploratory analyses, various multiple logistic regression models were used to explore the contribution of AKT2 haplotype to PCOS risk while simultaneously considering the risk haplotype from GSK3B (13). Analyses were performed with Statview 5.0 (SAS Institute, Cary, NC).
RESULTS
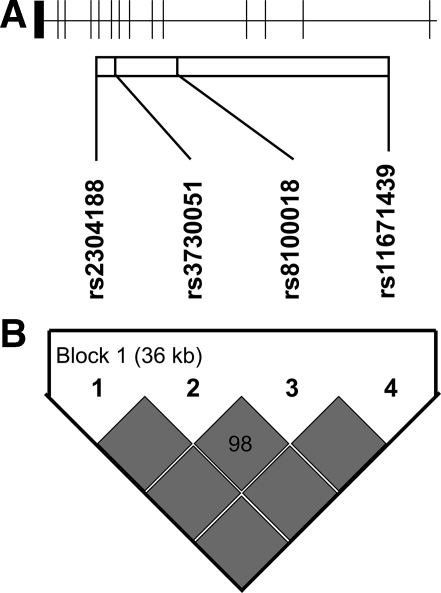
Clinical features of the cohort are given in Table 1. Strong LD (D′ ≥0.95) was observed among each of the four AKT2 SNPs (Table 2, Fig. 1). Minor allele carriers of two SNPs had an increased frequency of PCOS. The presence of the G allele at rs8100018 conferred an odds ratio (OR) of 2.4 (95% CI 1.4–4.1, P = 0.001), whereas the presence of the G allele at rs3730051 conferred an OR of 2.2 (95% CI 1.3–3.7, P = 0.004). There were no significant associations with any quantitative traits.
Table 1.
Clinical features of women with PCOS and control subjects
| Control | PCOS | |
|---|---|---|
| n | 187 | 287 |
| Age (years) | 33.0 (17.0) | 27.5 (11.5)* |
| BMI (kg/m2) | 24.1 (6.4) | 34.7 (13.5)* |
| WHR | 0.78 (0.08) | 0.83 (0.10)* |
| mFG score | 0 (0) | 7.0 (5.0)* |
| Hirsute (%) | 0 | 73.9* |
| Total testosterone (nmol/l) | 1.42 (0.92) | 2.77 (1.07)* |
| Free testosterone (pmol/l) | 12.1 (9.0) | 29.1 (16.3)* |
| DHEAS (μmol/l) | 2.58 (2.03) | 5.66 (4.61)* |
| SHBG (nmol/l)† | 220.0 (120.0) | 150.0 (70.0)* |
| Insulin (pmol/l) | 49.5 (45.9) | 129.15 (129.2)* |
| Glucose (mmol/l) | 4.77 (0.56) | 4.77 (0.72) |
| HOMA-IR | 0.92 (0.83) | 2.29 (1.93)* |
| HOMA-%B | 103.9 (59.5) | 175.3 (99.3)* |
Data are median (interquartile range).
P < 0.001 compared with control group.
SHBG activity was measured by competitive binding analysis using Sephadex G-25 and [3H]testosterone as the ligand; this assay gives values of approximately 100–300 nmol/l in normal adult women. DHEAS, dehydroepiandrosterone sulfate; HOMA-%B, β-cell function estimated by the homeostasis model assessment; HOMA-IR, insulin resistance estimated by the homeostasis model assessment; mFG score, modified Ferriman-Gallwey hirsutism score; SHBG, sex hormone–binding globulin; WHR, waist-to-hip ratio.
Table 2.
SNP location and frequency data
| Variant | Location | Alleles (major/minor) | Overall MAF | PCOS MAF | Control MAF |
|---|---|---|---|---|---|
| rs11671439 | Intron 1 | C/T | 0.078 | 0.068 | 0.088 |
| rs8100018 | Intron 4 | C/G | 0.262 | 0.296 | 0.216 |
| rs3730051 | Intron 8 | A/G | 0.221 | 0.247 | 0.180 |
| rs2304188 | Intron 10 | C/T | 0.153 | 0.141 | 0.178 |
MAF, minor allele frequency.
Figure 1.
Gene structure and LD plot for AKT2. A: The gene structure of AKT2 is shown; the gene has 14 exons and is located on the reverse strand of chromosome 19q13. The locations of the genotyped SNPs relative to the exons are indicated. B: The LD plot displays D′ values (percent) for each pair of SNPs in the box at the intersection of the diagonals from each SNP. D′ between each pair of SNPs was 1.0 (solid boxes) and was 0.98 between rs3730051 and rs8100018, indicating strong LD across the region.
Five haplotypes, comprising SNPs rs11671439, rs8100018, rs3730051, and rs2304188, accounted for >99% of the population (Table 3). There was a significant association between haplotype T-G-C-T and PCOS (OR 2.0, 95% CI 1.1–3.4, P = 0.01). This haplotype includes the minor alleles of both rs8100018 and rs3730051, the two SNPs associated with PCOS. There were no significant associations between haplotypes and any quantitative traits.
Table 3.
Haplotype frequency data in the women with PCOS and control subjects
| Haplotype | Overall frequency | PCOS frequency | Control frequency |
|---|---|---|---|
| T-A-G-T | 0.504 | 0.497 | 0.517 |
| T-G-C-T | 0.216 | 0.240 | 0.176 |
| C-A-G-T | 0.154 | 0.138 | 0.181 |
| T-A-G-C | 0.075 | 0.067 | 0.088 |
| T-A-C-T | 0.047 | 0.053 | 0.037 |
GSK3B was previously analyzed for association with PCOS susceptibility (13). The nine-SNP haplotype C-A-C-C-G-G-A-G-G was significantly associated with PCOS (OR 1.7, 95% CI 1.03–2.85, P = 0.028) and was the most common haplotype among the white subjects with PCOS but the second most common in control subjects. Taking into account the previous association between GSK3B haplotype and PCOS, we conducted exploratory analyses with a set of logistic regression models that simultaneously considered AKT2 and GSK3B (Table 4). The first model was designed to evaluate the independence of the risk haplotypes of both AKT2 and GSK3B on PCOS susceptibility. In this model, each risk haplotype retained a significant association with PCOS (AKT2 risk haplotype carriers, OR 2.1, P = 0.01; GSK3B risk haplotype carriers OR 1.8, P = 0.036), demonstrating independence. In the next logistic regression with PCOS as the dependent variable, the independent variables were age, BMI, and number of risk haplotypes (for each subject, ranging from 0 to 4). This analysis revealed that each additional risk haplotype conferred a 58% increase in the odds of PCOS (P = 0.01). In the final combined model, carriers of both risk haplotypes had an increased odds of PCOS compared with subjects with neither haplotype (OR 3.1, P = 0.005).
Table 4.
Logistic regression models simultaneously considering AKT2 and GSK3B in PCOS risk
| Model | Independent variables | OR (95% CI) | P value |
|---|---|---|---|
| Independence | Carrier state (Y/N) for AKT2 risk haplotype* | 2.10 (1.2–3.7) | 0.010 |
| Carrier state (Y/N) for GSK3B risk haplotype* | 1.80 (1.0–3.1) | 0.036 | |
| Additive | Number of AKT2 or GSK3B risk haplotypes† | 1.58 (1.1–2.2) | 0.010 |
| Combined | Carrier state (Y/N) for both risk haplotypes in AKT2 and GSK3B‡ | 3.11 (1.4–6.9) | 0.0050 |
PCOS diagnosis was the dependent variable in all models. Each analysis also included age and BMI as independent variables.
Carriers are homozygous or heterozygous for risk haplotype (T-G-C-T in AKT2 and C-A-C-C-G-G-A-G-G in GSK3B).
Number of risk haplotypes per individual is 0–4.
Compares subjects who are carriers of at least one AKT2 risk haplotype and at least one GSK3B risk haplotype to all other subjects.
CONCLUSIONS
Our data demonstrate that polymorphisms in the AKT2 gene are significantly associated with PCOS. The minor alleles of rs3730051 and rs8100018 were associated with PCOS, and the corresponding haplotype was also associated with PCOS. We used independent, additive, and combined logistic regression models to demonstrate that the association between AKT2 haplotype T-G-C-T and PCOS was independent of the GSK3B risk haplotype, but PCOS risk was increased when both were present. These data offer two potential susceptibility loci from the insulin signaling pathway that may confer increased PCOS risk and suggest that the presence of multiple lesions in a single pathway confers increased risk.
The significant association of rs3735001 and rs8100018 with PCOS extends to a haplotype that includes the minor alleles of these two AKT2 SNPs. Carriers of both minor alleles, in a haplotype, had the same OR as carriers of either risk allele alone, as a SNP. This finding suggests that these alleles are markers tagging the same variant in the gene region. The unknown functional variant can be a coding variant or a noncoding variant that alters AKT2 promoter activity or mRNA transport and stability, resulting in changes in protein expression.
Our analyses did not show any significant associations with quantitative traits related to glucose homeostasis. This was also the case for GSK3B (13). Because analyses to detect association between quantitative traits and genotype are conducted only within women with PCOS, the reduced sample may have decreased power to detect an effect. Also, in our cohort insulin resistance was quantified via homeostatic model assessment, which may be insufficiently reflective of insulin resistance to allow detection of association with genetic variants. Analysis in a larger cohort or one characterized by physiological studies (e.g., euglycemic clamp) would be necessary to definitively rule out whether there is an association of AKT2 variants with insulin resistance and whether such a relationship mediates the effect of genetic variants on PCOS risk. Alternatively, whereas Akt2 and GSK3β are best known for their role in glucose uptake (5), it is possible that their role in PCOS does not manifest as an alteration in androgen levels or metabolic disturbance, but in other pathways not reflected in typical quantitative traits. Akt is known to participate in several pathways including inflammation, lipogenesis, and endothelial function (5), and it is possible that aberrant function in these pathways contributes to the pathophysiology of PCOS.
Akt is expressed in granulosa and theca cells of primordial follicles and is involved in signal transduction, cell cycle, and cell fate (19,20). Recent studies have shown altered rates of apoptosis in PCOS ovarian tissue including granulosa (21) and theca (22). Overexpression of Akt2 has been shown to result in a reduced rate of apoptosis in a number of cell types including ovary (5) and is a potential causal factor in the increased follicular growth and lack of atresia associated with PCOS. Aberrant Akt2 and GSK3β expression and activation could result in increased cell survival in PCOS follicles and contribute to the theca cell hypertrophy and abnormal follicular development and promote the proliferation of granulosa. An increase in the latter less proliferative and highly steroidogenic cell type (23) could potentially increase androgen production by the ovary, a characteristic of PCOS. Increased basal, luteinizing hormone- and insulin-stimulated Akt phosphorylation has been reported in PCOS ovarian theca (22), with a subsequent increase in levels of aromatase and luteinizing hormone receptor mRNA expression (20), resulting in stimulation of granulosa cell proliferation. Increased serine and tyrosine phosphorylation of Akt in the ovary has been demonstrated in an animal model exhibiting PCOS-like symptoms (24).
We have performed a number of genetic association studies in this cohort. Each report represented a separate genotyping experiment performed over the past several years, testing an independent hypothesis; therefore, each was analyzed separately. We have published a positive association of variants in six genes with PCOS (supplemental Table A1, available in an online appendix at http://dx.doi.org/10.2337/dc08-0532). To assess the independence of these associations and their relative significance, we conducted a logistic regression simultaneously analyzing all of the associated variants, with PCOS status as the dependent variable (supplemental Table A2). This joint analysis revealed that the variants most significantly associated with PCOS were the AKT2 and GSK3B risk haplotypes.
Two AKT2 SNPs and the haplotype characterized by them were significantly associated with an increased odds of PCOS. Genes with pleiotropic effects are sensible candidates for PCOS, a syndrome characterized by dysfunction in multiple systems. AKT2 is expressed in several key PCOS tissues including adipose tissue, pancreas, and ovary and has a potential role in the regulation of insulin signaling and glucose uptake, insulin secretion, and cell proliferation in the ovary, all of which may be deranged in PCOS (1). By examining multiple members of a pathway that has been previously implicated in both the genetics (13) and physiology (11) of PCOS, we have demonstrated that the presence of variants in multiple members of a single pathway may increase PCOS susceptibility.
Supplementary Material
Acknowledgments
This study was supported in part by National Institutes of Health Grants R01-HD29364 and K24-HD01346 (to R.A.) and M01-RR00425 (General Clinical Research Center Grant from the National Center for Research Resources) and by an endowment from the Helping Hand of Los Angeles, Inc.
Parts of this study were presented in abstract form at the 88th annual meeting of the Endocrine Society, Boston, Massachusetts, 24–27 June 2006.
Published ahead of print at http://care.diabetesjournals.org on 3 September.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Goodarzi MO, Azziz R: Diagnosis, epidemiology, and genetics of the polycystic ovary syndrome. Best Pract Res Clin Endocrinol Metab 20:193–205, 2006 [DOI] [PubMed] [Google Scholar]
- 2.Carmina E, Lobo RA: Use of fasting blood to assess the prevalence of insulin resistance in women with polycystic ovary syndrome. Fertil Steril 82:661–665, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Chang L, Chiang SH, Saltiel AR: Insulin signaling and the regulation of glucose transport. Mol Med 10:65–71, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diamanti-Kandarakis E, Papavassiliou AG: Molecular mechanisms of insulin resistance in polycystic ovary syndrome. Trends Mol Med 12:324–332, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Vanhaesebroeck B, Alessi DR: The PI3K-PDK1 connection: more than just a road to PKB. Biochem J 346 (Pt. 3):561–576, 2000 [PMC free article] [PubMed]
- 6.Ishiki M, Klip A: Minireview: Recent developments in the regulation of glucose transporter-4 traffic: new signals, locations, and partners. Endocrinology 146:5071–5078, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Hojlund K, Glintborg D, Andersen NR, et al.: Impaired insulin-stimulated phosphorylation of Akt and AS160 in skeletal muscle of women with polycystic ovary syndrome is reversed by pioglitazone treatment. Diabetes 57:357–366, 2008 [DOI] [PubMed] [Google Scholar]
- 8.Hajduch E, Litherland GJ, Hundal HS: Protein kinase B (PKB/Akt)—a key regulator of glucose transport? FEBS Lett 492:199–203, 2001 [DOI] [PubMed] [Google Scholar]
- 9.Book CB, Dunaif A: Selective insulin resistance in the polycystic ovary syndrome. J Clin Endocrinol Metab 84:3110–3116, 1999 [DOI] [PubMed] [Google Scholar]
- 10.Wu XK, Zhou SY, Jiu JX, et al.: Selective ovary resistance to insulin signalling in women with polycystic ovary syndrome. Fertil Steril 80:954–965, 2003 [DOI] [PubMed] [Google Scholar]
- 11.Chang W, Goodarzi MO, Williams H, et al.: Adipocytes from women with polycystic ovary syndrome demonstrate altered phosphorylation and activity of glycogen synthase kinase 3. Fertil Steril. In press [DOI] [PMC free article] [PubMed]
- 12.Munir I, Geller DH, deBruin CE, et al.: Dysregulation of GSK3B activity in polycystic ovarian syndrome (PCOS) theca: a mechanism to promote excessive androgen biosynthesis in PCOS (Abstract). In Proceedings of the 88th Annual Meeting of the Endocrine Society, Boston, MA, 2006. Washington, DC, Endocrine Society.
- 13.Goodarzi MO, Antoine HJ, Pall M, et al.: Preliminary evidence of glycogen synthase kinase 3β as a genetic determinant of polycystic ovary syndrome. Fertil Steril 87:1473–1476, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zawadzki J, Dunaif A: Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. In Polycystic Ovary Syndrome. Dunaif A, Givens JR, Haseltine FP, Merriam GR, Eds. Boston, Blackwell Scientific, 1992, p. 377–384
- 15.Azziz R, Woods KS, et al.: The prevalence and features of the polycystic ovary syndrome in an unselected population. J Clin Endocrinol Metab 89:2745–2749, 2004 [DOI] [PubMed] [Google Scholar]
- 16.The International HapMap Consortium: The International HapMap Project. Nature 426:789–796, 2003 [DOI] [PubMed] [Google Scholar]
- 17.Livak KJ: SNP genotyping by the 5′-nuclease reaction. Methods Mol Biol 212:129–147, 2003 [DOI] [PubMed] [Google Scholar]
- 18.Barrett JC, Fry B, Maller J, et al.: Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 21:263–265, 2005 [DOI] [PubMed] [Google Scholar]
- 19.Carvalho CR, Carvalheira JB, Lima MH, et al.: Novel signal transduction pathway for luteinizing hormone and its interaction with insulin: activation of Janus kinase/signal transducer and activator of transcription and phosphoinositol 3-kinase/Akt pathways. Endocrinology 144:638–647, 2003 [DOI] [PubMed] [Google Scholar]
- 20.Zeleznik AJ, Saxena D, Little-Ihrig L: Protein kinase B is obligatory for follicle-stimulating hormone-induced granulosa cell differentiation. Endocrinology 144:3985–3994, 2003 [DOI] [PubMed] [Google Scholar]
- 21.Das M, Djahanbakhch O, Hacihanefioglu B, et al.: Granulosa cell survival and proliferation are altered in polycystic ovary syndrome. J Clin Endocrinol Metab 93:881–887, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wood JR, Nelson-Degrave VL, Jansen E, et al.: Valproate-induced alterations in human theca cell gene expression: clues to the association between valproate use and metabolic side effects. Physiol Genomics 20:233–243, 2005 [DOI] [PubMed] [Google Scholar]
- 23.Goto M, Iwase A, Ando H, et al.: PTEN and Akt expression during growth of human ovarian follicles. J Assist Reprod Genet 24:541–546, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lima MH, Souza LC, Caperuto LC, et al.: Up-regulation of the phosphatidylinositol 3-kinase/protein kinase B pathway in the ovary of rats by chronic treatment with hCG and insulin. J Endocrinol 190:451–459, 2006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.