Abstract
Equinovarus of the foot is the most common lower extremity deformity following traumatic brain injury. We evaluated outcomes of the split anterior tibialis tendon transfer (SPLATT) for correction of equinovarus in 47 patients with hemiplegic traumatic brain injury and specifically studied differences in outcomes with two tendon fixation techniques. Seventeen patients constituting Group I underwent fixation with one technique and 30 constituting Group II had another technique. Patients in both groups had appropriate procedures based on dynamic electromyography and gait analyses. Both groups were demographically comparable. All 47 feet were corrected to plantigrade position. Thirty-six of 47 patients became brace-free at final followup. There was a notable decrease in the use of ambulatory aids and ambulatory status improved in both groups. There were three fixation-related complications in Group I and none in Group II. Surgical correction of the spastic equinovarus with SPLATT, in the appropriate patient, with or without associated tendon procedures helps to achieve and maintain correction, improves the ambulatory status of the patient, and eliminates the need for bracing in as much as 77% of patients. We recommend the Group II construct owing to the considerably lower complication rate.
Level of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Each year, approximately 1.5 million Americans sustain a traumatic brain injury (TBI). Approximately 5.3 million Americans currently live with disabilities resulting from TBI. One in four adults with TBI is unable to return to work 1 year after injury, and patients with TBIs requiring hospitalization cost the nation approximately $56.3 billion each year [1, 16].
Although cognitive deficits in TBI are most pervasive, physical deficits also occur. The most common deformity noted in the lower extremity after hemiplegic TBI or stroke is the spastic equinovarus foot (SEV), which is a well-recognized cause of functional disability in the survivors of hemiplegic TBI [3, 9, 10]. Brace wear often is difficult or impossible secondary to the dynamic forces of spastic muscles and the static soft tissue contractures that may develop with time.
Perry and Garrett originated the surgical procedure of split anterior tibialis tendon transfer (SPLATT) for spastic varus hindfoot and initially reported its use in children with cerebral palsy [5]. Success of surgical correction for SEV in hemiplegic stroke is well known [2, 6, 9, 11, 12, 15]. Success of this procedure in adult patients with TBI also has been established [7, 8, 10]. However, little attention has been devoted to analyzing the type of tendon fixation and tendon-routing and its tunnel characteristics. The senior author (MAK) has been using a technique of dorsoplantar routing of the tendon through the cuboid tunnel with biointerference screw placement, which has been modified to lateromedial routing of the tunnel and similar fixation in recent years. Conceptually, lateromedial routing of the tendon in the cuboid shows the biomechanical advantage of this construct. Moreover, posteromedial angulation of the tract offers two distinct advantages: (1) better pullout resistance because there is more angulation at the insertion; and (2) a longer bony canal and therefore a larger surface area for tendon healing to bone and better tract for screw placement (Fig. 1). Also, when analyzed by vector forces, Construct 2 has two distinct advantages: (1) the resultant vector force exerted by Construct 1 at the interface point tends to constantly pull out the tendon from its new insertion unlike in Construct 2; and (2) the net eversion force created by Construct 2 is greater than that of Construct 1 thereby helping to better correct the varus and inversion (Fig. 2).
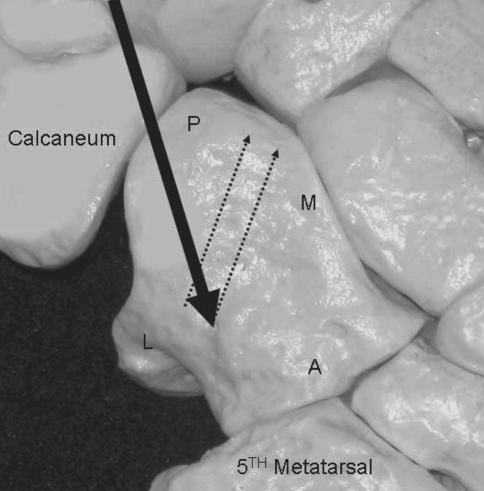
Fig. 1.
Tendon routing and tunnel placement for SPLATT Construct 2 (lateromedial routing) are shown. The split tibialis anterior tendon is indicated with the bold black arrow. The tunnel tract runs posteromedially into the cuboid and is indicated with dotted lines.
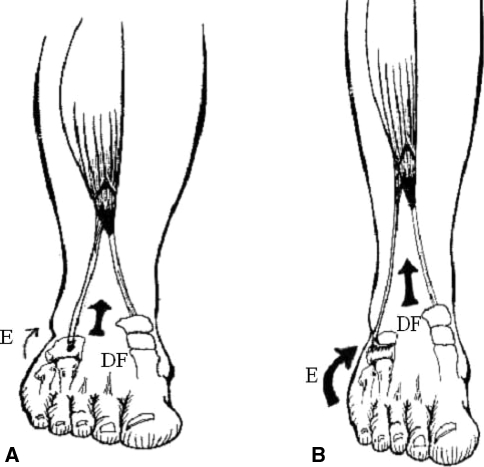
Fig. 2A–B.
The illustrations show the split anterior tibialis tendon transfer procedure using (A) Construct 1 (dorsoplantar routing) (dorsiflexion force [DF] is indicated by the bold black arrow and the small arrow [E] represents the eversion force) and (B) Construct 2 (lateromedial routing) (DF [bold arrow] represents the dorsiflexion force equivalent to that in Construct 1, whereas E [bold arrow] represents eversion force greater than in Construct 1).
Considering this, we asked the following question: Is there any difference in outcomes related to the tendon routing, tunnel placement, and fixation technique used for the SPLATT procedure? We hypothesized that lateromedial routing with interference screw fixation of the split tibialis anterior tendon is biomechanically and clinically superior as compared with dorsoplantar.
While evaluating the outcomes of the fixation techniques, we also reviewed the long-term outcomes of using screw fixation for SPLATT in SEV and present this series of adult patients with spastic hemiplegic TBI treated at a tertiary-level neuroorthopaedic center by one orthopaedic surgeon.
Materials and Methods
This study is a retrospective review of medical records from a tertiary-level neuroorthopaedic center. After appropriate Institutional Review Board approval was obtained, the surgical database from 1998 to 2005 of our senior author (MAK) was reviewed. The initial search of the database identified 47 consecutive patients with hemiplegic TBI with SEV who underwent SPLATT with or without additional procedures. Mechanisms of injury included motor vehicle accidents (35), gunshot injuries (six), and other mechanisms (six patients). The mean time since injury was 18 months (range, 11–48 months).
Patients were included in the study if they underwent SPLATT, surgery was performed by the senior author (MAK), and patients had a TBI resulting in SEV. In addition, all patients underwent inpatient rehabilitation including activity modification and environmental modification and education. All patients were seen in followup at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months after surgery and then annually thereafter.
Patients were excluded from the study if their SEV did not result from a TBI, they did not have preoperative dynamic electromyography (EMG) and gait testing, and did not return for followup.
Data parameters collected from the patients’ preoperative medical records included age, gender, ethnicity, mechanism of injury resulting in TBI, mean time since injury, hemiplegic side, detailed physical and neurologic examination findings, assessment of ankle-foot deformity, preoperative orthotic and ambulatory aid needs, and ambulatory scale scores [17] (Table 1). In addition, preoperative gait analysis and dynamic EMG results were reviewed, which were part of the normal preoperative workup for patients undergoing correction for SEV (Table 2). The anterior and posterior tibialis, gastrocnemius, soleus, flexor hallucis longus, flexor digitorum longus, peroneus longus, and peroneus brevis during barefoot walking were tested during EMG. Self-selected velocity and maximal walking velocity also were recorded. Shoe insole foot switches, and ankle goniometer recordings, allowed for correlation of specific muscle activity with gait cycle. All patterns with respect to the type of phasic activity and its duration in the gait cycle were analyzed [18]. Abnormal activity patterns were classified based on Perry’s classification system [13] (Table 2). In view of the dynamic nature of the deformity, no attempts were made to preoperatively grade the severity of these cases.
Table 1.
Functional ambulation scale [17]
| Level | Status of ambulation |
|---|---|
| 0 | Nonambulatory |
| 1 | Nonfunctional ambulation |
| 2 | Household ambulation |
| 3 | Neighborhood ambulation |
| 4 | Independent community ambulation |
| 5 | Normal ambulation |
Table 2.
Dynamic electromyographic gait patterns in current patients
| Muscle | Continuous | Silent | Phasic premature | Phasic, premature prolonged | Normal phasic |
|---|---|---|---|---|---|
| Tibialis anterior | 27 | 1 | 9 | 10 | — |
| Tibialis posterior | 8 | 19 | 10 | 8 | 2 |
| Gastrocnemius | 24 | 8 | 13 | 2 | — |
| Soleus | 11 | 10 | 22 | 4 | — |
| Flexor hallucis longus | 29 | 5 | 6 | 4 | 3 |
| Flexor digitorum longus | 16 | 7 | 19 | 5 | — |
| Peroneus longus | 4 | 3 | 28 | 12 | — |
| Peroneus brevis | 5 | 18 | 20 | 4 | — |
Definitions: 1 = premature: action begins before the normal onset; 2 = prolonged: action continues beyond the normal cessation time; 3 = continuous: electromyography uninterrupted for 90% or more of the gait cycle; 4 = curtailed: early termination of the electromyography; 5 = delayed: onset later than normal; 6 = silent: electromyography of insufficient amplitude or duration; 7 = out of phase: swing or stance time reversed.
The surgical operative notes of these patients also were reviewed. Data collected from the operative notes included method of tendon fixation and additional surgical procedures performed in addition to the SPLATT indicated by the preoperative gait and EMG analyses (ie, gastrocnemius/tendo-Achilles [TA] lengthening, tibialis posterior tendon lengthening, flexor hallucis longus/flexor digitorum longus [FHL/FDL] to calcaneus, extensor hallucis longus [EHL) to middle cuneiform dorsum, plantar fascia release, and long toe-flexor release) (Fig. 3). Based on the initial technique of tendon routing and fixation [4] and subsequent modification in the surgical technique used in later cases, patients were classified into two groups, Construct 1 and Construct 2. In Construct 1, the split tendon is routed through the cuboid bone in a dorsoplantar manner and fixed with a 7-mm bioabsorbable screw. In Construct 2, the split tendon is routed through the cuboid bone in a lateromedial fashion with the tract angulated posteromedially (Fig. 3) rather than direct medial, and fixation is provided with a 7-mm bioabsorbable screw. Patients were divided into Groups I and II based on these fixation techniques used for SPLATT (Fig. 4).
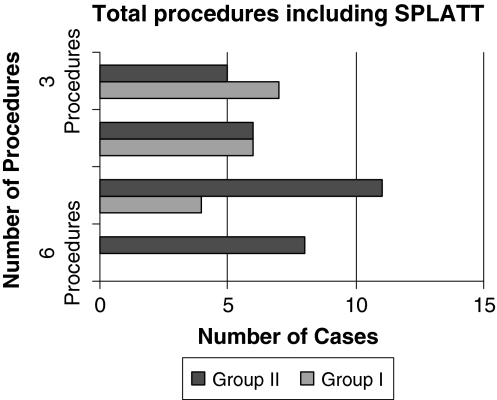
Fig. 3.
The cumulative surgical procedures done in both groups and the number of cases are shown.
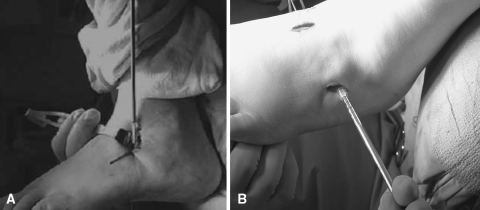
Fig. 4A–B.
Intraoperative photographs show the SPLATT technique with (A) Construct 1 in which the tendon is routed in a dorsoplantar manner and fixed with a biointerference screw, and with (B) Construct 2 in which the tendon is routed in a lateral-to-medial manner and fixed with a biointerference screw.
Seventeen patients underwent SPLATT fixation with Construct 1 (Group I) and 30 with Construct 2 (Group II). In Group I, there were 14 males and three females. Of the 17 patients, 12 had left-sided and five had right-sided hemiplegia. There were 10 Caucasians, five African-Americans, and two Hispanics. The mean age for patients in Group I was 46 years (range, 32–61 years), whereas the mean time since injury was 34 months (range, 18–54 months). Four patients had five procedures, six had four procedures, and seven had three procedures. The mean followup was 51 months (range, 37–84 months) (Fig. 5).
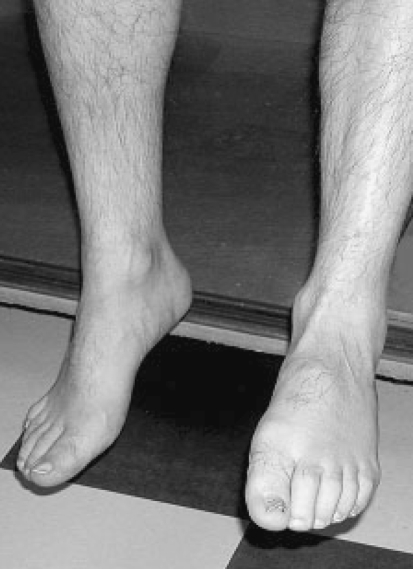
Fig. 5.
The photograph, obtained at the 5-year followup of a patient who had SPLATT using Construct 1, shows active dorsiflexion and correction of equinovarus.
In Group II, there were 30 patients. This construct included 23 males and seven females. Nineteen patients were Caucasians, seven were African-Americans, three were Asian, and one was Hispanic. The mean age of patients treated by Construct 2 was 42 years (range, 29–67 years). No difference in the demographics, side of injury, or length of followup was noted between the groups. In Group II, 22 patients had left-sided and eight had right-sided hemiplegia, which was a similar distribution to Group I. The mean time since injury for Group II patients was 28 months (range, 20–66 months). Eight patients had six procedures, 11 had five procedures, six had four procedures, and five had three procedures. The mean followup was 29 months (range, 24–48 months) (Fig. 6).
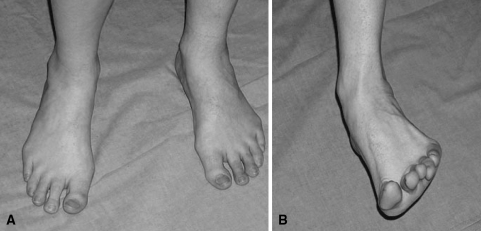
Fig. 6A–B.
The photograph, obtained at the 4-year followup of a patient who had SPLATT using Construct 2, shows an active (A) plantigrade foot with corrected equinovarus and (B) active dorsiflexion and eversion.
Postoperative data collected included postoperative complications (fixation pullout, wound complications), foot position (equinovarus or plantigrade), need for orthotics, need for ambulatory aids, and ambulatory scale.
The unpaired Student’s t-test was used to determine major differences between Group I and Group II in terms of age, mean time since injury, preoperative and postoperative ambulatory scale, mean followup, and number of additional procedures performed. Fisher’s exact test was used to determine major differences between Group I and Group II in terms of race, gender, mechanism of injury, hemiplegic side, preoperative and postoperative ankle-foot position, preoperative and postoperative orthotic and ambulatory aid needs, and postoperative complications. The paired Student’s t-test also was performed within each group to determine major differences between preoperative and postoperative ambulatory scale scores. Fisher’s exact test was performed within each group to determine preoperative and postoperative differences in ankle-foot position and orthotic and ambulatory aid needs. Statistical significance was set at an alpha value of 0.05.
Results
All 47 feet were in a plantigrade position at last followup. The mean ambulation scale was 2.4 preoperatively and 4.4 postoperatively for Group I and 2.5 preoperatively and 4.1 postoperatively for Group II [17].
Ten of 17 patients in Group I had decreased needs for ambulatory aids, whereas seven of 17 continued with the same status. Fifteen of 30 patients in Group II had decreased needs for ambulatory aids, whereas 15 of 30 continued with the same status (Table 3).
Table 3.
Use of ambulatory aids preoperatively and postoperatively
| Group I (17 patients) | Group II (30 patients) | ||||
|---|---|---|---|---|---|
| Support device | Preoperatively | Postoperatively | Support device | Preoperatively | Postoperatively |
| Walker | 9 | 3, walker | Walker | 14 | 6, walker |
| 6, cane | 8, cane | ||||
| Cane | 6 | 2, cane | Cane | 11 | 4, cane |
| 4, no support | 7, no support | ||||
| No support | 2 | 2, no support | No support | 5 | 5, no support |
After cast removal (6 weeks) and at final followup after therapy and rehabilitation, 36 of the 47 patients became brace-free (Table 4). Fixation-related complications were more common in Group I in which three patients experienced screw pullouts (p = 0.0419). One of these three patients had wound breakdown. However, none of the patients in Group II had wound healing problems or screw pullouts.
Table 4.
Use of braces and orthoses preoperatively and postoperatively
| Group I (17 patients) | Group II (30 patients) | |||||
|---|---|---|---|---|---|---|
| Type of brace | Preoperatively | At cast removal | Final followup | Preoperatively | At cast removal | Final followup |
| Polypropylene AFO | 10 | 7, AFO | 3, AFO | 17 | 7, AFO | 4, AFO |
| 2, BiCAAL | 1, BiCAAL | |||||
| 3, free | 7, free | 8, free | 12, free | |||
| BiCAAL dual-channel adjustable metal ankle | 5 | 1, AFO | 1, BiCAAL | 7 | 5, BiCAAL | 2, BiCAAL |
| 2, BiCAAL | 4 free | 2, free | 5, free | |||
| 2, free | ||||||
| Nonbraceable | 2 | 2, AFO | 2, free | 6 | 1, AFO | 6 free |
| 3, BiCAAL | ||||||
| 2, free | ||||||
AFO = ankle-foot orthosis; BiCAAL = bichannel adjustable ankle lock.
Discussion
In this study, we hypothesized that lateromedial routing of the split tibialis anterior tendon through the cuboid with interference screw fixation is biomechanically and clinically superior compared with dorsoplantar placement of the tunnel with less complications. We evaluated the outcomes of the fixation techniques and reviewed the long-term outcomes of using screw fixation for SPLATT in SEV and present this large series of adult patients with spastic hemiplegic TBI treated at a tertiary-level neuroorthopaedic center by one orthopaedic surgeon. We found that SPLATT with combined procedures (mean, 4.4) was successful in all cases to improve ambulation and function. Construct 2 in this series seemed to be biomechanically superior to Construct 1 in that complications with Construct 1 (three of 17) were more common than with Construct 2 (zero of 30) (p = 0.0419). Ambulation and functional improvement were related to the procedure and were independent of the construct type.
The success of surgical correction of the spastic equinovarus ankle-foot deformity in patients with hemiplegic stroke is well known [7, 14, 15]. All 47 patients in this series had plantigrade feet at final followup and deformity correction was maintained in all cases. Even beyond the minimum 2 years followup (combined mean, 3.3 years; range, 2–7 years), these patients continued to maintain plantigrade feet. These patients with TBI generally were active and placed notable stress on the surgical correction often despite or as a consequence of many associated injuries and residual neurologic deficits. Despite this, all feet remained in a plantigrade position at final followup.
Seventy-seven percent of the patients (36 of 47 cases) were brace-free at final followup. Brace wear was continued in selected patients for various reasons, including mild calf weakness or spasticity and proprioceptive deficits. Twenty-five of 47 patients had an objective decrease in their needs for ambulatory aids after the SPLATT procedure. Numerous patients changed their brace wear from the more cumbersome and controlled bichannel adjustable ankle lock (BiCAAL) to the more flexible and cosmetically appealing polypropylene ankle-foot orthosis.
Use of ambulatory aids persisted in numerous patients as well, reflecting the continued need for external support for balance in some of these patients, although the plantigrade position was achieved. The mean ambulation score improved postoperatively in both groups and notably no patient was less functional after surgery. Split anterior tibialis tendon transfer helped improve the functional ambulation status in our cohort of patients with hemiplegic TBI.
All patients with SEV after TBI in this series had multiple procedures as needed on a case-by-case basis. These included gastrocnemius/TA lengthening, FHL/FDL to calcaneus, EHL to midfoot, plantar fascia release, and long toe-flexor release. Keenan et al. reported the results of improved calf muscle strength in patients with spastic equinovarus deformity by transfer of the long toe flexors to the os calcis [8]. The multiple tendon releases and transfers in patients of this series ranged from two to six with a mean of 4.4. Notable improvements in preoperative and postoperative ambulation scales helped us conclude that multiple tendon procedures (as deemed necessary on a case-by-case basis) improve the functional and surgical outcomes of SEV correction in patients with hemiplegic TBI.
Fuller et al. discussed the use of the bioabsorbable interference screw for fixation of SPLATT [4]. All patients in the current study regardless of the tendon routing technique used (Construct 1 or 2), had the tendon-to-bone fixation performed with a bioabsorbable screw. The 17 patients in the first cohort had a SPLATT procedure with the initial technique in which the tendon was routed through a dorsoplantar tunnel in the cuboid (Construct 1). During followup of these patients, a few anecdotal problems of fixation and wound breakdown were observed. Because of the problems, Construct 2 was created. Along with its clinical application, its mechanical superiority and vector force analysis were studied. Followup of the 30 patients in Construct 2 eventually established the clinical superiority of the fixation. None of the patients in this group had any of the complications experienced by patients in Group I. At this time, we advocate Construct 2 (ie, lateral-to-medial routing of the tendon with bioabsorbable screw fixation) as a modality of fixation for SPLATT.
There are limitations in our study. This analysis was performed on a relatively small sample size of 47 patients. The study reflects the perspective of one institution, although it is one of the largest tertiary neuroorthopaedic referral centers. Comparison with additional institutions would have allowed not only a greater number of patients to be analyzed, but also variations in treatment regimens. Many clinicians are resistant to performing surgery of deformities in patients with TBI, and therefore a multicenter prospective, randomized, and controlled study is likely difficult in this situation. Because the technique of fixation has changed with time, the followup of patients in Group II (mean, 29 months) is shorter as compared with patients in Group I (mean, 51 months). However, for patients with equinovarus deformity, once the surgical correction has been performed to reestablish a plantigrade foot, the transposed tendon has healed, and the foot has remained as such for 24 months, it is unlikely that with a nonprogressive neurologic condition, there would be a relapse. We therefore do not consider this a major limitation. Unpublished preliminary findings from a biomechanical analysis performed with four cadaver models that were used to determine pullout strength of a 7 × 25-mm screw in a SPLATT construct revealed that in Construct 1, the mean was 132 N ± 5.4 (range, 128–140 N), whereas in Construct 2, the mean was 166 N ± 13.4 (range, 148–180 N). The pullout strength was notably higher in Construct 2, although there was no statistically significant difference between the two groups (p = 0.2893) as a result of a small sample size (n = 4).
Our study population is typical in that each patient’s nonsurgical course varied in terms of duration and extent of care with many having a notably prolonged surgical course. This is partly the result of the concern and limited experience among nonsurgical physicians (primary care physicians, physiatrists, and neurologists) with surgical treatments for this condition. Numerous referrals in our patient population were initiated by contact with other patients or their families.
Split anterior tibialis tendon transfer and associated tendon procedures (combined as necessary) based on dynamic EMG are safe and effective for management of SEV in patients sustaining head trauma because it corrects the equinovarus deformity, allowing for improved foot wear, function, and ambulation. Construct 2 is superior with considerably lower complication rates. We recommend surgical correction of SEV in patients with hemiplegic TBI who have prospects of maintaining an active lifestyle because we have found it predictably and effectively corrects an equinovarus foot deformity, improves functional outcomes, and can be done in a therapeutic manner with minimal risk to the patient. We also recommend multiple procedures as necessary (ie, tendon releases or transfers as deemed necessary on a case-by-case basis) based on dynamic EMG evaluation and fixation of tendon with Type 2 (lateromedial routing of tendon with interference screw fixation within the cuboid tunnel) construct.
Acknowledgments
We thank Margaret Perry for help with data collection.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Adekoya N, Thurman DJ, White DD, Webb KW. Surveillance for traumatic brain injury deaths-United States, 1989–1998. MMWR Surveill Summ. 2002;51:1–14. [PubMed]
- 2.Banks HH. The management of spastic deformities of the foot and ankle. Clin Orthop Relat Res. 1977;122:70–76. [PubMed]
- 3.Edwards P, Hsu J. SPLATT combined with tendo achilles lengthening for spastic equinovarus in adults: results and predictors of surgical outcome. Foot Ankle. 1993;14:335–338. [DOI] [PubMed]
- 4.Fuller DA, McCarthy JJ, Keenan MA. The use of the absorbable interference screw for a split anterior tibial tendon (SPLATT) transfer procedure. Orthopedics. 2004;27:372–374. [DOI] [PubMed]
- 5.Hoffer MM, Reiswig JA, Garrett AM, Perry J. The split anterior tibial tendon transfer in the treatment of spastic varus hindfoot in childhood. Orthop Clin North Am. 1974;5:31–38. [PubMed]
- 6.Hosalkar HS, Reddy S, Mariani C, Keenan MA. What’s new in orthopaedic rehabilitation. J Bone Joint Surg Am. 2007;89:2316–2324. [DOI] [PubMed]
- 7.Keenan MA, Creighton J, Garland DE, Moore T. Surgical correction of spastic equinovarus deformity in the adult head trauma patient. Foot Ankle. 1984;5:35–41. [DOI] [PubMed]
- 8.Keenan MA, Lee GA, Tuckman AS, Esquenazi A. Improving calf muscle strength in patients with spastic equinovarus deformity by transfer of the long toe flexors to the Os calcis. J Head Trauma Rehabil. 1999;14:163–175. [DOI] [PubMed]
- 9.Keenan MA, Perry J, Jordan C. Factors affecting balance and ambulation following stroke. Clin Orthop Relat Res. 1984;182:165–171. [PubMed]
- 10.Lawrence SJ, Botte MJ. Management of the adult, spastic, equinovarus foot deformity. Foot Ankle Int. 1994;15:340–346. [DOI] [PubMed]
- 11.Lemperg R, Hagberg B, Lundberg A. Achilles tenoplasty for correction of equinus deformity in spastic syndromes of cerebral palsy. Acta Orthop Scand. 1969;40:507–519. [DOI] [PubMed]
- 12.Ono K, Hiroshima K, Tada K, Inoue A. Anterior transfer of the toe flexors for equinovarus deformity of the foot. Int Orthop. 1980;4:225–229. [DOI] [PubMed]
- 13.Perry J. Dynamic electromyography. In: Perry J, ed. Gait Analysis: Normal, Pathologic Function. Thorofare, NJ: Slack Inc; 1992:381–411.
- 14.Pinzur MS, Sherman R, DiMonte-Levine P, Kett N, Trimble J. Adult-onset hemiplegia: changes in gait after muscle-balancing procedures to correct the equinus deformity. J Bone Joint Surg Am. 1986;68:1249–1257. [PubMed]
- 15.Roper BA, Williams A, King JB. The surgical treatment of equinovarus deformity in adults with spasticity. J Bone Joint Surg Br. 1978;60:533–535. [DOI] [PubMed]
- 16.Thurman DJ, Alverson C, Dunn KA, Guerrero J, Sniezek JE. Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil. 1999;14:602–615. [DOI] [PubMed]
- 17.Viosca E, Martinez JL, Almagro PL, Gracia A, Gonzalez C. Proposal and validation of a new functional ambulation classification scale for clinical use. Arch Phys Med Rehabil. 2005;86:1234–1238. [DOI] [PubMed]
- 18.Waters RL, Frazier J, Garland DE, Jordan C, Perry J. Electromyographic gait analysis before and after operative treatment for hemiplegic equinus and equinovarus deformity. J Bone Joint Surg Am. 1982;64:284–288. [PubMed]