Abstract
Objectives:
Vitamin K has bone and cartilage effects, and previously shown to be associated with radiographic osteoarthritis. We evaluated vitamin K's effect on hand osteoarthritis in a randomised controlled trial.
Methods:
This was an ancillary study to a randomised controlled trial assessing the effects of phylloquinone supplementation (vitamin K arm) versus placebo on bone loss and vascular calcification among older adults regardless of their vitamin K status. At the final 3-year study visit, we assessed the effects of vitamin K versus placebo on hand x-ray features of osteoarthritis using logistic regression and intention to treat, and also restricted analysis to the subgroup that had insufficient vitamin K concentrations at baseline.
Results:
This ancillary study had 378 participants (193 in vitamin K arm, 185 in placebo arm). There were no effects of randomisation to vitamin K for radiographic osteoarthritis outcomes. Those with insufficient vitamin K at baseline who attained sufficient concentrations at follow-up had trends towards 47% less joint space narrowing (p = 0.02).
Conclusions:
There was no overall effect of vitamin K on radiographic hand osteoarthritis. Subjects that were insufficient in vitamin K at baseline who attained sufficient concentrations at follow-up may have had a benefit in joint space narrowing. A clinical trial in those who are vitamin K insufficient may be warranted.
Trial registration number:
The presence of vitamin K-dependent Gla proteins in bone and cartilage1 2 suggests that vitamin K may play a part in the normal functioning of these tissues. Inadequate intake of phylloquinone, the predominant dietary form of vitamin K, may be widespread.3 As vitamin K antagonism or deficiency in certain Gla proteins affects bone and cartilage4 5 in ways that may have implications for osteoarthritis, we previously evaluated the association of plasma phylloquinone with radiographic hand and knee osteoarthritis in a large cohort study; we found that higher phylloquinone concentrations were associated with a significantly lower prevalence of radiographic osteoarthritis.6
To further evaluate vitamin K's therapeutic effect in osteoarthritis, we performed an ancillary study to an ongoing randomised clinical trial assessing the effects of vitamin K supplementation on bone loss and vascular calcification among older adults who were not necessarily vitamin K deficient at baseline.7 The primary objective was to determine whether 3 years of phylloquinone supplementation, in an amount expected to be both nutritionally optimal and safe, would be associated with a lower prevalence of radiographic hand osteoarthritis.
METHODS
Study participants
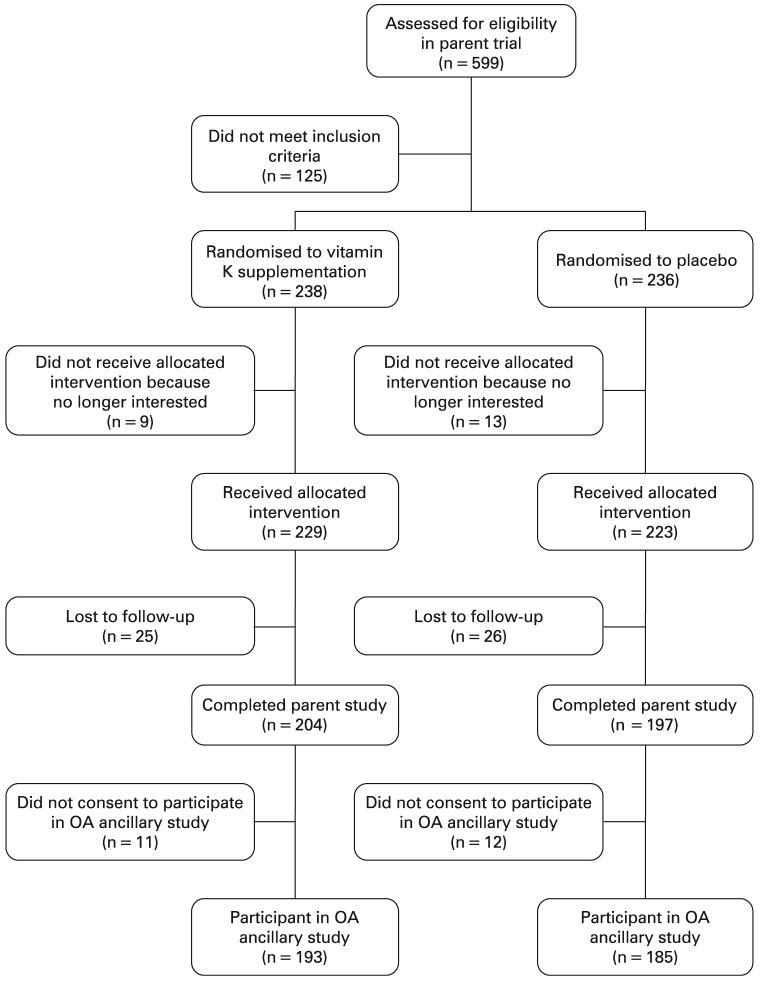
Details of the study participants in the parent study have been published elsewhere.7 In brief, healthy, ambulatory, community dwelling adults age 60–80 years were recruited. A total of 452 participants were enrolled in the parent study, 401 completed the parent study, and 378 consented to participate in our ancillary study (fig 1).
Figure 1.
Flow of study participants. OA, osteoarthritis.
The Institutional Review Boards for Human Research at Boston University Medical Center and Tufts-New England Medical Center approved the protocol.
Study design
The parent study was a 3-year double-blind controlled trial. Participants were randomised stratified by sex to either the treatment group (which received 500 μg of phylloquinone as part of a single daily effervescent multivitamin formulation), or the comparator group (which received an identical multivitamin formulation without phylloquinone) (Hermes Arzeneimittel GMBH, Munich, Germany), hereafter referred to as the placebo group. All study participants also received elemental calcium (600 mg/day) and vitamin D (400 IU/day) as separate tablets. All investigators in this ancillary study were blinded.
For our ancillary study, which was funded after the parent study had already begun, participants were assessed at the final third year study visit with bilateral hand x-rays (see below). Although it is possible that the prevalence of hand osteoarthritis was not evenly distributed in the two groups at baseline, ideally randomisation should lead to an even distribution of participant characteristics at baseline. Thus, our assessment was based upon differences between the two groups at the final study visit, as has been done in other studies.8
Radiographs
Bilateral posteroanterior hand radiographs were obtained at the final study visit using standard techniques. Each hand joint was scored using the OARSI (Osteoarthritis Research Society International) osteoarthritis atlas for Kellgren and Lawrence grade (0–4), largest osteophyte (grade 0–3), and joint space narrowing (grade 0–3). All radiographs were read in a blinded fashion by a board-certified musculoskeletal radiologist after calibration and adjudication sessions. The intra-rater reliability κ values for the radiographic features were 0.72–0.76.
Statistical analyses
We defined hand osteoarthritis on a per-joint basis. Specifically, an individual hand joint was defined as having osteoarthritis if the Kellgren and Lawrence grade was ≥2 in the given joint. We evaluated osteophytes and joint space narrowing separately in a similar per-joint manner, defined as osteophytes ≥grade 2 and joint space narrowing ≥grade 2. We evaluated the effects of randomisation to vitamin K supplementation versus placebo on the presence of these specific radiographic features on a per-joint basis using logistic regression with generalised estimating equations to adjust for correlation among hand joints within an individual.
We also evaluated the effects of achieving sufficient phylloquinone concentrations (≥1 nM) at the final study visit on the same per-joint basis radiographic outcomes among those that had insufficient phylloquinone concentrations (<1 nM) at baseline for two reasons. First, the efficacy of vitamin D is dependent upon achieving an optimal concentration post-intervention.9 Second, we postulated that the effects of phylloquinone supplementation may be most effective for those who were insufficient at baseline based on our earlier study.6
All analyses were adjusted for age, sex, body mass index, smoking status, baseline 25(OH)-vitamin D concentration, education, and adherence to vitamin D/calcium supplements.
RESULTS
Of the 401 participants enrolled in the parent study who attended the final study visit, 378 consented to participate in our ancillary study (193 in the treatment arm, 185 in the placebo arm). The mean age of participants in our ancillary study was 68.2 years, with mean body mass index 28.0 kg/m2 and 59.5% were women. Participant characteristics by treatment groups are shown in table 1.
Table 1.
Participant characteristics of ancillary hand osteoarthritis study
| Vitamin K supplementation arm (n = 193) |
Placebo arm (n = 185) |
|
|---|---|---|
| Mean age, years (SD) | 68.0 (5.5) | 68.3 (5.6) |
| % Female | 57.5 | 61.6 |
| BMI, kg/m2 (SD) | 28.5 (5.4) | 27.6 (4.6) |
| % Ever smoker | 54.9 | 56.8 |
| % Attained any college education |
55.4 | 49.7 |
| Baseline 25(OH) vitamin D, ng/ml (SD) |
23.0 (8.6) | 22.8 (8.9) |
| Baseline plasma phylloquinone, nM (SD) |
1.27 (1.76) | 1.10 (1.37) |
| Final plasma phylloquinone, nM (SD) |
3.13 (2.81) | 1.09 (1.02) |
BMI, body mass index.
In our ancillary study, 222 participants had insufficient phylloquinone concentrations (≤1 nM) at baseline (114 in the treatment arm, 108 in the placebo arm), of whom 125 achieved a concentration of >1 nM by the end of the study. Overall, 52.9% had >2 hand joints, 34.9% had >2 distal interphalangeal joints, and 37.3% had ≥1 first carpometacarpal joint involved with radiographic osteoarthritis, respectively.
There was no effect of randomisation to vitamin K supplementation on prevalence of radiographic hand osteoarthritis (OR 1.03, 95% CI 0.80 to 1.34, p = 0.8), joint space narrowing (OR 1.04, 95% CI 0.68 to 1.57, p = 0.9) or osteophytes (OR 0.95, 95% CI 0.64 to 1.40, p = 0.8).
When evaluating whether participants achieved a phylloquinone concentration >1 nM at follow-up among those with insufficient concentrations (≤1 nM) at baseline, there were trends towards 47% lower prevalence of joint space narrowing (95% CI 0.32 to 0.89, p = 0.02), but not for radiographic osteoarthritis (OR = 0.78, 95% CI 0.56 to 1.07, p = 0.1) or osteophytes (OR = 0.88, 95% CI 0.56 to 1.40, p = 0.5).
DISCUSSION
In this 3-year randomised double-blind placebo-controlled trial, daily supplementation with vitamin K in amounts achievable by dietary intake did not have any effect on radiographic hand osteoarthritis in older adults who were calcium and vitamin D replete. There was a suggestion that those insufficient in phylloquinone at baseline and who achieved sufficient concentrations at follow-up may have had a lower prevalence of joint space narrowing at the end of the trial.
There are several effects of vitamin K on articular cartilage and subchondral bone that could potentially affect the pathological processes occurring in osteoarthritis, including endochondral ossification, chondrocyte hypertrophy and apoptosis, and inflammation.4 5 10-12 Despite a plausible biological rationale and a positive observational study,6 our trial results do not support a significant effect of vitamin K supplementation on osteoarthritis for all persons. Of note, despite previous studies demonstrating an association between poor vitamin K status and bone health,13 the parent trial did not demonstrate a significant effect of vitamin K supplementation on bone mineral density in the hip or spine.7
Why might study results be conflicting? Although we previously demonstrated a cross-sectional association between low phylloquinone concentrations and higher prevalence of radiographic hand osteoarthritis in an observational study independent of vitamin D concentrations,6 all participants of this trial received a daily vitamin D supplement containing 400 IU. Because vitamin D may have effects on osteoarthritis,14 it is possible that modest daily vitamin D supplementation was potentially beneficial for both study arms, and thus any potential small benefit of vitamin K supplementation could not be detected.
Additionally, participants of this trial had self-reported intakes of foods containing phylloquinone above current adequate intakes,15 and were generally a well-functioning and healthy population for this age group. Thus, it is plausible that the additional vitamin K did not confer any additional benefit. In support of this, there was a suggestion that those who were insufficient in vitamin K at baseline, and achieved a sufficient concentration by the end of the study had some benefit with reduced prevalence of joint space narrowing. This group made up 33% of our study population; thus one would not expect to see an effect over the whole study population. Further, longer-term exposure to vitamin K is likely required for an effect on osteoarthritis to occur. This may be why we found an association in our earlier observational study, in which vitamin K status was likely a reflection of long-term adulthood vitamin K intakes.
Another limitation of our study was that we were not able to evaluate change in radiographic osteoarthritis as we were only able to obtain final study visit x-rays. Although it is possible that the baseline distribution of hand osteoarthritis may have differed between the two groups, it is unlikely given the principles of randomisation. Thus end-of-study between-group differences can be validly compared, as has been done previously.8 Another possible reason for a null finding is that the trial was not of long enough duration for differences in osteoarthritis prevalence to be detected. Nevertheless, this was a well-conducted trial, with a relatively large sample size, high adherence, an approximately 90% follow-up in the parent study, and high participation rate in our ancillary study.
In conclusion, vitamin K supplementation in amounts that are achievable in the diet, when taken with recommended amounts of calcium and vitamin D, does not confer any additional benefit on radiographic hand osteoarthritis or joint-related symptoms in healthy, community dwelling, older adults who were not necessarily insufficient in vitamin K. Treatment of vitamin K deficiency, which is common in older people, may have an as yet unproven favourable effect on osteoarthritis. A clinical trial in those who are vitamin K insufficient may be warranted.
Acknowledgments
Funding: Arthritis Foundation Innovative Research Grant, and based upon work supported by the US Department of Agriculture, Agricultural Research Service under Cooperative Agreement No. 58-1950-7-707, and NIH (AG14759, HL696272 and AR47785). Any opinions, findings, conclusions, or recommendations expressed in this publication are those of the authors and do not necessarily reflect the view of the US Department of Agriculture. TN was supported by the Arthritis Foundation Postdoctoral Fellowship Award and the Abbott Scholar Award in Rheumatology Research during the course of this work
Footnotes
Competing interests: None.
REFERENCES
- 1.Hale JE, Fraser JD, Price PA. The identification of matrix Gla protein in cartilage. J Biol Chem. 1988;263:5820–4. [PubMed] [Google Scholar]
- 2.Price PA. Gla-containing proteins of bone. Connect Tissue Res. 1989;21:51–7. doi: 10.3109/03008208909049995. discussion 57–60. [DOI] [PubMed] [Google Scholar]
- 3.Booth SL, Suttie JW. Dietary intake and adequacy of vitamin K. J Nutr. 1998;128:785–8. doi: 10.1093/jn/128.5.785. [DOI] [PubMed] [Google Scholar]
- 4.Luo G, Ducy P, McKee MD, Pinero GJ, Loyer E, Behringer RR, et al. Spontaneous calcification of arteries and cartilage in mice lacking matrix GLA protein. Nature. 1997;386:78–81. doi: 10.1038/386078a0. [DOI] [PubMed] [Google Scholar]
- 5.Price PA, Williamson MK, Haba T, Dell RB, Jee WS. Excessive mineralization with growth plate closure in rats on chronic warfarin treatment. Proc Natl Acad Sci USA. 1982;79:7734–8. doi: 10.1073/pnas.79.24.7734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neogi T, Booth SL, Zhang YQ, Jacques PF, Terkeltaub R, Aliabadi P, et al. Low vitamin K status is associated with osteoarthritis in the hand and knee. Arthritis Rheum. 2006;54:1255–61. doi: 10.1002/art.21735. [DOI] [PubMed] [Google Scholar]
- 7.Booth SL, Dallal G, Shea MK, Gundberg C, Peterson JW, Dawson-Huges B. Effect of Vitamin K supplementation on bone loss in elderly men and women. J Clin Endocrinol Metab. 2008;93:1217–23. doi: 10.1210/jc.2007-2490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nevitt MC, Felson DT, Williams EN, Grady D. The effect of estrogen plus progestin on knee symptoms and related disability in postmenopausal women: the Heart and Estrogen/Progestin Replacement Study, a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2001;44:811–18. doi: 10.1002/1529-0131(200104)44:4<811::AID-ANR137>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 9.Bischoff-Ferrari HA, Dawson-Hughes B. Where do we stand on vitamin D? Bone. 2007;41:S13–19. doi: 10.1016/j.bone.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 10.Loeser RF, Varnum BC, Carlson CS, Goldring MB, Liu ET, Sadiev S, et al. Human chondrocyte expression of growth-arrest-specific gene 6 and the tyrosine kinase receptor axl: potential role in autocrine signaling in cartilage. Arthritis Rheum. 1997;40:1455–65. doi: 10.1002/art.1780400814. [DOI] [PubMed] [Google Scholar]
- 11.Shea MK, Booth SL, Massaro JM, Jacques PF, D'Agostino RB, Sr, Dawson-Hughes B, et al. Vitamin K and vitamin D status: associations with inflammatory markers in the Framingham Offspring Study. Am J Epidemiol. 2008;167:313–20. doi: 10.1093/aje/kwm306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yagami K, Suh JY, Enomoto-Iwamoto M, Koyama E, Abrams WR, Shapiro IM, et al. Matrix GLA protein is a developmental regulator of chondrocyte mineralization and, when constitutively expressed, blocks endochondral and intramembranous ossification in the limb. J Cell Biol. 1999;147:1097–108. doi: 10.1083/jcb.147.5.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cockayne S, Adamson J, Lanham-New S, Shearer MJ, Gilbody S, Torgerson DJ. Vitamin K and the prevention of fractures: systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2006;166:1256–61. doi: 10.1001/archinte.166.12.1256. [DOI] [PubMed] [Google Scholar]
- 14.McAlindon TE, Felson DT, Zhang Y, Hannan MT, Aliabadi P, Weissman B, et al. Relation of dietary intake and serum levels of vitamin D to progression of osteoarthritis of the knee among participants in the Framingham Study. Ann Intern Med. 1996;125:353–9. doi: 10.7326/0003-4819-125-5-199609010-00001. [DOI] [PubMed] [Google Scholar]
- 15.IOM . Dietary reference intakes for vitamin A, vitamin K, arsenic boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. National Academy Press; Washington, DC: 2001. [PubMed] [Google Scholar]