Abstract
Background and purpose:
Hydrogen sulphide (H2S) has been involved in cardiovascular homoeostasis but data about its role in animal models of diabetic pathology are still lacking. Here, we have analysed H2S signalling in a genetic model of diabetes, the non-obese diabetic (NOD) mice.
Experimental approach:
NOD mice exhibit a progressive endothelial dysfunction characterized by a reduced reactivity of blood vessels as diabetes develops. NOD mice were divided into three groups according to different glycosuria values: NOD I, NOD II and NOD III. Age-matched non-obese resistant (NOR) mice were used as controls. H2S levels in plasma and aortic tissue were measured. Functional studies in aorta were carried out in isolated organ baths using both an exogenous source of H2S (NaHS) and the metabolic precursor (L-cysteine). Real time PCR and western blot analysis were also carried out on aortic tissues.
Key results:
NOD mice exhibited a progressive reduction of H2S plasma levels, which paralleled disease severity. L-cysteine-induced H2S production by aortic tissues was also progressively reduced. L-cysteine-induced vasorelaxation was significantly reduced in NOD mice while NaHS-induced relaxation was unaffected. ODQ (guanylate cyclase inhibitor), L-NAME (NO synthase inhibitor) or PAG, an inhibitor of cystathionine-γ-lyase (CSE) inhibited H2S production induced by L-cysteine.
Conclusions and implications:
In NOD mice, endogenous H2S production is significantly impaired. Also, the ability of isolated aorta to respond to exogenous H2S is enhanced and endothelium-derived NO appears to be involved in the enzymatic conversion of L-cysteine into H2S.
Keywords: hydrogen sulphide, L-cysteine, endothelium, NOD mice
Introduction
Hydrogen sulphide (H2S) is a gas endogenously generated from L-cysteine, a sulphur-containing amino acid derived from alimentary sources or liberated from endogenous proteins. L-cysteine can also be synthesized from L-methionine through the transsulphuration pathway, with homocysteine as an intermediate (Zhao et al., 2001; Chen et al., 2004; Stipanuk, 2004). Production of H2S from L-cysteine is catalysed by two enzymes: cystathionine-β-synthase (CBS) and cystathionine-γ-lyase (CSE). Both enzymes are pyridoxal-5′-phosphate (vitamin B6)-dependent but differ in the specific mechanism of H2S formation (Braunstein and Azarkh, 1950). CBS and CSE are widely distributed in mammalian tissues and present data suggest that CBS is predominantly expressed in the CNS, whereas CSE is mostly present in the cardiovascular environment (Hosoki et al., 1997; van der Molen et al., 1997; Levonen et al., 2000; Yap et al., 2000; Meier et al., 2001; Wang, 2002; Moore et al., 2003). However, presence of CBS has also been assessed in endothelial cells (Wang et al., 1992).
Recent literature has supported the involvement of H2S in cardiovascular homoeostasis (Zhong et al., 2003; Yan et al., 2004; Bhatia, 2005; O'Sullivan, 2006; Pearson et al., 2006; Qu et al., 2006). In particular, it has been demonstrated that H2S (i) exhibits vasodilator activity in vitro and in vivo (Ali et al., 2006), (ii) is pro-apoptotic on vascular smooth muscle cells (Zhao et al., 2001; Cheng et al., 2004; Yang et al., 2004) and (iii) is involved in leukocyte–endotheliium interactions (Zanardo et al., 2006). All these findings, taken together with the fact that H2S levels, as well as aortic CSE mRNA, are reduced in spontaneously hypertensive rats, further support a role for H2S in cardiovascular inflammation (Du et al., 2003).
Here we have evaluated the effect of H2S on vascular tone in a genetic model of diabetes in mice, the non-obese diabetic (NOD) strain. NOD mice spontaneously develop diabetes, where the autoimmune disease is directly associated with a progressive endothelial dysfunction (Makino et al., 1980; Bucci et al., 2004).
In particular, we have evaluated the effect of H2S on aortic rings by using an exogenous source such as sodium hydrosulphide hydrate (NaHS) or its physiological precursor such as L-cysteine; this approach led us to evaluate both the direct effect of H2S on vessels and the contribution of endogenous pathways in regulating vascular tone.
Our results suggest that diabetes-related endothelial dysfunction in NOD mice is associated with an impairment of endogenous H2S production, without affecting the ability of vascular tissue to react to exogenous sources of H2S.
Materials and methods
Animals
All animal procedures were in compliance with the European Community guidelines for the use of experimental animals and approved by the Committee Centro Servizi Veterinari of the University Federico II; this work was carried out with NOD/Ltj mice purchased from Charles River Laboratories (Milan, Italy). All experiments were performed by using 7- to 27-week-old female mice. NOR/Ltj female mice were used as age-matched controls. Animals were bred and housed in our animal facility having free access to water and food.
NOD/Ltj mice
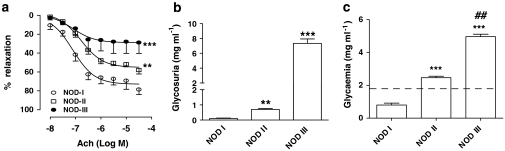
NOD mice represent a strain with an elevated susceptibility in developing type 1 diabetes (IDDM) (Makino et al., 1980). These mice show changes with evolution of pathology, in particular there is an early phase characterized by a localization of inflammatory cells, such as T cells and activated macrophages, around pancreatic islet, inducing peri-insulitis (4–10 weeks of age); consequently, these cells infiltrate islets and initiate a progressive destruction of pancreatic β cells, resulting in a drastic reduction in insulin plasma levels (12–30 weeks of age). The progression of diabetic pathology and its clinical outcomes in these animals are similar to those in humans and associated with vascular disorders. Indeed a gradual reduction of ACh-induced relaxation was found in aortic tissues harvested from NOD mice (Figure 1a) and this hyporeactivity correlated with a reduced availability of circulating nitric oxide (NO) (Bucci et al., 2004).
Figure 1.
(a) ACh-induced vasorelaxation was progressively reduced in NOD mice (**P<0.01 vs NOD I; ***P<0.001 vs NOD I; two-way ANOVA). (b) Glycosuria was progressively increased in NOD mice. (c) Increase in blood glucose levels was related to glycosuria (glycosuria: NOD I: 0 mg mL−1; NOD II: ∼0.8 mg mL−1; NOD III: ∼8 mg mL−1; blood glucose: NOD I: ∼0.9 mg mL−1; NOD II: ∼2.5 mg mL−1; NOD III: ∼5 mg mL−1) (**P<0.01 vs NOD I; ***P<0.001 vs NOD I; ##P<0.01 vs NOD II; one-way ANOVA). Discontinuous line indicates physiological value of blood glucose. NOD, non-obese diabetic.
NOD mice were divided into three groups, as follows, by measurement of glycosuria, and each group can be considered representative of different diabetic states (10 animals per group). Indeed, NOD I is a mouse group in which diabetic state is not yet present; NOD II group has glycosuria and elevated glycaemia; NOD III group displays a severe pathology with even higher levels of glycosuria and glycaemia (Doi et al., 1990) (Figures 1b and c).
Glycosuria measurement
In these animals, diabetic state was assessed by using a non-invasive approach such as measurement of glycosuria, the increase of which is positively correlated to glycaemia. Animals were deprived of food for 2 h to normalize glucose plasma levels and then put in metabolic cages for 4 h, where urine samples were collected. Glycosuria levels were measured by glucose-6-oxidase colorimetric assay (Trinder reaction kit; Biogamma, Roma, Italy). According to the glucose assays, mice were divided into three groups: NOD I, glycosuria, 0–0.20 mg mL−1; NOD II glycosuria, 0.2–5 mg mL−1; NOD III, glycosuria, >5 mg mL−1 (Figure 1b), to provide different stages of pathology.
Measurement of H2S: plasma and tissues
Tissue H2S production rate was measured according to Stipanuk and Beck (1982), with modifications. Briefly, aortas were homogenized in a lysis buffer (potassium phosphate buffer 100 mM pH=7.4, sodium orthovanadate 10 mM and proteases inhibitors). Protein concentration was determined by using Bradford assay (Bio-Rad Laboratories, Milano, Italy). Homogenates were added to a reaction mixture (total volume 500 μL) containing pyridoxal-5′-phosphate (2 mM, 20 μL), L-cysteine (10 mM, 20 μL) and saline (30 μL). The reaction was performed in sealed Eppendorf tubes and initiated by transferring tubes from ice to a water bath at 37 °C. After 40 min incubation, zinc acetate (1%, 250 μL) was added followed by trichloroacetic acid (10%, 250 μL). Subsequently, N,N-dimethylphenylendiamine sulphate (20 mM, 133 μL) in 7.2 M HCl and FeCl3 (30 mM, 133 μL) in 1.2 M HCl were added and optical absorbance of the solutions was measured after 20 min at a wavelength of 650 nm. All samples were assayed in duplicate and H2S concentration was calculated against a calibration curve of NaHS (3.12–250 μM). To determine basal release of H2S, L-cysteine was not added to the reaction mixture. Results were expressed as nmol per milligram of protein per minute (nmol per mg protein per min).
Plasma determination of H2S was performed without addition of L-cysteine. Plasma samples (100 μL) were added to Eppendorf tubes containing zinc acetate (1 % 150 μL). Trichloroacetic acid (10 % 300 μL) was then added. Subsequently, N,N-dimethylphenylendiamine sulphate (20 mM, 100 μL) in 7.2 M HCl and FeCl3 (30 mM, 133 μL) in 1.2 M HCl were added to the reaction mixture and absorbance of the solution was measured after 20 min at a wavelength of 650 nm. All samples were assayed in duplicate and H2S concentration was calculated against a calibration curve of NaHS (3.12–250 μM).
Tissue preparation
Animals were killed at different stages of pathology with age-matched NOR mice control and aortas were excised and plasma collected from each animal. Then tissues and plasma were used to quantify H2S amount by using the method described above. Furthermore, aortic tissues were also used for functional studies in isolated organ baths filled with oxygenated Krebs solution at 37 °C, linked to isometric force transducers (Fort 10, Ugo Basile, Comerio, Varese, Italy). The composition of Krebs solution was as follows (in mM): NaCl 118, KCl 4.7, MgSO4 1.2, KH2PO4 1.2, CaCl2 2.5, NaHCO3 25 and glucose 11. Rings were stretched until a resting tension of 1.5 g was reached and allowed to equilibrate for at least 45 min during which time tension was adjusted, as necessary, to 1.5 g and bathing solution was periodically changed. In a preliminary study, a resting tension of 1.5 g was found to develop optimal tension to stimulation with contracting agents.
In another set of experiments, aortic tissues harvested from NOR mice were incubated with 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one (ODQ) (5 μM), Nω-nitro-L-arginine methyl ester (L-NAME) (100 μM) and DL-propargylglycine (PAG) (10 mM) for 15 min at 37 °C in six-well plates in an oxygenated environment and then challenged with L-cysteine (3 mM) for 5 min. After incubation, tissues were snap-frozen in liquid nitrogen and H2S content was determined.
Experimental protocol and drug treatments
In our experiments, we used 5-HT as vasoconstrictor agent, as its action is unaffected in NOD mice (Bucci et al., 2004). In each set of experiments, rings were first challenged with 5-HT (1 μM) until the responses were reproducible. To verify endothelium integrity, an ACh cumulative concentration–response curve (10 nM–30 μM) was performed on 5-HT-precontracted rings. In this study, we used both NaHS and L-cysteine as source of H2S, a direct H2S donor and the physiological metabolic precursor, respectively. In particular, H2S release from L-cysteine is correlated to enzymatic activity of both CBS and CSE. NaHS and L-cysteine cumulative concentration–response curves were performed on 5-HT-precontracted rings harvested from NOR and NOD I, II and III mice.
A preliminary study on the optimal incubation time of the drug treatments and concentration was carried out (data not shown). L-NAME (100 μM) and ODQ (5 μM) were added to the organ baths containing 5-HT-precontracted rings. After 15 min of incubation, cumulative concentration–response curves to NaHS and L-cysteine were performed.
Western blots
Aortic tissue or BAEC was homogenized in modified RIPA buffer (Tris-HCl 50 mM, pH 7.4, Triton 1%, Na-deoxycholate 0.25%, NaCl 150 mM, EDTA 1 mM, phenylmethanesulphonylfluoride 1 mM, aprotinin 10 mg mL−1, leupeptin 20 mM, NaF 50 mM) using a Polytron homogenizer (two cycles of 10 s at maximum speed). After centrifugation of homogenates at 6500 g for 10 min, 10, 30 μg of the denatured proteins were separated on 10% sodium dodecyl sulphate polyacrylamide gels and transferred to a polyvinylidene fluoride membrane. Membranes were blocked by incubation in phosphate-buffered saline containing 0.1% v/v Tween 20 and 5% non-fat dry milk for 2 h, followed by overnight incubation at 4 °C with mouse polyclonal CBS (Abnova Novus Biologicals, Littleton, CO, USA) antibody (1:500) or mouse monoclonal CSE (Abnova Novus Biologicals) antibody (1:500). The filters were washed extensively in phosphate-buffered saline containing 0.1% v/v Tween 20, before incubation for 2 h with anti-horseradish-peroxidase-conjugated secondary antibody. Membranes were then washed and developed using Enhanced Chemiluminescence Substrate (ECL; Amersham Pharmacia Biotech, San Diego, CA, USA).
Quantitative real-time PCR
Quantization of the expression level of selected genes was performed by quantitative real-time PCR. Total RNA was isolated with TRIzol reagent (Invitrogen, Carlsbad, CA, USA) from mouse aortic rings. One microgram RNA was incubated with DNaseI (Invitrogen) for 15 min at room temperature followed by 95 °C for 5 min in the presence of 2.5 mM EDTA. The RNA was reverse-transcribed with Superscript III (Invitrogen) with random primers in a volume of 20 μL. For real-time PCR, 10 ng template was used in a 25 μL reaction containing 0.3 μM each primer and 12.5 μL of 2 × DyNAmo SYBR Green qPCR Kits (Finnzymes, Espoo, Finland).
All reactions were performed in triplicate using the following cycling conditions: 10 min at 95 °C, followed by 50 cycles of 95 °C for 10 s, 60 °C for 20 s and 72 °C for 20 s, using an iCycler iQ instrument (Biorad, Hercules, CA, USA). The mean value of the replicates for each sample was calculated and expressed as cycle threshold (CT: cycle number at which each PCR reaches a predetermined fluorescence threshold, set within the linear range of all reactions). The amount of gene expression was then calculated as the difference (ΔCT) between the CT value of the sample for the target gene and the mean CT value of that sample for the endogenous control (GAPDH). Relative expression was calculated as the difference (ΔΔCT) between the ΔCT values of the test and control samples for each target gene. The relative level of expression was measured as 2−ΔΔCT. All PCR primers were designed using the software PRIMER3-OUTPUT using published sequence data obtained from the NCBI database.
Mouse primers were as follows: CBS, (FWD) agaagtgccctggctgtaaa and (REV) caggactgtcgggatgaagt; CSE, (FWD) tgctgccaccattacgatta and (REV) gatgccaccctcctgaagta; GAPDH, (FWD) ctgagtatgtcgtggagtctac and (REV) gttggtggtgcaggatgcattg.
Statistical analysis
All data were expressed as mean±s.e.mean. Statistical analysis was performed by using one-way ANOVA and Dunnet as post-test, or two-way ANOVA and Bonferroni as post-test. Differences were considered statistically significant when P-value was less than 0.05.
Drugs
ACh, 5-HT, L-NAME, ODQ, pyridoxal-5′-phosphate hydrate, iron chloride (III) (FeCl3), N,N-dimethylphenylendiamine sulphate, zinc acetate and PAG were purchased from Sigma Chemical Co. (Milano, Italy). Trichloroacetic acid was purchased from Carlo Erba Reagents (Milano, Italy). NaHS and L-cysteine hydrochloride were purchased from Aldrich (Milano, Italy). Kit for enzymatic measurement of glucose levels (Trinder reaction kit) was purchased from BioGamma.
Results
Impairment of H2S production in NOD mice
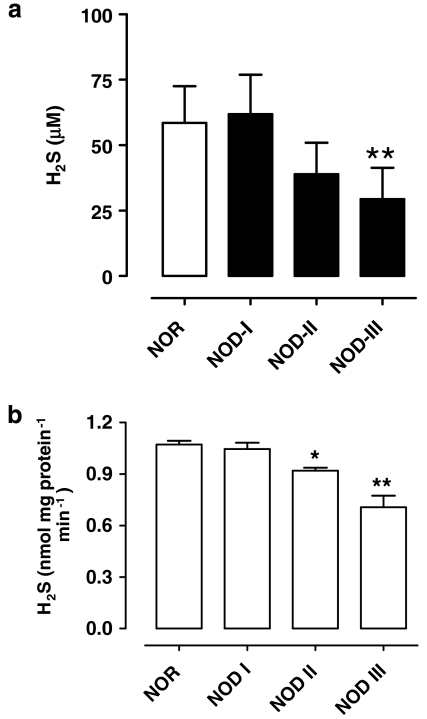
Plasma concentrations of H2S were between 50 and 65 μM in NOR mice. NOD mice exhibited a progressive reduction in H2S plasma levels, which paralleled the pathology development; in particular in NOD III mice, where the pathology is well established, there was a 50% reduction in H2S levels (Figure 2a; **P<0.01 vs NOR; n=6).
Figure 2.
(a) Plasma levels of H2S gradually decrease in NOD mice (**P<0.01 vs NOR; one-way ANOVA). (b) L-cysteine-stimulated H2S production in aortic tissues was significantly reduced in NOD II or NOD III mice (*P<0.05 and **P<0.01 vs NOR; one-way ANOVA). Basal values were unchanged (data not shown). NOD, non-obese diabetic.
To assess if impaired H2S production was reflected by an analogous dysfunction at vascular level, we evaluated the production of H2S in aortic tissues harvested from NOR or NOD mice. Our results showed that H2S basal production was not affected in NOD mice (data not shown), whereas the ability to convert L-cysteine into H2S was significantly impaired in aortic tissues harvested from NOD II mice and even more so in NOD III mice (Figure 2b; *P<0.05; **P<0.01 vs NOR; n=6).
Disease progression significantly affects L-cysteine-induced relaxation in NOD mice
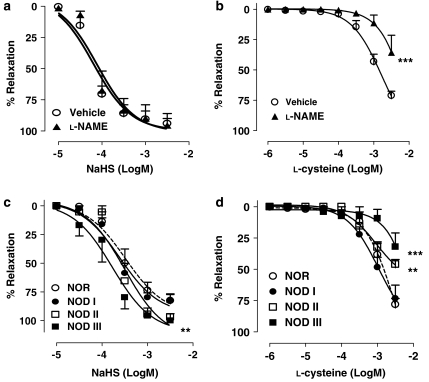
NaHS (1 μM–3 mM) induced a concentration-dependent vasorelaxation on 5-HT precontracted aortic rings harvested from NOR mice that was not affected by L-NAME (100 μM) pretreatment (Figure 3a). The relaxant response induced by NaHS in aortic rings from NOD I and NOD II mice was not significantly different from NOR mice (Figure 3c). Conversely, in NOD III mice, in which the pathology is well established and the endothelium is severely damaged, NaHS-induced vasorelaxation was significantly increased (Figure 3c; P<0.01 vs NOR; n=6).
Figure 3.
(a) NaHS vasorelaxant effect was not modified by L-NAME (100 μM) in NOR mice. (b) L-NAME (100 μM) pretreatment affected L-cysteine vasorelaxation in NOR mice (***P<0.001 vs vehicle; two-way ANOVA). (c) NaHS-induced vasorelaxation was not significantly affected in NOD I or NOD II mice, but enhanced in NOD III mice (dashed line: NOR mice) (P<0.01 vs NOR). (d) L-cysteine-induced vasodilatation was impaired in NOD mice and paralleled the disease development (dashed lines: NOR mice) (**P<0.01 vs NOR; ***P<0.001 vs NOR; two-way ANOVA). L-NAME, Nω-nitro-L-arginine methyl ester; NOD, non-obese diabetic.
Administration of L-cysteine (1 μM–3 mM) induced a relaxant effect on NOR mice aortic tissues, which was significantly inhibited by L-NAME (Figure 3b; ***P<0.001 vs vehicle; n=6). Disease progression leads to a significant decrease in L-cysteine-induced vasodilatation of aortic rings harvested from NOD II or NOD III mice (Figure 3d; **P<0.01 and ***P<0.001 vs NOR respectively; n=6). Endothelial removal did not affect vasorelaxation induced by either NaHS or L-cysteine (data not shown).
NO/cGMP signalling is involved in L-cysteine-induced vasorelaxation
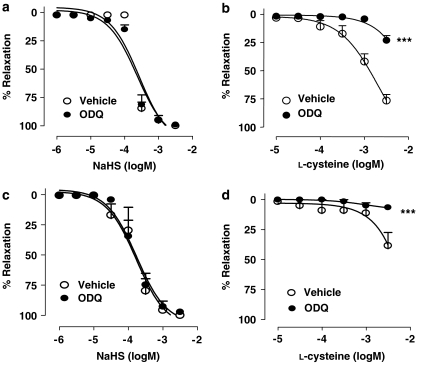
As we found that L-cysteine elicited an L-NAME-sensitive vasorelaxation and that its vasorelaxant effect was significantly reduced in NOD mice, we investigated the involvement of NO/cGMP pathway in the relaxant effects of L-cysteine by using ODQ, an NO-sensitive GC inhibitor. Incubation of NOR aortic rings with ODQ (5 μM, 10 min, n=6) inhibited L-cysteine-induced relaxation (Figure 4a; ***P<0.001 vs vehicle; n=6).
Figure 4.
ODQ (5 μM) does not affect NaHS-induced vasorelaxation either in (a) NOR or in (c) NOD III mice (ns, n=5). Conversely, in (b), ODQ (5 μM) significantly inhibits L-cysteine-induced vasorelaxant response in NOR mice (***P<0.001 vs vehicle, n=5; two-way ANOVA). (d) ODQ (5 μM) abolished L-cysteine-induced vasorelaxant response, already reduced in NOD III mice (d) (***P<0.001 vs vehicle, n=5; two-way ANOVA). NOD, non-obese diabetic; ODQ, 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one.
A similar pattern of inhibition was obtained in NOD mice aortas. In particular, in NOD III mice, the already impaired L-cysteine-induced vasorelaxation was abolished by pretreatment with ODQ (Figure 4d; ***P<0.001 vs vehicle; n=6). Conversely, the GC inhibitor did not affect NaHS-induced vasorelaxation in either NOR or NOD III mice (Figures 4a and c).
ODQ and L-NAME affect L-cysteine-derived H2S production
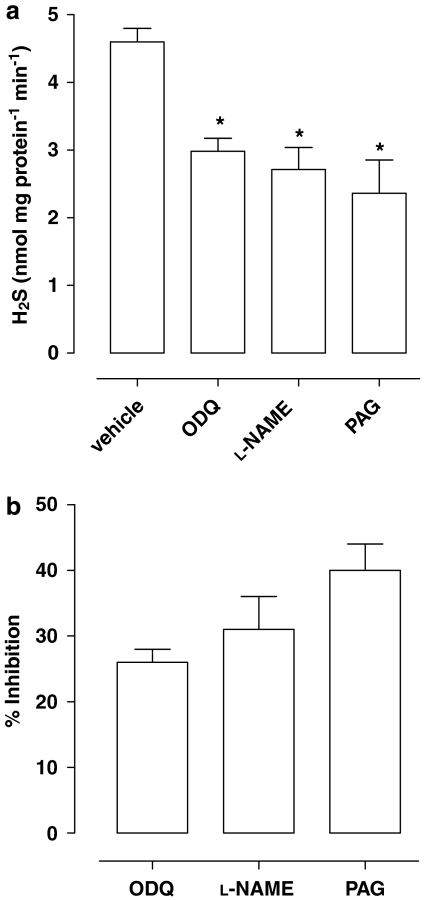
The inhibitory effect of ODQ on L-cysteine-induced vasorelaxation suggested an involvement of the NO/cGMP pathway in H2S signalling; to assess if this inhibitory effect was ascribed to the ability of ODQ to interfere with H2S release, aortic tissues harvested from NOR mice were incubated with L-cysteine in the presence of ODQ (5 μM, 15 min, n=3), and H2S production was measured; in another set of experiments, aortic tissues were pretreated with L-NAME or the CSE inhibitor, PAG (10 mM, 15 min).
Data obtained showed that incubation with ODQ or L-NAME reduced L-cysteine-induced H2S release in aortic tissues, as well as that with PAG (Figure 5; *P<0.05 vs L-cysteine), whereas they did not affect H2S basal release (data not shown).
Figure 5.
(a) Addition of exogenous L-cysteine (3 mM) to aortic tissues increased production of H2S by 40% (139±10 nmol per mg tissue), an effect that is lost when aortic tissues were pretreated with ODQ (5 μM) or L-NAME (100 μM). PAG (10 mM), an inhibitor of CSE, was used as positive control (*P<0.05 vs L-cysteine; one-way ANOVA, n=3). In (b), the data from (a) are expressed as % inhibition of L-cysteine-derived H2S production. The inhibitors used were without effect on basal H2S release (data not shown). CSE, cystathionine-γ-lyase; L-NAME, Nω-nitro-L-arginine methyl ester; ODQ, 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one; PAG, DL-propargylglycine.
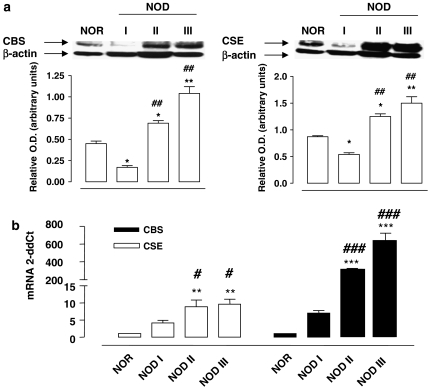
CBS and CSE expression is increased in NOD mice
Western blot and real-time PCR analysis was performed to evaluate if low levels of H2S in NOD mice correlated with a reduced expression of CBS or CSE. Despite the reduced circulating and tissue H2S levels measured in NOD mice, both western blot (Figure 6a) and quantitative real-time PCR (Figure 6b) showed a significant upregulation of either CBS and CSE in vessels harvested from NOD II and NOD III mice. This finding could be ascribed to a compensatory response to restore physiological H2S production.
Figure 6.
(a) Western blots show a significant increase in both CBS and CSE expression in NOD mice (*P<0.05 vs NOR; **P<0.01 vs NOR; ##P<0.01 vs NOD I; one-way ANOVA). Similarly, in (b), qRT-PCR confirmed the progressively increased expression of mRNA for CBS and CSE (**P<0.01 vs NOR; ***P<0.001 vs NOR; #P<0.05 vs NOD I; ###P<0.001 vs NOD I; one-way ANOVA). CBS, cystathionine-β-synthase; CSE, cystathionine-γ-lyase; NOD, non-obese diabetic; qRT-PCR, quantitative real-time PCR.
Discussion
NOD mice gradually develop a type 1 diabetes (Makino et al., 1980) that is characterized by a progressive endothelial dysfunction leading to an impaired response of vascular tissues in vitro (Bucci et al., 2004). Here we have addressed the involvement of the H2S pathway in vascular dysfunction in NOD mice. When we measured H2S plasma levels, we found values around 50 μM in NOR mice, whereas NOD mice exhibited a progressive reduction of H2S plasma levels that paralleled the disease severity, reaching 50% reduction in NOD III mice. To determine if the reduced plasma levels reflected a similar impairment in the vessels, we determined the amount of H2S produced by homogenates of aortic tissues harvested from NOR, NOD I, NOD II or NOD III mice; the assay was performed both in the absence (basal) and in the presence (stimulated) of the substrate L-cysteine. Although the basal release of H2S was unchanged, the stimulated production was progressively reduced, paralleling the disease progression.
Taken together, the biochemical data suggest that in this experimental model, there is a gradual impairment of H2S production. The functional studies showed that in NOD mice, the response to exogenous H2S (as NaHS) was not altered whereas the response to L-cysteine was impaired. Indeed, responses of NOD mice to NaHS were not significantly different from those of NOR (background) mice, with the only exception of NOD III mice where they were potentiated. Conversely, L-cysteine-induced vasodilatation was significantly impaired in all three NOD groups, paralleling the disease progression. As NOD mice exhibited a specific impairment in NO-mediated vasorelaxation (Bucci et al., 2004), we assessed the involvement of the endothelium-derived NO in L-cysteine-induced vasorelaxation. Functional studies showed that in physiological conditions (NOR mice), L-NAME pretreatment significantly reduced L-cysteine-induced vasorelaxation, whereas NaHS-induced vasodilatation was unaffected. A similar pattern was observed in NOD I mice that have normal glycosuria/glycaemia. Thus, the endothelial-derived NO pathway seems to be involved in L-cysteine-induced vasorelaxation, as also confirmed by experiments performed with ODQ.
It has been shown that H2S-induced vasorelaxation is not affected by endothelium removal, suggesting that endothelium is not involved in the H2S effect at vascular level (Hosoki et al., 1997; Zhao et al., 2001; Wang, 2002). This finding is apparently in contrast with our data. However, it has to be said that mechanical removal of endothelium only partially mimics the pathological condition known as endothelial dysfunction. Indeed, the alteration of endothelium functionality, in the majority of the cases, is a gradual and progressive process and cannot be simply and directly related to a mechanical and a nonspecific disruption of whole endothelium. Therefore, it is feasible that modulation of GC, in turn, could modulate L-cysteine-induced response (endogenous H2S response; that is, involving conversion of the substrate) without affecting NaHS-induced vasodilatation (exogenous H2S response). To test this hypothesis, we compared the vasodilatory response elicited by either NaHS or L-cysteine following pharmacological modulation with ODQ, an inhibitor of soluble GC. This comparison was performed by using tissues harvested from either NOR (normal) or NOD III mice (severe diabetes). As expected, incubation with ODQ did not affect NaHS-induced vasorelaxation in either NOR or NOD III mice, whereas it did cause a marked inhibition of L-cysteine-induced vasorelaxation. In particular, L-cysteine-induced vasorelaxation was significantly inhibited in rings harvested from NOR mice and abolished in tissues harvested from NOD III mice, where the L-cysteine response was already impaired. These findings, together with the previous data, imply that, in NOD mice, endogenous L-cysteine-induced vasorelaxation (endogenous H2S) could be modulated by the NO pathway through GC activation.
Different levels of interaction have been shown for NO and H2S pathways. Thus, NO may directly act on CSE protein to increase its activity (Zhao et al., 2003). Also, NO may increase the activity of cGMP-dependent protein kinase, which in turn stimulates CSE, and NO can upregulate the expression of CSE, promoting cell uptake of cysteine, the substrate for CSE (Zhang and Hogg, 2005; Sheng and Wharton, 2006).
To assess if both L-NAME and ODQ inhibited L-cysteine-induced vasorelaxation by reducing L-cysteine-derived H2S production, we measured H2S in aortic tissues harvested from NOR mice. Our results showed that ODQ, L-NAME or the CSE inhibitor PAG, significantly affected the ability of vascular tissue to metabolize L-cysteine in H2S.
In conclusion, our results showed that endogenous H2S production is significantly impaired in hyperglycaemic conditions in NOD mice, although the ability of vascular tissue to respond to exogenous H2S was not altered. Furthermore, we suggest that endothelium-derived NO has an active role in modulating activity of the L-cysteine/H2S pathway and that the reduced vasorelaxant effect of L-cysteine may originate in a reduced ability of vascular tissue to convert L-cysteine to H2S.
Abbreviations
- CBS
cystathionine-β-synthase
- CSE
cystathionine-γ-lyase
- H2S
hydrogen sulphide
- L-NAME
Nω-nitro-L-arginine methyl ester
- NOD
non-obese diabetic
- NOR
non-obese resistant
- ODQ
1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one
- PAG
DL-propargylglycine
Conflict of interest
The authors state no conflict of interest.
References
- Ali MY, Ping CY, Mok YY, Ling L, Whiteman M, Bhatia M, et al. Regulation of vascular nitric oxide in vitro and in vivo; a new role for endogenous hydrogen sulphide. Br J Pharmacol. 2006;149:625–634. doi: 10.1038/sj.bjp.0706906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatia M. Hydrogen sulfide as a vasodilator. IUBMB Life. 2005;57:603–606. doi: 10.1080/15216540500217875. [DOI] [PubMed] [Google Scholar]
- Braunstein AE, Azarkh RM. Participation of vitamin B6 in enzymic formation of hydrogen sulfide from L-cysteineteine. Dokl Akad Nauk SSSR. 1950;71:93–96. [Google Scholar]
- Bucci M, Roviezzo F, Brancaleone V, Lin MI, Di Lorenzo A, Cicala C, et al. Diabetic mouse angiopathy is linked to progressive sympathetic receptor deletion coupled to an enhanced caveolin-1 expression. Arterioscler Thromb Vasc Biol. 2004;24:721–726. doi: 10.1161/01.ATV.0000122362.44628.09. [DOI] [PubMed] [Google Scholar]
- Chen X, Jhee KH, Kruger WD. Production of the neuromodulator H2S by cystathionine beta-synthase via the condensation of cysteine and homocysteine. J Biol Chem. 2004;279:52082–52086. doi: 10.1074/jbc.C400481200. [DOI] [PubMed] [Google Scholar]
- Cheng Y, Ndisang JF, Tang G, Cao K, Wang R. Hydrogen sulfide-induced relaxation of resistance mesenteric artery beds of rats. Am J Physiol Heart Circ Physiol. 2004;287:H2316–H2323. doi: 10.1152/ajpheart.00331.2004. [DOI] [PubMed] [Google Scholar]
- Doi T, Hattori M, Agodoa LY, Sato T, Yoshida H, Striker LJ, et al. Glomerular lesions in nonobese diabetic mouse: before and after the onset of hyperglycemia. Lab Invest. 1990;63:204–212. [PubMed] [Google Scholar]
- Du J, Yan H, Tan C. Endogenous H2S is involved in the development of spontaneous hypertension. Beijing Da Xue Xue Bao. 2003;35:102–109. [PubMed] [Google Scholar]
- Hosoki R, Matsuki N, Kimura H. The possible role of hydrogen sulphide as an endogenous smooth muscle relaxant in synergy with nitric oxide. Biochem Biophys Res Commun. 1997;237:527–531. doi: 10.1006/bbrc.1997.6878. [DOI] [PubMed] [Google Scholar]
- Levonen AL, Lapatto R, Saksela M, Raivio KO. Human cystathionine gamma-lyase: developmental and in vitro expression of two isoforms. Biochem J. 2000;347:291–295. [PMC free article] [PubMed] [Google Scholar]
- Makino S, Kunimoto K, Muraoka Y, Mizushima Y, Katagiri K, Tochino Y. Breeding of a non-obese, diabetic strain of mice. Jikken Dobutsu. 1980;29:1–13. doi: 10.1538/expanim1978.29.1_1. [DOI] [PubMed] [Google Scholar]
- Meier M, Janosik M, Kery V, Kraus JP, Burkhard P. Structure of human cystathionine beta-synthase: a unique pyridoxal 5′-phosphate-dependent heme protein. EMBO J. 2001;20:3910–3916. doi: 10.1093/emboj/20.15.3910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore PK, Bhatia M, Moochhala S. Hydrogen sulfide: from the smell of the past to the mediator of the future. Trends Pharmacol Sci. 2003;24:609–611. doi: 10.1016/j.tips.2003.10.007. [DOI] [PubMed] [Google Scholar]
- O'Sullivan SE. What is the significance of vascular hydrogen sulphide (H2S) Br J Pharmacol. 2006;149:609–610. doi: 10.1038/sj.bjp.0706907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson RJ, Wilson T, Wang R. Endogenous hydrogen sulfide and the cardiovascular system—what's the smell all about. Clin Invest Med. 2006;29:146–150. [PubMed] [Google Scholar]
- Qu K, Chen CP, Halliwell B, Moore PK, Wong PT. Hydrogen sulfide is a mediator of cerebral ischemic damage. Stroke. 2006;37:889–893. doi: 10.1161/01.STR.0000204184.34946.41. [DOI] [PubMed] [Google Scholar]
- Sheng L, Wharton RA. Functional characterization of two S-nitroso-L-cysteineteine transporters, which mediate movement of NO equivalent into vascular cells. Am J Physiol Cell Physiol. 2006;292:C1263–C1271. doi: 10.1152/ajpcell.00382.2006. [DOI] [PubMed] [Google Scholar]
- Stipanuk MH. Sulfur amino acid metabolism: pathways for production and removal of homocysteine and cysteine. Annu Rev Nutr. 2004;24:539–577. doi: 10.1146/annurev.nutr.24.012003.132418. [DOI] [PubMed] [Google Scholar]
- Stipanuk MH, Beck PW. Characterization of the enzymatic capacity for cysteine desulphydration in liver and kidney of the rat. Biochem J. 1982;206:267–277. doi: 10.1042/bj2060267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Molen EF, Hiipakka MJ, van Lith-Zanders H, Boers GH, van den Heuvel LP, Monnens LA, et al. Homocysteine metabolism in endothelial cells of a patient homozygous for cystathionine beta-synthase (CS) deficiency. Thromb Haemost. 1997;78:827–833. [PubMed] [Google Scholar]
- Wang J, Dudman NP, Wilcken DE, Lynch JF. Homocysteine catabolism: levels of 3 enzymes in cultured human vascular endothelium and their relevance to vascular disease. Atherosclerosis. 1992;97:97–106. doi: 10.1016/0021-9150(92)90055-l. [DOI] [PubMed] [Google Scholar]
- Wang R. Two's company, three's a crowd: can H2S be the third endogenous gaseous transmitter. FASEB J. 2002;16:1792–1798. doi: 10.1096/fj.02-0211hyp. [DOI] [PubMed] [Google Scholar]
- Yan H, Du J, Tang C. The possible role of hydrogen sulfide on the pathogenesis of spontaneous hypertension in rats. Biochem Biophys Res Commun. 2004;313:22–27. doi: 10.1016/j.bbrc.2003.11.081. [DOI] [PubMed] [Google Scholar]
- Yang G, Sun X, Wang R. Hydrogen sulfide-induced apoptosis of human aorta smooth muscle cells via the activation of mitogen-activated protein kinases and caspase-3. FASEB J. 2004;18:1782–1784. doi: 10.1096/fj.04-2279fje. [DOI] [PubMed] [Google Scholar]
- Yap S, Naughten ER, Wilcken B, Wilcken DE, Boers GH. Vascular complications of severe hyperhomocysteinemia in patients with homocystinuria due to cystathionine beta-synthase deficiency: effects of homocysteine-lowering therapy. Semin Thromb Hemost. 2000;26:335–340. doi: 10.1055/s-2000-8100. [DOI] [PubMed] [Google Scholar]
- Zanardo RC, Brancaleone V, Distrutti E, Fiorucci S, Cirino G, Wallace JL. Hydrogen sulfide is an endogenous modulator of leukocyte-mediated inflammation. FASEB J. 2006;20:2118–2120. doi: 10.1096/fj.06-6270fje. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Hogg N. S-nitrosothiols: cellular formation and transport. Free Radic Biol Med. 2005;38:831–838. doi: 10.1016/j.freeradbiomed.2004.12.016. [DOI] [PubMed] [Google Scholar]
- Zhao W, Ndisang JF, Wang R. Modulation of endogenous production of H2S in rat tissues. Can J Physiol Pharmacol. 2003;81:848–853. doi: 10.1139/y03-077. [DOI] [PubMed] [Google Scholar]
- Zhao W, Zhang J, Lu Y, Wang R. The vasorelaxant effect of H2S as a novel endogenous gaseous K(ATP) channel opener. EMBO J. 2001;20:6008–6016. doi: 10.1093/emboj/20.21.6008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong G, Chen F, Cheng Y, Tang C, Du J. The role of hydrogen sulfide generation in the pathogenesis of hypertension in rats induced by inhibition of nitric oxide synthase. J Hypertens. 2003;21:1879–1885. doi: 10.1097/00004872-200310000-00015. [DOI] [PubMed] [Google Scholar]