Abstract
The literature suggests preoperative autologous blood donation in total joint arthroplasty is associated with increased overall transfusion rates compared with nondonation and is not cost-effective for all patients. We asked whether the amount of intraoperative blood loss and blood replacement differs between autologous donors and nondonors in elective spine surgery and whether the rates of allogeneic blood transfusions differ between the two groups; we then determined the cost of wasted predonated units. We retrospectively reviewed 676 patients who underwent elective lumbar spine surgery and compared relevant data to that in a matched cohort of 51 patients who predonated blood and 51 patients who received only cell-saver blood and underwent instrumented spinal fusion. Patients who predonated blood had similar blood loss as patients who did not predonate, but they had more blood replacement (1391 cc compared with 410 cc). Patients who predonated blood also had a lower preoperative hemoglobin level and wasted a half unit of blood on average. There was no major difference in allogeneic blood transfusion rates between the two groups. Our data suggest for short, instrumented lumbar fusion surgeries in patients with a normal coagulation profile, preoperative blood donation is not beneficial.
Level of Evidence: Level II, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Several methods reportedly reduce blood loss and avoid allogeneic blood transfusion associated with spinal surgery: (1) autologous blood predonation [3]; (2) intraoperative salvage of shed blood (cell saver) [6]; (3) controlled hypotensive anesthesia [12]; and (4) acute normovolemic hemodilution [1, 23]. Although the efficacy of these methods has been examined in the orthopaedic literature, it is not clear which, if any, method used in adult spine surgery results in greater reduction of blood loss and allogeneic blood transfusions. Additionally, the need for autologous blood transfusion is more difficult to predict for patients undergoing spine surgery because of the diversity of surgical procedures and the increased amount of blood loss expected with more extensive surgery.
Most studies evaluating blood loss and blood transfusion in patients undergoing spine surgery have been limited by small sample size or have been conducted in the pediatric population [7, 9, 11, 14, 18, 22, 25]. Published studies of total joint arthroplasty have outlined possible differences in postoperative complications for patients who predonated autologous blood compared with patients who received washed cell-saver blood during surgery [4, 17, 24]. Aside from the waste that may accompany an inaccurate prediction of how much blood will be required for surgery [5], there are risks of donation reactions and anemia that accompany predonation of blood [10, 13]. Although cell-saver use has become increasingly common, one study of blood replacement in children undergoing spine surgery reported cell-saver blood volume was not sufficient in satisfying perioperative transfusion requirements [9]. Cell-saver blood replacement in adults undergoing spine surgery appears to provide adequate amounts of blood [8, 19] but it is not known whether this method of blood replacement compares favorably with autologous predonation in patients undergoing instrumented spinal fusion.
To answer the questions regarding whether amount of intraoperative replacement and allogeneic transfusion rates differ between preoperative donors and nondonors, we compared (1) amount of intraoperative blood loss and replacement between predonors and nondonors; (2) rates of allogeneic blood transfusion between predonors and nondonors; and (3) cost of wasted predonated units of blood in a subgroup of patients undergoing elective instrumented spinal fusion surgery.
Materials and Methods
We retrospectively reviewed data for 676 consecutive patients undergoing elective lumbar spine surgery from 1994 to 2004 by one surgeon (MDB). From the patient records we determined estimated blood loss and amount and method of blood replacement. Blood loss was estimated by the anesthesiologist by observing the amount of blood in suction containers and that absorbed by surgical sponges. We recorded the following variables: number of operated levels, duration of surgery, comorbidities, patient age, gender, body mass index, type of procedure (one-level bilateral laminectomy and foraminotomy, laminectomy and disc excision, multilevel bilateral laminectomy and foraminotomy, and lumbar fusion), and diagnosis (herniated disc, spinal stenosis, or degenerative spondylolisthesis). These variables have been identified as factors influencing blood loss and transfusion [2, 15, 16, 20]. All patients received general anesthesia. Institutional Review Board approval was obtained before conducting the study.
We anticipated patients undergoing instrumented spinal fusion would be at greater risk of needing a blood transfusion compared with patients having noninstrumented or nonfusion surgery secondary to the need for additional exposure of the spine and a possible second operative site in the case of iliac crest grafting. To address our objectives, we analyzed data from a sample of 51 patients who predonated blood for surgery from 1985 to 1993 who were matched for age within 3 years and gender with 51 patients who did not predonate blood for surgery from 1994 to 2004. All patients in the matched group underwent decompression with instrumented lumbar fusion. No patient in either group received erythropoietin, but patients who predonated blood were prescribed iron supplementation. Many patients reported not tolerating iron therapy secondary to gastric upset and we have no reliable data regarding the number of patients who actually took iron. The study had 80% power to detect a 3% difference in the need for allogeneic blood transfusion between patients who predonated blood and patients who had cell-saver transfusion alone.
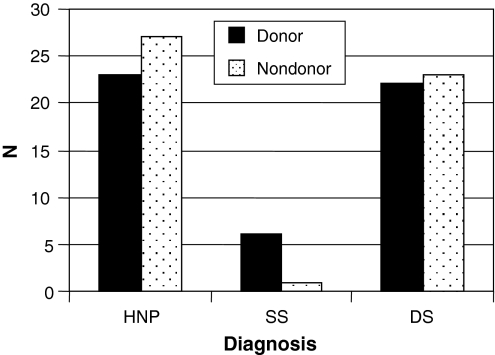
Of 676 consecutive patients, 195 patients underwent lumbar fusion, of which 102 patients who had instrumented spinal fusion were matched for age and gender (Table 1). The remaining 93 patients were unable to be matched for either age or gender. There were no differences in the distribution of spinal stenosis, degenerative spondylolisthesis, or other diagnoses between patients who predonated blood and those who did not (Fig. 1). The mean number of comorbidities was greater (p < 0.01) for the patients who predonated blood, with the most common comorbidities in both groups being hypertension and coronary artery disease (Table 2).
Table 1.
Distribution of surgical procedures
| Procedure | Number |
|---|---|
| One-level bilateral laminectomy/foraminotomy | 266 |
| Laminectomy with disc excision | 114 |
| Multilevel bilateral laminectomy/foraminotomy | 101 |
| Lumbar fusion | 195 |
Fig. 1.
The distribution of diagnoses in patients undergoing instrumented fusion with a diagnosis of spinal stenosis (SS), degenerative spondylolisthesis (DS), or herniated nucleus pulposus (HNP) is shown. There was no difference in the distribution of diagnoses among patients who predonated blood compared with those who did not predonate blood for spinal fusion surgery (χ2 = 3.91; p = 0.14). The majority of patients undergoing fusion were diagnosed with either herniated nucleus pulposus or degenerative spondylolisthesis.
Table 2.
Univariate analysis
| Variable | Donors | Nondonors | p Value |
|---|---|---|---|
| Mean duration of surgery (minutes) | 191 | 193 | 0.95 |
| Mean number comorbidities | 1.54 | 1.27 | < 0.01 |
| Mean number of levels operated | 2.0 | 2.3 | 0.07 |
| Mean blood loss (cc) | 963 | 796 | 0.16 |
| Mean blood replacement (cc) | 1391 | 410 | < 0.01 |
| Mean preoperative hemoglobin (g/dL) | 11.7 | 13.2 | 0.04 |
| Mean postoperative hemoglobin (g/dL) | 11.3 | 10.9 | 0.40 |
| Mean age (years) | 61.4 | 61.3 | 0.86 |
| Mean BMI (kg/m2) | 25.9 | 23.6 | 0.05 |
The blood donation protocol was as follows. At the time data for this study were collected, blood preservatives were eligible only for use within 28 days of donation. We therefore attempted to have patients predonate three units of blood at weekly intervals with a 1-week interval before surgery for the last unit. Patients were advised that we would obtain between one to three units of blood, depending on their hematocrit and their tolerance to donation (orthostatic hypotension, etc). We discontinued having patients predonate blood in the 1990s because too many patients were not able to tolerate donation of three units, fainting, losing the blood, blood not being transported in time for surgery, wasting of blood, and efficiency of the cell-saver machine.
With the exception of four patients who received only their predeposited autologous blood secondary to religious beliefs, patients who predonated blood received predonated autologous blood and autologous packed cell-saver blood. Patients who did not predonate their own blood received only autologous packed cell-saver blood. Intraoperatively and postoperatively, any combination of mean systolic blood pressure less than 70 mm Hg, orthostatic hypotension, and hematocrit less than 24% in young, healthy individuals or less than 27% in older individuals triggered a blood transfusion. Postoperative hemoglobin values were collected after intraoperative transfusion of blood, but not after postoperative transfusion of allogeneic blood in cases in which this occurred. None of the patients received allogeneic banked blood during surgery.
We used a t-test to compare donors and nondonors with respect to age, body mass index, duration of surgery, number of comorbidities, number of operated levels, blood loss, blood replacement, and preoperative and postoperative hemoglobin levels. A chi square test was used to compare the distribution of diagnoses among donors and nondonors. In patients who predonated blood, univariate analysis of variance and linear regression were used to evaluate whether the amount of perioperative blood loss and blood replacement could be predicted by preoperative hemoglobin level, postoperative hemoglobin level on Day 1, and amount of blood predonated.
Results
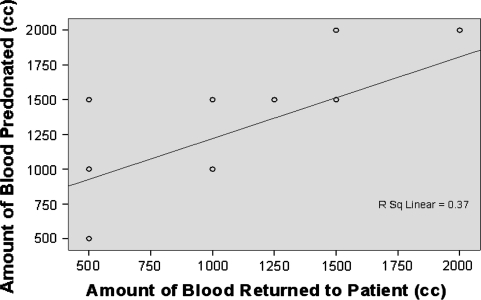
Mean blood loss in the group that predonated blood was similar to blood loss in the group that did not predonate blood (963 cc versus 796 cc, respectively) (Table 2). However, the mean blood replacement for patients who predonated blood was greater (p < 0.01) than replacement for patients who did not predonate blood (1391 cc versus 410 cc, respectively). The mean preoperative hemoglobin level was higher (p = 0.04) for the group of patients that did not predonate blood for surgery; however, the postoperative hemoglobin levels were similar for patients who predonated blood for surgery and those who did not. There also was no difference in the preoperative to postoperative change in hemoglobin levels between the two groups. The amount of blood predonated was associated (p = 0.02) with blood replacement in patients undergoing fusion but was not associated with intraoperative blood loss. As the amount of blood donated before surgery increased, so did the amount of blood replacement using predonated blood (Fig. 2).
Fig. 2.
The linear regression of the amount of blood predonated on the amount of blood returned to the patient is shown (p = 0.02). Although patients who predonated blood did not experience significantly greater intraoperative blood loss compared with nondonors, the amount of blood replacement increased with an increasing amount of blood predonated.
The rates of allogeneic blood transfusion between patients who predonated blood and nondonors were similar (p = 0.99) Two patients who predonated blood (4%) and one patient (2%) who did not predonate blood required allogeneic blood transfusions the week after surgery. Among the patients who required an allogeneic blood transfusion postoperatively, the only distinguishing characteristic was that the patient who did not predonate blood was an admitted cocaine abuser.
At our institution, the total cost charged to the patient for predonation of blood is $217 per unit. In our study, on average, a half unit of blood (238 cc) was left over for patients who predonated blood, a waste of approximately $5508 for 51 patients. No major complications of surgery, including acute myocardial infarction, were observed in either group of patients; however, detailed data regarding possible minor complications were not available. No complications related to cell-saver use were observed in this population.
Discussion
The spine literature has not extensively addressed whether blood loss and rates of allogeneic transfusions are increased in patients who predonate blood before surgery compared with patients who receive only cell-saver blood intraoperatively. We asked whether (1) the amount of intraoperative blood loss and blood replacement differs between autologous donors and nondonors and (2) the rates of allogeneic blood transfusions differ between the two groups; we then determined the cost of wasted predonated units.
One limitation in this matched cohort analysis is accurate determination of intraoperative blood loss. Estimation of blood loss is difficult. Apart from measuring the volume of the suctioned blood, the anesthetist has to make a visual estimate of blood shed on the floor, spread in the surgeons’ gowns and gloves, and hidden in drapes and sponges. Meiser et al. [21] simulated typical blood loss scenes occurring during a mock hip arthroplasty and reported a broad deviation in visual estimates. We acknowledge accurate determination of blood loss is difficult; however, overestimations and underestimations are likely, and previous studies have used similar methodology [7, 25]. Although our study is retrospective, all of the operations in this study were performed in the same operative suite with the same protocol for determining blood loss in both cohorts. We were able to minimize the potential for bias by forming two matched cohort groups. In these groups, only preoperative hemoglobin levels differed (greater in nondonors; Table 2). However, to ensure the absence of any bias, a prospective, randomized trial is needed. Finally, our post hoc power analysis was based on a 3% difference in transfusion rates; we do not know whether this is a clinically important difference.
Patients undergoing instrumented lumbar fusion experienced more perioperative blood loss and were more likely to receive an allogeneic blood transfusion than patients having noninstrumented surgery. In our study, blood loss was similar in patients who predonated blood and patients who did not predonate blood. Although the group of patients who predonated blood did not lose statistically significantly more blood, they did have slightly greater mean blood loss (167 cc). Because none of the surgeries in this study were to correct spinal deformity, the results may not be generalized to patients undergoing larger surgeries in terms of amount of blood loss.
Cha et al. [7] reported, in patients who underwent fusion, preoperative autologous blood donation decreased the risk of allogeneic blood transfusion by 75% in noninstrumented fusions and 50% in instrumented fusions compared with patients who did not predonate blood before fusion; these authors did not use intraoperative blood salvage. Our data suggest blood replacement with washed cell-saver blood was adequate to meet the transfusion needs of the patients who did not predonate, because the rates of postoperative allogeneic transfusion were not different between the two groups. On average, these patients had 410 cc of blood replaced intraoperatively and only one patient required an allogeneic blood transfusion the week after surgery.
Although rates of allogeneic blood transfusion were similar in patients who predonated and those who received cell-saver blood alone, waste was a problem. Based on the last 5 years’ data from the blood transfusion department at the University of Miami, 45% to 55% of all predonated units are wasted each year. At our institution, the total cost charged to the patient is $217 per unit. Patients who predonated blood had an average of 1391 cc replaced intraoperatively. Although the retrospective nature of this study does not allow us to determine which criteria triggered transfusion, the results of this study suggest patients who predonate blood may require more blood replacement intraoperatively than patients who have blood replaced with a cell saver alone. These results support other studies that suggest predonation of blood increases the likelihood of autologous transfusion and increases healthcare costs [4, 5]. Johnson et al. [19] reported similar waste for a group of patients in which predeposited autologous blood and intraoperative blood salvage were used. In patients who underwent posterior lumbar fusion, 54% of the predeposited blood was wasted. Although the cost of cell-saver blood may be higher than that of autologous predonation of blood, the fact that a mix of predonated blood and cell-saver blood were returned to the patients who predonated and the considerable waste that occurred in this group suggest the benefits of cell-saver blood may outweigh the costs.
Considering the similar blood loss and need for allogeneic blood transfusion in patients who predonated blood compared with those who received cell-saver blood alone, our data suggest for short instrumented lumbar fusions in patients with a normal coagulation profile, preoperative blood donation is not beneficial.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Bennett J, Haynes S, Torella F, Grainger H, McCollum C. Acute normovolemic hemodilution in moderate blood loss surgery: a randomized controlled trial. Transfusion. 2006;46:1097–1103. [DOI] [PubMed]
- 2.Berenholtz SM, Pronovost PJ, Mullany D, Garrett E, Ness PM, Dorman T, Klag MJ. Predictors of transfusion for spinal surgery in Maryland, 1997 to 2000. Transfusion. 2002;42:183–189. [DOI] [PubMed]
- 3.Bern MM, Bierbaum BE, Katz JN, Losina E. Autologous blood donation and subsequent blood use in patients undergoing total knee arthroplasty. Transfus Med. 2006;16:313–319. [DOI] [PubMed]
- 4.Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999;81:2–10. [DOI] [PubMed]
- 5.Billote DB, Glisson SN, Green D, Wixson RL. A prospective, randomized study of preoperative autologous donation for hip replacement surgery. J Bone Joint Surg Am. 2002;84:1299–1304. [DOI] [PubMed]
- 6.Bridgens JP, Evans CR, Dobson PM, Hamer AJ. Intraoperative red blood-cell salvage in revision hip surgery: a case-matched study. J Bone Joint Surg Am. 2007;89:270–275. [DOI] [PubMed]
- 7.Cha CW, Deible C, Muzzonigro T, Lopez-Plaza I, Vogt M, Kang JD. Allogeneic transfusion requirements after autologous donations in posterior lumbar surgeries. Spine. 2002;27:99–104. [DOI] [PubMed]
- 8.Chandra A, Smith DR, Nanda A. Autotransfusion by cell saver technique in surgery of lumbar and thoracic spinal fusion with instrumentation. J Neurosurg. 2002;96(3 suppl 3):298–303. [DOI] [PubMed]
- 9.Copley LAB, Richards BS, Safavi FZ, Newton PO. Hemodilution as a method to reduce transfusion requirements in adolescent spine fusion surgery. Spine. 1999;24:219–222; discussion 223–224. [DOI] [PubMed]
- 10.Cregan P, Donegan E, Gotelli G. Hemolytic transfusion reaction following transfusion of frozen and washed autologous red cells. Transfusion. 1991;31:172–175. [DOI] [PubMed]
- 11.Epstein NE, Peller A, Korsh J, DeCrosta D, Boutros A, Schmigelski C, Greco J. Impact of intraoperative normovolemic hemodilution on transfusion requirements for 68 patients undergoing lumbar laminectomies with instrumented posterolateral fusion. Spine. 2006;31:2227–2230; discussion 2231. [DOI] [PubMed]
- 12.Eroglu A, Uzunlar H, Erciyes N. Comparison of hypotensive epidural anesthesia and hypotensive total intravenous anesthesia on intraoperative blood loss during total hip replacement. J Clin Anesth. 2005;17:420–425. [DOI] [PubMed]
- 13.Forgie MA, Wells PS, Laupacis A, Fergusson D. Preoperative autologous donation decreases allogeneic transfusion but increases exposure to all red blood cell transfusion: results of a meta-analysis. International Study of Perioperative Transfusion (ISPOT) Investigators. Arch Intern Med. 1998;158:610–616. [DOI] [PubMed]
- 14.Goulet JA, Bray TJ, Timmerman LA, Benson DR, Bargar WL. Intraoperative autologous transfusion in orthopaedic patients. J Bone Joint Surg Am. 1989;71:3–8. [PubMed]
- 15.Grosflam JM, Wright EA, Cleary PD, Katz JN. Predictors of blood loss during total hip replacement surgery. Arthritis Care Res. 1995;8:167–173. [DOI] [PubMed]
- 16.Guay J, Haig M, Lortie L, Guertin MC, Poitras B. Predicting blood loss in surgery for idiopathic scoliosis. Can J Anaesth. 1994;41:775–781. [DOI] [PubMed]
- 17.Hatzidakis AM, Mendlick RM, McKillip T, Reddy RL, Garvin KL. Preoperative autologous donation for total joint arthroplasty: an analysis of risk factors for allogenic transfusion. J Bone Joint Surg Am. 2000;82:89–100. [DOI] [PubMed]
- 18.Healy WL, Pfeifer BA, Kurtz SR, Johnson C, Johnson W, Johnston R, Sanders D, Karpman R, Hallack GN, Valeri CR. Evaluation of autologous shed blood for autotransfusion after orthopaedic surgery. Clin Orthop Relat Res. 1994;299:53–59. [PubMed]
- 19.Johnson RG, Murphy M, Miller M. Fusions and transfusions: an analysis of blood loss and autologous replacement during lumbar fusions. Spine. 1989;14:358–362. [DOI] [PubMed]
- 20.Keating EM, Meding JB, Faris PM, Ritter MA. Predictors of transfusion risk in elective knee surgery. Clin Orthop Relat Res. 1998;357:50–59. [DOI] [PubMed]
- 21.Meiser A, Casagranda O, Skipka G, Laubenthal H. [Quantification of blood loss: how precise is visual estimation and what does its accuracy depend on?][in German]. Anaesthesist. 2001;50:13–20. [DOI] [PubMed]
- 22.Moran MM, Kroon D, Tredwell SJ, Wadsworth LD. The role of autologous blood transfusion in adolescents undergoing spinal surgery. Spine. 1995;20:532–536. [DOI] [PubMed]
- 23.Murray D. Acute normovolemic hemodilution. Eur Spine J. 2004;13(suppl 1):S72–75. [DOI] [PMC free article] [PubMed]
- 24.Woolson ST, Wall WW. Autologous blood transfusion after total knee arthroplasty: a randomized prospective study comparing predonated and postoperative salvage blood. J Arthoplasty. 2003;18:243–249. [DOI] [PubMed]
- 25.Zheng F, Cammisa FP Jr, Sandhu HS, Girardi FP, Khan SN. Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine. 2002;27:818–824. [DOI] [PubMed]