Abstract
Orthopaedic surgical training in Nepal began in 1998, and four major centers now produce between 15 and 20 graduates annually. The duration of the training is four years in one center and three years in the remaining centers. Trainees have adequate trauma exposure. The major challenges include: tailoring training to suit local needs, avoiding the dangers of market driven orthopaedic surgery, adequately emphasizing and implementing time honored methods of closed fracture treatment, and ensuring uniformity of exposure to the various musculoskeletal problems. Training in research methods needs to be implemented more effectively. The evaluation process needs to be more uniform and all training programs need to complement one another and avoid unhealthy competition. Training for nonorthopaedists providing musculoskeletal care is virtually nonexistent in Nepal. Medical graduates have scant exposure to trauma and musculoskeletal diseases during their training. General surgeons provide the majority of trauma care and in the rural areas, health assistants, auxiliary health workers and physiotherapy assistants provide much needed basic services, but all lack formal training. Traditional “bone setters” in Nepal often cater to certain faithful clientele with sprains, minor fractures etc. A large vacuum exists in Nepal for trained nonorthopaedists leading to deficiencies in prehospital care, safe transport and basic, primary emergency care. The great challenges are yet to be addressed.
Introduction
Nepal is a small country that lies between China (Tibet Autonomous Region) in the north and India in the south. Although the history of traditional medicine dates back many centuries, the allopathic system was introduced to the country in a concrete way with the establishment of the Prithvi Bir Hospital at Kathmandu in 1947. The first medical school evolved to meet the needs of a developing nation and growing population.
We present the challenges that face the nation in addressing the disease burden and the current status of training both orthopaedists and nonorthopaedists in the treatment of musculoskeletal disease and trauma.
Overview of Nepal
Nepal occupies an area of 147,181 square kilometers; approximately 80% of the land is mountainous, which provides daunting challenges with regard to transportation, communication, and subsistence. The GDP is US $ 350, and the majority of people survive by practicing subsistence agriculture (Table 1). The country is at the threshold of a new political era with elections having been concluded for a new Constituent Assembly on April 10th 2008. The formation of a stable government could herald development of vast water resources to harness hydroelectric power and to further develop the tourism industry to boost the current fragile economy. Nepal is ethnically diverse, and while Indo-Aryan people occupy the southern parts of the country, the northern regions are populated by Tibeto-Burmese people. Although limited urbanization continues to take place, 85% of the population still resides in the countryside. About 55% of the population of 26 million is between 15 and 59 years of age. Large numbers of young Nepalese work as migrant laborers in India, the middle east, South Korea, Japan and Malaysia, contributing to an all important repatriation economy for the past decades of political uncertainty. Despite initiatives of the past few years, there has been relatively modest growth in the numbers of health care workers in recent decades (Table 2).
Table 1.
Health services in Nepal [6]
| Health service type | 2003/04 | 2004/05 | 2005/06 |
|---|---|---|---|
| Hospitals | 83 | 87 | 89 |
| Hospital beds | 5250 | 6796 | 6796 |
| Health posts | 700 | 699 | 699 |
| Health centers | 10 | 6 | 6 |
| Sub health posts | 3141 | 3131 | 3131 |
| Primary health centers | 180 | 180 | 180 |
| Doctors* | 1259 | 1259 | 1259 |
| Health assistant (HA & AHW) | 791 | 7491 | 7491 |
| Nurses and ANM | 10099 | 11637 | 11637 |
| Kaviraj† | 387 | 387 | 387 |
| Vaidya† | 354 | 354 | 354 |
| Ayurvedic services centers§ | 287 | 287 | 293 |
| Health workers (MCHW) | 3190 | 3190 | 3190 |
| Village-level health workers | 3985 | 3985 | 3985 |
| Other health workers (trained students, women health volunteers) | 62546 | 62546 | 62546 |
* Generally implies graduates of allopathic medical school; ANM = auxiliary nurse midwife, under class 10 personnel trained in basic nursing care; †almost synonymously used terms for traditional medical practitioner; §traditional, indigenous centers promoting natural healthcare measures including herbal medications and other natural cures.
Table 2.
Principle indicators [6]
| Indicator* | Data |
|---|---|
| Projected population for 2006 | 25,886,736 |
| Life expectancy at birth, 2006 | 63.3 years |
| Literate population %, 2001 | 54.1 |
| Per capita GDP at current prices (NRS), 2005/06 | 22,540 |
| Per capita GNP at current prices (NRS), 2005/06 | 23,032 |
| Percent change in GDP for 2004/05–2005/06 | 2.3 |
| GDP deflator for 2004/05–2005/06 | 7.13 |
| Population growth rate (1991–2001, % per annum) | 2.25 |
| Average household size, 2001 | 5.44 |
| % Urban population (based on total 23.1 million population), 2001 | 13.9 |
| % of population below poverty line, 2003/04, Nepal | 31 |
| % of population below poverty line, 2003/04, Urban | 10 |
| % of population below poverty line, 2003/04, Rural | 35 |
* Dates reflect the year in which the statistics were obtained.
History of Medical Training
The current status of musculoskeletal training for orthopaedists and nonorthopaedists would be incomplete without a brief review of the historical background of health care in Nepal. A civil medical school was started in 1934 for training compounders (apothecaries) and dressers who continued to be the sole health care providers for large segments of the urban population for many decades to come. An adequate health care system was virtually nonexistent for the nation at large prior to 1950, with whatever functioning meager services available only to a limited population in Kathmandu. In 1956 under the Ministry of Health umbrella, nursing training commenced and after the implementation of the New Education Plan in the 1970s, the Institute of Medicine (IOM) under Tribhuvan University (TU) initiated certificate level programs in nursing, general medicine, health laboratory, pharmacy, physiotherapy and health education and sanitation. The IOM started its MBBS Program in 1978. Diploma programs in a number of specialties commenced (DA 1984, DGO, DLO 1986, DCH 1987 and DMRD 1987) but were gradually dropped because of preference for degree courses by MBBS graduates. An MD program in general practice commenced in 1982, followed by ophthalmology (1987), medicine, surgery, and anesthesiology (1996), and orthopaedics (1998), all at IOM. In 1993, under the collective leadership of the Ministry of Health (MOH), World Health Organization (WHO), advisor government of India (represented by the Director, All India Institute of Medical Sciences) and senior Nepali Physicians, the Postgraduate Medical Education Committee was formulated to oversee the development of postgraduate training options inside Nepal. Five hospitals inside the Kathmandu Valley were designated training centers, and as of 2003, 208 students had been admitted into the various courses.
The BP Koirala Institute of Health Sciences (BPKIHS) in northeastern Nepal was established in 1993. This medical university, nurtured and supported by the central government of India, is playing a leading role in the education and training of a wide range of health professionals. It has expanded its postgraduate training in over 17 subjects, including orthopaedic surgery, which commenced in 1999.
Kathmandu University, being nongovernmental, took the bold step of starting a postgraduate training in orthopaedic surgery in 1999, in a unique collaborative effort with partner hospitals capable of providing the educational and training experience. Subsequently, this private university has initiated other postgraduate training initiatives in collaboration with the Manipal Academy of Health Education (India based) and other Kathmandu University affiliated medical schools.
The National Academy of Medical Sciences (NAMS) opened in 2003 and started postgraduate training courses in several disciplines, including orthopaedic surgery.
Musculoskeletal Training of Orthopaedists
As formal training of orthopaedic surgeons has been available for less than ten years, many lessons are still being learned. Although four universities run postgraduate training courses (Table 3), there are more similarities than differences, and each program has its strengths as well as weaknesses.
Table 3.
Institutions providing postgraduate orthopaedic surgery training
| Serial no. | Name | Commenced |
|---|---|---|
| I | Institute of Medicine (IOM) of Tribhuvan University | 1998 |
| II | Kathmandu University | 1999 |
| III | BP Koirala Institute of Health Sciences (BPKIHS) | 1999 |
| IV | National Academy of Health Sciences (NAMS) | 2003 |
The objectives of the curriculum as laid down by all four training centers are similar. The overall objective is “to train and educate so as to produce an orthopaedic surgeon who possesses the required standards necessary to function as a specialist.” These objectives are realized by: (1) Peer example: a 1:1 student/preceptor ratio per year is the set standard so the student has the advantage of close guidance through the course of his training; (2) intensive practical work, under supervision in the out patient service, inpatient wards, emergency room, and operating rooms; (3) interactive seminars, case presentations, specific discussions on previously assigned subjects, journal clubs and teaching ward rounds by the attending staff; (4) introduction to a wide range of reading material and provision of these services to the students, including the availability of the Internet; (5) presentation of a dissertation on a specific subject under the supervision of the assigned preceptor and designed to stimulate research analysis and writing skills of the student.
All four training institutes have similar and comprehensive curricula. The subjects that are covered throughout the course of the training period include anatomy (musculoskeletal and neural tissues), both macroscopic and where applicable microscopic, physiology (expected to correlate pathology with anatomy and normal physiological functions of the body), orthopaedic pathology, radiology and other forms of imaging as applied to musculoskeletal tissues, orthopaedic oncology, and practical anesthesiology (including the ATLS principles, local regional anesthesia, airway management and mechanical ventilation and insertion of CVP line). The course contents in the curriculum comprehensively cover the various aspects of diagnosis and treatment in trauma, adult disease, pediatric musculoskeletal problems and outline various orthopaedic surgery objectives that the trainee has to have mastered or at least been introduced to through the course of his training period. The subjects that are more strongly emphasized are: (1) fracture treatment principles and polytrauma care; (2) the correct management of wounds in musculoskeletal trauma; (3) diagnosis and management of orthopaedic infections.
The prerequisites for admission into the training process include: (1) MBBS graduates or equivalent and completion of the compulsory year of rotating internship; (2) one year of housemanship after the internship; (3) full registration with the Nepal Medical Council; (4) successful completion of the postgraduate entrance examination conducted by the institution. Exceptions are made by institutions for foreign nationals sponsored by their respective governments and candidates with diploma in orthopaedics seconded for additional training by government bodies.
No one can question the validity of a complete training process where a graduating candidate has soundly mastered the principles of musculoskeletal disorders and their management and is capable of devising treatment methods wisely. Ideally every trainee should be introduced to research, which is important for developing critical evaluative skills, reviewing literature, analyzing data, and communicating scientific work to colleagues.
How long should an optimal training course for orthopaedic surgery last? Defining mandatory basic skills is not an easy task because a surgeon is more than a technician. A skilled trainee possesses many competencies, including a large knowledge base, ethical values and surgical proficiency.
Three years is the usual duration of training time in most institutions in Nepal (Table 4). The IOM runs a 4 year course. One of the problems faced by the training institutions is providing a stipend through the course of training to the student. The training could be continued after graduation (as is the case now in KU program) to further enhance skills and responsibility components of the trainee, but the capability of the institution to financially support the graduate through an additional year of training is the challenge.
Table 4.
Duration of training
| Serial no. | Institute | Duration | Remarks |
|---|---|---|---|
| I | IOM (TU) | 4 years | |
| II | KU | 3 years | |
| III | BPKIHS | 3 years | |
| IV | NAMS | 3 years | For diploma holder duration is 2 years |
The Training Process
All trainees have practical experience in the emergency room, outpatient clinics, inpatient facilities, and operating rooms. For the IOM and BPKIHS, the training takes place entirely at their respective hospitals. NAMS rotates its orthopaedic residents through three hospitals (Bir Hospital, Patan Hospital and Birendra Army Hospital). Kathmandu University program is currently conducted at the B & B Hospital and The Hospital and Rehabilitation Center for Disabled Children. The residents are on call two or three times a week and the average weekly engagement comes to be 80–90 hours.
The Preceptor/Dissertation/Log Book
Each student is assigned a preceptor and the emphasis is on self-directed learning, with the teachers functioning as guides. At the end of the first six months of training, the student submits to the Postgraduate Medical Education Committee a plan for the chosen dissertation with all relevant references. The committee reviews the proposal and makes its recommendations to permit the study to proceed. Periodic review with the preceptor continues and the candidate is expected to have a dissertation completed six months prior to the final examination, this being one of the prerequisites of the training process. The thesis/dissertation is then sent for evaluation by an external examiner who marks it as satisfactory or unsatisfactory. Having a satisfactory mark is a prerequisite for passing the final examination. At the final examination, students are questioned to explain and defend various aspects of their research. A log book of all practical work assisted and independently performed is maintained and periodically reviewed by the preceptor.
Evaluation Process
The summary evaluations vary somewhat between institutions, but the goals are similar: to ensure a candidate on completion of the stipulated duration of training is ready to sit for the final university examination. These evaluations are based on performance in: (1) case presentations; (2) presentations made on specified subjects at the weekly conferences; (3) Applied Basic Sciences examination; (4) other evaluations (e.g., KU holds an annual in-training examination in which all trainees sit for the same examination and feedback is provided to the students based on the expected performance for their level of training).
Two internal and two external examiners are involved in the final evaluations. Each institution decides on the appointment of the Chief Examiner, whose job is to coordinate all the activities for the institution with its controller of examinations or similar authority.
Theory papers cover applied basic sciences, general orthopaedics and trauma, and specialty and recent advances in orthopaedic surgery. These subjects are covered in two or three theory papers depending upon the institution.
A practical examination includes: (1) One long case; the examinee presents the case to the panel of examiners and proceeds step by step to demonstrate clinical findings and discuss the steps in investigation, diagnosis and management. This is considered a crucial step in the entire evaluation process and a student can fail the entire examination if this step is unsuccessful; (2) Short cases; two or more cases are posted for demonstration of findings and specific questions asked about diagnosis and management; (3) Round table discussion; two examiners (one internal and one external) pose questions to the examinee covering a wide range of subjects (anatomy using the skeleton, pathology using specimens, radiological diagnosis using radiographs and other images, surgical instruments, implants and orthoses/prostheses). The candidate spends about half an hour with each set of examiners.
An objective structured clinical examination provides additional evaluation. Some institutions (e.g., KU) also post this objective structured clinical examination, where the candidate moves from one question item to another to answer the specific query (radiographic or other images, slide, surgical instrument, specimen, etc.).
The four examiners then compile all the marks and make the final recommendations to the university which reviews all the available information supplied and declares the final results. The degree awarded by all the institutions in Nepal is MS (Master of Surgery) in Orthopaedic Surgery.
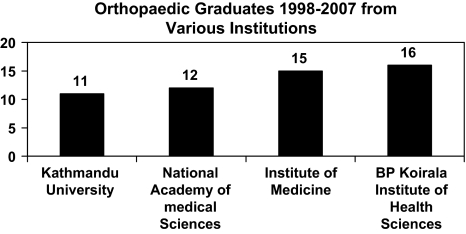
All the training institutions generally prefer to retain a fresh MS graduate as a registrar (the equivalent of a chief resident) for a year or so, so that more practical skills can be acquired. But the lack of resources makes this difficult and the practice cannot be implemented as a routine. Since the inception of musculoskeletal training for orthopaedists in 1998, 54 have successfully graduated with an MS from the four training centers (Fig. 1).
Fig. 1.
Orthopaedic graduates from 1998 to 2007 from various institutions are shown.
Costs of Training
Several categories of students may join a postgraduate training program: (1) A sponsored student whose sponsoring agency assumes all financial responsibility and provides the student a scholarship for living expenses; (2) a paying student who pays an amount (variable from institution to institution, but anywhere between 10 lakhs to 20 lakhs or more (roughly US $15–30,000) to cover the cost of admission, examination and a monthly stipend over the 3 years of training; (3) A full scholarship merit student whose out-of-pocket costs would be limited to living expenses.
Additional Training/Fellowships
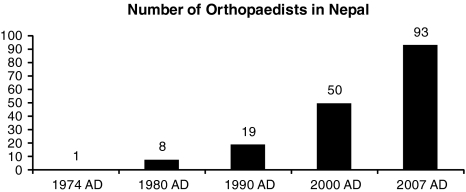
The development of the Masters level training in orthopaedic surgery has resulted in a gradually increasing demand for additional specialized training in certain subspecialties. Fellowship courses providing practical training are not readily available at this time in Nepal, although the development of in-country fellowships will need to be explored as more experience and expertise becomes available. Numerous workshops have been conducted on specific subjects in several of the teaching institutions on a regular basis. The workshops were conducted by national and international experts, and topics included basic skills such as the closed treatment of fractures (adults and children) and principles of rehabilitation in children (combined workshop with faculty from BPKIHS and HRDC), and more specialized skills including spinal cord injury rehabilitation, the principles of Ilizarov fixator application, the surgical treatment of acetabular fractures, and arthroplasty workshops with live demonstrations. The Nepal Orthopaedic Association played an important role in these activities and the numbers of orthopaedists has grown in recent years (Fig. 2).
Fig. 2.
The graph charts the number of orthopaedists in Nepal from 1974 to 2007.
Musculoskeletal Training of Nonorthopaedists
This category of care providers includes medical graduates, general surgeons, health assistants, physiotherapy assistants, ambulance drivers and helpers and the traditional bone setters including barbers (Table 1). All these groups of personnel provide care in the prehospital and transport setting or in the hospital itself. However, there is no structured training to specifically meet the needs for musculoskeletal care.
The Health Assistant (HA) plays an important role in the community in providing basic health care, including musculoskeletal care. These high school graduates are trained for 2½ to 3 years, and practice at health posts of primary health facilities within the districts. They are called upon to provide an array of basic services, including attending to those with accidents and other musculoskeletal ailments. Musculoskeletal services include basic splinting and casting, and appropriate referral of cases to higher levels of service.
The Community Medical Assistant (CMA) undergoes a 15 month long training consisting of a similar curricula to that of the Health Assistant and is placed in charge of the subhealth post. They assist doctors, and may provide basic fracture care (and even set up traction) in more remote locations. They may also work as technicians in the operating theatre.
The Hospital and Rehabilitation Center for Disabled Children (HRDC) which is a part of the Kathmandu University Teaching Hospital network, provides nonhospital based services throughout Nepal utilizing a Community Based Rehabilitation (CBR) worker program, which was established in 1988. To meet the staffing needs of its own outreach programs, the Hospital and Rehabilitation Center for Disabled Children conducted regular courses of 3 months duration in the basics of musculoskeletal disease, preventive health care and physical rehabilitation. The candidates who are high school graduates are either sponsored or have to pay personally the normal charges for the course. HRDC has employed twenty three of the graduates so far, while the remainders are working for other organizations throughout the country. The course has no official recognition, but the hospital continues to seek avenues for some form of accreditation and credit for these graduates.
HRDC has also conducted Physiotherapy and Rehabilitation Training (PRT) for 189 personnel since 1996, including 11 PRT trainees currently employed at our hospital. The 3 month curriculum includes the basic principles of applied anatomy, physiology, musculoskeletal diseases and rehabilitation. Trainees are often referred by community based organizations. These workers are able to provide basic musculoskeletal and rehabilitation care, promote preventive care, and assist in appropriate and timely referrals.
A recent workshop on International Community Based Health Emergency Preparedness Training (Inter CEPT) was held at BPKIHS in Dharan, and was attended by orthopaedic surgeons representing all the postgraduate training centers. A consensus document was drafted outlining a training program to enlighten all citizens on the role they can play in the event of a medical crisis in either the home or the community. This training emphasizes prevention of complications along with simple and safe measures to prevent a catastrophe. Prehospital care providers would be able to function far more efficiently with such basic training, which should be incorporated into the training curriculum for nonorthopaedists providing musculoskeletal care.
The type of care provided by nonorthopaedists include bone setting for simple fractures, application of casts and splints, wound dressings and drainage of abscesses, suturing wounds, providing after care, basic physiotherapy, etc. Unfortunately most of these activities are not supervised because of unavailability of resources (manpower and materials), and serious complications are not uncommon.
Discussion
Nepal has had to rapidly switch gears to catch up with the increasing demands for musculoskeletal care from a rapidly growing population, and there are many challenges to be faced. The burden of musculoskeletal trauma is increasing and can no longer be ignored. Preventive efforts must be an urgent priority in a nation strapped for resources. In the urban setting, attention must be directed towards education for safe driving and the development of better road infrastructure and public transport systems. Prehospital care and rapid safe transport to treatment facilities is virtually nonexistent, and will be difficult to develop given that a sizeable percentage of the population reside in mountainous regions that lack roads. The timely transport of the injured has no easy solution at first glance. Other challenges include how to address a lack of uniformity in accessing orthopaedic services, due to both health worker shortages (and maldistribution) and disparities in infrastructure and physical resources. The needs of the nation far outweigh the available resources. Financial concerns are also worthy of mention, as funding must become available to support the delivery of musculoskeletal trauma services. The lack of health insurance makes technologically intensive treatments (even some basic services) out of reach of most Nepalese at present. Manpower and material needs may be further developed by private and public partnerships, but incentives and opportunities will have to be developed for this to happen. Given the status of the country’s economy at present, this is indeed a daunting task.
The subject of this paper is providing human resources for musculoskeletal care, and our focus is on the newly developed training programs in orthopaedic surgery. The four training programs produce about 17 graduates annually. To date, most of these graduates have chosen to practice in an urban environment, and a persistent lack of trained caregivers in the more rural environments will need to be addressed. The ratio of orthopaedic surgeons to patients in sub-Saharan Africa is approximately 1 to 5 million people [5]. If this ratio were applied to the USA, there would be less than 60 orthopaedic surgeons for the entire country. The USA has about 20,000 orthopaedic surgeons (1 to 15,000 people). Nepal, with a population of about of about 26 million, has 90 orthopaedic surgeons (1 to 289,000 people). We will need to train more orthopaedic surgeons and ensure their services are distributed evenly throughout the country. The training of paraprofessionals in musculoskeletal diseases has yet to play a major role in the delivery of musculoskeletal trauma services, but should be explored as another way to enhance the health workforce. The ready availability of nonorthopaedists well-versed in basic primary care would play a very important role to bridge the gap between primary and the prehospital and definitive care by the orthopaedists.
Until formal training became available in our country, postgraduate medical education, including orthopaedic training, was obtained largely in the Indian subcontinent (India, Pakistan, Bangladesh) and elsewhere (former USSR, China, Japan, UK, USA etc) [4]. With graduates from these diverse environments, standards of practice lack uniformity. There has also been some lack of uniformity in training between the four postgraduate programs in Nepal. A feature of orthopaedics in the past century has been the rise and fall of many diseases, for example tuberculosis, polio, and rickets, which all remain prevalent in our region [3, 8]. While an imported model of training is not completely desirable, elements of an ideal training program should focus on the management of locally relevant problems using technology available in Nepal. Trainees should also be introduced to the breadth of orthopaedic treatment options available in economically developed countries, although many of these technologies will remain unavailable in the foreseeable future.
Goals and standards must also be established by our specialty societies. The Government, through the Ministry of Health and Education, has within its prerogative to influence the activities of all training institutions either directly or indirectly, and occasionally such influences may adversely affect these institutions. The World Health Organization works closely with the Ministry of Health and continues to play important roles in advisory capacities and funding of certain activities. Although no specific steps have been taken, the advantage of uniform requirements for training and the evaluation process has been recognized by the training programs. In the developed countries of the West, specialty societies have promoted greater subspecialization amongst trainees, and have defined criteria for both accreditation and reaccreditation. Other issues such as how to provide continuing education after graduation must be addressed [1, 2, 7].
Orthopaedic surgery is in an era of rapid technological advancements, and many simpler methods of orthopaedic treatments which are far less expensive are underutilized and frowned upon as inferior. We have to arm our future orthopaedic surgeons during their training period with more wisdom and counsel to strike a fair balance in the various treatment options available. Alternative and equally effective but less expensive treatment options for musculoskeletal disorders should be promoted by the professionals and government. All the parties involved in training need to consult with one another and collaborate on a regular basis to develop the most appropriate and uniform teaching experience for their students. The Government must play the role of a facilitator, providing advice and support in whatever way feasible to promote the preventive, curative and educational effort directed towards the burden of musculoskeletal disorders in Nepal.
Where Are We Now?
The burden of musculoskeletal disease is increasing by the day and no longer can be ignored. Prehospital care and rapid safe transport to treatment facilities is virtually nonexistent. Nonorthopaedists capable of delivering these services need to be trained in larger numbers all over the country.
Training of orthopaedic surgeons within the country has been a major step in meeting the manpower needs, with about 17 graduating annually. Services from orthopaedic surgeons are available in few pockets of urban communities. The standards of practice are nonuniform due to the varied backgrounds of training experiences of many from the group of orthopaedic surgeon trained abroad. Nonavailability of health insurance schemes makes technologically intensive musculoskeletal care out of reach of most Nepalese for the present.
Where Do We Need To Go?
Manpower and material needs will need to be further developed by both private and public partners in healthcare. Services have to be available more uniformly in the country. Incentives and opportunities will have to be developed for this to happen. The economic challenges to achieve these objectives have to be faced and solutions found. Given the status of the country’s economy at present, this is indeed a daunting task.
How Do We Get There?
Preventive effort in the spiraling musculoskeletal disease burden must take urgent priority in a nation strapped for resources. Attention will need to be directed towards education for safe driving and the development of better road infrastructure and public transport systems. In a mountainous country where many locations are inaccessible by roads, the timely transport of the injured and sick has no easy solution at first glance.
Alternative and equally effective but less expensive treatment options for musculoskeletal disorders should be promoted by the professionals and government. Technology which comes at an unaffordable price for the majority of our people must be tailored wherever feasible. All the parties involved in training need to consult with one another and collaborate on a regular basis to develop the most appropriate and uniform teaching experience for their students. The government must play the role of a facilitator, providing advice and support in whatever way feasible to promote the preventive, curative and educational effort directed towards the burden of musculoskeletal disorders in Nepal.
Acknowledgments
We thank Dr. Om Prasad Shrestha for his secretarial assistance.
Footnotes
The author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Bhattarai MD. Knowledge, skill and approach in postgraduate education. J Nepal Med Association (JNMA). 1999;38:95–99.
- 2.Bhattarai MD. Time to act: strengthening postgraduate medical education in Nepal. J Nepal Med Association (JNMA). 2001;40:I–I.
- 3.Debas HT, Gosselin R, McCord C, Thind A. Surgery. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P, eds. Disease Control Priorities in Developing Countries. 2nd ed. New York, NY: Oxford University Press and the World Bank; 2006:1245–1259. [PubMed]
- 4.Dixit H. Nepal’s Quest for HEALTH (Health Services of Nepal). 3rd ed. Kathmandu, Nepal: Educational Books Publishing Ltd; 2005:110–113.
- 5.Gosselin RA. War injuries, trauma, and disaster relief. Orthopaedic surgery in the developing world. Techniques in Orthopaedics. 2005;20:97–108. [DOI]
- 6.Government of Nepal National Planning Commission Secretariat. Central Bureau of Statistics Web site. Available at: http://www.cbs.gov.np/index.php. Accessed May 2008.
- 7.Karki DB, Dixit H. An overview of undergraduate and postgraduate medical education in Nepal and elsewhere. Kathmandu Univ Med J (KUMJ). 2004;2:69–74. [PubMed]
- 8.Rang M. The Story of Orthopaedics. Philadelphia, PA: WB Saunders Company; 2000:2–9.