Abstract
Traditional bonesetters (TBS) have been in Nigeria for centuries. Up to 85% of patients with fractures present first to the traditional bonesetters before coming to the hospital and therefore this mode of care delivery cannot be overlooked in Nigeria. We attempted to document the current practice of TBS in Ibadan and their methods of fracture treatment with a view to training and improving the services offered by them. We carried out a literature search to review all previous studies on traditional bonesetters’ practice and visited a few of them to document their current practice. The only change in the management of fractures by the TBS over the past 28 years was the use of spiritual methods of healing to treat open comminuted fractures; a technique for which no scientific basis was readily discernible. There is a need to educate and train the TBS in effective management of both open and closed fractures. Such training should be provided by orthodox orthopedic surgeons with a view to minimizing mismanagement of fractures. To this end, we propose a training algorithm.
Introduction
Traditional healers were practicing long before orthodox medicine was introduced to the developing world [8]. The first orthodox hospital was built in Nigeria (Lagos) in 1873 [18]. Before this, traditional medicine was the only available form of healthcare. Presently both orthodox and traditional medicines coexist side by side and both are patronized by patients [12].
Nigeria is in West Africa, bordering the Atlantic Ocean. It has a total area of 923,770 km2, stretching from the Gulf of Guinea on the Atlantic coast in the south to the fringes of the Sahara desert in the north. It is bounded by Benin on the west, Cameroon on the east, Chad on the northeast and Niger on the north. It has a population of 140 million with less than 200 orthopaedic surgeons (one per 700,000 people). Nigeria’s gross national income per capita is $1040 and the total expenditure on health per capita is $53 (government contribution to this is $16) while the total expenditure on health as a percentage of the GDP is 4.6. Nigeria operates a three-tier system of healthcare, namely the provision of primary, secondary, and tertiary healthcare [6].
Primary healthcare is the responsibility of the local government with support from the state ministries of health. Private medical practitioners also provide healthcare at this level. Secondary healthcare provides specialized services to patients referred from the primary level through outpatient and inpatient services of hospitals for general medical, surgical, pediatric, and community health services. Secondary healthcare is available at the district, divisional, and zonal levels of the states. Adequate supportive services such as laboratory, diagnostic, blood bank, rehabilitation, and physiotherapy are also provided. Tertiary healthcare consists of the provision of highly specialized services by teaching hospitals and other specialist hospitals for specific conditions and diseases such as those in orthopaedics, ophthalmology, psychiatry, maternity, and pediatrics. Care is taken to ensure an even distribution of these hospitals. Also, appropriate support services are incorporated into the development of these tertiary facilities to provide effective referral services.
Primary healthcare is the cornerstone of delivery of healthcare services in Nigeria. However, many problems plague the current primary healthcare system. These problems include insufficient number of medical personnel and their uneven distribution at urban centers to the detriment of rural areas, lack of transportation facilities to help medical personnel access communities, irregular accessibility to parts of the communities owing to natural topographical conditions like flooding, hilly or mountainous terrain, and lack of roads, lack of community involvement and participation, and misuse and abuse of scarce human, material, and financial resources by political and administrative leadership [2]. All these problems contribute to making primary healthcare inaccessible to rural communities, hence their reliance on traditional medical practitioners (and traditional bonesetters [TBS]) who are members of these communities.
Traditional healers may provide up to 90% of primary healthcare for the rural people in Nigeria [17]. Classes of traditional healers include traditional birth attendants (TBA), traditional medicine men (babalawo) and TBS [17]. The traditional bonesetter’s practice is a highly specialized form of traditional medicine [17]. It is usually passed from father to son but some outsiders also receive their training via apprenticeship [12]. There are however many complications attributed to the TBS [3, 5, 10–16].
Although we do not know the denominator (i.e., how many people are successfully treated by the TBS), commonly reported complications include gangrene of the affected limb, nonunion, malunion, contractures, osteomyelitis, and limb shortening [3, 10, 13, 14]. Despite these complications, there is a great demand for TBS services, and in fact some patients elect to leave orthodox hospitals in favor of treatment by a TBS. Possible reasons for this include cultural beliefs, ignorance, third-party advice, the short supply of trained orthodox manpower in rural areas [17], quicker and cheaper services, and the fear of amputation at an orthodox hospital [12]. Payment for TBS services is usually made in cash or in kind. Rehabilitation is virtually nonexistent among TBS services. Since not all the patients treated by TBS report back to the orthodox hospitals (except those with complications), we believe that there must be many patients with minimally displaced fractures who have been successfully treated by them.
The importance of traditional healers in healthcare delivery in Nigeria cannot be overemphasized [1]. A study funded by the World Health Organization’s Division of Strengthening Health Services concluded that incorporating trained traditional health practitioners in primary healthcare programs could be cost effective in providing essential and culturally relevant health services to communities in developing worlds [8]. Several authors have proposed training of TBS to reduce the incidence of gangrenous limbs and amputations [7, 12, 16].
We document the current practice of traditional bonesetters in Ibadan, their methods of fracture treatment, and the outcome of treatment with a view to improving the services offered by them.
Case Presentation
A.A. is a 17-year-old university student who presented 1 week following a football injury in which he sustained an open fracture to his right leg. Following 5 days of treatment by a TBS, he presented to the accidents and emergency department in University College Hospital, Ibadan. Both his parents are graduates; his father is a retired lecturer from the Polytechnic. Clinical evaluation revealed a gangrenous right leg (Fig. 1) for which he had an above-knee amputation.
Fig. 1.
After 5 days of treatment by a traditional bonesetter, a 17-year-old university student presented to the accidents and emergency department at University College Hospital, Ibadan. He had sustained an open fracture to his right leg playing football a week before. Clinical evaluation revealed a gangrenous right leg for which he underwent above-knee amputation.
Traditional Practice
We visited a traditional bonesetter in order to document his clinic sessions, consultations, and treatment of fractures. The first step for the TBS is to identify a fracture, which is accomplished by noting the following symptoms and signs: swelling, pain, loss of function, angulations, abnormal mobility, and crepitation on palpation of the fracture site. The TBS does not use radiographs to aid in the diagnosis or the management of fractures.
Once a fracture is diagnosed, the treatment includes reduction, application of an herbal cream, splinting, and bandaging. The first step taken is direct manipulation (reduction). The basis for this is to reduce the fracture to its anatomical position. This is done by holding the patient down while the TBS performs the necessary manipulation. Analgesics are not usually used during manipulation, but rather after the fracture is reduced. The analgesic consists of a cocktail of herbs mixed with a bottle of Schnapps (Fig. 2). The herbs used in the mixture were not disclosed to us by the TBS. The next step in the TBS treatment is the application of an herbal concoction made from various herbs and blended into a cream. This is applied on the skin over a fracture site by a bird’s feather (Fig. 3). The fracture site is then splinted. Materials used for splinting include raffia palm, plywood, tree bark, and hard cardboard (Fig. 4A–C). The splint is applied over the herbal cream. A bandage is then put around the limb to hold the splint in place. We observed that the bandage was applied with pressure, possibly compromising some blood supply and venous return along the lower part of the limb. The lower part of the limb is swollen when the dressings are changed (Fig. 5). The limb is then stabilized with stones to prevent any form of movement of the affected limb (Fig. 6). The bandages are changed frequently (about every 3–5 days). According to the TBS, the reason for the frequent change of the bandages is to reapply the herbal cream said to aid healing of the bone.
Fig. 2.
An herbal cocktail mixed with Schnapps is used as an analgesic before fracture reduction by traditional bonesetters.
Fig. 3.
Before splinting and at each bandage change, an herbal concoction blended into a cream is applied with a bird’s feather.
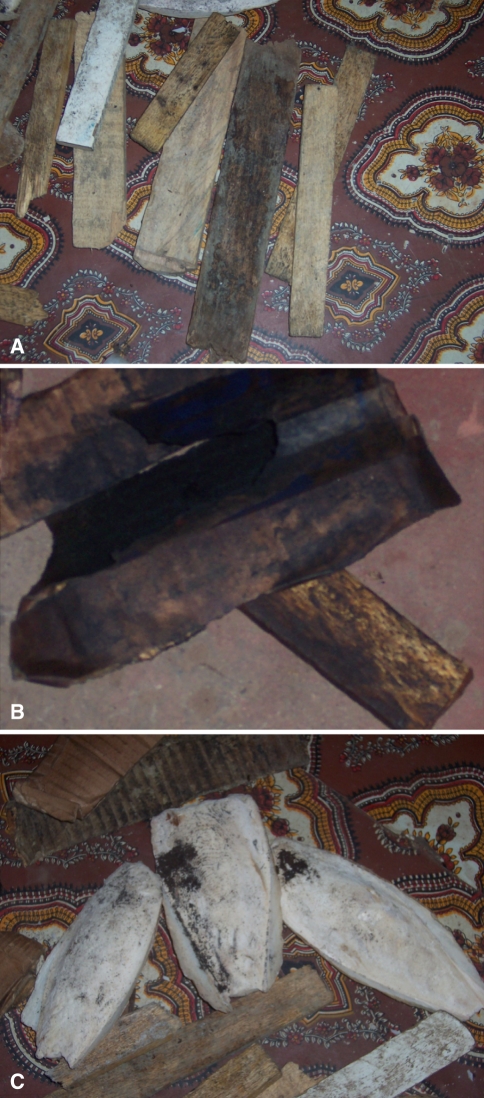
Fig. 4A–C.
Materials commonly used for splinting are (A) plywood, (B) hard cardboard, and (C) tree bark.
Fig. 5.
Swelling on the distal part of the leg from compression bandaging of the fracture site is common.
Fig. 6.
Traditional bonesetters stabilize the limb after splinting and bandaging using stones.
In modern orthopaedic practice in Nigeria, manipulation of a fracture is performed once adequate analgesic/anesthesia has been provided. Once the fracture is reduced, a plaster of Paris cast is applied to keep the reduction stable to aid in healing. The cast remains in place until fracture union; routine removal of casts and recasting is not common in our contemporary orthopaedic practice. An early reference to this technique is made by Barton “The practice of keeping a limb in splints...cannot be too earnestly deprecated...for the preservation of the motion of joints, it is indispensably necessary that these parts should be put into action frequently...” [4].
There are some esoteric aspects to the TBS practice, including incantations, amulets, and charms. This comes into play during the treatment of open fractures. Incantations are invoked to remove comminuted bone fragments from the fracture site. The bone is “commanded” to heal once the fragments are out. Amulets and charms are worn by the patient to ward off evil spirits, witches, and wizards, which are believed to hinder bone healing (Fig. 7).
Fig. 7.
Traditional culture and beliefs assert that a small gourd placed on the wall acts as a charm to ward off witches and wizards.
Bonesetters—Bane or Blessing?
Limb gangrene is but one of many complications of fracture treatment by the TBS [13]. It is quite devastating considering most patients with such trauma are young people in the productive age group. Such patients end up having limb amputations and become disabled at a young age. Eighty-five percent of patients with femoral fractures first present to TBS [9]. In spite of the complications, TBS continue to have patronage from both the highly educated and the illiterate. Possible reasons for this include culture and beliefs (people believe that when they are referred to a tertiary or specialized hospital, they are being sent there to die), ignorance and third-party advice, the short supply of orthodox trained health professionals and also overcrowding of tertiary institutions with trauma cases.
It is therefore important to recognize the TBS and to incorporate them into the health system to provide primary and possibly secondary care to patients with fractures. This requires a collaborative effort from stakeholders such as the government, professional orthopaedic societies, as well as the public. TBS can be trained in the proper management of fractures and referral of complicated fractures to tertiary institutions for management. A short fracture course has proven effective in decreasing the major complications following treatment by TBS [16].
Proposed Training Plan
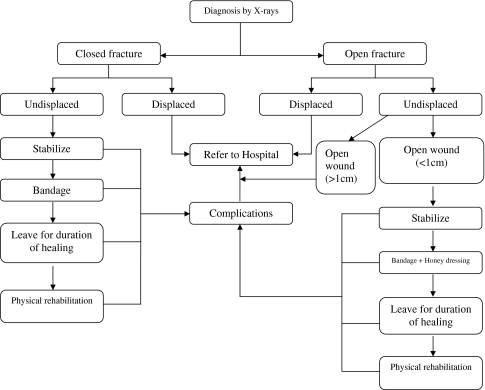
Training can be instituted at the various steps in the practice of the TBS as outlined below (Fig. 8).
Fig. 8.
Following a TBS training algorithm could help bring traditional healers into the National Health System at the primary healthcare level, reducing the burden on secondary and tertiary institutions.
Level of Diagnosis
The use of radiographs can be introduced to the TBS to aid their diagnosis. This would be difficult in the rural setting where radiology facilities are not available, but for TBS in urban settings, radiographs are readily available. The use of the terms open and closed fractures can also be introduced at this level. Understanding whether a fracture is open or closed is essential, and should be stressed in the training of the TBS.
Referrals
Displaced closed fractures should be referred to the hospital for management. The identification of displaced closed fractures again depends on the TBS understanding of radiographs as an aid to diagnosis. Undisplaced closed fractures can be managed by the TBS as before.
Displaced open fractures should be referred to the hospital for management. Undisplaced open fractures can be managed by the TBS provided the wound is less than 1 cm in diameter. Any undisplaced open fracture that has a wound more than 1 cm in diameter should be referred to the hospital for further management. Once again, the emphasis is on radiographic diagnosis and visual interpretation of the wound.
Duration of Healing
The recommended duration of healing of upper-limb and lower-limb fractures must be communicated to the TBS. This is important to prevent malunion and nonunion.
Complications
The various complications that could arise during the course of fracture healing must be made known to the TBS. This is crucial to the prevention of mismanagement. Any complications that arise during the course of fracture treatment must be referred to the hospital.
Physical Rehabilitation
Physical rehabilitation after fracture healing to prevent joint fibrosis and to regain full mobility of the affected limb should be emphasized. Simple rehabilitation exercises can be instituted by the TBS such as gentle walks, passive limb movement, etc.
Discussion
The delivery of fracture care by the TBS may complement that of the orthodox orthopaedic practitioner and improve the overall delivery of services, as the TBS can serve as the first point of contact for many patients with simple fractures, reducing the burden on the orthodox orthopaedic surgeon. However, in order for this to be feasible, successful, and sustainable, the TBS must be incorporated into orthodox medicine. The first step to achieving this is to identify the number of practicing TBS in the community, their geographic distribution, and their level of “expertise.” This would enable training programs to be directed towards re-educating them in the proper management of fractures keeping in mind the training algorithm. Record keeping will also be emphasized in their training. Substantial government participation would be required as well as participation by orthodox orthopaedic surgeons and the public. This training would be voluntary on the part of the TBS with certificate/licensure given by the government to practice as a TBS. Eventually all TBS would be required to take the training in order to be certified to practice by the government.
The role of the orthopaedic surgeon would be to provide the necessary expertise and experience in directly training the TBS without prejudice. Funding for such an endeavor would be from government, NGOs, and public as well as private sectors. TBS training would start from small communities in the various geographic zones of the country and recertification of the TBS would be done biannually. Government-appointed medical personnel would carry out routine inspection of TBS practices to ascertain conformation to set standards of healthcare provision. Above all, the TBS must be sufficiently motivated to the training program. This can be achieved by recognizing TBS as authentic “primary healthcare orthopods” and enjoining the public in rural communities to seek their services first before coming to a secondary or a tertiary institution for treatment.
The Future
It must be emphasized that any TBS training would have to be in the local language, as many of these practitioners are illiterate. Teaching basic hygiene and simple forms of sterilization commensurate with the local technology available is an important starting point to prevent infection. Education on common complications of fracture management must be emphasized and understood. Seminars on prevention of complications should be organized and the TBS invited to participate and provide their own experiences if possible. An interactive session with the TBS at such seminars would go a long way in fostering trust between the TBS and the orthopaedic surgeon. Importantly, the TBS must be incorporated into the National Health System at the primary healthcare level. Equally important is the recognition of TBS by orthodox orthopaedic surgeons as genuine primary healthcare providers for fracture management. Government legislations on limitation of TBS practice using certificates/licensure is crucial to maintaining some form of standard in provision of TBS services at the primary healthcare level in the country. Physiotherapists need to be included in the training program of TBS as they are instrumental in teaching the TBS some basic forms of rehabilitation exercises for patients. Eventually, the TBS would become an integrated part of the primary healthcare system of not just Nigeria but other developing countries as well.
Acknowledgments
We thank Mr. Dayo Owolabi and Mrs. Bose Omololu for being the bridge between the TBS and the orthopaedic surgeon, without which our interaction with the TBS would not have been possible. We also thank all the traditional bonesetters who interacted with us and provided us with the information needed to comprehend their practice and make this first step to establishing a training program for the TBS.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Ademuwagun ZA. The relevance of Yoruba medicine-men in public health practice in Nigeria. Pub Health Rep. 1969;84:1085–1091. [PMC free article] [PubMed]
- 2.Adeyemo DO. Local government and health care delivery in Nigeria: a case study. J Hum Eco. 2005;18:149–160.
- 3.Alonge TO, Dongo AE, Nottidge TE, Omololu AB, Ogunlade SO. Traditional bonesetters in south western Nigeria–friends or foes? West Afr J Med. 2004;23(1):81–84. [DOI] [PubMed]
- 4.Barton JR. Views and treatment of an important injury of the wrist. Med Examiner Philadelphia. 1838;1:365–368. [PMC free article] [PubMed]
- 5.Bickler SW, Sanno-Duanda B. Bone setter’s gangrene. J Pediatr Surg. 2000;35:1431–1433. [DOI] [PubMed]
- 6.Core Health Indicators for Nigeria, WHO Statistical Information System: World Health Organization Web site. Available at: http://www.who.int/whosis/database/core/core_select_process.cfm. Accessed April 2008.
- 7.Eshete M. The prevention of traditional bone setter’s gangrene. J Bone Joint Surg Br. 2005;87:102–103. [PubMed]
- 8.Hoff W. Traditional health practitioners as primary health care workers. Trop Doct. 1997;27 Suppl 1:52–55. [DOI] [PubMed]
- 9.Katchy AU, Nwankwo OE, Chukwu CC, Ukegbu ND, Onabowale BO. Traditional bonesetters’ treatment of femoral fractures. How far? Niger Med J. 1991;21:125.
- 10.Nwankwo OE, Katchy AU. Limb gangrene following treatment of limb injury by traditional bone setter (Tbs): a report of 15 consecutive cases. Niger Postgrad Med J. 2005;12:57–60. [PubMed]
- 11.Oguachuba HN. Mismanagement of elbow joint fractures and dislocations by traditional bone setters in Plateau State, Nigeria. Trop Geog Med. 1986;38:167–171. [PubMed]
- 12.Ogunlusi JD, Okem IC, Oginni LM. Why patients patronize traditional bone setters. Internet Journal of Orthopedic Surgery [serial online]. 2007;4(2). Available at: http://www.ispub.com/ostia/index.php?xmlPrinter=true&xmlFilePath=journals/ijos/vol4n2/bone.xml.
- 13.OlaOlorun DA, Oladiran IO, Adeniran A. Complications of fracture treatment by traditional bonesetters in southwest Nigeria. Fam Pract. 2001;18:635–637. [DOI] [PubMed]
- 14.Omololu B, Ogunlade SO, Alonge TO. The complications seen from the treatment by traditional bonesetters. West Afr J Med. 2002;21:335–337. [DOI] [PubMed]
- 15.Onuminya JE. The role of the traditional bone setter in primary fracture care in Nigeria. S Afr Med J. 2004;94:652–658. [PubMed]
- 16.Onuminya JE. Performance of a trained traditional bone setter in primary fracture care. S Afr Med J. 2006;96:320–322. [PubMed]
- 17.Oyebola DD. Yoruba traditional bonesetters: the practice of orthopaedics in a primitive setting in Nigeria. J Trauma. 1980;20:312–322. [PubMed]
- 18.Schram R. A History of the Nigerian Health Services. Ibadan: Ibadan University Press, 1971.