Abstract
OBJECTIVE:
Pulmonary surfactant is a complex molecule of lipids and proteins synthesized and secreted by type II alveolar cells into the alveolar epithelial lining. Both lipids and protein components are essential for lung function in postnatal life. Infection is a well-established cause of preterm delivery and several inflammatory cytokines play a role in the mechanisms of preterm parturition. An increased concentration of inflammatory cytokines in amniotic fluid or fetal plasma has been linked to the onset of preterm parturition and fetal/neonatal injury including cerebral palsy and chronic lung disease. Experimental evidence indicated that inflammatory mediators also regulated surfactant protein synthesis and histologic chorioamnionitis was associated with a decreased incidence of hyaline membrane disease in neonates. This study was conducted to determine if amniotic fluid concentration of surfactant protein (SP)-A, SP-B and SP-D changes in patients with and without intra-amniotic infection (IAI).
MATERIAL AND METHODS:
A case-control study was conducted to determine amniotic fluid concentrations of SP-A, SP-B, SP-D, and total protein in patients who had an amniocentesis performed between 18 and 34 weeks of gestation for the detection of IAI in patients with spontaneous preterm labor with intact membranes (n=42) and cervical insufficiency prior to the application for cerclage (n=6). Amniotic fluid samples were selected from a bank of biological specimens and included patients with (n=16) and without (n=32) IAI matched for gestational age at amniocentesis. Intra-amniotic infection was defined a positive amniotic fluid culture for microorganisms. Each group was further subdivided according to a history of corticosteroid administration within 7 days prior to amniocentesis into the following subgroups: 1) patients without IAI who had received antenatal corticosteroid (n=21); 2) patients with IAI who had received antenatal corticosteroid (n=9); 3) patients without IAI who had not received antenatal corticosteroid (n=11); and 4) patients with IAI who had not received antenatal corticosteroid (n=7). Amniotic fluid was obtained by trans-abdominal amniocentesis. SP-A, SP-B, and SP-D concentrations in amniotic fluid were determined by enzyme-linked immunosorbent assay (ELISA). Non-parametric statistics were used for analysis.
RESULTS:
Women with IAI had a higher median amniotic fluid concentration of SP-B and of SP-B/total protein, but not other SPs, than those without IAI (both p=0.03). Among patients who had received antenatal corticosteroids, the median amniotic fluid concentration of SP-B and of SP-B/total protein was significantly higher in patients with IAI than in those without IAI (SP-B; IAI: median 148 ng/ml, range 37.3-809 ng/ml vs. without IAI: median 7.2 ng/ml, range 0 -1,035 ng/ml; p=0.005 and SP-B/total protein; IAI: median 14.1 ng/mg, range 4.3-237.5 ng/mg vs. without IAI: median 1.45 ng/mg, range 0 79.5 ng/mg; p=0.003). Among women who had not received antenatal corticosteroid, the median amniotic fluid concentration of SP-B and of SP-B/total protein was not significantly different between patients with and without IAI (SP-B; IAI: median 4 ng/ml, range 0-31.4 ng/ml vs. without IAI: median 3.4 ng/ml, range 0-37 ng/ml; p=0.8 and SP-B/total protein; IAI: median 0.55 ng/mg, range 0-6.96 ng/mg vs. without IAI: median 0.59 ng/mg, range 0-3.28 ng/mg; p=0.9). The median amniotic fluid concentrations of SP-A, SP-A/total protein, SP-D and SP-D/total protein were not significantly different between patients with and without IAI whether they received antenatal corticosteroid or not (all p>0.05).
CONCLUSIONS:
IAI was associated with an increased amniotic fluid concentration of SP-B in patients who received antenatal corticosteroids within 7 days prior to amniocentesis.
Keywords: Surfactant protein, SP-A, SP-B, SP-D, intra-amniotic infection, amniotic fluid, preterm labor, preterm parturition
INTRODUCTION
Intrauterine infection has been implicated in the etiology of preterm birth and is present in approximately 25% of all preterm deliveries.[1,2] An increased concentration of proinflammatory cytokines in amniotic fluid and fetal plasma have been linked to the onset of preterm parturition and fetal or neonatal injury including cerebral palsy[3-5] and chronic lung disease.[6-8] A recent study suggests that neonates with histologic chorioamnionitis had a decreased incidence of hyaline membrane disease,[9] possibly through the increased production of surfactant protein (SP).[9]
Pulmonary surfactants are composed of a lipid-protein complex. Currently, four types of SPs have been characterized as SP-A, B, C and D. SP-A and SP-D are hydrophilic and involved in host defense against infection, regulation of surfactant structure or homeostasis and immunomodulation.[10-12] In contrast, SP-B and C are hydrophobic and essential for lung function after birth.[10-12] Alveolar type II cells in the lung alveoli synthesize all four SPs and surfactant lipids. That all SPs are present in amniotic fluid is thought to be the result of lung liquid production and fetal respiration.
Several studies reported a complex association between infection/inflammatory mediators and SP mRNA expression in lung tissues or protein concentration in bronchoalveolar lavage fluid.[13-15] Animal experiments in pregnant ewes,[16-18] rabbits,[19] and mice[20] have suggested that endotoxin and inflammatory cytokines regulate SP synthesis, the effects of which varied depending on the stage of pulmonary airway maturation (or gestational age),[14,21] duration of exposure,[16,21] and routes of administration (i.e., intratracheal or intraamniotic).[17,22,23] Moreover, the administration of glucocorticoids to animals[24-27] or lung tissue explants[28-31] modulates SP expression. However, there is paucity of information on SP concentration in human amniotic fluid in the context of intrauterine infection. The purpose of this study was to determine whether amniotic fluid concentration of SP-A, B and D changes in patients with and without intra-amniotic infection (IAI).
MATERIAL AND METHODS
Study design
A case-control study was conducted to determine the amniotic fluid concentration of SP-A, SP-B, SP-D and total protein in patients who had an amniocentesis performed between 18 and 34 weeks of gestation at Hutzel Women's Hospital from July 1998 to December 2000. Amniotic fluid samples were selected from a bank of biological specimens and included samples from patients with (n=16) and without (n=32) IAI. Intra-amniotic infection was defined as a positive amniotic fluid culture for microorganisms. Both groups were matched (1:2) for gestational age (within 2 weeks) at amniocentesis. The two groups were further subdivided according to a history of corticosteroid administration (to induce fetal lung maturity) within 7 days prior to amniocentesis into the following subgroups: 1) patients without IAI who had received antenatal corticosteroid (n=21); 2) patients with IAI who had received antenatal corticosteroid (n=9); 3) patients without IAI who had not received antenatal corticosteroid (n=11); and 4) patients with IAI who had not received antenatal corticosteroid (n=7). Amniotic fluid was obtained by trans-abdominal amniocentesis. A sample of amniotic fluid was transported to the laboratory for aerobic, anaerobic, and genital Mycoplasma cultures. Amniotic fluid not required for clinical purposes was centrifuged and stored. The indication for amniocentesis was for the detection of IAI in patients with the diagnosis of: 1) spontaneous preterm labor and intact membranes (n=42) and 2) cervical insufficiency prior to the application of cerclage (n=6).
All women provided informed consent prior to the collection of amniotic fluid. The collection and utilization of the samples was approved by the Human Investigation Committee of the Wayne state university, Detroit, MI, USA and approved for research purposes by the IRB of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Many of these samples have been used in previous studies of inflammatory mediators, antibacterial peptides and chemokines.[32-34]
Enzyme-linked immunosorbent assay for determining the SP-A, SP-B, and SP-D concentrations in amniotic fluid
The SP-A, SP-B, and SP-D concentrations in amniotic fluid were determined by a sandwich enzyme-linked immunosorbent assay (ELISA) system, which had been validated for amniotic fluid as previously described.[35-37] For SP-A, the inter- and intra-assay coefficients of variations (CV) were 33.5% and 7.7%, respectively; and the sensitivity was 10 ng/ml. For SP-B, the inter- and intra-assay CV were 34.2% and 18.7%, respectively; and the sensitivity was 2 ng/ml. For SP-D, the inter- and intra-assay CV were 19.6% and 4.6%, respectively; and the sensitivity was 10 ng/ml.
Statistical analysis
Mann-Whitney U test was utilized to determine differences in the median between groups. Contingency tables and Chi-square tests were employed for comparisons of proportions. A p value of <0.05 was considered significant. The statistic package used were SPSS 12.0 (SPSS Inc, Chicago, Illinois, USA).
RESULTS
Table I describes the clinical and obstetric characteristics of the study population. There was no significant difference in the median maternal age and gestational age at amniocentesis between patients with and without IAI. Patients with IAI had a median gestational age at delivery and neonatal birth weight lower than those without IAI.
Table I.
Clinical and obstetrical characteristics of patients with and without intra-amniotic infection (IAI)
| without IAI (n=32) |
with IAI (n=16) |
p | |
|---|---|---|---|
| Maternal age (years) | 21 (16-39) | 27 (16-36) | 0.09 |
| Nulliparity | 16 (50%) | 7 (43.8%) | 0.7 |
| Ethnicity | |||
| African-American | 26 (81.3%) | 15 (93.8%) | 0.4 |
| Caucasian | 4 (12.5%) | 1 (6.3%) | |
| Hispanic | 2 (6.3%) | 0 | |
| GA at amniocentesis (weeks) | 25.8 (18-33.3) | 25.7 (18.4-33.3) | 0.7 |
| GA at delivery (weeks) | 32 (19.1- 41.4) | 26.1 (18.5-33.3) | 0.01* |
| Birthweight (grams) | 1,610 (100-3750) | 625 (220-2300) | 0.007* |
GA: gestational age; values are presented as median (range) or numbers (percent);
p<0.05
SP-A was detected in all (46/46) samples, while SP-B was detected in 68.8% (33/48) of samples. SP-D was above the limit of detection in 40% (12/30) of cases.
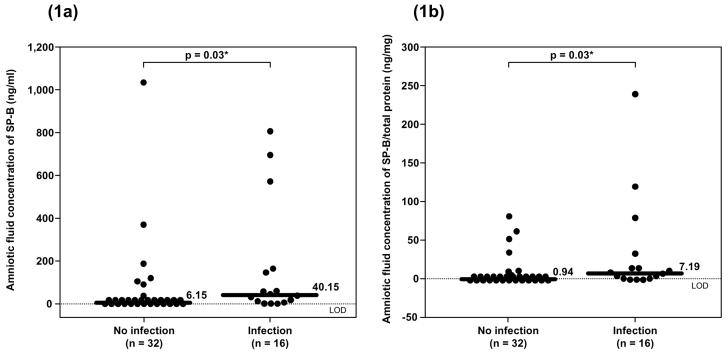
Patients with IAI had a significantly higher median amniotic fluid concentration of SP-B than those without IAI (IAI: median 40.2 ng/ml, range 0-809 ng/ml vs. without IAI: median 6.2 ng/ml, range 0-1,035 ng/ml; p=0.03; see Figure 1a). In contrast, there was no significant difference in the median amniotic fluid concentration of SP-A and SP-D (see Table II). Similar results were observed after adjusting the amniotic fluid SP concentration according to the total protein concentration (SP/total protein ratio; see Figure 1b and Table II). Using analysis of covariance adjusting for the duration of sample storage and gestational age at amniocentesis, similar results were obtained.
Figure 1a and 1b.
Median amniotic fluid concentration of SP-B was significantly higher in patients with intra-amniotic infection (IAI) than those without IAI (IAI: median 40.2 ng/ml, range 0-809 ng/ml vs. without IAI: median 6.2 ng/ml, range 0-1,035 ng/ml; p=0.03). Similar result was observed after adjusting the amniotic fluid SP-B concentration according to the total protein concentration (SP-B/ total protein; IAI: median 7.19 ng/mg, range 0-237.5 ng/mg vs. without IAI: median 0.94 ng/mg, range 0-79.5 ng/mg; p=0.03). *p<0.05. LOD = limit of detection.
Table II.
Amniotic fluid concentrations of SP-A and SP-D in patients with and without intra-amniotic infection (IAI)
| without IAI | with IAI | p | |
|---|---|---|---|
| SP-A (μg/ml) | 1.73 (0.74-4.45) | 1.56 (0.86-2.48) | 0.5 |
| n=32 | n=14 | ||
| SP-A/Pro (μg/mg) | 0.29 (0.07-1.24) | 0.21 (0.11-0.73) | 0.3 |
| n=32 | n=14 | ||
| SP-D (ng/ml) | 7.15 (0-25.2) | 8.05 (0-52.4) | 0.7 |
| n=20 | n=10 | ||
| SP-D/Pro (ng/mg) | 0 (0-7.27) | 0 (0-7.22) | 0.9 |
| n=20 | n=10 |
Values are presented as median (range)
Among patients who had received corticosteroid administration within 7 days before amniocentesis, there was no significant difference in the median gestational age at amniocentesis between patients with and without IAI (IAI: median 28.2 weeks range 24-33.3 weeks vs. without IAI: median 30 weeks range 23-33.3 weeks; p=0.9; see Table III).
Table III.
Clinical and obstetrics characters of patients who had and those who had not received antenatal corticosteroids within 7 days prior to amniocentesis classified by the presence or absence of intra-amniotic infection (IAI)
| steroids | no steroids | |||||
|---|---|---|---|---|---|---|
| without IAI (n=21) |
with IAI (n =9) |
p | without IAI (n=11) |
with IAI (n=7) |
p | |
| Maternal age (years) | 21 (19-39) | 25 (16-32) | 0.9 | 21 (16-26) | 30 (18-36) | 0.01* |
| GA at amniocentesis (weeks) | 30.0 (23.0-33.3) | 28.2 (24.0-33.3) | 0.9 | 22.0 (18.0-27.3) | 22.0 (18.4-26.2) | 0.9 |
| GA at delivery (weeks) | 35.0 (23.5-38.5) | 29.5 (24.1-33.3) | 0.1 | 26.0 (19.1- 41.4) | 22.6 (18.5-28.0) | 0.07 |
| Birthweight (grams) | 2230 (100-3750) | 1416 (500-2300) | 0.1 | 840 (320-3630) | 440 (220-1470) | 0.02* |
GA: gestational age; IAI: intra-amniotic infection; values are presented as median (range);
p<0.05
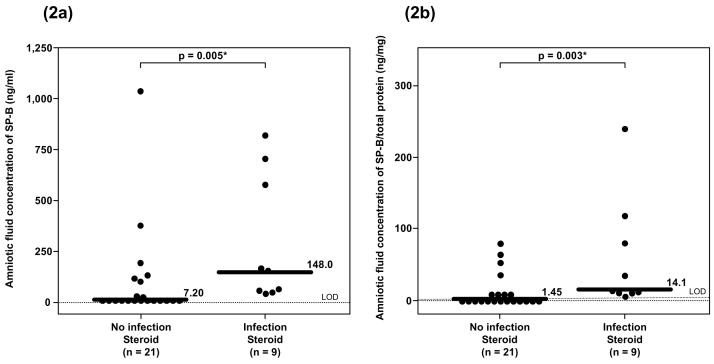
The median amniotic fluid concentration of SP-B and of SP-B/total amniotic fluid protein was significantly higher in patients with IAI than those without IAI (SP-B; IAI: median 148 ng/ml, range 37.3-809 ng/ml vs. without IAI: median 7.2 ng/ml, range 0-1,035 ng/ml; p=0.005 and SP-B/total protein; IAI: median 14.1 ng/mg, range 4.3-237.5 ng/mg vs. without IAI: median 1.45 ng/mg, range 0 -79.5 ng/mg; p=0.003; see Figure 2).
Figure 2a and 2b.
Among patients who had received antenatal corticosteroids within 7 days prior to amniocentesis, the median amniotic fluid concentration of SP-B was significantly higher in patients with intra-amniotic infection (IAI) than those without IAI (IAI: median 148 ng/ml, range 37.3-809 ng/ml vs. without IAI: median 7.2 ng/ml, range, 0-1,035 ng/ml; p=0.005). Similar result was observed after adjusting the amniotic fluid SP-B concentration according to the total protein concentration (SP-B/ total protein; IAI: median 14.1 ng/mg, range 4.3 -237.5 ng/mg vs. without IAI: median 1.45 ng/mg, range 0-79.5 ng/mg; p=0.003). *p<0.05. LOD = limit of detection.
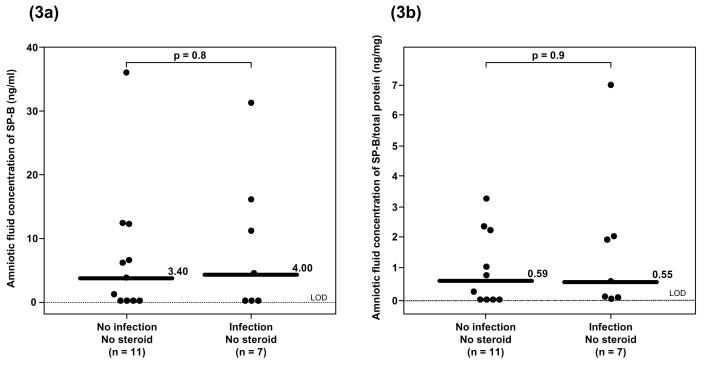
Similarly, among patients had not received have corticosteroid administration within 7 days before amniocentesis, there was no significant difference in the median gestational age at amniocentesis between patients with and without IAI (IAI: median 22 weeks range 18.4-26.2 weeks vs. without IAI: median 22 weeks range 18-27.3 weeks; p=0.9; see Table III). In contrast, among patients who had not received corticosteroid within 7 days before amniocentesis, the median amniotic fluid concentration of SP-B and of SP-B/total protein was not significantly different between patients with and without IAI (SP-B; IAI: median 4 ng/ml, range 0-31.4 ng/ml vs. without IAI: median 3.4 ng/ml, range 0-37 ng/ml; p=0.8 and SP-B/total protein; IAI: median 0.55 ng/mg, range 0-6.96 ng/mg vs. without IAI: median 0.59 ng/mg, range 0-3.28 ng/mg; p=0.9; see Figure 3).
Figure 3a and 3b.
Among patients who had not received antenatal corticosteroids within 7 days prior to amniocentesis, there was no significant difference in the median amniotic fluid concentration of SP-B between patients with and without intra-amniotic infection (IAI) (IAI: median 4 ng/ml, range 0-31.4 ng/ml vs. without IAI: median 3.4 ng/ml, range 0-37 ng/ml; p=0.8). Similar result was observed after adjusting the amniotic fluid SP-B concentration according to the total protein concentration (SP-B/total protein; IAI: median 0.55 ng/mg, range 0-6.9 ng/mg vs. without IAI: median 0.59 ng/mg, range 0-3.3 ng/mg; p=0.9). LOD = limit of detection.
The median amniotic fluid concentration of SP-A, SP-A/total protein, SP-D and SP-D/total protein were not significantly different between patients with and without IAI whether they had received antenatal corticosteroid or not (see Table IV).
Table IV.
Amniotic fluid concentrations of SP-A and SP-D in patients who had and those who had not received antenatal corticosteroids within 7 days prior to amniocentesis
| steroids | no steroids | |||||
|---|---|---|---|---|---|---|
| without IAI | with IAI | p | without IAI | with IAI | p | |
| SP-A (μg/ml) | 2.12 (0.74-4.45) | 1.75 (1.08-2.48) | 0.41 | 0.33 (0.82-4.34) | 1.49 (0.86-1.76) | 0.8 |
| n=21 | n=8 | n=11 | n=6 | |||
| SP-A/Pro (μg/mg) | 0.36 (0.08-1.24) | 0.27 (0.11-0.73) | 0.4 | 0.23 (0.07-0.84) | 0.20 (0.14-0.34) | 0.4 |
| n=21 | n=8 | n=11 | n=6 | |||
| SP-D (ng/ml) | 6.10 (0-25.2) | 10.6 (6.50-23.0) | 0.2 | 11.8 (0-24.4) | 6.2 (0-52.4) | 0.7 |
| n=15 | n=5 | n=5 | n=5 | |||
| SP-D/Pro (ng/mg) | 0 (0-7.27) | 1.03 (0-4.58) | 0.5 | 1.16 (0-4.01) | 0 (0-7.22) | 0.4 |
| n=15 | n=5 | n=5 | n=5 | |||
• IAI: intra-amniotic infection; values are presented as median (range)
DISCUSSION
Principal findings of this study
1) Intra-amniotic infection was found to be associated with an increase in the amniotic fluid concentration of SP-B, but not SP-A and SP-D, in patients who had received corticosteroid administration within 7 days prior to amniocentesis; 2) in contrast, among patients who had not received corticosteroids, amniotic fluid concentrations of SP-A, SP-B, and SP-D were not significantly different between those with and without IAI.
Infection, microbial products, pro-inflammatory cytokines and surfactant proteins
Intrauterine infection is associated with an increased amniotic fluid concentration of several pro inflammatory cytokines and chemokines such as interleukin (IL)-1, IL-8, IL-6, tumor necrosis factor (TNF)-α, monocyte chemotactic peptide-1 (MCP-1), etc.[1, 32, 38,39] Experimental evidence indicates that endotoxin and several cytokines regulate surfactant protein synthesis.[13-15] Administration of lipopolysaccharides (LPS) or IL-1α into the amniotic fluid cavity of rabbits up-regulates SP-A and SP-B mRNA expression in lung tissue, SP-A and SP-B protein in bronchoalveolar lavage, and improves lung function.[19] Recombinant IL-6 increases the production of SP-A mRNA expression and protein in H441-4, a human pulmonary adenocarcinoma cell line.[9] In contrast, TNF-α inhibited SP-A mRNA and protein synthesis but not SP-B.[40] Subsequent studies showed that the effect of infection/inflammation on the fetal lung differs depending on the gestational age and duration of exposure to intra-amniotic endotoxin/cytokines. For example, in rabbits, IL-1 α increased SP-A, SP-B and SP-C mRNA expression in immature lung explants but decreased the expression of these SPs in mature lungs.[14]
Similarly, studies in sheep suggested that intra-amniotic endotoxin in early gestation [21] programmed a response that resulted in an increased mRNA expression for SP-A, SP-B, as well as SP-C 65 days later (without a consistent effect on SP-D), and also markedly induced the processing of SP-B protein to its mature form.[17] However, the response was not normal maturation, but more likely to represent maldevelopment of the surfactant system since the large increase in lung tissue surfactant lipids was not accompanied by a corresponding increase in alveolar surfactant lipids and proteins. This increase in lung tissue surfactant without effective secretion is similar to the abnormalities observed in ventilated[21] preterm baboons who develop bronchopulmonary dysplasia.[21,41,42] In contrast, endotoxin exposure in later gestation causes parallel increases in tissue and alveolar surfactants.[21]
A time-course study in late-gestation sheep indicated that endotoxin induced injury in the first 24 hours causing a decrease in pneumocyte type II cells as well as SP-B protein, but an increase in HSP70 expression followed by an increase in pneumocyte type II cells, SP-B mRNA and protein in lung tissue and lavage fluid at 72 hours, which is consistent with tissue remodeling process.[43] Moreover, this group of investigators also suggested that a single endotoxin exposure in early gestation preferentially induce surfactant without alterations in alveolarization and a subtle increase in alveolar wall thickness. In contrast, endotoxin exposure in later gestation, around the period of alveolarization, or chronic exposure prior to that period, caused a decrease in alveolar numbers and the development of a small lung.[21] However, a subsequent study showed that the fetal lung, when assessed closer to term gestation, could recover and develop relatively normal.[44] Interestingly, LPS-induced changes in the lung following intra-amniotic injection required direct contact between LPS and the fetal lung, since occlusion of the airway prevented changes in the fetal lung.[45] Prince et al[20] suggested that LPS improved lung function in mice and increased the number of alveolar type II cells through stimulation of Toll-like receptor 4, and NF kappa B pathways.
In the present study, we did not find significant changes in the amniotic fluid concentration of any SPs in patients with IAI and without antenatal corticosteroid exposure. Since the median gestational age at aminocentesis in this group was only 22 weeks, it is possible that there was an increased concentration of SPs in the lung tissue of patients with IAI. However, these proteins might not be secreted into the amniotic fluid cavity similar to the ovservation from experiment in sheep [17]. Finally, information from experimentally-induced IAI may be different from that of natural-occurring human IAI.
Glucocorticoids and surfactant protein
Experimental evidence derived from human fetal lung explants suggest that glucocorticoids have marked dose-dependent, reversible, stimulatory effects on the mRNA expression for SP-B, SP-C[28] and a modest effect on SP-D.[30] In contrast, glucocorticoids had a biphasic response in SP-A mRNA expression.[29] An increase mRNA expression of SP-A was observed in human lung explants with exposure to low concentrations of dexamethasone (≤10 nM) for less than 48 hours, but decreased expression was observed after a longer exposure to low concentrations or incubation with high concentrations (100 nM) of dexamethasone.[29] However, these results contrast with those reported in lambs. Administration of betamethasone at weekly intervals for three weeks resulted in increased mRNA expression and protein expression for both SP-A and SP-B in fetal lung tissues and bronchoalveolar lavage fluid. In contrast, animals treated for 48 hours, had overexpression of SP-B mRNA.[31]
Our study did not examine the effect of steroids alone on the amniotic fluid concentration of SP in patients with and without IAI, since the median gestational age in patients who had not received antenatal steroids (22 weeks) was much lower than those who had received antenatal steroids (28 weeks) and the amniotic fluid concentrations of SP change with gestational age.[35,46-49]
Combined effects of cytokines and glucocorticoids on surfacta proteins
The present study showed that IAI was associated with an increased amniotic fluid concentrations of SP-B, but not SP-A or SP-D, in women who received corticosteroid administration within 7 days prior to amniocentesis. This observation is consistent with a study in rabbit lung explants.[50] Vayrynen et al[50] noted the synergistic effect of glucocorticoids and cytokines on lung surfactant and concluded that dexamethasone consistently increased SP-B mRNA in explants of lung tissue from all gestational ages. This study indicated that in immature lungs, IL-1α and dexamethasone additively increased the mRNA expression of SP-A and of SP-B. In contrast, in lung explants obtained later in gestation, SP-B and SP-C expression was suppressed by IL-1α, while glucocorticoids tended to increase the expression of SP-B and SP-C and prevented the IL-1-induced suppression effects.[50]
Strength and limitation of the study
This study is the first report evaluating amniotic fluid concentrations of SPs in patients with IAI. Moreover, the effects of antenatal steroid administration were examined. The majority of patients in our study had received antenatal steroids, which reflects clinical practice. After the NICHD consensus statement on the use of corticosteroids for fetal lung maturation in 1994, most patients who are at risk for preterm delivery between 24 to 34 weeks of gestation receive antenatal steroids. However, among patients who did not receive antenatal steroids, our study did not find significant changes in the amniotic fluid concentrations of any SPs in patients with IAI. This is probably due to the fact that the median gestational age of patients in these subgroups was 22 weeks (range 18-27 weeks), which may be too early to observe a significant changes in SPs because of the low concentrations of these proteins in amniotic fluid. Moreover, the ELISA assay system which had been validated for amniotic fluid [35-37] had slightly high inter- and intra-assay coefficients of variation. So far, there was no commercially available assay for surfactant proteins (except SP-D).
In conclusion, intra-amniotic infection was associated with a variable, but significantly increased amniotic fluid concentration of SP-B in patients who received antenatal corticosteroids within 7 days prior to amniocentesis. This observation supports the view that there may be a beneficial effect of antenatal steroids administration in patients with sub-clinical intrauterine infection.
Acknowledgment
This research was supported in part by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS.
Reference List
- 1.Romero R, Mazor M, Wu YK, Sirtori M, Oyarzun E, Mitchell MD, Hobbins JC. Infection in the pathogenesis of preterm labor. Semin.Perinatol. 1988;12:262–279. [PubMed] [Google Scholar]
- 2.Goncalves LF, Chaiworapongsa T, Romero R. Intrauterine infection and prematurity. Ment.Retard.Dev.Disabil.Res.Rev. 2002;8:3–13. doi: 10.1002/mrdd.10008. [DOI] [PubMed] [Google Scholar]
- 3.Yoon BH, Jun JK, Romero R, Park KH, Gomez R, Choi JH, Kim IO. Amniotic fluid inflammatory cytokines (interleukin-6, interleukin-1beta, and tumor necrosis factor-alpha), neonatal brain white matter lesions, and cerebral palsy. Am.J Obstet.Gynecol. 1997;177:19–26. doi: 10.1016/s0002-9378(97)70432-0. [DOI] [PubMed] [Google Scholar]
- 4.Yoon BH, Romero R, Park JS, Kim CJ, Kim SH, Choi JH, Han TR. Fetal exposure to an intra-amniotic inflammation and the development of cerebral palsy at the age of three years. Am.J Obstet.Gynecol. 2000;182:675–681. doi: 10.1067/mob.2000.104207. [DOI] [PubMed] [Google Scholar]
- 5.Yoon BH, Park CW, Chaiworapongsa T. Intrauterine infection and the development of cerebral palsy. BJOG. 2003;110(Suppl 20):124–127. doi: 10.1016/s1470-0328(03)00063-6. [DOI] [PubMed] [Google Scholar]
- 6.Yoon BH, Romero R, Jun JK, Park KH, Park JD, Ghezzi F, Kim BI. Amniotic fluid cytokines (interleukin-6, tumor necrosis factor-alpha, interleukin-1 beta, and interleukin-8) and the risk for the development of bronchopulmonary dysplasia. Am.J Obstet.Gynecol. 1997;177:825–830. doi: 10.1016/s0002-9378(97)70276-x. [DOI] [PubMed] [Google Scholar]
- 7.Ghezzi F, Gomez R, Romero R, Yoon BH, Edwin SS, David C, Janisse J, Mazor M. Elevated interleukin-8 concentrations in amniotic fluid of mothers whose neonates subsequently develop bronchopulmonary dysplasia. Eur.J Obstet.Gynecol Reprod.Biol. 1998;78:5–10. doi: 10.1016/s0301-2115(97)00236-4. [DOI] [PubMed] [Google Scholar]
- 8.Yoon BH, Romero R, Kim KS, Park JS, Ki SH, Kim BI, Jun JK. A systemic fetal inflammatory response and the development of bronchopulmonary dysplasia. Am.J Obstet.Gynecol. 1999;181:773–779. doi: 10.1016/s0002-9378(99)70299-1. [DOI] [PubMed] [Google Scholar]
- 9.Shimoya K, Taniguchi T, Matsuzaki N, Moriyama A, Murata Y, Kitajima H, Fujimura M, Nakayama M. Chorioamnionitis decreased incidence of respiratory distress syndrome by elevating fetal interleukin-6 serum concentration. Hum.Reprod. 2000;15:2234–2240. doi: 10.1093/humrep/15.10.2234. [DOI] [PubMed] [Google Scholar]
- 10.Whitsett JA. Surfactant proteins in innate host defense of the lung. Biol.Neonate. 2005;88:175–180. doi: 10.1159/000087580. [DOI] [PubMed] [Google Scholar]
- 11.Whitsett JA, Weaver TE. Hydrophobic surfactant proteins in lung function and disease. N.Engl.J Med. 2002;347:2141–2148. doi: 10.1056/NEJMra022387. [DOI] [PubMed] [Google Scholar]
- 12.Wright JR. Immunoregulatory functions of surfactant proteins. Nat.Rev.Immunol. 2005;5:58–68. doi: 10.1038/nri1528. [DOI] [PubMed] [Google Scholar]
- 13.Dhar V, Hallman M, Lappalainen U, Bry K. Interleukin-1 alpha upregulates the expression of surfactant protein-A in rabbit lung explants. Biol.Neonate. 1997;71:46–52. doi: 10.1159/000244396. [DOI] [PubMed] [Google Scholar]
- 14.Glumoff V, Vayrynen O, Kangas T, Hallman M. Degree of lung maturity determines the direction of the interleukin-1- induced effect on the expression of surfactant proteins. Am.J Respir.Cell Mol.Biol. 2000;22:280–288. doi: 10.1165/ajrcmb.22.3.3788. [DOI] [PubMed] [Google Scholar]
- 15.Vayrynen O, Glumoff V, Hallman M. Regulation of surfactant proteins by LPS and proinflammatory cytokines in fetal and newborn lung. Am.J Physiol Lung Cell Mol.Physiol. 2002;282:L803–L810. doi: 10.1152/ajplung.00274.2001. [DOI] [PubMed] [Google Scholar]
- 16.Kramer BW, Moss TJ, Willet KE, Newnham JP, Sly PD, Kallapur SG, Ikegami M, Jobe AH. Dose and time response after intraamniotic endotoxin in preterm lambs. Am.J Respir.Crit Care Med. 2001;164:982–988. doi: 10.1164/ajrccm.164.6.2103061. [DOI] [PubMed] [Google Scholar]
- 17.Bachurski CJ, Ross GF, Ikegami M, Kramer BW, Jobe AH. Intra-amniotic endotoxin increases pulmonary surfactant proteins and induces SP-B processing in fetal sheep. Am.J Physiol Lung Cell Mol.Physiol. 2001;280:L279–L285. doi: 10.1152/ajplung.2001.280.2.L279. [DOI] [PubMed] [Google Scholar]
- 18.Jobe AH, Newnham JP, Willet KE, Moss TJ, Gore EM, Padbury JF, Sly P, Ikegami M. Endotoxin-induced lung maturation in preterm lambs is not mediated by cortisol. Am.J Respir.Crit Care Med. 2000;162:1656–1661. doi: 10.1164/ajrccm.162.5.2003044. [DOI] [PubMed] [Google Scholar]
- 19.Bry K, Lappalainen U, Hallman M. Intraamniotic interleukin-1 accelerates surfactant protein synthesis in fetal rabbits and improves lung stability after premature birth. J Clin.Invest. 1997;99:2992–2999. doi: 10.1172/JCI119494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prince LS, Okoh VO, Moninger TO, Matalon S. Lipopolysaccharide increases alveolar type II cell number in fetal mouse lungs through Toll-like receptor 4 and NF-kappaB. Am.J Physiol Lung Cell Mol.Physiol. 2004;287:L999–1006. doi: 10.1152/ajplung.00111.2004. [DOI] [PubMed] [Google Scholar]
- 21.Moss TJ, Newnham JP, Willett KE, Kramer BW, Jobe AH, Ikegami M. Early gestational intra-amniotic endotoxin: lung function, surfactant, and morphometry. Am.J Respir.Crit Care Med. 2002;165:805–811. doi: 10.1164/ajrccm.165.6.2108053. [DOI] [PubMed] [Google Scholar]
- 22.Newnham JP, Moss TJ, Kramer BW, Nitsos I, Ikegami M, Jobe AH. The fetal maturational and inflammatory responses to different routes of endotoxin infusion in sheep. Am.J Obstet.Gynecol. 2002;186:1062–1068. doi: 10.1067/mob.2002.122293. [DOI] [PubMed] [Google Scholar]
- 23.Mulrooney N, Jobe AH, Ikegami M. Lung inflammatory responses to intratracheal interleukin-1alpha in ventilated preterm lambs. Pediatr.Res. 2004;55:682–687. doi: 10.1203/01.PDR.0000112104.48903.3C. [DOI] [PubMed] [Google Scholar]
- 24.Ballard PL, Ning Y, Polk D, Ikegami M, Jobe AH. Glucocorticoid regulation of surfactant components in immature lambs. Am.J Physiol. 1997;273:L1048–L1057. doi: 10.1152/ajplung.1997.273.5.L1048. [DOI] [PubMed] [Google Scholar]
- 25.Newnham JP, Kallapur SG, Kramer BW, Moss TJ, Nitsos I, Ikegami M, Jobe AH. Betamethasone effects on chorioamnionitis induced by intra-amniotic endotoxin in sheep. Am.J Obstet.Gynecol. 2003;189:1458–1466. doi: 10.1067/s0002-9378(03)00758-0. [DOI] [PubMed] [Google Scholar]
- 26.Moss TJ, Mulrooney NP, Nitsos I, Ikegami M, Jobe AH, Newnham JP. Intra-amniotic corticosteroids for preterm lung maturation in sheep. Am.J Obstet.Gynecol. 2003;189:1389–1395. doi: 10.1067/s0002-9378(03)00622-7. [DOI] [PubMed] [Google Scholar]
- 27.Bolt RJ, van Weissenbruch MM, Lafeber HN, Delemarre-van de Waal HA. Glucocorticoids and lung development in the fetus and preterm infant. Pediatr.Pulmonol. 2001;32:76–91. doi: 10.1002/ppul.1092. [DOI] [PubMed] [Google Scholar]
- 28.Liley HG, White RT, Warr RG, Benson BJ, Hawgood S, Ballard PL. Regulation of messenger RNAs for the hydrophobic surfactant proteins in human lung. J Clin.Invest. 1989;83:1191–1197. doi: 10.1172/JCI114000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iannuzzi DM, Ertsey R, Ballard PL. Biphasic glucocorticoid regulation of pulmonary SP-A: characterization of inhibitory process. Am.J Physiol. 1993;264:L236–L244. doi: 10.1152/ajplung.1993.264.3.L236. [DOI] [PubMed] [Google Scholar]
- 30.Dulkerian SJ, Gonzales LW, Ning Y, Ballard PL. Regulation of surfactant protein D in human fetal lung. Am.J Respir.Cell Mol.Biol. 1996;15:781–786. doi: 10.1165/ajrcmb.15.6.8969273. [DOI] [PubMed] [Google Scholar]
- 31.Ballard PL, Ertsey R, Gonzales LW, Gonzales J. Transcriptional regulation of human pulmonary surfactant proteins SP-B and SP-C by glucocorticoids. Am.J Respir.Cell Mol.Biol. 1996;14:599–607. doi: 10.1165/ajrcmb.14.6.8652188. [DOI] [PubMed] [Google Scholar]
- 32.Esplin MS, Romero R, Chaiworapongsa T, Kim YM, Edwin S, Gomez R, Mazor M, Adashi EY. Monocyte chemotactic protein-1 is increased in the amniotic fluid of women who deliver preterm in the presence or absence of intra-amniotic infection. J Matern.Fetal Neonatal Med. 2005;17:365–373. doi: 10.1080/14767050500141329. [DOI] [PubMed] [Google Scholar]
- 33.Espinoza J, Chaiworapongsa T, Romero R, Edwin S, Rathnasabapathy C, Gomez R, Bujold E, Camacho N, Kim YM, Hassan S, et al. Antimicrobial peptides in amniotic fluid: defensins, calprotectin and bacterial/permeability-increasing protein in patients with microbial invasion of the amniotic cavity, intra-amniotic inflammation, preterm labor and premature rupture of membranes. J Matern.Fetal Neonatal Med. 2003;13:2–21. doi: 10.1080/jmf.13.1.2.21. [DOI] [PubMed] [Google Scholar]
- 34.Chaiworapongsa T, Romero R, Espinoza J, Kim YM, Edwin S, Bujold E, Gomez R, Kuivaniemi H. Macrophage migration inhibitory factor in patients with preterm parturition and microbial invasion of the amniotic cavity. J Matern.Fetal Neonatal Med. 2005;18:405–416. doi: 10.1080/14767050500361703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pryhuber GS, Hull WM, Fink I, McMahan MJ, Whitsett JA. Ontogeny of surfactant proteins A and B in human amniotic fluid as indices of fetal lung maturity. Pediatr.Res. 1991;30:597–605. doi: 10.1203/00006450-199112000-00023. [DOI] [PubMed] [Google Scholar]
- 36.LeVine AM, Whitsett JA, Hartshorn KL, Crouch EC, Korfhagen TR. Surfactant protein D enhances clearance of influenza A virus from the lung in vivo. J Immunol. 2001;167:5868–5873. doi: 10.4049/jimmunol.167.10.5868. [DOI] [PubMed] [Google Scholar]
- 37.Kingma PS, Whitsett JA. In defense of the lung: surfactant protein A and surfactant protein D. Curr.Opin.Pharmacol. 2006;6:277–283. doi: 10.1016/j.coph.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 38.Romero R, Mazor M, Brandt F, Sepulveda W, Avila C, Cotton DB, Dinarello CA. Interleukin-1 alpha and interleukin-1 beta in preterm and term human parturition. Am.J Reprod.Immunol. 1992;27:117–123. doi: 10.1111/j.1600-0897.1992.tb00737.x. [DOI] [PubMed] [Google Scholar]
- 39.Romero R, Manogue KR, Mitchell MD, Wu YK, Oyarzun E, Hobbins JC, Cerami A. Infection and labor. IV. Cachectin-tumor necrosis factor in the amniotic fluid of women with intraamniotic infection and preterm labor. Am.J Obstet.Gynecol. 1989;161:336–341. doi: 10.1016/0002-9378(89)90515-2. [DOI] [PubMed] [Google Scholar]
- 40.Wispe JR, Clark JC, Warner BB, Fajardo D, Hull WE, Holtzman RB, Whitsett JA. Tumor necrosis factor-alpha inhibits expression of pulmonary surfactant protein. J Clin.Invest. 1990;86:1954–1960. doi: 10.1172/JCI114929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Awasthi S, Coalson JJ, Crouch E, Yang F, King RJ. Surfactant proteins A and D in premature baboons with chronic lung injury (Bronchopulmonary dysplasia). Evidence for an inhibition of secretion. Am.J Respir.Crit Care Med. 1999;160:942–949. doi: 10.1164/ajrccm.160.3.9806061. [DOI] [PubMed] [Google Scholar]
- 42.Seidner SR, Jobe AH, Coalson JJ, Ikegami M. Abnormal surfactant metabolism and function in preterm ventilated baboons. Am.J Respir.Crit Care Med. 1998;158:1982–1989. doi: 10.1164/ajrccm.158.6.9804128. [DOI] [PubMed] [Google Scholar]
- 43.Kramer BW, Kramer S, Ikegami M, Jobe AH. Injury, inflammation, and remodeling in fetal sheep lung after intra-amniotic endotoxin. Am.J Physiol Lung Cell Mol.Physiol. 2002;283:L452–L459. doi: 10.1152/ajplung.00407.2001. [DOI] [PubMed] [Google Scholar]
- 44.Kallapur SG, Nitsos I, Moss TJ, Kramer BW, Newnham JP, Ikegami M, Jobe AH. Chronic endotoxin exposure does not cause sustained structural abnormalities in the fetal sheep lungs. Am.J Physiol Lung Cell Mol.Physiol. 2005;288:L966–L974. doi: 10.1152/ajplung.00389.2004. [DOI] [PubMed] [Google Scholar]
- 45.Moss TJ, Nitsos I, Kramer BW, Ikegami M, Newnham JP, Jobe AH. Intra-amniotic endotoxin induces lung maturation by direct effects on the developing respiratory tract in preterm sheep. Am.J Obstet.Gynecol. 2002;187:1059–1065. doi: 10.1067/mob.2002.126296. [DOI] [PubMed] [Google Scholar]
- 46.Miyamura K, Malhotra R, Hoppe HJ, Reid KB, Phizackerley PJ, Macpherson P, Lopez BA. Surfactant proteins A (SP-A) and D (SP-D): levels in human amniotic fluid and localization in the fetal membranes. Biochim.Biophys.Acta. 1994;1210:303–307. doi: 10.1016/0005-2760(94)90233-x. [DOI] [PubMed] [Google Scholar]
- 47.King RJ, Ruch J, Gikas EG, Platzker AC, Creasy RK. Appearance of paoproteins of pulmonary surfactant in human amniotic fluid. J Appl.Physiol. 1975;39:735–741. doi: 10.1152/jappl.1975.39.5.735. [DOI] [PubMed] [Google Scholar]
- 48.Shelley SA, Balis JU, Paciga JE, Knuppel RA, Ruffolo EH, Bouis PJ., Jr Surfactant “apoproteins” in human amniotic fluid: an enzyme-linked immunosorbent assay for the prenatal assessment of lung maturity. Am.J Obstet.Gynecol. 1982;144:224–228. doi: 10.1016/0002-9378(82)90632-9. [DOI] [PubMed] [Google Scholar]
- 49.Dilger I, Schwedler G, Dudenhausen JW. Determination of the pulmonary surfactant-associated protein SP-B in amniotic fluid with a competition ELISA. Gynecol Obstet.Invest. 1994;38:24–27. doi: 10.1159/000292439. [DOI] [PubMed] [Google Scholar]
- 50.Vayrynen O, Glumoff V, Hallman M. Inflammatory and anti-inflammatory responsiveness of surfactant proteins in fetal and neonatal rabbit lung. Pediatr.Res. 2004;55:55–60. doi: 10.1203/01.PDR.0000100462.41671.C6. [DOI] [PubMed] [Google Scholar]