Abstract
Caesarean section rates have risen in recent years, sparking renewed debate about the circumstances under which such deliveries are being, and should be, performed. Some commentators suggest that increasing rates may, in part, be explained by women in higher-income brackets requesting elective caesareans (the so-called “too posh to push” hypothesis). After adjusting for maternal age, Canadian data do not support this theory. In fact, age-adjusted caesarean section rates were significantly lower in Canada’s highest-income neighbourhoods than in the lowest-income areas in 2002–03.
Rising caesarean section rates have helped rekindle the debate over when and under what circumstances caesarean section births should be performed, both in Canada and elsewhere. In some circumstances, caesarean sections are clearly essential, life-saving operations, and some studies have suggested potential long-term benefits for scheduled caesarean sections for certain groups of women (Dodd et al. 2004).
However, like other surgical procedures, caesarean sections are not risk-free. The associated risks include increased chances of haemorrhage, longer recovery from childbirth and increased odds of severe pain and infection (House of Commons Health Committee 2003; Hannah 2004; Jackson and Paterson-Brown 2001).
In the long term, studies have shown that women who have had a caesarean delivery are at increased risk for certain reproductive problems (e.g., ectopic pregnancies), serious problems pertaining to the placenta (e.g., placenta accreta and placenta previa) or uterine rupture (Minkoff and Chervenak 2003). Babies born by caesarean section may also be at increased risk. For example, respiratory problems following birth (Minkoff and Chervenak 2003; House of Commons Health Committee 2003) and difficulties initiating breastfeeding (DiGirolamo et al. 2001; Bond and Holloway 1992) have been highlighted as concerns for infants born by caesarean section. Given these and other risks, the Society for Obstetricians and Gynaecologists of Canada (2004) recently stated that caesarean sections should be performed only when medically indicated.
In spite of this guidance and similar guidelines from some other countries (National Collaborating Centre for Women’s and Children’s Health 2004), it has been suggested that a driver of rising caesarean section rates is the so-called “too posh to push” phenomenon in which women, particularly wealthier women, request surgery even though they do not have recognized medical indications for the procedure (Song 2004). A few high-profile cases and statistics showing higher caesarean section rates in private hospitals in Australia, Brazil and other countries have fuelled the debate (Roberts et al. 2000; Potter et al. 2001; Béhague et al. 2002). Researchers in the United Kingdom, however, have recently rejected this argument based on an analysis of National Health Service hospital data. They found that women in the lowest-income group were less likely to have elective caesarean sections, but there was no significant difference between women in the four other income quintiles (Barley et al. 2004).
To determine whether Canadian caesarean section rates are related to socio-economic status, we investigated whether women in high-income urban neighbourhoods are more likely to have surgical deliveries than other women.
Study Design and Methods
Data source and study population
Women who gave birth in Canadian hospitals between April 1, 2002 and March 31, 2003 were identified using the Hospital Morbidity Database of the Canadian Institute for Health Information. Using an approach developed by Statistics Canada that assigns neighbourhoods to five equally sized quintiles based on income data reported on the 2001 Census, we derived patients’ socio-economic status based on their residential postal codes (Wilkins 2004). Women who gave birth in the territories and Quebec, as well as those with invalid residential postal codes, were excluded, as socio-economic characteristics could not be reliably assigned on the basis of available data, using this approach.
Data analysis
Caesarean section rates were calculated for each neighbourhood income quintile. Given that maternal age has a strong independent relationship to the odds of having a caesarean section and that higher-income mothers tend to be older, age-standardized rates were also calculated for each quintile. The standard population used in this calculation was all Canadian residents who gave birth in Canadian hospitals between April 1, 2002 and March 31, 2003.
Separate analyses were performed for all deliveries and for deliveries by patients residing in urban areas only. Using data for urban areas only minimizes potential socio-economic misclassification (Willkins 2004), and as such we focus on these results in this paper.
Results
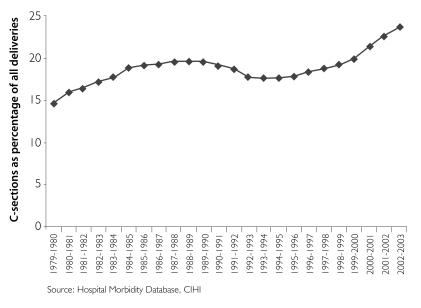
Currently, more than one in five births in Canada are delivered by caesarean section. Rates vary across the country (from 15% to 33% by health region in 2002–03), but the national rate has been rising since the mid-1990s (Canadian Institute for Health Information 2005). As Figure 1 shows, Canada’s caesarean section rate grew by six percentage points (from 17.7% to 23.7%) between 1992–93 and 2002–03. Increases in the rate of primary caesarean sections and a decline in the rate at which women deliver vaginally following previous caesarean section births both contributed to this trend (Canadian Institute for Health Information 2004).
FIGURE 1.
Trend in Canadian caesarean section rates, 1979–80 to 2002–03
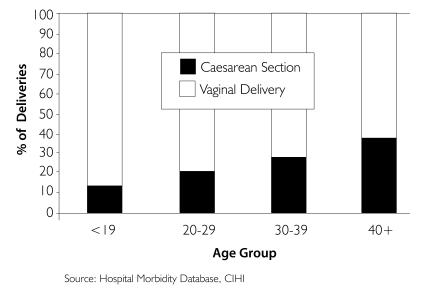
As in other countries, caesarean section rates are higher for older mothers. Urban mothers younger than 19 years of age had a 14% caesarean section rate in 2002–03; the rate for those 40 years of age or older was 38% (see Figure 2). Younger mothers were also more likely to live in low-income neighbourhoods. Two in five of those younger than 19 years (41%) lived in areas ranked in the bottom fifth of the income distribution. The rate for older mothers was much less – only 19% of new mothers 40 years or age or older lived in the lowest-income neighbourhoods.
FIGURE 2.
Mode of delivery in urban areas by maternal age, 2002–03
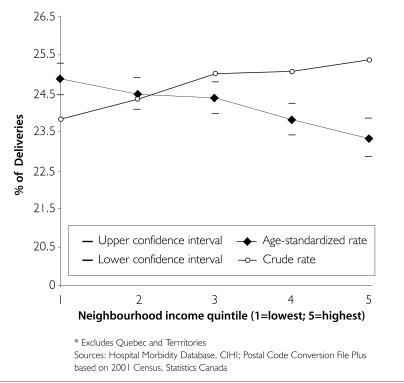
This finding emphasizes the importance of taking age profiles into account in analyses of the relationship between socio-economic status and caesarean section rates. In fact, women in the lowest-income urban neighbourhoods had lower crude caesarean section rates in 2002–03 (see Figure 3). However, when adjusted for age, this relationship reversed. Based on this analysis, women living in the lowest-income areas were significantly more likely to have caesarean deliveries (24.9% rate for areas in the lowest-income quintile) than those in the most prosperous areas (23.3% rate in the highest-income quintile neighbourhoods) (p<0.05). A similar trend was found when rural areas were included in the analysis.
FIGURE 3.
Crude and age-adjusted caesarean section rates in urban areas by neighbourhood income quintile, 2002–03
Conclusion
While Canadian data do not distinguish between elective and medically indicated delivery procedures, analysis of Canadian hospital data for 2002–03 does not support widespread “too posh to push” concerns. After adjusting for maternal age, women in Canada’s highest-income urban neighbourhoods are significantly less likely to have caesarean sections than those in the lowest-income areas.
Contributor Information
Kira Leeb, Manager, Health Services Research, Canadian Institute of Health Information.
Akerke Baibergenova, Senior Analyst, Health Services Research, Canadian Institute of Health Information.
Eugene Wen, Senior Methodologist, Research and Indicator Development, Canadian Institute of Health Information.
Greg Webster, Director, Research and Indicator Development, Canadian Institute of Health Information.
Jennifer Zelmer, Vice-President, Research and Analysis, Canadian Institute of Health Information.
References
- Barley K., Aylin P., Bottle A., Jarman B. Social Class and Elective Caesareans in the English NHS. British Medical Journal . 2004;328(7453):1399. doi: 10.1136/bmj.328.7453.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Béhague D.P., Victoria C., Barros F. Consumer Demand for Caesarean Sections in Brazil: Informed Decision Making, Patient Choice, or Social Inequality? A Population Based Birth Cohort Study Linking Ethnographic and Epidemiological Methods. British Medical Journal . 2002;324(7343):942–45. doi: 10.1136/bmj.324.7343.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond G.M., Holloway M. Anaesthesia and Breast-Feeding – The Effect on Mother and Infant. Anaesthesia and Intensive Care . 1992;20(4):426–30. doi: 10.1177/0310057X9202000404. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information. Giving Birth in Canada: A Regional Profile . Ottawa: Author; 2004. [Google Scholar]
- Canadian Institute for Health Information. Health Indicators, 2005. Ottawa: Author; 2005. [Google Scholar]
- DiGirolamo A.M., Grummer-Strawn L., Fein S. Maternity Care Practices: Implications for Breastfeeding. Birth . 2001;28(2):94–100. doi: 10.1046/j.1523-536x.2001.00094.x. [DOI] [PubMed] [Google Scholar]
- Dodd J.M., Crowther C., Huertas E., Guise J., Horey D. Planned Elective Repeat Caesarean Section versus Planned Vaginal Birth for Women with a Previous Caesarean Birth. Cochrane Database of Systematic Reviews . 2004;18(4):CD004224. doi: 10.1002/14651858.CD004224.pub2. [DOI] [PubMed] [Google Scholar]
- Hannah M.E. Planned Elective Caesarean Section: A Reasonable Choice for Some Women? Canadian Medical Association Journal . 2004;170(5):813–14. doi: 10.1503/cmaj.1032002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House of Commons Health Committee. Provision of Maternity Services: Fourth Report of Session 2002–03, Volume 1 . London, UK: The Stationary Office Limited; 2003. [Google Scholar]
- Jackson N., Paterson-Brown S. Physical Sequelae of Caesarean Section. Clinical Obstetrics and Gynecology . 2001;15(1):49–61. doi: 10.1053/beog.2000.0148. [DOI] [PubMed] [Google Scholar]
- Minkoff H., Chervenak F. Elective Primary Caesarean Delivery. New England Journal of Medicine . 2003;348(10):946–50. doi: 10.1056/NEJMsb022734. [DOI] [PubMed] [Google Scholar]
- National Collaborating Centre for Women’s and Children’s Health, National Institute for Clinical Excellence. Caesarean Section. London: RCOG Press; 2004. Retrieved August 4, 2005. http://www.nice.org.uk/pdf/CG013fullguideline.pdf . [DOI] [PubMed] [Google Scholar]
- Potter J.E., Berquo E., Perpetuo I., Leal O., Hopkins K., Souza M., Formiga M. Unwanted Caesarean Sections among Public and Private Patients in Brazil: Prospective Study. British Medical Journal . 2001;323(7322):1155–58. doi: 10.1136/bmj.323.7322.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts C.L., Tracy S., Peat B. Rates for Obstetric Intervention among Private and Public Patients in Australia: Population Based Descriptive Study. British Medical Journal . 2000;321(7254):137–41. doi: 10.1136/bmj.321.7254.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Society of Obstetricians and Gynaecologists of Canada. C-Sections on Demand – SOGC’s Position. 2004 Retrieved August 4, 2005. http://www.sogc.org/sogcnet/sogc_docs/press/releases2004/pdfs/ElectiveCaesareansPart%20II.pdf .
- Song S. Too Posh to Push? As More Pregnant Women Schedule C-Sections, Doctors Warn That the Procedure Is Not Risk Free. Time. 2004 Apr 19; Retrieved August 4, 2005. http://www.time.com/time/archive/preview/0,10987,1101040419-610086,00.html .
- Wilkins R. Automated Geographic Coding Based on the Statistics Canada Postal Code Conversion Files, Including Postal Codes to December 2003. Catalogue no. 82F0086-XDB. Ottawa: Health Analysis and Measurement Group, Statistics Canada; 2004. PCCF+ Version 4D User’s Guide (Geocodes/PCCF) [Google Scholar]