Abstract
Although hemiarthroplasties are an important treatment for femoral neck fractures, the literature does not provide a clear approach for selecting the implant fixation method. Therefore, we performed a systematic search of the medical literature and identified 11 prospective and retrospective studies that compared results between cemented and uncemented femoral implant fixation methods. After independent blind data extraction, we compared variables between cemented and uncemented cohorts using two different meta-analysis models. Pooled data represented 1632 cemented and 981 uncemented hemiarthroplasties (average age of patients, 78.9 and 77.5 years, respectively). The average operating room times and blood loss volumes were 95 minutes and 467 mL, respectively, for the cemented and 80 minutes and 338 mL for the uncemented cohorts. Postoperative mortality rates, overall complications, and pain were similar between the two cohorts. Despite a few potential trends, we found few statistical differences between cemented and uncemented techniques based on reported outcome measurements. In addition, inspection of this literature underscored the lack of and need for consistent and standardized reporting of outcome variables regarding these procedures.
Level of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-008-0368-3) contains supplementary material, which is available to authorized users.
Introduction
Hip fractures, including intracapsular fractures of the proximal femur, in elderly women are common and may be increasing among elderly men [3]. Despite continued discussion regarding the treatment of these fractures, controversies continue regarding their optimal treatment, including the choice of implant and fixation method [1, 2, 11, 13, 22].
Although there is a plethora of reports concerning these fractures, the outcome measures and treatments advocated are inconsistent and varied [1, 2, 11, 13, 22]. Hemiarthroplasty remains a common and important treatment in the United States; however, the literature does not clearly suggest whether cementing the femoral stem enhances outcomes [5, 7–10, 12, 14–18, 21, 23]. Systematic reviews have been performed but are either too stringent in criteria or do not provide quantitative assessments [15, 21]. A recent Cochrane review included only five studies (all randomized, prospective; two were published in abstract form only) for analysis and data from only one or two studies for evaluation of almost all outcomes of interest [21]. In this context of limited numbers of studies compared, no significant differences were found.
Our objective was to provide useful quantitative assessment of outcomes data comparing cemented and uncemented methods as treatment for femoral neck fractures by including clinically important variables that were amenable to meta-analysis (blood loss, operative time, perioperative and postoperative mortality, complications, pain, and revisions) and by including retrospective and prospective studies while using statistical methods to account for variability in and between studies.
Materials and Methods
We (JA, LM) performed a systematic search of the English language medical literature on cemented and uncemented hemiarthroplasties for treatment of femoral neck fractures in the elderly published between 1980 and August 2005. We used the terms (fracture OR fractures OR fractured) AND (femur OR femoral OR femurs) AND (cement OR cemented OR cementing) AND (hemi-arthroplasty OR hemiarthroplasty OR arthroplasty) AND (neck OR basi-cervical OR basicervical OR sub-capital OR subcapital OR intra-capsular OR intracapsular) to search the PubMed databases and Cochrane Library with a resultant 190 matches. All 190 titles and abstracts were examined and those that did not address the topics of proximal intracapsular femoral fractures treated at least in part by arthroplasty were discarded. This was supplemented by hand searches of reference lists and our personal files. The final list of 120 articles agreed on by two authors (JA, ML) included 116 published articles and four abstracts not published as full peer-reviewed manuscripts. (Supplementary materials are available with the online version of CORR.)
We (all authors) applied preset inclusion (randomized trial or comparison of cemented and uncemented methods, intracapsular proximal femoral fractures, clinical outcomes studied) and exclusion criteria (mixed age population, average age younger than 60 years, review article, multiple publication of identical cohort, femoral head fractures, intertrochanteric or pertrochanteric fractures, studies without extractable outcomes, fewer than 10 patients in either group). We did not exclude appropriate cohort comparison studies based on low Cochrane methodologic quality score alone (Table 1). For studies published as abstracts only, we contacted authors for provision of outcomes of interest; however, no data were returned. Two investigators (JA, LM) independently reviewed all studies and agreement was obtained on 11 studies (Table 2), including three randomized, controlled trials and eight retrospective cohort comparisons [5, 7–10, 12, 14–18, 21, 23].
Table 1.
Methodologic quality of included studies
| Score* | Authors | Year | Score |
|---|---|---|---|
| 4 | Eiskjaer et al. [7] | 1989 | (Parker and Gurusamy 2006 [21]) |
| 4 | Holt et al. [12] | 1994 | |
| 5 | Lennox and McLauchlan [17] | 1993 | |
| 3 | Gebhard et al. [10] | 1992 | |
| 4 | Lausten et al. [16] | 1987 | |
| 4 | Lo et al. [18] | 1994 | |
| 6 | Sonne-Holm et al. [23] | 1982 | 6 |
| 6 | Dorr et al. [5] | 1986 | 6 |
| 8 | Emery et al. [8] | 1991 | 8 |
| 6 | Khan et al. [14] | 2002 | |
| 2 | Foster et al. [9] | 2005 | |
| Branfoot (from Parker and Gurusamy [21]) | 2000 | 8 | |
| Harper (from Parker and Gurusamy [21]) | 1994 | 3 | |
| 4.7 | Average | 6.2 | |
| 6.9 | Average minus maximum† | 5.8 | |
* Based on Cochrane 12-point index for methodologic quality of clinical studies; scores on the left represent studies included in this report; those on the right are from the meta-analysis by Parker and Gurusamy [21]; †average of values in which the points given on the Cochrane index were subtracted from the total points possible; for the study by Holt et al., items 1 and 9 in the Cochrane index were not applicable.
Table 2.
Screening and identification of studies to include for analysis
| Type of article | Number of studies |
|---|---|
| Initial search | |
| Review article | 9 |
| Case report | 15 |
| Letter | 1 |
| Mechanical experiment article | 5 |
| Surgical technique article | 1 |
| Experimental article | 1 |
| Multiple publication | 1 |
| Data not extractable | 0 |
| Without population of interest | 22 |
| Without treatment of interest | 38 |
| Without outcome of interest | 4 |
| Meets criteria for further reading | 19 |
| Abstracts for further reading | 4 |
| Total | 120 |
| Secondary screening | |
| Without population of interest | 0 |
| Without treatment of interest | 3 |
| Without outcome of interest | 1 |
| Unable to obtain article | 1 |
| Meets criteria for further reading | 14 |
| Total | 20 |
| Detailed reading | |
| Data not extractable | 4 |
| Abstracts (contacted authors) | 4 |
| Duplicate data | 1 |
| Data appropriate for extraction | 11 |
Two investigators (SP, JS) independently performed blind data extraction for relevant perioperative and postoperative patient factors, including method of randomization, implant type, fixation method, number of patients and hips, gender, age, operative time, blood loss, mortality, all complications, revisions (all procedures for any reason as reported by authors), hospitalization days, discharge disposition, followup, subsidence, radiolucency, heterotopic ossification, hip scores, pain (presence or absence), and use of assistive devices. Methodology quality was assessed (JA, LM) using the 12-point Cochrane system [20, 21].
Pooled data from 11 studies were comprised of 1632 cemented and 981 noncemented hemiarthroplasties (1568 patients in the cemented group and 930 patients in the uncemented group). The average reported age of the patients was 78.9 years for cemented and 77.5 years for uncemented cohorts (n = 7). Males comprised 38.5% and 45.2%, respectively. Outcome variables that were reported in a comparable manner among at least three studies (criteria set a priori) were included in the meta-analysis. Variables such as comorbidities, intraoperative pulmonary emboli, and ASA scores did not meet these criteria. Also implant types were not included for analysis as they were not consistently and unambiguously reported. We compared differences in variables meeting inclusion criteria (perioperative, intermediate, long-term mortality; postoperative complication; pain; revision surgery; estimated blood loss; and operative time) in the cemented and uncemented cohorts using a fixed effects (FE; Mantel-Haenszel) model and a random effects (RE; DerSimonian and Laird) model to control for increased study heterogeneity [3, 18]. The FE model assumes that all studies draw from essentially the same sample and have one true affect; therefore, a single study’s influence on the model is related to the sample size of the study. The RE model assumes that studies draw from different samples and have different true effects (heterogeneity); the influence of one study on the model relies less on sample size contribution but to various factors. The RE model is typically (but not always—see Fig. 1) the more stringent of the two. Increased heterogeneity was tested using the Cochrane Q test with p < 0.10 generally signifying significant heterogeneity) [6]. We used both models because some variables appeared more appropriate for the FE and others for the RE model (according to the Q test) and because the results of the two models could be compared with each other as another gauge of study to study variation; when there is lesser between-study variation, the results of the FE and RE models are similar. Relative risk, p values, and 95% confidence intervals are reported. Analysis was performed with a commercial statistical package (STATA; StataCorp LP, College Station, TX). Significance was set at p < 0.05.
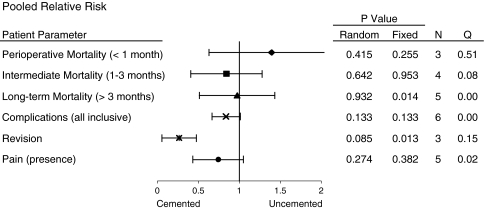
Fig. 1.
The overall pooled relative risk using a RE model is shown. Relative risk (RR) is represented graphically with 95% confidence interval bars. The RR favoring the cemented cohort is left of the vertical bar and the uncemented cohort is on the right. Probability values for RE and FE models and number of studies included in pooled data are shown. Column Q shows the p value of the Cochrane’s Q test for heterogeneity.
Results
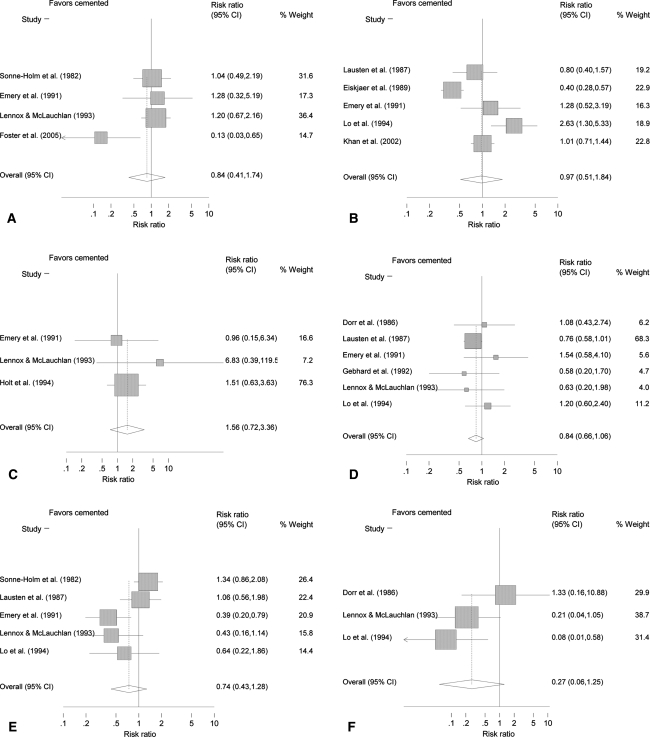
Relative risk of postoperative outcomes for mortality, complications, and pain were similar between cohorts. Mortality rates at intermediate (up to 3 months after surgery) and long-term (6 months or greater) followup (Figs. 1, 2A–B) also were similar (p > 0.05) between cohorts, as was perioperative mortality (less than 1 month) (p > 0.05) (Figs. 1, 2C). Total postoperative complications and persistence of pain did not reach statistical significance between groups (Figs. 1, 2D–E). The revision rate was lower (p = 0.01) for the cemented cohort (Figs. 1, 2F; FE model).
Fig. 2A–F.
Forest plots of the pooled RR for (A) perioperative mortality (less than 1 month), (B) intermediate followup (less than 3 months), (C) long-term followup (6 months and greater), (D) all complications, (E) revision, and (F) pain are shown. Each contributing manuscript (with summary effect at bottom) is shown with 95% confidence intervals for the RR (X axis) and percent weight contributing to the RE model.
Two operative parameters of blood loss and surgical time were lower for the uncemented cohorts (Table 3). The weighted average blood loss was 476 mL for the cemented and 338 mL for the uncemented groups. Surgical time was greater for the cemented cohort than the uncemented (95 minutes versus 80 minutes, respectively) (Table 3).
Table 3.
Pooled demographics and select treatment parameters
| Variables | Cemented | Uncemented | Number of studies | p Value | |
|---|---|---|---|---|---|
| Fixed* | Random* | ||||
| Number of hips | 1632 | 981 | 11 | ||
| Number of patients | 1568 | 930 | 10 | ||
| Average age (years) | 78.9 | 77.5 | 7 | NS | NS |
| Percent male | 38.5 | 45.2 | 5 | NS | NS |
| Length of stay (days) | 19.37 | 19.07 | 3 | NS | NS |
| Operative time (minutes) | 96 | 80 | 5 | < 0.001 | < 0.002 |
| Blood loss (mL) | 467 | 338 | 4 | < 0.005 | 0.071 |
* Cohorts compared using a FE model (Mantel-Haenszel) and a RE model (DerSimonian and Laird); NS = not significant.
Discussion
Accumulating evidence should allow for better outcomes-based decision-making for treatment of hip fractures in elderly patients. Hemiarthroplasty is an often-chosen option for treatment of a displaced intracapsular proximal femoral fracture, but clear guidelines are difficult to establish because of considerable variability in the literature and the dearth of randomized, controlled trials [1, 2, 11, 13, 22]. In this context, we performed a systematic review of prospective and retrospective studies comparing the clinical outcomes (blood loss, operative time, perioperative and postoperative mortality, complications, pain, and revisions) of cemented and uncemented hemiarthroplasty techniques and report the results of a meta-analysis of the pooled data using FE and RE modeling.
As with other systematic reviews, the results are limited by the availability and quality of available data. First, our analysis is limited by the high variability in and between reports used. All but two of our examined patient outcomes (perioperative mortality and revision) had considerable heterogeneity. We attempted to partially account for this by using a random effects model and a standard FE model of meta-analysis. This underscores the need for uniformity in outcomes measurement methods and better controlled cohorts in clinical orthopaedic research. The result will be not only improved studies in general, but also enhanced ability to use studies collectively to obtain valid conclusions. Second, we included (1) a long time (more than two decades); (2) different types of prostheses during that time; and (3) different prostheses in the same study. We believed it important to include these studies (as long as they compared cement versus no cement) spanning decades and including varying implants because they represent our body of literature; these are the papers we turn to when considering the use of cement. By expanding our inclusion, this study represents a systematic analysis of the best our literature has offered on this topic in numbers that make our conclusions useful. The methodologically best study will not yield the best comparison. A randomized trial in which the same prosthesis is implanted with and without cement betrays our current standards of practice, the implantation of a press-fit stem without cement, and the use of a smooth cemented stem with modern cementation techniques. Third, the considerable number of prospective trials published in abstract form only (no full peer-reviewed paper) begs the question of publication bias. The dearth of comparable data points between reports prevented formal evaluation of this bias.
Our analysis suggests increased operative time and blood loss for the cemented technique; one therefore might speculate patients having increased operative times and blood losses would experience a higher risk for early postoperative mortality using this technique although we found no such risk. We found no advantage for either approach regarding mortality at intermediate to long-term followup, postoperative complications, and pain; however, the revision rate was higher using the FE model. In distinction to the suggestions of the study of Parker and Gurusamy [21], our evaluation suggested no difference between the two cohorts regarding postoperative pain.
Despite the limitations, we believe the analysis offers useful conclusions based on available evidence; there were few differences between cemented and uncemented techniques for outcome measurements currently reported in the literature. We found only trends favoring the cemented cohort with regard to middle- to long-term mortality, overall complications, need for revision, and postoperative pain but none were significant and each trend requires further study to confirm or refute. Our data also indicate that despite decades of collective experience, the literature does not provide clear and convincing answers to many questions regarding stem fixation in the treatment of a common orthopaedic injury. We need to more carefully consider issues of long-term outcomes and intraoperative and perioperative factors and report them in a reliable, consistent, and standardized manner.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-008-0368-3) contains supplementary material, which is available to authorized users.
References
- 1.Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a randomized, controlled trial. J Bone Joint Surg Am. 2006;88:2583–2589. [DOI] [PubMed]
- 2.Bhandari M, Devereaux PJ, Swiontkowski MF, Tornetta P 3rd, Obremskey W, Koval KJ, Nork S, Sprague S, Schemitsch EH, Guyatt GH. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck: a meta-analysis. J Bone Joint Surg Am. 2003;85:1673–1681. [DOI] [PubMed]
- 3.Centers for Disease Control and Prevention (CDC). Fatalities and injuries from falls among older adults—United States, 1993–2003 and 2001–2005. MMWR Morb Mortal Wkly Rep. 2006;55:1221–1224. [PubMed]
- 4.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. [DOI] [PubMed]
- 5.Dorr LD, Glousman R, Hoy AL, Vanis R, Chandler R. Treatment of femoral neck fractures with total hip replacement versus cemented and noncemented hemiarthroplasty. J Arthroplasty. 1986;1:21–28. [DOI] [PubMed]
- 6.Egger M, Smith GD, Altman DG, eds. Systematic Reviews in Health Care: Meta-analysis in Context. London, England: BMJ; 2001.
- 7.Eiskjaer S, Gelineck J, Soballe K. Fractures of the femoral neck treated with cemented bipolar hemiarthroplasty. Orthopedics. 1989;12:1545–1550. [DOI] [PubMed]
- 8.Emery RJ, Broughton NS, Desai K, Bulstrode CJ, Thomas TL. Bipolar hemiarthroplasty for subcapital fracture of the femoral neck: a prospective randomised trial of cemented Thompson and uncemented Moore stems. J Bone Joint Surg Br. 1991;73:322–324. [DOI] [PubMed]
- 9.Foster AP, Thompson NW, Wong J, Charlwood AP. Periprosthetic femoral fractures: a comparison between cemented and uncemented hemiarthroplasties. Injury. 2005;36:424–429. [DOI] [PubMed]
- 10.Gebhard JS, Amstutz HC, Zinar DM, Dorey FJ. A comparison of total hip arthroplasty and hemiarthroplasty for treatment of acute fracture of the femoral neck. Clin Orthop Relat Res. 1992;282:123–131. [PubMed]
- 11.Gillespie WJ. Extracts from ‘clinical evidence’: hip fracture. BMJ. 2001;322:968–975. [DOI] [PMC free article] [PubMed]
- 12.Holt EM, Evans RA, Hindley CJ, Metcalfe JW. 1000 femoral neck fractures: the effect of pre-injury mobility and surgical experience on outcome. Injury. 1994;25:91–95. [DOI] [PubMed]
- 13.Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty: treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006;88:249–260. [DOI] [PubMed]
- 14.Khan RJ, MacDowell A, Crossman P, Datta A, Jallali N, Arch BN, Keene GS. Cemented or uncemented hemiarthroplasty for displaced intracapsular femoral neck fractures. Int Orthop. 2002;26:229–232. [DOI] [PMC free article] [PubMed]
- 15.Khan RJ, MacDowell A, Crossman P, Keene GS. Cemented or uncemented hemiarthroplasty for displaced intracapsular fractures of the hip: a systematic review. Injury. 2002;33:13–17. [DOI] [PubMed]
- 16.Lausten GS, Vedel P, Nielsen PM. Fractures of the femoral neck treated with a bipolar endoprosthesis. Clin Orthop Relat Res. 1987;218:63–67. [PubMed]
- 17.Lennox IA, McLauchlan J. Comparing the mortality and morbidity of cemented and uncemented hemiarthroplasties. Injury. 1993;24:185–186. [DOI] [PubMed]
- 18.Lo WH, Chen WM, Huang CK, Chen TH, Chiu FY, Chen CM. Bateman bipolar hemiarthroplasty for displaced intracapsular femoral neck fractures: uncemented versus cemented. Clin Orthop Relat Res. 1994;302:75–82. [PubMed]
- 19.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–748. [PubMed]
- 20.Moja LP, Telaro E, D’Amico R, Moschetti I, Coe L, Liberati A. Assessment of methodological quality of primary studies by systematic reviews: results of the metaquality cross sectional study. BMJ. 2005;330:1053. [DOI] [PMC free article] [PubMed]
- 21.Parker MJ, Gurusamy K. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. 2006;3:CD001706. [DOI] [PubMed]
- 22.Sikorski JM, Barrington R. Internal fixation versus hemiarthroplasty for the displaced subcapital fracture of the femur: a prospective randomised study. J Bone Joint Surg Br. 1981;63:357–361. [DOI] [PubMed]
- 23.Sonne-Holm S, Walter S, Jensen JS. Moore hemi-arthroplasty with and without bone cement in femoral neck fractures: a clinical controlled trial. Acta Orthop Scand. 1982;53:953–956. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.