Abstract
Ludloff’s medial approach has been described as a simple procedure for open reduction of developmental dysplasia of the hip (DDH) requiring minimal dissection and tissue disruption. Many patients undergo subsequent reconstruction of the acetabulum after skeletal maturity for residual dysplasia. Femoral head deformity reportedly influences the long-term outcome of these osteotomies. The literature suggests this deformity may be related to the patient’s age at the time of a medial approach. We therefore asked whether femoral head deformity (roundness index, femoral head enlargement) at skeletal maturity correlates with patient age at surgery. We assessed the radiographs of 40 patients (42 hips). Their mean age at surgery was 14.3 months (range, 6–31 months); the minimum followup was 10 years (mean, 15.8 years; range, 10–27 years). The mean roundness index at skeletal maturity correlated with increased age at the time of the operation (mean index, 58.3; range, 47–79) while enlargement did not. Using a medial approach for correction of DDH in older patients increases the risk of femoral head deformity at skeletal maturity.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The medial approach for open reduction of DDH was introduced by Ludloff in 1913 [11]. His method has been described as a simple procedure needing minimal dissection and tissue destruction; it allows correction of anteroinferior tightness by releasing the tight iliopsoas tendon and the constricted anteroinferior part of the capsular ligament. Numerous reports have described open reduction using the medial approach [1, 5, 8–10, 12–14, 24, 27], but many patients in these studies subsequently underwent open reduction for reconstruction of the acetabulum [1, 5, 8–10, 12–14, 24, 27]. Periacetabular osteotomy to reduce the risk of late osteoarthrosis usually is selected to reconstruct the hip after skeletal maturity when there is residual dysplasia after open reduction [18–21, 25, 26]. One study suggests deformity of the femoral head after open reduction influences the long-term outcome of later periacetabular osteotomy for residual dysplasia [21]. The question arises, then, whether prior medial approach influences deformity of the femoral head.
We therefore asked whether (1) the age at the time of open reduction using a medial approach correlated with femoral head deformity (roundness and enlargement indices) and (2) the postoperative radiographic results (assessed using the Severin [23] and the Kalamchi and MacEwen [7] classification systems) were satisfactory at skeletal maturity.
Materials and Methods
We retrospectively reviewed 45 consecutive patients with complete hip dislocation treated with Ludloff’s approach between 1979 and 1996. The indications for the original surgery were: the dislocated hip could not be reduced, or reduction could not be maintained without a forced position (> 90–100° flexion or > 60° abduction) when examined under anesthesia. This approach was used for all patients treated by open reduction during this period. We ascertained the deformity of the femoral head at skeletal maturity and the relationship between age at the time of the surgery and femoral head deformity. The minimum postoperative followup was 10 years (mean, 15.8 years; range, 10–27 years). Five of the 45 patients (11%) were lost to followup before the minimum 10-year followup. The mean age of these five patients at the time of surgery was 14.1 months (range, 6–24 months), and the minimum followup was 1 year (mean, 3.7 years; range, 1–6 years). At last followup, relocation had been maintained in all five patients. The remaining 40 patients (42 hips) had a mean age at surgery of 14.3 months (range, 6–31 months). There were 33 girls and seven boys. Two were affected bilaterally. Twenty-four of the hips were right and 18 were left. Three patients (three hips) had an additional osteotomy less than 10 years after open reduction. Excluding these three patients we had 37 patients (39 hips) in two groups: one comprising 25 hips in patients younger than 17 months at surgery, and the other 14 hips in patients 17 months or older at the time of surgery. The mean ages of patients at followup were similar (p = 0.89) in both groups: 15.1 years (range, 10–22 years) and 15.7 years (10–27 years), respectively. We did not obtain Institutional Review Board approval because our institution does not require such approval for retrospective studies.
To obtain open reduction at surgery we excised the anterior part of the capsule down to the femoral neck together with the hypertrophied ligamentum teres. We detached the psoas tendon near its insertion and allowed it to retract proximally. The transverse ligament was divided to allow stable reduction, and the labrum was partially excised in 13 hips because concentric reduction was not obtained. In one patient, redislocation was diagnosed radiographically immediately after surgery; this patient underwent manual reduction and cast fixation the same day. No major neurovascular damage or deep infections were observed in any patient.
Postoperatively, all patients wore a hip spica cast in 90° to 100° flexion and 70° abduction. Extreme abduction was avoided to maintain blood circulation in the femoral head. After 4 weeks, patients were instructed to wear a flexion-abduction brace full time for 4–6 months. Once the patients began walking, they wore the brace only during naps and at night. Every 6 months, the hip was examined, and radiographs were obtained with the patient in the supine position. Anteroposterior radiographs were taken with a source-to-film distance of 110 cm. The patient’s feet were internally rotated with the toes at 15° ± 5° to ensure that the xray beam was centered on the superior aspect of the pubic symphysis.
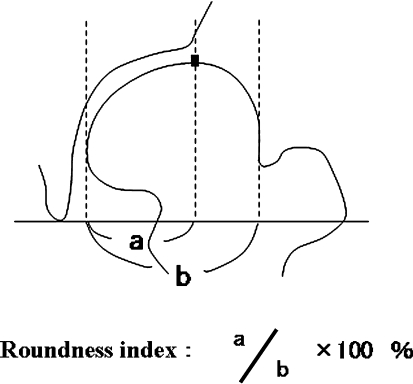
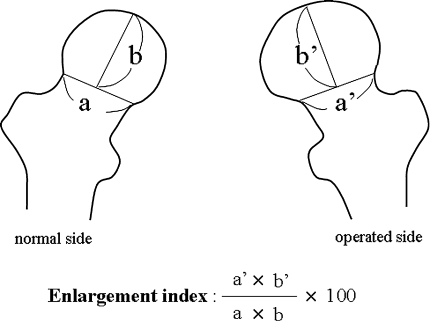
We also evaluated the deformity and enlargement of the femoral head. To evaluate the femoral head deformity, we measured its roundness index [22], which is the ratio between the distance from the medial border to the top of the femoral head and that from the medial to the lateral border of the femoral head (Fig. 1). To evaluate enlargement of the femoral head, we measured its enlargement index [6]. The baseline was drawn through the lateral end of the epiphyseal line or the distal edge of the line’s lateral end of the femoral head on anteroposterior radiographs [15]. The enlargement index is calculated by multiplying the distance of the baseline of the femoral head with the vertical distance from the midpoint of the baseline to the joint surface of the femoral head. It is presented as a relative percentage of the calculated values on the surgically treated side as the numerator and that of the nonsurgically treated side as the denominator (Fig. 2). We evaluated this parameter only in 35 patients who underwent unilateral hip reduction. We examined the femoral head condition at followup and at the time of surgery.
Fig. 1.
The roundness index of the femoral head is the distance from the medial border to the top of the femoral head (a) and from the medial to the lateral border of the femoral head (b). (Published with permission from Okano K, Enomoto H, Harada S, Ito S, Doiguchi Y, Shindo H. [Clinical results of rotational acetabular osteotomy (RAO) for advanced osteoarthritis of the hip: evaluation of the shape of the femoral head.] Hip Joint. 2003;29:102–108.)
Fig. 2.
The enlargement index of the femoral head is the distance of the baseline of the femoral head (a, a′) and the vertical distance from the midpoint of the baseline to the joint surface of the femoral head (b, b′).
To test reproducibility of the radiographic measurements, two of the authors (KO, HE) measured the roundness and enlargement indices in 20 randomly selected hips. Each observer measured each hip two times at a 1-week interval. The coefficients of variation of roundness and enlargement indices were 2.6% and 3.5% for interobserver variation and 1.9% and 2.1% for intraobserver variation, respectively. To assess reliability of the Severin [23] and the Kalamchi and MacEwen [7] classification systems, all radiographs were reviewed independently by two authors (KO, HE). Interobserver variability (kappa statistics) was 0.94 and 0.91, respectively.
Using the radiographs obtained at last followup, we (KO, HE) classified the hips according to the Severin classification [23], and classified osteonecrosis (ON) using the criteria of Kalamchi and MacEwen [7]. Severin Classes I and II were considered good because the patients have no acetabular dysplasia [23], while Classes III, IV, and V were considered poor. We excluded Kalamchi and MacEwen Type I ON from the analysis because those classes do not influence the radiographic results at skeletal maturity [7].
We tested differences in roundness and enlargement indices using the Wilcoxon rank test. The correlation between radiographic parameters and age of the patient at surgery was evaluated using Pearson’s correlation coefficient. As an additional test of the indices, they were compared in patients younger than 17 months and patients 17 months or older at the time of surgery. We used StatView software (Abacus Concepts, Berkeley, CA).
Results
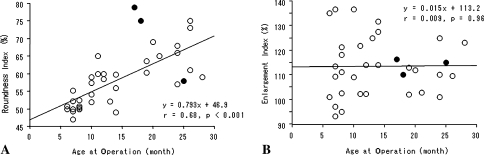
Deformity (roundness index) correlated (r = 0.68; p < 0.0001) with age at the time of surgery. The mean roundness index for all patients at followup was 58.3 (range, 47–79). The mean enlargement index, however, did not correlate (r = 0.009; p = 0.96) with age at the time of surgery (mean index at followup 113.4; range, 93–137) (Fig. 3). When we excluded three patients with Kalamchi and MacEwen Type III or IV ON (see below), the roundness index more strongly correlated (r = 0.77; p < 0.001) with age at surgery, and the enlargement index (r = 0.005; p = 0.98) did not. We found no correlation (r = −0.12; p = 0.49) between the two indices. The mean roundness index in patients with a good Severin class (mean, 52.9; range, 47–60) was lower (p = 0.0003) than that of patients with a poor Severin class (mean, 62.2; range, 50–79). However, the mean values of the enlargement index were similar (p = 0.70) in the two groups (mean, 113.7; range, 101–128 in the good group versus mean, 113.1; range, 93–137 in the poor group). The average roundness index at followup was lower (p < 0.0001) in patients younger than 17 months compared with patients 17 months and older (53.8, range, 47–65 versus 66.3, range, 47–79, respectively). The average roundness index was similar (p = 0.14) in patients without and with resection of the labrum (56.7, range, 47–75 versus 61.6, range, 49–79, respectively).
Fig. 3A–B.
The correlation between age at the time of surgery and (A) the roundness and (B) enlargement indices of the femoral head at followup are shown. The black circles represent hips classified as Kalamchi and MacEwen Type III or IV.
At last followup six hips were rated as Severin Class I, 10 as Class II, 18 as Class III, three as Class IV, and two as Class V. Thirteen of 42 hips (31%) had ON of the femoral head, including 10 hips classified as Kalamchi and MacEwen Type II, one as Type III, and two as Type IV. Five operations performed later for acetabular reconstruction included a shelf operation plus derotation varus osteotomy in one hip 3 years and in two hips 4 years after open reduction; a Chiari pelvic osteotomy in one hip 11 years after open reduction, and a rotational acetabular osteotomy in one hip 16 years after open reduction. Two patients, in whom osteotomies were performed more than 10 years after open reduction, were evaluated just before the osteotomy. Three hips (three patients) in which osteotomies were performed less than 10 years after open reduction, and which were classified as Severin Class II at final followup, were excluded from evaluation. Four patients with hips classified as Severin Class IV or V refused additional surgery for subluxation of the femoral head and acetabular dysplasia despite our recommendation.
Discussion
The medial approach described by Ludloff [11] for open reduction of a dysplastic hip has been described as simple requiring minimal dissection and tissue disruption. However, one study suggests deformity of the femoral head after open reduction influences the long-term outcome of later periacetabular osteotomy for residual dysplasia [21]. The question arises, then, whether prior medial approach influences deformity of the femoral head. We therefore assessed femoral head deformity at skeletal maturity after open reduction by the medial approach and asked whether a relationship exists between femoral head deformity and age at the time of surgery.
Our study has several limitations. First, the roundness and enlargement indices were used, which addressed only a two-dimensional aspect of a three-dimensional structure of the femoral head. However, anteroposterior radiographs usually were obtained to evaluate the condition of the femoral head [15, 17] and determine the indications for pelvic osteotomy [21]. Second, patients in this series were treated by more than one surgeon (KO, HE, and KT), however, a standardized therapeutic protocol for DDH at our institution was followed for indication, surgical procedure, casting, and brace fixation after surgery. Third, we cannot explain the mechanism for pathogenesis of the femoral head deformity after open reduction using the medial approach. This approach allows releasing only anteroinferior tightness of the hip; posterosuperior tightness attributable to the posterior dislocated position associated with weightbearing compression remained. Insufficient anatomic reduction and instability of the femoral head in patients who undergo correction after reaching the age at which they begin to walk may cause deformation of the femoral head associated with growth.
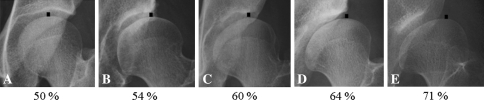
Our patients had various degrees of deformity of the femoral head at skeletal maturity after open reduction through a medial approach (Fig. 4), and the deformity correlated with increased age at the time of surgery. The roundness index was larger in patients who were 17 months or older than in patients who were younger than 17 months when treated. Our results suggest that selection of patients younger than 17 months for this approach would result in a better femoral head condition at skeletal maturity.
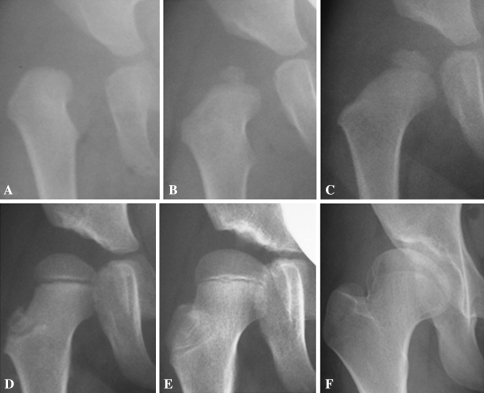
Fig. 4A–E.
Deformities of the femoral head of (A) 50%, (B) 54%, (C) 60%, (D) 64%, and (E) 71% and the associated roundness index are shown. As deformation of the femoral head increases, the top of the femoral head moves laterally. The black square shows the top of the femoral head. (Published with permission from Okano K, Enomoto H, Harada S, Ito S, Doiguchi Y, Shindo H. [Clinical results of rotational acetabular osteotomy (RAO) for advanced osteoarthritis of the hip: evaluation of the shape of the femoral head.] Hip Joint. 2003;29:102–108.)
Osteonecrosis rates of 0% to 67% have been reported after open reduction through a medial approach [1, 5, 8–10, 12–14, 24, 27], and some describe the relationship between age at open reduction and presence of ON at followup. Mergen et al. observed ON only in patients younger than 7 months and older than 18 months [14]. Castillo and Sherman and Mankey et al. reported ON correlated positively with increased age at surgery [1, 12]. We believe the relatively high percent of ON in our series (31%) is attributable to our patients being a little older than patients in other series.
The medial approach for open reduction is a minimally invasive method for correcting DDH; however, satisfactory or unsatisfactory long-term results have been reported, and many patients needing additional surgery after this approach were included at the time of followup [10, 13, 16, 27]. Satisfactory long-term results of periacetabular osteotomy for residual dysplasia after open reduction have been reported [18, 20, 25, 26]. Satisfactory middle- or long-term clinical and radiographic results of periacetabular osteotomy also have been reported for patients with severe dysplasia [2, 19, 26]. In contrast, unsatisfactory long-term radiographic results of periacetabular osteotomy have been reported for patients with severe deformity of the femoral head, particularly those with early osteoarthritis of the hip [21]. Periacetabular osteotomy combined with proximal femoral valgus osteotomy was performed in patients with severe deformity of the femoral head, and the complexity of these procedures increased the risk of perioperative complications [3].
Mergen et al. reported patients having a medial approach for open reduction and between 7 and 18 months old at the time of surgery had good results based on the Severin classification [14]. Castillo and Sherman similarly reported patients between 5 and 14 months old at the time of surgery had good results [1]. Mankey et al. reported the medial approach was effective in infants younger than 24 months old [12]. However, patients in these three studies had less than 10 years followup. Isiklar et al. compared radiographic results for children 12 to 18 months and younger than 12 months at the time of surgery, with a followup of 19.6 years (range, 13–28 years) [5]. They reported that although additional bone surgery is needed more frequently in children 12 to 18 months old, the radiographic outcome is similar to that for patients younger than 12 months [5].
We observed enlargement of the femoral head after open reduction; however, there was no relationship with age at the time of surgery, and all four patients (four hips) with greater than 130% of the enlargement index had correction when younger than 15 months. Thus, the mechanism of enlargement of the femoral head may differ from that of deformation of the femoral head. Matsushita et al. compared the radiographic results at skeletal maturity between open reduction using the wide exposure method [13], which is more invasive, and the medial approach; femoral head enlargement was observed more frequently with the wide exposure method than with the medial approach. Increased blood supply to the femoral head caused by invasion during surgery may influence subsequent enlargement of the femoral head [4, 6]. We found no relationship between enlargement of the femoral head and radiographic results at skeletal maturity. Our experience suggests that when the femoral head is set in a concentrically reduced position, the acetabulum grows well, even with an enlarged femoral head caused by open reduction. However, deformity of the femoral head was associated with unacceptable radiographic results (Fig. 5). Incomplete growth of the acetabulum and deformation of the femoral head might be influenced by each other. In our series, three patients underwent osteotomy less than 10 years after open reduction for residual dysplasia; the average roundness index in these patients was 52.6% at followup. Early reconstruction of the acetabulum may lead the femoral head to become round with skeletal growth.
Fig. 5A–F.
A series of radiographs of a young girl with developmental dysplasia of the hip are shown. Open reduction was performed using Ludloff’s medial approach when she was 19 months old. The radiographs were obtained (A) before surgery, (B) when the patient was 24 months old, (C) 30 months old, (D), 4 years old, (E) and 7 years old. When the patient was 16 years old, (F) the roundness index was 60% and her hip was Severin Class III.
The occurrence of severe deformity of the femoral head at greater than 10 years followup correlated with increased age at the time of surgery. Indications for using the medial approach for correction of DDH in older patients must take into account the risk of subsequent femoral head deformity at skeletal maturity.
Acknowledgments
We thank Dr. Katsuro Iwasaki and Dr. Kenji Yamada for assistance and advice concerning open reduction by Ludloff’s medial approach.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Castillo R, Sherman FC. Medial adductor open reduction for congenital dislocation of the hip. J Pediatr Orthop. 1990;10:335–340. [DOI] [PubMed]
- 2.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005;87:254–259. [DOI] [PubMed]
- 3.Clohisy JC, Nunley RM, Curry MC, Schoenecker PL. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am. 2007;89:1417–1423. [DOI] [PubMed]
- 4.Imatani J, Miyake Y, Nakatsuka Y, Akazawa H, Mitani S. Coxa magna after open reduction for developmental dislocation of the hip. J Pediatr Orthop. 1995;15:337–341. [DOI] [PubMed]
- 5.Isiklar ZU, Kandemir U, Ucar DH, Tumer Y. Is concomitant bone surgery necessary at the time of open reduction in developmental dislocation of the hip in children 12–18 months old? Comparison of open reduction in patients younger than 12 months old and those 12–18 months old. J Pediatr Orthop B. 2006;15:23–27. [DOI] [PubMed]
- 6.Iwasaki K, Suzuki R, Miyata S, Matsumoto N, Tazoe S, Katayama M. [Coxa magna after open reduction for congenital dislocation of the hip][in Japanese]. Rinsho Seikeigeka. 1978;13:10–21.
- 7.Kalamchi A, MacEwen GD. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am. 1980;62:876–888. [PubMed]
- 8.Kalamchi A, Schmidt TL, MacEwen GD. Congenital dislocation of the hip: open reduction by the medial approach. Clin Orthop Relat Res. 1982;169:127–132. [PubMed]
- 9.Kiely N, Younis U, Day JB, Meadows TM. The Ferguson medial approach for open reduction of developmental dysplasia of the hip: a clinical and radiological review of 49 hips. J Bone Joint Surg Br. 2004;86:430–433. [DOI] [PubMed]
- 10.Koizumi W, Moriya H, Tsuchiya K, Takeuchi T, Kamegaya M, Akita T. Ludloff’s medial approach for open reduction of congenital dislocation of the hip: a 20-year follow-up. J Bone Joint Surg Br. 1996;78:924–929. [DOI] [PubMed]
- 11.Ludloff K. The open reduction of the congenital hip dislocation by an anterior incision. Am J Orthop Surg. 1913;10:438–454.
- 12.Mankey MG, Arntz GT, Staheli LT. Open reduction through a medial approach for congenital dislocation of the hip: a critical review of the Ludloff approach in sixty-six hips. J Bone Joint Surg Am. 1993;75:1334–1345. [DOI] [PubMed]
- 13.Matsushita T, Miyake Y, Akazawa H, Eguchi S, Takahashi Y. Open reduction for congenital dislocation of the hip: comparison of the long-term results of the wide exposure method and Ludloff’s method. J Orthop Sci. 1999;4:333–341. [DOI] [PubMed]
- 14.Mergen E, Adyaman S, Omeroglu H, Erdemli B, Isiklar U. Medial approach open reduction for congenital dislocation of the hip using the Ferguson procedure: a review of 31 hips. Arch Orthop Trauma Surg. 1991;110:169–172. [DOI] [PubMed]
- 15.Meyer J. Treatment of Legg-Calvé-Perthes disease: assessment of therapeutic results with particular reference to the value of traction in bed. Acta Orthop Scand. 1966;86(suppl):9–111. [DOI] [PubMed]
- 16.Morcuende JA, Meyer MD, Dolan LA, Weinstein SL. Long-term outcome after open reduction through an anteromedial approach for congenital dislocation of the hip. J Bone Joint Surg Am. 1997;79:810–817. [DOI] [PubMed]
- 17.Mose K. Methods of measuring in Legg-Calve-Perthes disease with special regard to the prognosis. Clin Orthop Relat Res. 1980;150:103–109. [PubMed]
- 18.Nakamura S, Ninomiya S, Takatori Y, Morimoto S, Umeyama T. Long-term outcome of rotational acetabular osteotomy: 145 hips followed for 10–23 years. Acta Orthop Scand. 1998;69:259–265. [DOI] [PubMed]
- 19.Nozawa M, Shitoto K, Hirose T, Matsuda K, Michino K, Kajihara H, Maezawa K, Kurosawa H. Rotational acetabular osteotomy for severely dysplastic acetabulum. Arch Orthop Trauma Surg. 2000;120:376–379. [DOI] [PubMed]
- 20.Nozawa M, Shitoto K, Matsuda K, Maezawa K, Kurosawa H. Rotational acetabular osteotomy for acetabular dysplasia: a follow-up for more than ten years. J Bone Joint Surg Br. 2002;84:59–65. [DOI] [PubMed]
- 21.Okano K, Enomoto H, Osaki M, Shindo H. Outcome of rotational acetabular osteotomy for early hip osteoarthritis secondary to dysplasia related to femoral head shape: 49 hips followed for 10–17 years. Acta Orthop. 2008;79:12–17. [DOI] [PubMed]
- 22.Okano K, Enomoto H, Harada S, Ito S, Doiguchi Y, Shindo H. [Clinical results of rotational acetabular osteotomy (RAO) for advanced osteoarthritis of the hip: evaluation of the shape of the femoral head] [in Japanese]. Hip Joint. 2003;29:102–108.
- 23.Severin E. Contribution to the knowledge of congenital dislocation of the hip joint: late results of closed reduction and arthrographic studies of recent cases. Acta Chir Scand. 1941;84:1–142.
- 24.Sosna A, Rejholec M, Rybka V, Popelka S Jr, Fric V. [Long-term results of Ludloff’s repositioning method][in Czech]. Acta Chir Orthop Traumatol Cech. 1990;57:213–223. [PubMed]
- 25.Takatori Y, Ninomiya S, Nakamura S, Morimoto S, Moro T, Nagai I, Mabuchi A. Long-term results of rotational acetabular osteotomy in patients with slight narrowing of the joint space on preoperative radiographic findings. J Orthop Sci. 2001;6:137–140. [DOI] [PubMed]
- 26.Takatori Y, Ninomiya S, Nakamura S, Morimoto S, Sasaki T. Long-term follow-up results of rotational acetabular osteotomy in painful dysplastic hips: efficacy in delaying the onset of osteoarthritis. Am J Orthop. 1996;25:222–225. [PubMed]
- 27.Ucar DH, Isiklar ZU, Stanitski CL, Kandemir U, Tumer Y. Open reduction through a medial approach in developmental dislocation of the hip: a follow-up study to skeletal maturity. J Pediatr Orthop. 2004;24:493–500. [PubMed]