Abstract
No diploma for orthopaedic surgery is available in the current medical education and licensing system in China. The orthopaedist generally receives on-the-job training in a clinical practice after getting a license to practice surgery. There are multiple training pathways to and opportunities in orthopaedic surgery, and these vary from hospital to hospital and from region to region. These include on-the-job training, academic visits, rotation through different departments based on local medical needs, fellowship training in large general or teaching hospitals (locally, regionally, nationally, or internationally), English language training, postgraduate diploma training, and Internet CME. Due to the current training system, orthopaedic techniques and skill levels vary greatly from hospital to hospital.
Introduction
China is a country with a population over 1.3 billion; however, despite an increase in resources for health, a standardized training program has yet to be developed for orthopaedic surgery. This review will outline the training as currently practiced.
An Overview of Medicine in China
The Chinese medical system includes elements of Western medicine, traditional medicine (traditional Chinese medicine [TCM], Tibetan medicine, Uygur nationality medicine, Mongolian medicine, and medicine of other minorities), and Western medicine plus TCM. The most common of these are Western medicine, TCM, and Western medicine plus TCM. Most doctors, including orthopaedists and nonorthopaedists, come from medical schools (including Western medicine, TCM, and minority medicine), but some traditional practitioners in TCM learn their skills through an apprenticeship with a master. Traditional practitioners may treat fractures or dislocations by manipulation and splinting, mostly in the more remote regions of the country. Generally, there are departments of Western medicine in TCM hospitals and minority medicine hospitals, and vice versa. Most hospitals of TCM now treat patients not only with TCM, but also with Western medicine. The diagnosis is often made with Western medicine, while the treatment is often a combination of TCM plus Western medicine.
TCM and traditional minority medicine are both an integral part of the Chinese culture. The role of TCM in primary healthcare has been recognized by the World Health Organization [22]. TCM emphasizes the attainment of health by maintaining a state of equilibrium between the various systems and functions of the person as a whole, and considers that health depends upon the continuous and unobstructed circulation of blood and “qi” (pronounced “chee,” and often translated as “vital air” or “energy”) throughout the body. TCM practitioners comprise three categories: herbalists, bonesetters, and acupuncturists. For orthopaedic injuries, herbal medicine may be taken orally to restore general health and/or used topically to reduce swelling, improve local blood flow, and recover from soft tissue injury. Bonesetting is used by some to treat fractures and dislocations, and the techniques for manipulation are similar to those in the West; wooden splints are widely used for immobilization in both the Western medical hospitals and the TCM hospitals. If applied too tightly, the use of a wooden splint may be complicated by compartment syndrome (Volkmann’s ischemic contracture) and even limb necrosis. Massage may reduce muscle soreness, and chiropractic care can aid in rehabilitation by working through the spine; many professional athletes rely on chiropractors to aid rehabilitation. Studies show that chiropractic is particularly effective for neck pain/sprain [24] and low-back pain. Acupuncture can regulate the flow of “qi” and blood and bring about powerful therapeutic effects by using the body’s own regulatory systems and self-healing potential. Stimulation of acupuncture nodes with needles, heat, pressure, electricity, or other means initiates a complex cascade of subtle but powerful neural, vascular, endocrine, lymphatic, and immunological responses that result in analgesia, muscle relaxation, enhancement of blood flow to affected areas, normalization of organ activity, reduction of inflammation and swelling, tissue and wound healing, enhanced immune response, increased joint range of motion, stress reduction, and mood enhancement [1]. The practice of minority medicine has similar ideas and principles, and mainly serves the local people with the same language and cultural backgrounds.
Medical Licensing in China
Medical licenses may be categorized as follows: (1) clinical (internal medicine or surgery), (2) traditional Chinese medicine, (3) oral medicine, and (4) public health care. Doctors may be licensed as either “assistant” or “practicing,” depending on their medical education and experience.
Several scenarios may qualify an individual to sit for the national licensing examination for practitioners [10]: (1) The candidate received a medical college education (5 years or more of higher medical education) and has served under the supervision of a medical practitioner for at least 1 year in an institution of medical treatment, prevention, or healthcare; (2) the candidate qualified for a practicing certificate for assistant medical practitioner, has received junior college medical training in an institution of higher learning (3-year secondary medical school education), and has served at least 2 years in an institution of medical treatment, prevention, or healthcare (or has received medical training in a 2-year program in secondary training school and has served at least 5 years in an institution of medical treatment, prevention, or healthcare); (3) to participate in the national license examination for the qualification of assistant medical practitioner, the candidate must have received junior college medical training at an institution of higher learning (3-year secondary medical school education) or received medical training in a secondary training school (2-year secondary medical school education) and served at least 1 year (under the supervision of a medical practitioner) in an institution of medical treatment, prevention, or healthcare; and (4) to participate in either the examination for the qualification of medical practitioner or the examination for the qualification of assistant medical practitioner, the candidate will have studied traditional medicine under a master for at least 3 years (or acquired specialized knowledge of medicine in his career) and is recommended by an organization of the traditional medicine profession or an institution of medical treatment, prevention, or health care which shall be designated by the administrative department of health under the people’s government at or above the county level. The examination contents and form shall be separately fixed by the administrative department of health under the State Council.
Anyone who has passed the examination and been awarded the qualifications as a doctor or assistant doctor may apply to the administrative department of health under the local people’s government at or above the county level for registration [10].
The diploma of assistant surgeon allows the surgeon to practice under the supervision of a practicing surgeon. The assistant surgeon cannot prescribe medicine and perform surgery independently. Graduates from higher medical education (universities, colleges, schools, including TCM and minority medical education) can take the national examination for a diploma of surgery if he or she majored in Western medicine (generally speaking, but it is not absolutely required because the law does not say that in detail [10]), get a graduate certificate in clinical medicine, and find a position in a department of surgery or subspecialty in a hospital. The contents of the national license examination for clinical practitioners are the same for all participants applying for a diploma in specific areas. For example, the exams for surgery, internal medicine, orthopaedics, and other subspecialties of surgery such as cardiology, and other subspecialties of internal medicine such as emergency, obstetrics and gynecology, ear-nose-throat disorders, ophthalmology, etc., would be identical.
To perform surgery, one must possess a diploma of surgery. This document is only valid in the hospital where the practitioner works. In order to perform consultations or surgery at another institution, permission must be granted from the primary institution. If a surgeon has a diploma in surgery, he or she can legally perform any type of surgery (eg, general surgery, neurosurgery, orthopaedic surgery, urological surgery). No subspecialty licenses or certificates are available. While some surgeons may become subspecialized, all will assist their colleagues in performing procedures from the range of subspecialties. Medical school graduates are employed in a hospital; those working in the department of orthopaedic surgery are considered orthopaedic surgeons, while those working in the department of general surgery are general surgeons, and so on. The administrative authority of each hospital is most powerful in determining each doctor’s scope of practice. In underdeveloped and/or remote areas with limited human resources, the assistant surgeon can perform surgery (and prescribe medicine) under the supervision of the local hospital administration. In some areas, doctors who have not been formally credentialed nonetheless perform surgery.
At the county-level facilities, musculoskeletal trauma care is generally provided by the department of surgery, although an independent department of orthopaedic surgery may be present in some economically advanced areas. Orthopaedic specialists are found at most hospitals above the township and county levels, and there is often an independent department of orthopedics specializing in musculoskeletal trauma care.
There are an increasing number of private orthopaedic hospitals. In 2006, there were 271 orthopaedic hospitals (57 government funded, 37 community funded, 6 jointly funded by government and another investment source, 131 privately funded, and 40 other sources) [18]). The large majority of orthopaedic surgeons, however, work in state-owned Grade III general hospitals (over 500 beds) and some well-developed Grade II hospitals (100–499 beds), and are generally more experienced and skilled than those in underdeveloped Grade II hospitals and Grade I hospitals (20–100 beds). The government-owned hospitals still deliver the large majority of musculoskeletal trauma care in China.
Medical Education and Pathways for Surgical Training
By the year 2000, there were 177 higher medical schools (universities and colleges including TCM, minority medicine), 714,800 students, and 489 secondary medical schools [15]. In 2005, there were four higher minority medical colleges, including two Tibetan medical colleges, one Mongolian medical college, and one Uygur medical school. Departments of traditional minority medicine (Tibetan medicine, Zhuang medicine, and Mongolian medicine) are included in some traditional Chinese medicine colleges [7]. Training in TCM is required in the Western medical schools, and Western medical sciences are taught at both TCM schools and minority medical schools. In 2006 there were 1,384,488 students [17].
There are three stages in mainstream medical education: premedical school, medical school, and postmedical school including postgraduate education and continuing medical education. This is similar to other higher education programs in science, industry, agriculture, and other disciplines.
The first stage is premedical education, also known as primary education, which includes preschool (ages 3–6 years), primary school (ages 5–12), and high school (ages 13–18). After graduation from high school, based on national higher education admission examination scores (and the student’s interests), students can enroll in a university, college, or medical school (including TCM or minority medicine).
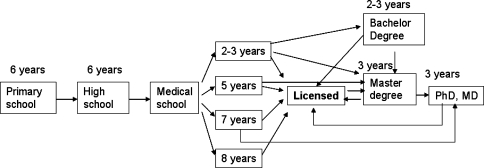
For doctors, the next stage is a secondary medical school education (including TCM and minority medicine). Minority medical schools are generally open only to students of that minority, and the graduates ultimately serve local patients with the same cultural background. Several pathways for higher medical education are possible, namely a 2-year or 3-year education in a secondary medical school, or a program with 5 to 8 years of higher education in a university (Fig. 1). Admission to a specific program is based on the national higher education admission examination scores; higher scores are associated with the opportunity to train in better institutions, and graduates from higher medical universities typically have better opportunities for both employment and seeking further education. Generally, large general hospitals (Grade III and some Grade II hospitals) in urban areas would rather not have graduates from secondary medical schools, unless there is a previous relationship between the individual and the institution.
Fig. 1.
The medical education flow in China is shown.
In the 2-year secondary medical schools (Yi Xue Zhong Zhuan Jiao Yu), 1.5 years are spent on didactic learning, with 6 months reserved for an internship. One year after graduation, with work experience in a medical facility, the graduate can take part in the examination for getting an assistant doctor license. If the graduate works in a department of surgery, the license he or she applies for is diploma of assistant surgeon. After getting the license of assistant surgeon, the graduate has to work 5 more years in medical facilities, and then can apply for the national license examination to be a practicing surgeon.
In the 3-year secondary medical school education (Yi Xue Da Zhuan Jiao Yu), 2.5 years are spent on didactic information, followed by a 6-month internship. If the student passes the school’s graduation examination, a graduate certificate is awarded to find a job, or the student may wait for the permission to take part in the national license examination for clinical practice. One year after graduation, with 1 year experience in a medical facility, a graduate from a 3-year secondary medical school can take the examination for getting a license as an assistant doctor. If the graduate works in department of surgery, they are granted the diploma or license of assistant surgeon. After getting the license of assistant surgeon, the graduate has to work 2 more years, and then applies for the national license examination to be a practicing surgeon.
Graduates from a secondary medical school may also earn a bachelor’s degree in medical science with 2 to 3 years of school or by correspondence learning from a higher medical university. After getting the bachelor’s degree and completing 1 year of work in a medical facility under the supervision of a senior surgeon, the graduate is eligible to take the national license examination for a practicing surgeon.
The 5- to 8-year program of higher medical education includes 4 years of didactic learning, followed by a 1-year internship in a hospital. The graduate from a 5-year higher medical university has to work 1 year in a department of surgery under a senior practicing surgeon’s instruction, and then take the national license examination to become credentialed as a practicing surgeon. The graduate can also go on directly to postgraduate education for a master’s degree in medical science in a 3-year program. Upon completing the program, the postgraduate is eligible to take the national license examination to be a practicing surgeon in the same year, or he or she may continue for 3 more years for a doctoral degree (PhD or MD). After getting a PhD or MD degree, the postgraduate can take part in the national examination to be a practicing surgeon in the same year. The 7- and 8-year programs are generally only offered at some of the elite medical universities. The first 5 years of these programs are similar to the 5-year program of education, but in the added 2 or 3 years the student will select a subspecialty under a senior practicing surgeon’s instruction, take part in clinical practice, and do some medical research. The graduate from the 7-year program earns a master’s degree in basic scientific research. The graduate from the 8-year program earns an MD degree.
Didactic education in orthopaedics varies from school to school, from about 16 class hours in the 3-year secondary medical education, to 20 to 34 class hours in 5-year medical school education, and 44 class hours in the 7- to 8-year medical school education [2–6].
The third stage is postgraduate medical education (Yan Jiu Sheng Jiao Yu, including TCM, minority medicine), either a master’s degree program or a doctoral degree program. The candidate for the master’s degree can be a graduate from a 5-year higher medical education university with a bachelor’s degree or a graduate from a 2- or 3-year secondary medical school with 2 years’ work experience. The candidate for the doctoral degree will already have a master’s degree. A surgeon who has worked with a bachelor’s degree after graduation can only take part in the examination of the master’s program after 2 years of working experience in a medical facility. Policies for enrollment vary between medical universities.
Alongside economic development and an expansion in the need for healthcare services, higher medical school education enrollment increased from 35% in 1999 to 52% in 2005, postgraduate education enrollment increased from 3% in 1999 to 8% in 2005; however, secondary medical school education enrollment decreased from 62% in 1999 to 40% in 2005. Overall, these changes have generally improved the quality of staff in the medical service system [15]. In order to retain medical staff in rural areas, students from poor areas are encouraged to go back to work for the medical service system in those areas by reducing their school (or tuition) fees.
Continuing Medical Education for the Nonorthopaedist and Orthopaedist
After graduation from medical school, doctors are typically employed by a hospital. If there is a need for an orthopaedist, continuing medical education in orthopaedics will begin once they are posted at that facility.
Prelicense CME education
Prelicense CME education generally is for doctors who work at the grassroots level, including community and/or rural medical service. The education is based on the Law of China on Medical Practitioners (as of May 1, 1999). The curriculum includes general medical theory in all medical disciplines, laws on practicing medicine, and related clinical procedures. The doctors must be completely or partially released from regular work to receive this job training. The participants take an organized examination after completing their education. Upon passing this examination they are certified as a general practitioner working in community medical service and rural medical health service. In this way, a basic health service with prevention, medical treatment, healthcare, rehabilitation, health education, and family planning services can be provided for the communities and rural areas with good quality and stability. It is an effective way to adequately staff the more rural health facilities with general practitioners [8].
Hospital-based Education in Musculoskeletal Care
For on-the-job training and academic visits, doctors are trained to master the three “basics” (basic theory, basic techniques, and basic knowledge) in the specialty in which he or she works. Surgeons are encouraged to take part in the CME programs sponsored by the Chinese Medical Association (CMA), such as the Orthopedic Society of CMA, to obtain “learning scores” each year. These CME activities are self-funded. Doctors are also encouraged to participate in the academic activities in their hospitals. The senior practice surgeon in their department instructs and supervises the new surgeon in practice for about 3 to 6 months, and then the new surgeon independently improves their skills under the leadership of the director. However, in the operating theater the situation varies between different hospitals and different surgeons. If the senior surgeon always chooses to be the primary surgeon, then the apprentice surgeon may find it difficult to develop hands-on skills and to improve professionally. If the hospital has rotation training requirements, then the new surgeon will be required to finish the rotation training before moving on to a subspecialty. Experts from larger hospitals with or without a university affiliation are frequently invited for lectures or workshops on selected subjects and to instruct trainees in patient consultation and some basic surgery. Most orthopaedists and nonorthopaedists begin professional training through these invited experts. In some municipal hospitals and most county hospitals, the surgeons are trained in multidisciplinary surgery at the beginning.
Most hospitals now have a rotation training system for newly arrived surgeons (residents). The organization and length of the in-hospital rotations vary between individual facilities and regions of the country. Rotations in a selected department are based on the needs of the local hospital and area. In town- and/or county-level hospitals (Grade I and some Grade II hospitals), rotations in the departments of emergency medicine, internal medicine, surgery, obstetrics and gynecology, and pediatrics are required. In the department of internal medicine, all the subspecialties, such as pulmonary disorders, cardiovascular disorders, endocrine and nutritional disorder, gastrointestinal disorders, neurological disorders, etc, are covered. In the department of surgery, all the subspecialties, such as trauma, general surgery, orthopaedics, chest surgery, neurosurgery, urologic surgery, etc, are covered. The total rotation time is 1 to 2 years.
In large municipal or provincial general hospitals (Grade III and some Grade II hospitals), the rotation time is 2 to 3 years based on the local needs of the hospital. Rotations include the departments of emergency medicine, general surgery, orthopaedics, chest surgery, urologic surgery, cardiovascular disorder, pulmonary disorders, gastrointestinal disorders, and neurological disorders. In each rotation, residents work under the supervision of senior practicing surgeons in each department. The rotation provides the residents experience in dealing with diseases in other specialties and gives residents a wide base for future specialization. During each rotation residents learn the work flow of the hospital in different departments and the relationship among different departments familiarizes them with all staff in the same hospital and allows them to develop colleagues for the future. The rotations allow the staff an opportunity to get to know the trainees and to provide the leader of the hospital with sufficient information to generate a letter of recommendation for future specialty arrangements.
In August 2007, a trial national standards on specialty residents training was put into effect by the Ministry of Health of China, and at the same time, the standards of training bases (centers) were also put into effect by the Ministry of Health [19, 20, 23].
National Standards and Requirements for Surgical Training
In the new trial standards, surgical training requires residents to have completed 5 to 8 years higher medical school education. These individuals will receive surgical training for 3 years, through subspecialty rotations, at a training center designated by the Ministry of Health (Table 1) [23]. Rotations through the surgical subspecialties including general surgery, orthopaedics, urology, chest-cardiovascular surgery, neurosurgery, anesthesiology, intensive care, and emergency medicine provide the residents with an understanding of the pathogenesis, clinical manifestations, diagnosis, and treatment principles for common conditions seen in each surgical subspecialty. This approach provides a strong foundation in the basic knowledge and techniques for future career development and better trauma care service.
Table 1.
Rotation time in related departments for the training of surgeons in China
| Department | Duration (months) |
|---|---|
| General surgery | 15 (including 3 months outpatient department rotation under the instruction of senior surgeons) |
| Orthopaedics | 6 (including 1 month outpatient department rotation under the instruction of senior surgeons) |
| Urology | 3 |
| Chest/cardiovascular surgery | 3 |
| Neurosurgery | 3 |
| Anesthesiology | 2 |
| Surgical intensive care unit | 1 |
| Surgical emergency room | 3 |
| Total | 36 |
Trial Standards and Requirements for Orthopaedic Specialist Training
These new standards and requirements are just beginning during a trial period in very few selected areas and hospitals, and are not widely in effect in China [20]. The duration of training is 3 years. The resident should have finished the 3 years of surgical training, and can then continue further orthopaedic specialist training by rotation in subspecialty areas within a department of orthopaedics. The rotation arrangement in the first year is: 1 month in the plaster room, 2 months in the outpatient department, and 3 months each in spine, trauma, and osteopathy.
The resident should have a good mastery of basic theory and knowledge of orthopaedics, including commonly used treatments and operative procedures in trauma (fractures and dislocations), principles of open wound débridement and closure, skills and principles of prevention and treatment of complications in casting, tourniquet usage, local injection, arthrocentesis, skeletal traction, and internal fixation.
The resident should master skills required for orthopaedic examination for lumbar disc herniation, cervical spondylosis, arthritis, bone and joint infection, and bone tumors, and should also know orthopaedic-related imaging and laboratory tests well. The resident should understand the pathogenesis, clinical manifestation, diagnosis, and differentiation, treatment principles of common orthopaedic ailments, débridement of hand injury, skin defect repair, tendon repair, and skeletal internal fixation.
During the second and third year of orthopaedic training, the resident rotates through the subspecialties, with 7 months each in spine, osteopathy, and trauma, and 3 months in the outpatient department. The following standards apply [20].
In the last 2 years, the resident should master anatomy, histology, embryology, physiological and biochemical knowledge of the musculoskeletal system, and the effects, side effects, and dosages of commonly used drugs in orthopaedics and how to properly prescribe them. The resident should understand diagnostic techniques such as reading orthopaedic imaging films for common orthopaedic disorders. The resident will be able to independently treat soft tissue and hand injuries, including débridement, skin graft harvesting, free skin graft, skin flap, and basic vascular repair. The resident will be able to treat fractures and dislocations (including closed reduction, external fixation, perform open reduction and internal fixation, and apply an external fixator). The resident should have a mastery of the clinical manifestations, diagnosis, differentiation, nonoperative and operative treatment principles and preventive protocols of common orthopaedic disorders and some difficult and complex disorders (such as spinal and joint degenerative disorders, infectious disorders, neoplasms, bone and joint deformity). The residents should have good skills in routine preoperative preparation and postoperative management.
The resident should know common operative approaches, techniques, management of complications, biomechanics, and biomaterials.
The resident should know the rehabilitation regimen for common orthopaedic disorders.
Residents are required to read medical literature in other languages such as English fluently. The resident should have abilities in reading, writing, listening, and speaking in English.
Fellowship Training in Large General or Teaching Hospitals (locally, regionally, nationally, or internationally)
Most surgeons in China are fellowship-trained for a specialty practice such as orthopaedics. The time of fellowship training varies from 3 months to 1 year based on a selected field, but most programs are available for 1 year. Specific arrangements differ between institutions. In the department of orthopaedics at Xijing Hospital (the author’s hospital), Huang et al. [9] analyzed the diploma of the fellows in 5 years: 13% of the fellows had secondary medical education (2–3 years) diploma, 84% had higher medical education (5 years) diploma, and 3% a postgraduate diploma. As for the original position, 79% were orthopaedists, 18% had other surgical experience, and in 3% the trainees had performed no prior orthopaedic surgery. Sixty-five percent of the fellows came from county- or city-level hospitals (Grade II hospitals) and 35% from provincial hospitals. Seventy-five percent had worked for over 3 years in orthopaedics. Supervisors must pay close attention to the differences between trainees and arrange specific tailored programs. Some hospitals have introduced specific training guidelines, but in reality, it is difficult to ensure they are followed owing to busy daily work.
Fellowship training may take place in a large local, regional, or national hospital, or internationally, and international fellowship training generally requires the strong support of a sponsor and financial support from industry.
English Training
To improve communication (and promote the exchange of ideas) with surgeons from other countries, English language skills are more important in China than ever before. In some large or teaching hospitals, selected educational activities are held in English. Some surgeons attend formal education in English for 3 to 6 months.
Postgraduate Diploma Training
The surgeon (assistant or practicing surgeon) with a lower diploma, such as a bachelor’s degree or with 2–3 years secondary medical school, can apply for a 3-year program leading to a postgraduate diploma (master’s degree or doctorate) in teaching hospitals affiliated with a higher medical university. The first year involves didactic education, while the second year involves clinical rotations in a department of orthopaedics. The third year involves research. The best way to find a position in a good hospital is to complete such a program; individuals who have previously worked in smaller hospitals in remote areas rarely return to the more rural communities. Therefore, hospitals in remote areas lose staff as time goes on and generally, the authorities at these local hospitals may restrict entry of newly arrived surgeons into these postgraduate programs, unless the surgeon signs an agreement to return to the original hospital after their training. Surgeons already working in large general hospitals in large cities often do not want to take part in the postgraduate program of another medical university-affiliated hospital, as they may lose their positions after graduation because the previous position has been taken by another surgeon. Recently the government has addressed this at the policy level, and individuals will be able to return to their original hospital after graduation. Some higher medical universities have an on-the-job postgraduate training program for surgeons working in their hospitals who do not want to lose their positions (and, of course, hospitals do not want to lose qualified surgeons). Through this sort of program, the surgeons can receive higher postgraduate diploma training without losing official contact with their hospital. The program can be instituted full time or with partial release from the usual work. At present, more and more postgraduates finishing such programs have difficulty in finding employment in large hospitals within cities.
Internet CME
The Internet may be used as a (1) rapid reference, (2) a large-volume library, (3) for asynchronous communication, and (4) for synchronous communication. The Internet has value as a journal library because the volume and indexing required cannot be matched in paper libraries. Asynchronous communication includes bulletin board, forum, Wiki, and other similar formats, and can be used for any purpose, including online orthopaedic interactive training. Orthochina.org is a successful web forum for continuing education and debate [11–14, 25]. Orthochina.org is a password-protected, interactive Web site open to (identity-confirmed) orthopaedic surgeons for case discussions and orthopaedic information sharing (electronic textbooks, videos, orthopaedic images, papers, and failures in practice). It has been online for 10 years. As of December 31, 2007, there were 33,984 registered users, of which 9,759 had passed the confirmation procedures. An average of 208 registrants visit daily. The average number of first page clicks is 4,248 clicks per day, and the average number of posts is 75 per day. The orthopaedist can gain experience dealing with difficult cases from many sources (other orthopaedists online, relevant orthopaedic textbooks, papers, and videos) by just staying at home or at work.
A new Wiki, Orthopaedia, (www.orthopaedia.com) is being hosted by the Association of Bone and Joint Surgeons and could potentially be used to distribute information relevant to low- or middle-income countries. The Stryker orthopaedic hyperguide (http://www.ortho.hyperguides.com/) is a password-protected educational resource that could be used to improve access of orthopaedic information for education.
Interactive online case discussion is the most important, easiest, closely-related with learners’ clinical practice, cost-effective method of CME, allowing orthopaedic surgeons to conveniently follow distant case discussions from their homes anywhere, anytime. The participants can be teachers and/or learners at the same time.
Training to Serve the Needs in Rural and Remote Areas
Beginning in 2005, the Ministry of Health of China organized a project called “10,000 doctors go to work in rural hospitals to help and improve the health system” [16]. In this program, from 2006 to 2008, 10,000 doctors in large city hospitals are or will be sent to work in rural hospitals, especially in the areas in the poor western and eastern part of China, to improve the local health system. Orthopaedic surgeons are part of the main work force in the program. When the doctors from cities work in rural areas, the local healthcare system is supported and improved in work staff. Local surgeons can learn from lectures, patient consultations, and by observing procedures presented by surgeons from large city hospitals.
From 2001 to 2005, the Ministry of Health of China, with cooperation from the Ministry of General Logistics of the People’s Liberation Army of China, started a project called “100 military hospitals help 105 county hospitals in western areas based on one-to-one policy” [21]. In the program, the military hospital sent doctors to work in county hospitals, and donated free instruments and equipment for county hospitals. The doctors in county hospitals can also have fellowship training in the corresponding military hospital. The authors have worked in two hospitals in this program. In 5 years, 1255 medical teams and 9093 individuals from military hospitals worked in county hospitals.
Advancement/Promotion within the Field of Orthopaedic Surgery
In the Chinese medical system, a mechanism for promotion operates throughout the working life of an orthopaedist. Stages include intern, resident, general resident or chief resident (Zong Zhu Yuan Yi Shi in Chinese), surgeon in charge (Zhu Zhi Yi Shi in Chinese, corresponding to lecturer in a teaching hospital affiliated to medical university), associate chief surgeon (Fu Zhu Ren Yi Shi, corresponding to associate professor in teaching hospital affiliated to medical university), and chief surgeon (Zhu Ren Yi Shi, corresponding to professor in teaching hospital affiliated to medical university). Requirements for promotion vary between individual facilities and different regions. The orthopaedist has to pass tests in both English competency and computer skills, have demonstrated adequate skills in clinical practice, and should have published papers. Despite the same title of “orthopaedist,” practitioners vary greatly in their level of skills and experience. For example, the chief surgeon at a county hospital might have less experience than a resident in a large university-affiliated hospital.
Discussion
Currently, the Chinese medical system includes elements of Western medicine, traditional medicine, and Western medicine plus TCM due to its large population with different cultures and languages. Accordingly, medical school education and training programs address these varied demographics with varying levels of quality.
No diploma for orthopaedic surgery is presently available from the medical education and licensing system in China and so the question arises of what is an orthopaedist? What should an orthopaedist know? What can the orthopaedist do? How should the orthopaedist be trained? Chinese law regarding medical practitioners does not address these questions nor does it supply any guidelines. Even now, the national licensing examination for medical practitioners is identical for all specialties and/or subspecialties of clinical medicine. Based on the law, if an applicant has successfully passed the national licensing examination and found a hospital for registration, then he or she may perform any surgery, or any procedures in clinical practice regardless of whether he or she is a surgeon or internal medicine physician. With current social and economic developments, more fields have been professionalized, but in China, medical doctors are still not trained and certified in subspecialties. The medical schools need more standardized programs to qualify physicians to practice medicine in a specialty or subspecialty.
The orthopaedist generally receives on-the-job training in a clinical practice after obtaining a license to practice surgery. The hospital’s administration has the power to decide if a medical school graduate becomes a surgeon in a particular area or an internist; the graduates themselves have no power to make that decision. The graduates can express their willingness to be orthopaedists, but the decision is not in their hands. There are multiple training opportunities in orthopaedic surgery, and these vary from hospital to hospital and from region to region. The hospital’s administrative authorities are the only deciding factor in the fate of orthopaedists.
Variations in training pathways have resulted in considerable variability in knowledge, skills, and level of experience between health professionals including orthopaedic surgeons. As such, the quantity and quality of services delivered may vary widely. The government has recognized these disparities and has organized the Chinese Medical Doctor Association, and edited a trial version of standards and requirements for orthopaedist training in limited areas, and limited hospitals, but it is still a very long way to go to make the trial version of standards applicable nationwide. This template will undoubtedly evolve over time, and should help to standardize the education of practitioners at the different levels of education. It is hoped that before a graduate goes to work in a hospital, he or she has been well-trained in orthopaedics, but due to the current managing system even the well-trained orthopaedist may not find a position. The on-job training also varies from hospital to hospital due to the administrators’ role in arranging such instruction. Those who have a good relationship with the administrative authorities will have better opportunities to receive training. No nationalized standard of orthopaedic training is yet available. Orthopaedic training protocols should range from basic musculoskeletal care (such as fracture, dislocation, bone and joint infection, hand injury) to advanced treatment strategies (joint replacement, complex fracture such as pelvic fracture or spine fracture, spinal and bony deformity, spinal degenerative disease, etc.). The medical system should be reformed with subspecialty diploma requirements, such as in orthopaedics, and the student physician should have more control in making his or her career decisions. When diplomas are granted in subspecialties such as orthopaedics, training will follow. We believe that the delivery of specific services should be regulated, based on the level of education of the orthopaedic surgeon and the capacities of the treatment facility.
Acknowledgments
We thank Dr. David A. Spiegel for inviting the first author to participate in the ABJS-Carl T. Brighton Workshop on Musculoskeletal Trauma in The Developing World. We thank the editors of CORR for reviewing, editing, and rewriting the manuscripts the authors submitted.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Reference
- 1.Acupuncture orthopedics, injury recovery, pain relief, stress reduction, sports medicine, internal medicine. Available at: http://www.essentialhealthcare.com/welcome.html. Accessed on May 24, 2008.
- 2.Arrangement standards in teaching surgery in Fudan University. Available at: http://www.jwc.fudan.edu.cn/kcjs/2005/yj/356.007.2.doc. Accessed on December 22, 2007.
- 3.Arrangement standards in teaching surgery in School of Basic Medicine, Peking Union Medical College. Available at: http://222.28.170.153/jiaoxue/jiaoyujiaoxue/kecheng/dagang/linchuangyixuedagang/waike.doc. Accessed December 22, 2007.
- 4.Arrangement standards in teaching surgery in Shenyang Medical University. Available at: http://202.112.29.197/wk/ArticleShow.asp?ArticleID=582. Accessed on December 22, 2007.
- 5.Arrangement standards in teaching surgery in Wannan Medical University. Available at: http://61.191.208.243/lcyxx/linchuangjiaoxue/jiaoxuedagang/waike.htm. Accessed on December 22, 2007.
- 6.Arrangement standards in teaching surgery in Zhongshan University. Available at: http://202.116.64.61/waikexue/jxnr/jxnr2/jxdg2007/jiaoxuedagang.htm. Accessed on December 22, 2007.
- 7.Chu Guo-Ben. Medicine of minorities in China. J Med Pharm Chinese Minorities. 2006;12:1–4.
- 8.He HY. Exploration of continuing education mode of medical workers in our country. Ji Xu Jiao Yu Yan Jiu (Continue Education Reseach). 2007;27:12–14.
- 9.Huang LY, Hu YY, Jia Y. Clinical education for orthopaedic fellow. J Shanxi Med Univ (Basic medical education edition). 2006;8:178–180.
- 10.Law of the Peoples Republic of China on Medical Practitioners. Chinese J Geriatr Dent. 2003;1:123–126.
- 11.Ma ZS, Qiu Y, Zhang HJ, Wang YH. Internet online discussions of a case with scalded scoliosis. China J Orthop Trauma. 2001;14:439–440.
- 12.Ma ZS, Zhang HJ, Wang XB, Wang YH, Yang-Jun, Wang J, Gao DH. Application of internet in orthopaedics. J Fourth Mil Med Univ. 2001;22:2104–2107.
- 13.Ma ZS, Zhang HJ, Wang XB, Wang YH, Yang-Jun, Wang J. Online case discussions of multi-fractures. China J Orthop Truama. 2001;14:52.
- 14.Ma ZS, Zhang HJ, Wang XB, Wang Yong-Hua, Yang-Jun, Wang J, Gao DH. Establishment and introduction of the web on orthopaedics in China. (http://www.chinaortho.org). Chin J Traumatol. 2001;17:511–512.
- 15.Ministry of Education of China. An outline of Chinese medical education reform and development. Medical Education (China). 2001;5:1–6.
- 16.Ministry of Health of China. 10,000 doctors go to work in rural hospitals to help and improve the health system. Available at: http://www.moh.gov.cn/newshtml/10093.htm. Accessed on December 22, 2007.
- 17.Ministry of Health of China. Medical education and scientific research. In: China Annual Health Statistics Book of 2007. 1st edition. Beijing, China: China Union Medical College Press; 2007:327.
- 18.Ministry of Health of China. Medical facility. In: China Annual Health Statistics Book of 2007. 1st edition. Beijing, China: China Union Medical College Press; 2007:6.
- 19.Notice for printing and distributing the draft of specialist training standards and training base standards by the post-medical-school medical education committee. Available at: http://www.moh.gov.cn/newshtml/19799.htm. Accessed on December 20, 2007.
- 20.Qiu GX, Jin J, Yu B. Detailed requirement of orthopaedist training. In: Post-medical-school Medical Education Committee, eds. The Draft of Specialist Training Standards. 1st ed. Beijing, Peking Union Medical College; 2007:282–286.
- 21.Summary of “100 military hospitals help 105 county hospitals in western areas based on one-to-one policy”. Available at: http://www.hnyywsw.gov.cn/article/news_view.asp?newsid=3618. Accessed on December 22, 2007.
- 22.Vuori H. The World Health Organisation and traditional medicine. Community Med. 1982;4:129–137. [DOI] [PubMed]
- 23.Wang B, Jiang KW. Detailed requirement of surgeon training. In: Post-medical-school Medical Education Committee, eds. The Draft of Specialist Ttraining Standards. 1st ed. Beijing, Peking Union Medical College; 2007:24–33.
- 24.Woodward MN, Cook JC, Gargan MF, Bannister GC. Chiropractic treatment of chronic ‘whiplash’ injuries. Injury. 1996;27:643–645. [DOI] [PubMed]
- 25.Zhen-Sheng M, Hong-Ju Z, Tao Y, Gang R, Guo-Sheng D, Yong-Hua W. The OrthoChina project. J Bone Joint Surg Br. 2007;89:717–720. [DOI] [PubMed]