Abstract
The lag screw technique has historically been a successful and accepted way to treat oblique metacarpal fractures. However, it does take additional time and involve multiple steps that can increase the risk of fracture propagation or comminution in the small hand bones of the hand. An alternate fixation technique uses bicortical interfragmentary screws. Other studies support the clinical effectiveness and ease of this technique. The purpose of this study is to biomechanically assess the strength of the bicortical interfragmentary screw versus that of the traditional lag screw. Using 48 cadaver metacarpals, oblique osteotomies were created and stabilized using one of four methods: 1.5 mm bicortical interfragmentary (IF) screw, 1.5 mm lag technique screw, 2.0 mm bicortical IF screw, or 2.0 mm lag technique screw. Biomechanical testing was performed to measure post cyclic displacement and load to failure. Data was analyzed using one-way analysis of variance (ANOVA). There was no significant difference among the fixation techniques with regard to both displacement and ultimate failure strength. There was a slight trend for a higher load to failure with the 2.0 mm IF screw and 2.0 mm lag screw compared to the 1.5 mm IF and 1.5 mm lag screws, but this was not significant. Our results support previously established clinical data that bicortical interfragmentary screw fixation is an effective treatment option for oblique metacarpal fractures. This technique has clinical importance because it is an option to appropriately stabilize the often small and difficult to control fracture fragments encountered in metacarpal fractures.
Keywords: Metacarpal fracture, Hand fracture, Metacarpal fixation, Screw fixation metacarpal fracture, Biomechanical metacarpal fracture
Introduction
The lag screw technique has historically been a successful and accepted way to treat oblique metacarpal fractures. The technique involves drilling a glide hole in the near cortex followed by a concentrically placed smaller hole in the far cortex for appropriate compressed fixation [11]. Compression occurs when the screw head abuts the near cortex and pulls the far fragment closer to it as the threads are advanced [11, 12]. Whereas this technique is a standard model of rigid fixation and primary bone healing, it does take additional time and involve multiple steps that, when used in the small bones of the hand, can increase the risk of fracture propagation or comminution [12].
Roth and Auerbach examined an alternate technique with bicortical interfragmentary screw fixation [12]. Thirty-seven patients with metacarpal and phalangeal fractures were treated with this method. Fracture fragment compression was initially achieved with a clamp and then maintained with bicortical screw purchase without additional compression by overdrilling. All patients began early range of motion protocols and all healed at an average of 7 weeks with no malunion or hardware failure. These results support the clinical effectiveness and highlight the desirable ease of this technique.
The purpose of this study is to assess, biomechanically, the strength of the bicortical interfragmentary screw versus that of the traditional lag screw. Our hypothesis is that there is no statistical difference between the two techniques.
Materials and Methods
Twelve cadaver hand specimens (six matched pairs) were used, providing 12 each of the second through fifth metacarpals. A total of 48 metacarpals were tested. All bones were radiographed to rule out any significant bony lesions or osteopenia. Using ordered randomization, each specimen was assigned to one of four testing groups (Fig. 1a and b, Table 1): 1.5 mm bicortical interfragmentary screw (1.5 IF), 1.5 mm lag technique screw (1.5 L), 2.0 mm bicortical interfragmentary screw (2.0 IF), or 2.0 lag technique screw (2.0 L). (Screws were made by Synthes [Paoli, PA, USA].)
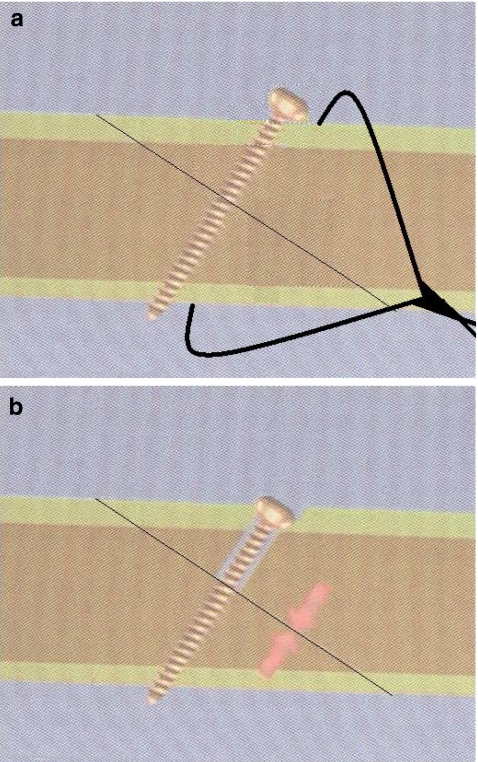
Figure 1.
a ‘Bicortical interfragmentary’ screws were placed after standard drilling whereas holding the fracture fragments compressed with a clamp. b ‘Lag technique’ screws were placed using standard lag technique: overdrilling near cortex and drilling far cortex.
Table 1.
Grouping of specific metacarpals into categories of fixation technique.
| 1.5 IF | 1.5 L | 2.0 IF | 2.0 L | Total | |
|---|---|---|---|---|---|
| Second metacarpal | 3 | 3 | 3 | 3 | 12 |
| Third metacarpal | 3 | 3 | 3 | 3 | 12 |
| Fourth metacarpal | 3 | 3 | 3 | 3 | 12 |
| Fifth metacarpal | 3 | 3 | 3 | 3 | 12 |
| Total | 12 | 12 | 12 | 12 | 48 |
1.5 IF: 1.5 mm bicortical interfragmentary screw, 1.5 L: 1. 5 mm lag technique screw, 2.0 IF: 2.0 mm bicortical interfragmentary screw, 2.0 L: 2.0 mm lag technique screw
Oblique, midshaft osteotomies were created 45° to the long axis in a dorsal distal to volar proximal orientation (Fig. 2). Osteotomies were stabilized as noted above, and the specimens were potted in a custom-fashioned aluminum jig with 5 min Epoxy™ (ITW Performance Polymers, Riviera Beach, FL, USA) (Fig. 2). Biomechanical testing was carried out on an Instron 4400 Universal Testing System (Instron, Canton, MA, USA). Axial loading and cantilever bending force vectors were resolved into a single 45° vector (Fig. 3a) and specimens loaded at 45° to the long axis (Fig. 3b). A 30-N load was selected based on previous assays and on the load that would likely need to be resisted for gentle range of motion [3, 10, 16]. Displacement was recorded after a 30-N preload and then after cyclic loading with 30 N at 0.1 mm/s for 400 cycles. Specimens were then tested to failure.
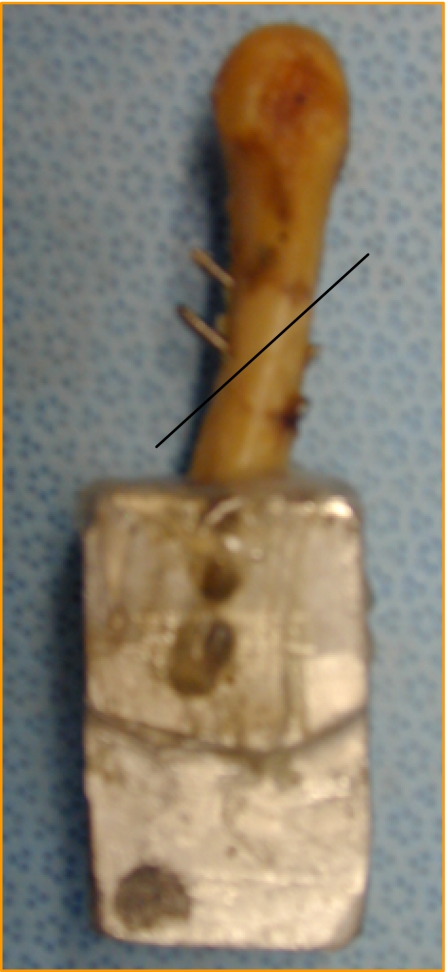
Figure 2.
Oblique, midshaft osteotomy made 45° to long axis.
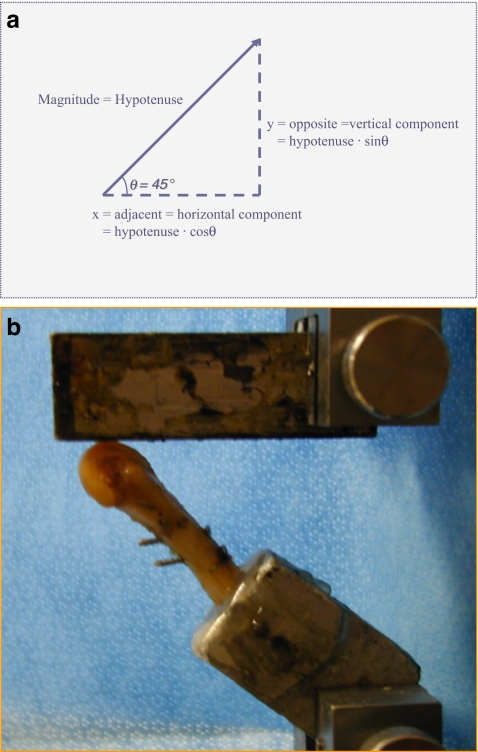
Figure 3.
a Axial loading and cantilever bending force vectors were resolved into single 45° vector. b Specimens loaded at 45° to the long axis.
Data was analyzed using one-way analysis of variance (ANOVA) and stratified by metacarpal type and by type of fixation technique. Statistical significance was defined as a P value <0.05.
Results
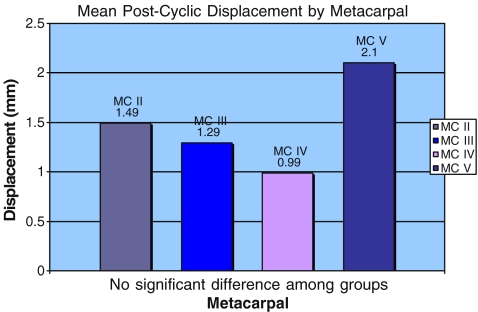
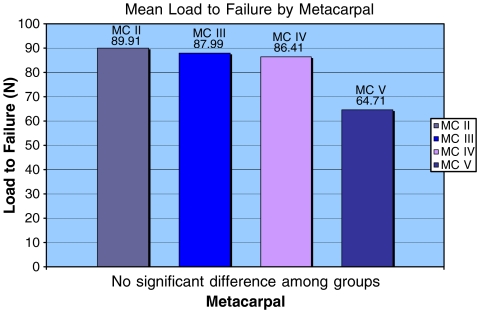
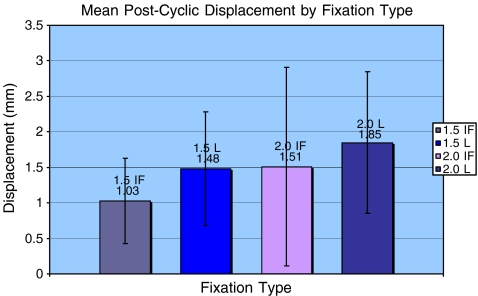
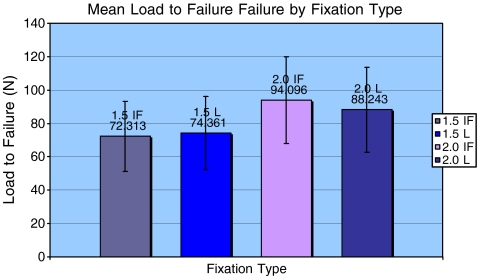
The values for average post cyclical displacement and load to failure are shown in Tables 2 and 3. There were no statistically significant differences among any of the tested groups. Data among metacarpal groups (II–V) and among fixation method (1.5 IF, 1.5 L, 2.0 IF, 2.0 L) were statistically similar (Figs. 4, 5, 6, and 7). There was a slight trend for a higher load to failure with the 2.0 IF and 2.0 L compared to the 1.5 IF and 1.5 L, but this was not significant. Thus, there was no statistically significant difference between screw size (1.5 or 2.0 mm) or fixation technique (lag or interfragmentary fixation with compression provided by bone reduction clamp).
Table 2.
Average post cyclical displacement and load to failure based on metacarpal.
| Metacarpal | Average post cyclic displacement (mm) | Average load to failure (N) |
|---|---|---|
| II | 1.49 | 89.91 |
| III | 1.29 | 87.99 |
| IV | 0.99 | 86.41 |
| V | 2.1 | 64.71 |
Table 3.
Average post cyclical displacement and load to failure based on fixation type.
| Fixation type | Average post cyclic displacement (mm) | Average load to failure (N) |
|---|---|---|
| 1.5 IF | 1.03 | 72.31 |
| 1.5 L | 1.48 | 74.36 |
| 2.0 IF | 1.51 | 94.1 |
| 2.0 L | 1.85 | 88.24 |
Figure 4.
Mean post cyclic displacement by metacarpal.
Figure 5.
Mean load to failure by metacarpal.
Figure 6.
Mean post cyclic displacement by fixation type.
Figure 7.
Mean load to failure by fixation type.
Discussion
Numerous studies, biomechanical and clinical, have been done in an effort to optimize treatment of unstable metacarpal fractures. The overall goal is to maintain sufficiently rigid fixation for bony union whereas allowing early motion to prevent stiffness and maximize function. Several biomechanical studies have been done to assess the relative strengths of various fixation methods of metacarpal fractures, including multiple K-wire, intramedullary and intraosseous wiring techniques, lag screws, and dorsal and lateral plating [1–9, 11, 13, 15, 16].
Vanik et al. tested human embalmed cadaver metacarpals [16]. Transverse osteotomies were created and fixed using 32 multiple fixation techniques (single to multiple sizes and configurations of K-wires and intraosseous wires, dorsal bone plates, and lateral bone plates). Constant bending forces were applied. They found that 26-gauge right angle intraosseous loops and dorsal bone plates were the strongest constructs and were comparable to each other. Black et al. also used a transverse osteotomy metacarpal model to assess torsion and bending rigidity and failure of five types of fixation [1]. Techniques included dorsal plating with and without lag screws, crossed K-wires, intraosseous wires and K-wires with intraosseous wires. Dorsal plating, with or without lag screws, was significantly more stable than the other fixation types. Prevel et al. performed biomechanical testing on fresh-frozen cadaver metacarpals with transverse osteotomies fixed with a combination of dorsal and lateral plates and 1.7 or 1.2 mm screws [9]. Three-point bending was applied to create apex dorsal and palmar loads. The 1.7-mm dorsal plate/screw configuration had the highest rigidity against apex dorsal loading.
Firoozbakhsh et al. tested metacarpals with oblique osteotomies stabilized with dorsal plating plus a lag screw, two interfragmentary lag screws, crossed K-wires, and paired and stacked intramedullary K-wires [3]. Construct strength was assessed with cyclical bending, torsional loading, and axial loading. The results showed that the initial rigidity of the dorsal plate was significantly higher than the two lag screws and the two lag screws significantly higher than the crossed K-wires in axial loading (but not bending or torsion). Fatigue strength followed the same order with dorsal plating highest, followed by the two lag screws, followed by the crossed K-wires. Variances in fracture models and biomechanical testing methods make it difficult to compare results among studies. In a subsequent study, Firoozbakhsh et al. used a similar model to test resistance to compressive and bending impact loading [4]. These results showed the two screws to be 59% weaker in compressive impact and 47% weaker in bending impact than dorsal plating.
Clinically, however, the strongest construct may not be the most desirable. Stern noted that plate fixation of metacarpal fractures is a “double edge sword” [14]. Dorsal plating with miniplate fixation does provide rigid fixation and has been used successfully in clinical application by allowing early range of motion and return to function [2, 5, 6]. However, it involves relatively significant soft tissue dissection and can be complicated by symptomatic hardware, tendon irritation, and stiffness and has complication rates reported as high as 35–45% [7, 8, 13, 15]. Furthermore, the strongest biomechanical construct may not be necessary in the clinical setting. As noted in the Roth study, clinical evaluation of the bicortical interfragmentary screw technique showed excellent results: 100% union at 7 weeks with no loss of fixation or malunion [12]. One hundred percent of the metacarpal fractures returned to full or near full motion.
We have identified certain limitations to our study. As our specimens were metacarpal bones stripped of all soft tissue, we could not simulate physiologic conditions (which allow for additional soft tissue support). However, without soft tissues, we created the most unstable construct and, therefore, were able to isolate fixation as the only variable being tested. Also, we did not include additional fixation groups, e.g., dorsal miniplates. However, with our available resources, we thought it necessary to test different screw diameters to get a more complete comparison between lagged and nonlagged screws and make additional comparisons using historic controls. Another limitation is the lack of a power analysis. We would certainly be able to more confidently reject a beta error had a power analysis been done. However, we initially elected not to perform one as there were more than the usual six specimens per group. And, our results are supported by the noted clinical data [12].
In conclusion, there was no significant biomechanical difference found between the four different fixation techniques with regard to both displacement and ultimate failure strength of the constructs. Thus, our current results support previously established clinical data that bicortical interfragmentary screw fixation is an effective treatment option for oblique metacarpal fractures. These results have clinical importance because they support being able to appropriately stabilize the often small and difficult to control fracture fragments encountered in metacarpal fractures.
References
- 1.Black D, Mann RJ, Constine R, Daniels AU. Comparison of internal fixation techniques in metacarpal fractures. J Hand Surg Am 1985;10(4):466–72. [DOI] [PubMed]
- 2.Bosscha K, Snellen JP. Internal fixation of metacarpal and phalangeal fractures with AO minifragment screws and plates: a prospective study. Injury 1993;24(3):166–8. [DOI] [PubMed]
- 3.Firoozbakhsh KK, Moneim MS, Howey T, Castaneda E, Pirela-Cruz MA. Comparative fatigue strengths and stabilities of metacarpal internal fixation techniques. J Hand Surg Am 1993;18(6):1059–68. [DOI] [PubMed]
- 4.Firoozbakhsh KK, Moneim MS, Doherty W, Naraghi FF. Internal fixation of oblique metacarpal fractures. A biomechanical evaluation by impact loading. Clin Orthop Relat Res 1996;325:296–301. [DOI] [PubMed]
- 5.Fischer KJ, Bastidas JA, Provenzano DA, Tomaino MM. Low-profile versus conventional metacarpal plating systems: a comparison of construct stiffness and strength. J Hand Surg Am 1999;24(5):928–34. [DOI] [PubMed]
- 6.Ford DJ, el-Hadidi S, Lunn PG, Burke FD. Fractures of the metacarpals: treatment by A. O. screw and plate fixation. J Hand Surg Br 1987;12(1):34–7. [DOI] [PubMed]
- 7.Fusetti C, Meyer H, Borisch N, Stern R, Santa DD, Papaloizos M. Complications of plate fixation in metacarpal fractures. J Trauma 2002;52(3):535–9. [DOI] [PubMed]
- 8.Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am 1998;23(5):827–32. [DOI] [PubMed]
- 9.Prevel CD, McCarty M, Katona T, Moore K, Jackson JR, Eppley BL, Sood R. Mini and micro plating of phalangeal and metacarpal fractures: a biomechanical study. J Hand Surg Am 1995;20(1):44–9. [DOI] [PubMed]
- 10.Putnam MD, Meyer NJ, Nelson EW, Greensway D, Lewis JL. Distal radial metaphyseal forces in an extrinsic grip model: implications for postfracture rehabilitation. J Hand Surg Am 2000;25(3):469–75. [DOI] [PubMed]
- 11.Rüedi TP, Murphy WM, Colton CL, et al. AO Principles of fracture management. Thieme: New York; 2000. Chapter 3.2.1.
- 12.Roth JJ, Auerbach DM. Fixation of hand fractures with bicortical screws. J Hand Surg Am 2005;30(1):151–3. [DOI] [PubMed]
- 13.Stern PJ, Wieser MJ, Reilly DG. Complications of plate fixation in the hand skeleton. Clin Orthop Relat Res 1987;214:59–65. [PubMed]
- 14.Stern PJ. Management of fractures of the hand over the last 25 years. J Hand Surg Am 2000;25(5):817–23. [DOI] [PubMed]
- 15.Trevisan C, Morganti A, Casiraghi A, Marinoni EC. Low-severity metacarpal and phalangeal fractures treated with miniature plates and screws. Arch Orthop Trauma Surg 2004;124(10):675–80. [DOI] [PubMed]
- 16.Vanik RK, Weber RC, Matloub HS, Sanger JR, Gingrass RP. The comparative strengths of internal fixation techniques. J Hand Surg Am 1984;9(2):216–21. [DOI] [PubMed]