Abstract
A 6-month-old child developed cutaneous mucormycosis of the forearm 5 weeks after liver transplantation, which progressed to osteomyelitis of the proximal ulna. Aggressive treatment, which included serial radical debridements, intravenous administration of amphotericin B, and eventually split thickness skin graft coverage resulted in successful functional salvage of the forearm, wrist, and hand. Of the nine previously reported cases of mucormycosis affecting the forearm or hand in immunocompromised patients, all either required amputation of the hand or below elbow amputation, or resulted in the patient’s death. Definitive early diagnosis and serial radical debridements may allow salvage of a functional hand.
Keywords: Cutaneous mucormycosis, Forearm, Infection, Liver transplantation
Introduction
Mucormycosis is a very rare, fulminant opportunistic fungal infection caused by members of the class phycomycetes, which are ubiquitous soil saprophytes. Although rhinocerebral, pulmonary, and widely disseminated forms of the disease have been extensively reported, mucormycosis can affect the hand and upper extremity as a localized cutaneous infection through direct inoculation of spores [3]. Cutaneous mucormycosis can also occur as a secondary infection following skin injuries such as burns, lacerations, and at intravenous injection sites [5, 7]. Like its more devastating disseminated form, cutaneous mucormycosis tends to occur in debilitated or immunocompromised patients [2, 6, 9–11, 13–15, 18, 19], though it can be seen in immunocompetent patients following extensive wound contamination or farming injuries [15].
This case report describes a very young child immunosuppressed after liver transplantation who presented with a localized mucormycosis infection of the forearm, which progressed to osteomyelitis of the proximal ulna. Treatment consisted of serial radical surgical debridements, intravenous amphotericin B, and split thickness skin grafts, which resulted in successful salvage of a functional forearm, wrist, and hand. To our knowledge, this is the only case in the hand surgery literature documenting successful salvage of the upper extremity following mucormycosis infection of the forearm or hand in an immunocompromised patient. The nine previous cases involving the hand or forearm have necessitated either a below elbow amputation or amputation of the hand, or have resulted in death [2, 5, 7, 10, 11, 13, 15, 18, 19].
Case Report
A 6-month-old infant boy with a history of neonatal hepatitis underwent an allograft orthotopic liver transplantation. Following transplantation, the patient was started on immunosuppression with azathioprine and prednisone.
Approximately 1 month posttransplant, he developed an extensive area of necrosis over the left forearm, initially thought to be consistent with intravenous fluid infiltration. The area of necrosis extended from the volar aspect of the distal forearm to just distal to the olecranon. In spite of brisk capillary refill of the fingers, radial and ulnar pulses were difficult to palpate. The area of necrosis was surgically debrided on posttransplant day 35 (Fig. 1), and frozen section histology demonstrated broad, nonseptate branching hyphae consistent with mucormycosis (Fig. 2). The patient was started on intravenous amphotericin B. Azathioprine was discontinued, prednisone was decreased, and he was started on low-dose cyclosporine.
Figure 1.
Preoperatively the area of necrosis extended from the volar aspect of the distal forearm to just distal of the olecranon.
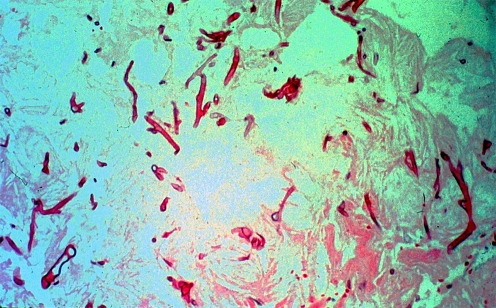
Figure 2.
Following surgical debridement of the necrotic areas, broad, nonseptate branching hyphae consistent with mucormycosis were identified on histologic examination.
On posttransplant day 37, the patient underwent a more radical debridement of the left forearm. A 1-cm margin of normal-appearing skin was excised all around the necrotic areas, and the forearm extensor muscles were carefully debrided until normal-appearing muscle fibers were visualized. The flexor digitorum superficialis and flexor carpi ulnaris muscles were radically excised leaving only the flexor carpi radialis, the flexor digitorum profundus, and the flexor pollicis longus muscle bellies, which appeared normal, as well as the median and ulnar nerves and the radial and ulnar arteries (Fig. 3). The proximal portion of the subcutaneous border of the ulna was exposed over a 2-cm distance just distal to the olecranon. This area of the ulna demonstrated radiographic findings suggestive of osteomyelitis, and this was subsequently confirmed histologically (Fig. 4). A window was created using a rongeur to remove the involved cortex of the ulna, and the medullary cavity was extensively curetted. Intraoperatively, excellent pulses were recorded using a Doppler probe from the radial and ulnar arteries. It was hypothesized that the necrotic muscles of the superficial flexor compartment of the forearm produced a compartment syndrome, thereby compromising the vascular supply to the hand.
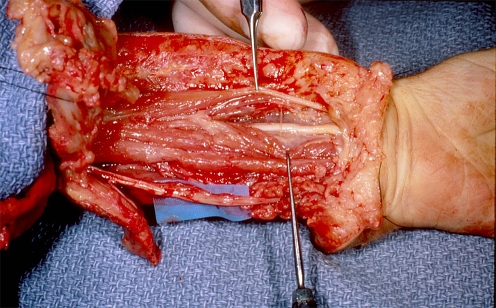
Figure 3.
A 1-cm margin of skin was excised around the necrotic areas. Following radical debridement of the forearm musculature, normal-appearing neurovascular structures were preserved.
Figure 4.
Radiographs of the forearm suggested osteomyelitis involving the proximal ulna and olecranon. These areas were extensively debrided on posttransplant day 37.
Following this radical surgical excision, frozen section analysis of the margins demonstrated no fungal elements in any of the skin or muscle margins. Pig skin allograft was used to provide temporary cover of the wound, even of the exposed medullary cavity of the ulna. On posttransplant day 43, multiple biopsies were again taken from all tissues of the left forearm. All the permanent sections were negative for mucormycosis. At the final fourth operation, the pig skin allograft was removed and a split thickness skin graft from the left thigh was applied to the wound (Fig. 5).
Figure 5.
After multiple biopsies confirmed the absence of any remaining infection, pig skin allograft was used to provide temporary coverage of the wound. This was subsequently replaced with a split thickness skin graft from the left thigh.
The child was allowed to begin unrestricted motion of the left upper extremity on posttransplant day 66, and amphotericin B was discontinued on posttransplant day 75. One year postoperatively, the child had excellent flexion and extension of his left elbow and wrist and could fully flex and extend his fingers and thumb. His liver function tests returned to normal.
Discussion
To our knowledge, 18 cases of cutaneous mucormycosis affecting the upper extremity have been described in the medical literature [2, 3, 5, 6, 9–11, 13, 15, 17–19] with 11 involving the forearm or hand and seven involving the upper arm. Nine of the 11 cases specifically involving the forearm or hand required a through or above-elbow amputation, and even then two of these patients died (Table 1) [2, 5, 10, 11, 13, 15, 17–19]. The remaining two patients underwent attempted salvage of the forearm and hand, but unfortunately one died [3]. All of the previous cases of mucormycosis affecting the upper extremity have been reported in adults with the single exception of a 12-year-old female reported in a series of immunocompetent patients afflicted with cutaneous mucormycosis [15].
Table 1.
Mucormycosis involving the upper extremity.
| No. | Age | Sex | Predisposing factors | Infection site | Treatment | Outcome | Reference |
|---|---|---|---|---|---|---|---|
| 1 | 79 | F | Diabetes mellitus | Right forearm | Excision | Died | Baker et al. [3] |
| 2 | 20 | M | Burn injury | Right hand | Through wrist amputation | Well | Foley and Shuck [5] |
| 3 | 41 | M | Crush injury, diabetes mellitus | Right hand | Index and middle finger ray amputations, amphotericin B | Well | Palmer et al. [17] |
| 4 | 39 | F | Chronic myelogenous leukemia, diabetes mellitus | Right upper arm | Excision, amphotericin B | Well | Jain et al. [9] |
| 5 | 80 | F | Prednisone therapy for polymyalgia rheumatica | Right upper arm | Excision, amphotericin B | Well | Hennessy and Mosher [6] |
| 6 | 56 | F | Hemodialysis for analgesic nephropathy | Right small finger | Below elbow amputation, amphotericin B | Well | Kerr et al. [10] |
| 7 | 15 | F | Acquired immunodeficiency syndrome (AIDS) | Left forearm | Through elbow amputation, amphotericin B | Well | Al-Qattan and Al Mazrou [2] |
| 8 | 37 | F | Diabetes mellitus, corticosteroid therapy for panhypopituitarism | Left hand | Above-elbow amputation, amphotericin B | Died | La Hausse-Brown et al. [11] |
| 9 | 28 | F | Burn injury, diabetes mellitus | Hand and forearm | Above-elbow amputation, amphotericin B | Well | Lidor and Nunley [13] |
| 10 | 52 | F | Diabetes mellitus | Right hand | Above-elbow amputation, amphotericin B | Well | Stevanovic et al. [19] |
| 11 | 12 | F | Motor vehicle injury, open fractures of humerus, radius, and ulna | Upper arm and forearm | Excision, amphotericin B | Well | Moran et al. [15] |
| 12 | 26 | M | Conveyor belt injury | Unknown | Excision, amphotericin B | Well | Moran et al. [15] |
| 13 | 28 | M | Motor vehicle injury, open fracture of humerus | Upper arm | Above-elbow amputation, amphotericin B | Well | Moran et al. [15] |
| 14 | 46 | M | Motor vehicle injury, open fractures of humerus, radial neck and olecranon | Upper arm and elbow | Glenohumeral disarticulation, amphotericin B | Well | Moran et al. [15] |
| 15 | 56 | F | Conveyor belt injury, open fractures of radius and ulna | Forearm | Excision, amphotericin B | Well | Moran et al. [15] |
| 16 | 52 | F | Conveyor belt injury, closed anterior elbow dislocation | Elbow | Ring and small finger ray amputations, amphotericin B | Well | Moran et al. [15] |
| 17 | 70 | M | Corn auger injury, open thumb dislocation | Hand | Below elbow amputation, amphotericin B | Well | Moran et al. [15] |
| 18 | 38 | F | Alcoholic encephalopathy | Left forearm | Below elbow amputation | Died | Raizman et al. [18] |
| 19 | 6 months | M | Immunosuppression for liver transplantation | Left forearm | Serial radical excisions, amphotericin B | Well | Present case |
Numbers 11 to 17 convey immunocompetent patients
Mucormycosis infection in all its forms is rarely reported in the absence of any immunodeficiency. Risk factors include diabetes mellitus [3, 7, 9, 11, 13, 17] hematologic malignancy [16], drug abuse [8], steroid use [6, 11], transplant recipients [4, 12, 20], burn injuries [5, 13], and hemodialysis [10]. Like this case, 11 of the other reported mucormycosis infections in the upper extremity were found to have associated risk factors. However, Moran et al. [15] presented a series of seven immunocompetent patients with mucormycosis infections following motor vehicle accidents with gross contamination or farming injuries. Despite the favorable immunologic status of these patients, multiple debridements were still necessary and four of the seven patients ultimately required some form of upper extremity amputation.
Successful treatment of cutaneous mucormycosis infections of the upper extremity depends upon three principles: early diagnosis, prompt administration of high-dose amphotericin B, and serial radical surgical resection with debridement of all necrotic tissues. In spite of appropriate management, the mortality rate for cutaneous mucormycosis has been reported to be up to 16% [1].
Early diagnosis of cutaneous mucormycosis is facilitated by having a high level of suspicion, particularly in susceptible patients who develop a necrotic area of their extremity. Prompt diagnosis is mandatory to ensure the patient’s best chance of survival. Clinically, cutaneous mucormycosis may initially present with pustules, blisters, bullae, and discoloration. Definitive diagnosis is made by histologic examination of a tissue biopsy demonstrating the characteristic hyphae. Intraoperative frozen sections should be considered to facilitate rapid identification of the offending organism and eventually to confirm clear margins.
Amphotericin B is the mainstay of medical treatment for cutaneous mucormycosis even though it may be limited by its adverse effects, which include hypokalemia, renal impairment, and infusion-related intolerance reaction [16]. It may complement surgical debridement by slowing the progression of spread of mucormycosis and by controlling infection in areas where vital structures cannot be completely resected.
Complete or serial radical debridement of all necrotic and infected tissues is unquestionably the single most important component of treatment. Since the fungus rapidly disseminates via the vasculature, a wide margin of resection must be employed. With deep infection or involvement of vital structures, partial or total amputation of the limb should be strongly considered. There has been only one other report of mucormycosis osteomyelitis of the hand, but this patient required above-elbow amputation [19]. Successful salvage of a functional hand was achieved in our patient despite osteomyelitis of the ulna by rapid diagnosis, intravenous amphotericin B, and serial radical debridements of the forearm followed by delayed reconstruction using skin grafts, but only after total eradication of the fungus from all the affected tissues—bone, muscle, and skin—had been confirmed by permanent sections.
References
- 1.Adam RD, Hunter G, DiTomasso J, et al. Mucormycosis: emerging prominence of cutaneous infections. Clin Infect Dis. 1994;19:67–76. [DOI] [PubMed]
- 2.Al-Qattan MM, Al Mazrou AM. Mucormycosis of the upper limb. J Hand Surg. 1996;21B:261–2. [DOI] [PubMed]
- 3.Baker RD, Seabury JH, Schneidau JD. Subcutaneous and cutaneous mucormycosis and subcutaneous phycomycosis. Lab Invest. 1962;11:1091–102. [PubMed]
- 4.Baraia J, Munoz P, Berdaldo de Quiros JC, et al. Cutaneous mucormycosis in a heart transplant patient associated with a peripheral catheter. Eur J Clin Microbiol Infect Dis. 1995;14:813–5. [DOI] [PubMed]
- 5.Foley FD, Shuck JM. Burn-wound infection with phycomycetes requiring amputation of hand. JAMA. 1968;203:596. [DOI] [PubMed]
- 6.Hennessy MJ, Mosher TF. Mucormycosis infection of an upper extremity. J Hand Surg. 1981;6A:249–52. [DOI] [PubMed]
- 7.Hopkins MA, Treloar DM. Mucormycosis in diabetes. Am J Crit Care. 1997;6:363. [PubMed]
- 8.Hopkins RJ, Rothman M, Fiore A, et al. Cerebral mucormycosis associated with intravenous drug use: three case reports and review. Clin Infect Dis. 1994;19:1133–7. [DOI] [PubMed]
- 9.Jain JK, Markowitz A, Khilanani PV, et al. Localized mucormycosis following intramuscular corticosteroid: case report and review of the literature. Am J Med Sci. 1978;275:209–16. [DOI] [PubMed]
- 10.Kerr PG, Turner H, Davidson A, et al. Zygomycosis requiring amputation of the hand: an isolated case in a patient receiving haemodialysis. Med J Aust. 1988;148:258–9. [DOI] [PubMed]
- 11.La Hausse-Brown TP, Suvarna SK, Brotherston TM. Fatal rhizopus infection in a hand. Br J Plast Surg. 1996;49:572–3. [DOI] [PubMed]
- 12.Leong KW, Crowley B, White B, et al. Cutaneous mucormycosis due to Absidia corymbifera occurring after bone marrow transplantation. Bone Marrow Transplant. 1997;19:513–5. [DOI] [PubMed]
- 13.Lidor C, Nunley JA. Mucormycosis of the hand and forearm. N Engl J Med. 1997;20:1511. [DOI] [PubMed]
- 14.Mizutari K, Nishimoto K, Ono T. Cutaneous mucormycosis. J Dermatol. 1999;26:174–7. [DOI] [PubMed]
- 15.Moran SL, Strickland J, Shin AY. Upper-extremity mucormycosis infections in immunocompetent patients. J Hand Surg. 2006;31A:1201–5. [DOI] [PubMed]
- 16.Pagano L, Offidani M, Fianchi L, et al. Mucormycosis in hematologic patients. Haematologica. 2004;89:207–14. [PubMed]
- 17.Palmer DL, Weitzner S, Simpson JC. Progressive gangrene of an extremity due to mucormycosis in a diabetic patient. Diabetes. 1970;19:881–3. [DOI] [PubMed]
- 18.Raizman NM, Parisien M, Grafe MW, et al. Mucormycosis of the upper extremity in a patient with alcoholic encephalopathy. J Hand Surg. 2007;32A:384–8. [DOI] [PubMed]
- 19.Stevanovic MV, Mirzayan R, Holtom PD, et al. Mucormycosis osteomyelitis in the hand. Orthopedics. 1999;22:449–50. [DOI] [PubMed]
- 20.Vainrub B, Macareno A, Mandel S, et al. Wound zygomycosis (mucormycosis) in otherwise healthy adults. Am J Med. 1988;84:546–8. [DOI] [PubMed]