Abstract
The aim of this in-depth, longitudinal, qualitative case study was to understand and explain the dynamics of implementing a pilot project to deliver integrated healthcare for type 2 diabetic patients. Data gathering included in-depth, face-to-face interviews with family physicians, nurses and other healthcare providers, managers and policy makers (n = 25) at various points during the research period, and focus groups (n = 3) with patients. These data were complemented by onsite observations of numerous committee meetings, and analysis of project documentation. Benson’s (1975) political economy perspective provided a valuable conceptual framework for tracking the complex dynamics of implementing service integration. Manipulative strategies (continuing medical education, new information technology) did not engage physicians. Of the cooperative strategies attempted (disease management, patient education, community mobilization), only patient education appears to have succeeded: patients acknowledged that project educational activities enabled them to improve self-management of their disease. However, the project’s emphasis on patient education effectively increased nurses’ bargaining power within the healthcare team, to the detriment of the focus on integrated care. Integrating care is a laborious process that takes time to reach fruition. This one-year pilot project was insufficient for mobilizing health professionals away from fragmented practices toward integrated ones. New resources mostly allowed them to maintain or increase their power positions within the network of care providers. Nevertheless, this initiative raised physicians’ awareness and appreciation of the care that other health professionals provided to their patients.
Abstract
La présente étude de cas longitudinale et qualitative visait à comprendre et à expliquer la dynamique nécessaire à la mise en oeuvre d’un projet pilote en matière de prestation de soins de santé aux personnes souffrant de diabète de type 2. Les données ont été recueillies, entre autres, auprès de médecins de famille, de personnel infirmier et autres prestataires de soins, gestionnaires et responsables des politiques dans le domaine des soins de santé (n = 25) qui ont été interviewés en personne à différents moments au cours de la période d’étude, et auprès de patients à l’occasion de groupes de discussions (n = 3). Des observations faites sur place par les participants et responsables et une analyse de la documentation du projet ont permis de complémenter ces données. Le concept d’économie politique de Benson (1975) a permis de disposer d’un cadre conceptuel précieux pour suivre la dynamique complexe de l’intégration des services. Les stratégies de manipulation (formation médicale permanente, nouvelle technologie de l’information) n’ont pas attiré les médecins. Parmi les stratégies de coopération mises en oeuvre (gestion thérapeutique, éducation des patients, mobilisation de la communauté), seule l’éducation des patients semble avoir été un succès : les patients ont reconnu en effet que les activités visant à les informer sur leur maladie leur avaient permis de mieux gérer eux-mêmes cette maladie. Cependant, l’accent mis par le projet sur l’éducation des patients a augmenté en réalité le pouvoir de négociation du personnel infirmier au sein de l’équipe soignante au détriment de l’attention à porter sur les soins intégrés. L’intégration des soins est un processus laborieux qui ne porte pas ses fruits du jour au lendemain. Le projet pilote, qui a duré un an, n’a pas réussi à détourner les professionnels de la santé de pratiques fragmentées vers des pratiques intégrées. Les nouvelles ressources leur ont principalement permis de conserver ou d’augmenter leur autorité au sein du réseau des prestataires de soins. Ce projet a quand même permis aux médecins de prendre conscience des soins offerts par d’autres professionnels de la santé à leurs patients et d’en apprécier la valeur.
This evaluation was conducted with the aim of exploring implementation of a new model of integrated care delivery for patients with type 2 diabetes in the Côte-des-Neiges area, Montreal, Quebec, Canada. Diabetes mellitus has become an important public health problem owing to the disease’s high prevalence, its short- and long-term morbidity effects, its complex management and the considerable health expenditures, for both patients and society, entailed in its treatment (Greenlink 1992; Harris 1993; Wagner 1995; Meltzer et al. 1998; Rosnick 1998; Weiss 1998; Gerber and Stewart 1998; McKinlay and Marceau 2000; O’Brien et al. 2003; Jiang et al. 2003; Safran et al. 2003; Centers for Disease Control and Prevention, Primary Prevention Working Group 2004). Among the different types of diabetes, type 2 is the most prevalent, accounting for about 90% of diagnosed diabetes cases (American Diabetes Association 1998).
It has been noted that the more healthcare for diabetic patients is provided by a multidisciplinary cooperative and coordinated clinical team, the higher the chances of adequate control of the disease (Hiss 1996; Meltzer et al. 1998; American Diabetic Association 1998; Bayless and Martin 1998; Larsen et al. 2003). However, healthcare systems in Western countries have typically been developed around acute health problems (Wagner et al. 1996; Etzweiler 1997), an evolution that has led to autonomous clinical practices, organizational independence and fragmentation of care delivery. The complexity and rising prevalence of chronic diseases such as diabetes are among the factors that call into question the traditional lack of collaboration among healthcare providers and organizations (Contandriopoulos 2000). Chronic disease treatment challenges, such as those posed by diabetes, foster the collaborative trend that, since the early 1990s, has swept the healthcare industry in North America under the label “integrated delivery systems” (Shortell et al. 1996; Leatt et al. 2000).
The sponsors of the Côte-des-Neiges pilot project1 established their initiative with a twofold purpose: (1) to understand and explain the emergence of integrative processes of healthcare delivery to chronic patients in a traditionally fragmented healthcare system and (2) to generate evidence about the added value for individuals and the healthcare system of providing integrated care for diabetic patients. This paper focuses particularly on the first of these aims.
The remainder of the paper is structured as follows. First, we briefly describe the Quebec healthcare delivery system and the integrated model of care elaborated by the Côte-des-Neiges sponsors. Next, we present the key conceptual elements that underpin the implementation analysis, based on Benson’s (1975) view of the interorganizational network as a political economy. Then, we describe the research methods used for the implementation evaluation. Next, we present the findings from our investigation. The paper ends with an interpretation and explanation of these findings and a discussion of their implications.
The Quebec Healthcare Delivery System
Healthcare systems have experienced profound upheavals over the last two decades. Despite their differences in funding, organization and management, all have been affected by budgetary constraints, older populations and technological innovation. These trends hold true for the Canadian and Quebec healthcare systems (National Forum on Health 1997). Given the challenges of maintaining quality of care while improving cost control, numerous studies have recommended the reinforcement of primary care across the country.2
The Quebec healthcare system, which is publicly funded, is organized across 18 health regions. In all these regions, particularly in urban areas, primary medical care is practised in a variety of settings, which include primary care facilities, emergency rooms, ambulatory hospital clinics and long-term-care institutions. Most physicians have a mixed practice profile, and work in more than one milieu (Demers and Brunelle 2000). That said, primary care is mainly delivered in two kinds of facilities: local community health centres (CLSCs) and medical clinics. Twenty-two percent of physicians work in CLSCs, mostly on a salary basis (Demers and Brunelle 2000). Hence, family physicians working in fee-for-service private practices provide the bulk of primary medical care.
This dual/parallel primary care network has contributed to the fragmentation of healthcare delivery. Fragmentation has been intensified by the historically difficult relationship between the CLSCs and private medical clinics (Lemieux and Labrie 1979; Commission of Study on Health Services and Social Services of Quebec 2000).
The Côte-des-Neiges community health centre is one of 29 such facilities on Montreal Island. It is located in a densely populated multiethnic area – more than 130,000 inhabitants from 127 different ethnic groups – with significant inequality in socioeconomic status. Besides the community health centre, the healthcare network in the Côte-des-Neiges area comprises 12 medical clinics, more than 50 solo practitioners’ clinics, three acute care hospitals and one public long-term-care facility. All these organizations have been delivering care in silo fashion, with negative consequences particularly for such clients as the elderly and patients with chronic diseases (Bergman et al. 1997).
The Côte-des-Neiges Integrated Model of Healthcare Delivery for Type 2 Diabetic Patients
In 1997, the sponsors of the Côte-des-Neiges project began a process of reflection on integrated medical services. Their working sessions over the next year were held against a backdrop of informal exchanges, informative seminars and nominal groups with physicians from the community health centre and private clinics in the area (Nasmith et al. 2001). These meetings resulted in the identification of type 2 diabetes as the health problem most likely to engage healthcare providers in implementing integrated service delivery. In 1999, the sponsors established an inventory of all health resources in the area, wrote a literature review on the topic of integrated care and diabetes and successfully applied for financial support from the Canadian Health Transition Fund.
Working groups were established to address three main themes on integrated care for diabetics: patient education, family physician practices and communication among healthcare providers. The deliberations of these groups informed construction of the model of healthcare delivery to be implemented, as well as the strategies of change to be adopted in fostering integration.
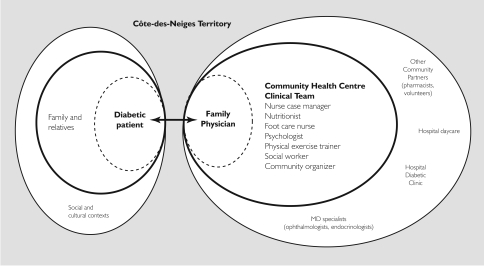
The model of healthcare delivery finally adopted (Figure 1) was based on the assumption that diabetic patients’ clinical responsibility had to be shared by a multidisciplinary team composed of the family physician (in the facility where he or she delivers care), a clinical team located at the community health centre (nurse case manager, nutritionist, foot care nurse, psychologist, physical exercise trainer, social worker and community organizer3) and the patients themselves.
FIGURE 1.
Côte-des-Neiges integrated healthcare delivery for type 2 diabetic patients
To promote clinical integration, five different levers of change were employed:
adoption of a disease management approach for patient follow-up (González and Crane 1995; Sylvestry and Marro 1996; Ellrodt et al. 1997);
development of patient educational activities inspired by the Prochaska model (Prochaska and DiClemente 1982; Prochaska 1994) to promote patient empowerment (Greenfield et al. 1988; D’Eramo-Melkus et al. 1992; Redhead et al. 1993; Anderson et al. 1995; Day et al. 1997);
organization of continuing medical education (CME) activities on diabetes to increase family physicians’ clinical expertise (Greenlink 1992; Borgiel et al. 1999);
adoption of a computerized clinical information system that links healthcare providers beyond organizational boundaries to facilitate transmission of patients’ clinical information and improve effectiveness and cost containment (Leape et al. 1995; Pestotnik et al. 1996; Bates et al. 1998; Hunt et al. 1998);
mobilization of community resources beyond the healthcare system to involve the Côte-des-Neiges community at large in improving its diabetic patients’ quality of life (Baker et al. 1994; Glasgow et al. 1999) and simultaneously reinforce community social capital.4
Together, these interventions constituted the Côte-des-Neiges project. To determine their impact on the dynamics of healthcare integration, we decided to adopt Benson’s (1975) political economy perspective as a conceptual framework.
Theoretical Background
In 1975, J. Kenneth Benson developed a theoretical scheme of the interorganizational network as a political economy. For Benson, an interorganizational network was an “emergent entity” compounded by a number of “distinguishable organizations” that interact over time. These interactions may take place at two different levels: (1) service delivery and (2) resource acquisition. Building on the resource-dependence approach (Yutchtman and Seashore 1967), Benson argued that the interactive pattern of service delivery is ultimately conditioned by interactions at the level of resource acquisition.
Benson’s political economy of interorganizational networks requires two essential and interrelated resources: money and authority. Money is necessary for the adequate supply of resources, and authority is crucial for legitimating decision-making and actions. These economic and political forces would underpin the “superstructure” of sentiments and cooperative interactions among the members of the network.
According to Benson (1975: 235), an interorganizational network achieves equilibrium “to the extent that participant organizations are engaged in highly coordinated, cooperative interactions based on normative consensus and mutual respect.” The four essential dimensions of this equilibrium are domains, ideologies, positive reciprocal evaluations and work coordination.
Interorganizational networks do not emerge in a vacuum; they are intimately linked to the environment within which the actors negotiate their interactions. In other words, in order for agents to work together, they must be surrounded by the symbolic and material conditions that favour collaboration. Those aspects of the social context that most significantly affect the political and economic forces of the network are, according to Benson, (1) the supply of money and authority and (2) the distribution of power within the network.
Benson also suggests that change in the dynamics of the interorganizational network may be driven by a variety of strategies. He notes four in particular: (1) cooperative strategies, which involve agreements and joint planning; (2) disruptive strategies, by which change is generated through activities that threaten an organization’s capacity to acquire resources; (3) manipulative strategies, by which the environmental constraints that affect resource acquisition are purposively altered; and (4) authoritative strategies, by which interorganizational relationships are mandated by a legitimated administrative or legislative governance structure.
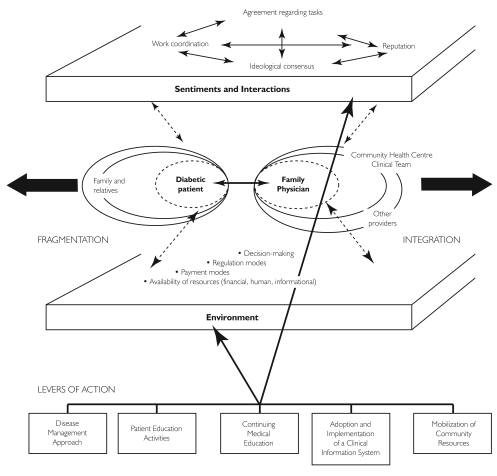
In summary, based on Benson’s conceptualization, healthcare provider clinical practices and patient behaviour (i.e., the level of service delivery) are influenced by two sets of forces: the superstructure of sentiments and interactions and the healthcare system’s environment. In our case, and thanks to the supply of new money from its sponsors (i.e., the level of resource acquisition), the Côte-des-Neiges project was viewed as a valuable opportunity for acting on those two levels. Through implementation of a number of cooperative and manipulative strategies aimed at triggering change, the project promoted the transformation of clinical practice for type 2 diabetic patients from a fragmented to an integrated model (Figure 2).
FIGURE 2.
Network dynamics in the Côte-des-Neiges integrated model of care for patients with type 2 diabetes (adapted from Benson 1975)
Methodology
Research strategy and design
In this evaluation, we adopted a qualitative case study strategy. As Patton (2002: 162) notes: “If a process of ongoing adaptation to local conditions characterizes program implementation, then the methods used to study implementation should correspondingly be open-ended, discovery oriented and capable of describing developmental processes and program changes. Qualitative methods are ideally suited to the task of describing such program implementation.”
Because of its considerable size and the richness and variety of its health and community resources, the Côte-des-Neiges area offered an exceptional context for experimentation with new forms of organizing. Because longitudinal research appears crucial for attaining a rich understanding of organizational change (Pettigrew 1990; Orlikowski 1996; Armenakis and Bedeian 1999), we conducted an in-depth, longitudinal, qualitative case study, the case being the implementation of integrated health services delivery for type 2 diabetic patients.
Data gathering and analysis
The pilot project – and thus data gathering – was carried out over 31 months, from June 1998 to December 2000. The main method for collecting data was qualitative interviewing (Rubin and Rubin 1995). Face-to-face, one-to-one, semi-structured interviews were carried out mostly over the last six months of the intervention. Owing to the number and variety of actors involved in the project, the selection of individuals to be interviewed (Table 1) had to be undertaken with care. A list of participants other than patients was drawn up, and 36 were selected according to their estimated capacity to provide information useful to the project’s development. In the case of physicians, steps were taken to ensure representation of all clinical settings involved in the initiative. These individuals were invited for a voluntary interview, to which 25 agreed. Interviews were tape-recorded and lasted an average of 45 minutes.
TABLE 1.
Côte-des-Neiges project: participant sample composition
| PROJECT STAKEHOLDERS | n | INITIAL n | FINAL n |
|---|---|---|---|
| Type 2 diabetic patients | 325 | 34 | 16 |
| Family physicians | 44 | 12 | 12 |
| Community centre | 5 | 2 | 2 |
| Polyclinic | 37 | 8 | 8 |
| Solo | 2 | 2 | 2 |
| Providers at community centre | 8 | 8 | 5 |
| Providers from specialized services | 4 | 4 | 1 |
| Managers | 11 | 4 | 2 |
| Advisory committee | 20 | 3 | 1 |
| Steering committee | 7 | 5 | 4 |
| TOTAL | 419 | 70 | 41 |
A second method of data collection was the focus group (Krueger and Casey 2000). Our intention was to engage patients in in-depth discussions about their opinions and experiences related to the project. To be eligible, patients had to have received more than one service from the clinical team at the community health centre, and they had to speak French or English. Again, an effort was made to ensure that all clinical settings were represented. Of 34 diabetic patients invited to participate in the focus groups, 16 agreed. Three group sessions were held in the fall of 2000. Group discussions were also tape-recorded. Careful listening to the recordings helped identify the most important points for discussion in successive sessions.
On-site participant and non-participant observations over the 18-month research period complemented the interviews. Observations were recorded mainly in sponsors’ work sessions and meetings of the project Advisory and Steering committees. Finally, archival materials (proceedings and minutes, e-mails exchanged between family physicians and nurse case managers, and other project documents) and extensive diary research notes complete the list of methods used to generate empirical material over the 31-month period of inquiry.
Transcripts of semi-structured interviews and focus groups were subjected to sequential thematic analysis (Paillé 1996) guided by the dimensions of the theoretical framework and supported by the software package N-Vivo 2.0. In combination with observations, documentary analysis and field notes, this technique facilitated the elaboration of a detailed narrative of the intervention (Langley 1999). The preparation of tables was helpful for condensing information and identifying patterns of interaction (Miles and Huberman 1994; Langley 1999).
Results: Working for Integration – Implementing the Côte-des-Neiges Diabetes Project
The implementation phase of the Côte-des-Neiges project spanned January to December 2000. Forty-four physicians were recruited from 10 different medical practices representing the variety of practice settings in the area, and 345 patients received services according to their identified needs. The five different strategies for change included in the new model of care (disease management, patient education, continuing medical education, computerized clinical information system and community mobilization) were put in place at the beginning of the implementation phase.
Sub-process 1: Adopting a disease management approach
Our disease management approach for diabetic patients assumed that the central role in diagnosis and treatment would be played by the family physician. Nursing roles would be enhanced through new activities developed by two nurse case managers specifically hired for this project. After medical referral, the nurses provided patient education services and coordinated these services with those provided by other members of the clinical team at the community health centre.
Nurses were based at the community health centre, and e-mail was the preferred method of communication with physicians. In this way, the nurses aimed to keep physicians informed about the intervention plans adopted for their patients, the results of follow-ups and any operational difficulties concerning the implementation of integrated care.
Such organization of service delivery, however, failed to promote clinical integration; each professional continued to provide care in parallel. As one physician in solo practice observed:
I am looking at this project as a physician who is sitting in my office. My patients go away to this place and different things are happening there in this place. I’m given the general outline, my patients told me the general outline a little bit, but all of the little details, the logistics and all of those things that I’m not really involved in, my involvement is my own logistics with filling out the forms, encouraging the patients to go, following the patients medically. … It’s more clinical, so I don’t really have a tremendous amount to say about the logistics of what’s happening at the community health centre.
The lack of physician involvement was also noted by members of the clinical team:
There is the aspect of communication between physicians and the other providers via the computer. … In fact, what we have seen is that there are not many links between general practitioners and us. There are very few contacts. But they have access to all the services we provide. For myself, I have no contact with physicians.
As a result, the pilot project was perceived as an addition of new services for diabetic patients. In other words, the supply of new money did not promote integrated delivery as expected, but allowed the main professionals involved in disease management to maintain (in the case of physicians) or increase (in the case of nurses) their bargaining power within the multidisciplinary team. As a result, the network superstructure did not change; rather, new fragmented services for diabetic patients were provided.
Sub-process 2: Empowering diabetic patients
To promote behavioural changes in patients, encourage empowerment and ultimately foster self-care, the clinical team from the community health centre created an assessment tool based on the Stages of Change model of behaviour acquisition (Prochaska and DiClemente 1984; Prochaska 1994). Upon entry into the project, each patient was evaluated in six different spheres pertinent to diabetes: general knowledge about the disease, nutrition, physical activity, foot care, medication use and emotional stress. According to this first evaluation – which was very time-consuming, lasting about 90 minutes on average – an individualized service plan was elaborated, detailing provision of services in response to identified patient needs. Such a plan could include either individual or group sessions that provided direct care, such as foot care or nutrition counselling, or education in one of the six spheres. The evolution of diabetic patients through the different stages of diabetes-related health behaviours was monitored and assessed periodically by the nurse case managers. However, fragmentation in service delivery prevailed. According to one physician from the community health centre:
Probably what I was expecting was a call from the nurse saying: “Listen, we have elaborated our plan of services, now how would you like to proceed? Could we discuss this together? Would you like me to send it to you? What can we do with this? Could we schedule periodic meetings? Do you want to speak with the nutritionist?” I think I expected some initiative from them. Perhaps they were waiting for some initiative from me. I do not know.
Furthermore, implementation of the patient education strategy highlighted a lack of understanding and consensus among healthcare providers regarding the philosophy of the intervention. As physicians questioned the utility of the Stages of Change model adopted by the nurse case managers, and expected more concrete and speedy results than were observed in their patients, nurses advocated for effective triggering of patients’ lifestyle modifications, a process that required time and appropriate adjustment to individuals’ personal characteristics. The infusion of new money, therefore, mainly served to reinforce the power positions of health professionals within the network, and the multidisciplinary team working with diabetic patients was unable to attain a clear consensus regarding delivery (Figure 1).
Despite the professionals’ lack of consensus, most patients described improved knowledge of diabetes and its management as the most important benefit of their participation in the project. Improved comprehension of their disease and of the effects of adequate diet and medication helped them modify their diet, physical exercise and stress control. Such modifications were also reported by their family physicians. As one doctor in solo practice stated: “… they started coming back to me and telling me how they are going to exercise classes, how they are seeing the dietician and they are going to the foot care clinics, and that all of these things have been done, and my patients are so happy with it.”
Sub-process 3: Updating medical knowledge on diabetes
The Côte-des-Neiges project intended to improve family physicians’ clinical expertise on diabetes through continuing medical education, easier access to consultation with specialists, availability of a CD-ROM developed by the Canadian Diabetes Association (CDA) and elaboration of a flow sheet that updated knowledge on diabetes according to CDA guidelines. The College of Family Physicians of Canada offered CME credits to participating physicians, which provided an incentive for their involvement in these activities.
However, implementation of these manipulative strategies for integration had limited success. Physician involvement in CME sessions was rare, typically due to agenda incompatibilities. A physician from a medical clinic stated: “I didn’t participate in any CME stuff. There were scheduling conflicts.” The CD-ROM was also poorly received. One physician in solo practice said: “I received the CD-ROM. I did not find it very useful. It was fairly elementary. I saw no disadvantage about receiving the same thing on paper.” In contrast, the flow sheet was accepted by 35 out of 44 physicians (79.55%) participating in the project. Some physicians even incorporated it into the medical record of their non-diabetic patients.
Sub-process 4: Adopting a computerized information system
In order to introduce new mechanisms of communication, sponsors of the Côte-des-Neiges pilot project invested considerable resources in the acquisition of a computerized information system. This purchase was intended to facilitate feedback among healthcare providers via patient records.
Implementation of the system was problematic. First, the installation of workstations and medical training sessions stretched out over six months of the 12-month pilot project. Hence, physicians had only a few months to integrate the new system into their practice. Second, the lack of interface between the project system and suppliers (e.g., the laboratory) hindered adoption of the new technology. Third, barriers to data entry (e.g., physicians in solo practice had to enter patient data themselves) discouraged more widespread use of the innovation. One physician from the community health centre stated: “I have found [the new system] less useful because of time constraints. I am here part-time. So when I am here, I am booked with patients and so, unless I book specific time so I can sit at the computer we have in the hallway … .” Finally, initial technical problems discouraged utilization of the system afterwards. As one physician in solo practice remarked: “There is a bug in the program. It will not save the flow sheet. So after trying a couple of times, I have not tried again. They tried to fix it once and it was not successful. But maybe it has been fixed by now.” As a result, most care settings maintained a double patient record (electronic and paper) during the pilot project period.
Despite these difficulties, physicians recognized the usefulness of a computerized system, particularly for quick feedback among members of the multidisciplinary team and for scheduling visits with specialists. As one physician from a medical clinic stated:
This is coming. We’re all learning it. But it is a great problem for this group here. However, in a certain sense, … this is stimulating us. It is really an advantage for the unit. I see it as very positive. It is difficult. It is difficult for me, for the others, but it is an advantage. In the long term, it is a great advantage.
Sub-process 5: Mobilizing the local community
The Côte-des-Neiges pilot project included the strategy of mobilizing community resources beyond those provided by the local healthcare system to generate activities that would enhance diabetic patients’ quality of life. To this effect, links were established with various community agencies, including a variety of ethnic patient groups, health resources such as pharmacists, sports centres and supervised housing for the elderly. Unfortunately, several circumstances hindered community mobilization, including (1) the emphasis nurses placed on individual interventions, resulting in underutilization of other team experts in community intervention, (2) lack of clarity regarding the project’s community actions and (3) the limited period of time available for the pilot project. The lack of community mobilization was noted by a member of the clinical team:
So I think that there are a lot of clinical interventions. … There is a lot of information available for the client to be able to know his or her disease and to take care of himself or herself as best as possible. Up to now, I’ve considered that there is absolutely nothing regarding the community in this project. It is a shame, but it is not tragic either.
Discussion: Political Economy of the Côte-des-Neiges Project
This initiative was one of 140 projects funded by the federal government through Health Canada between 1997 and 2001, in order to test and evaluate new ways of organizing healthcare delivery. The sponsors of the Côte-des-Neiges project saw this federal program as a valuable opportunity for integrating care for type 2 diabetic patients. The program provided access to the two essential resources of Benson’s political economy of interorganizational networks – money (CAN$1.0 million from the government for project development, implementation and evaluation) and authority (credibility and legitimacy of the project’s sponsors for decision-making and action).
Despite their credibility and legitimacy in academia, research, public health and healthcare delivery, none of the project sponsors had any formal authority over physicians, who participated on a totally voluntary basis, nor over the other health professionals involved in the team, who were contractually linked to the community health centre. In addition, despite the number of project sponsors, none could be identified as its key leader. This lack of leadership hampered implementation, as described by one member of the Steering Committee:
Our management from the beginning was quite participative, and there were many leaders, not one from the outset. And what needs to happen is … there has to be one leader who has power that says: “This is what you have to do.” An organizational chart should have been drawn up from the beginning, outlining the communications that should occur. And I think it was not clear from the beginning that there was one key leader; there was a day-to-day manager, but not a key leader.
Most of the funds were used to pay for the salaries of the clinical team at the community health centre and the acquisition of the information system and hardware, which were given to the physicians in appreciation for their participation in the project. In Benson’s terms, these resources were used to develop both cooperative strategies (disease management, patient education, community mobilization) and manipulative strategies (CME and information technology). At the context level, these strategies directly altered the availability of resources during the year-long project. Initially, sponsors also intended to provide a financial incentive (payment mode) to physicians to encourage their participation, but this proposition was not accepted by the funding agency (the federal government).
The combination of cooperative and manipulative strategies seemed appropriate for supporting integrated care. However, as Benson notes, cooperative strategies succeed only when partners have strong bargaining power, each holding something of value to the others. This was not the situation in the Côte-des-Neiges pilot project – at least, not at the beginning. The manipulative strategies – which favoured the most powerful team members, i.e., physicians – were not as effective as expected: the physicians did not participate in CME and made little use of the information system. This lack of efficacy of manipulative strategies was compounded by the impossibility of remunerating the physicians for their participation. As a result, the pilot project would succeed or fail based on cooperative strategies that were set up under difficult conditions. Indeed, the three cooperative strategies were practically reduced to one – patient education. This unintended shift in emphasis increased the nurses’ bargaining power within the network to the detriment of the focus on integrated care, a drawback noted by one member of the Steering Committee:
My own feeling is that the use of the Prochaska model actually side-tracked the main emphasis of the project, which should be, and I believe was, integration of care. Now, people would say the Prochaska model enabled the provision of better care for the patients, but in reality the Prochaska model is a model that has yet to be proven, is a model that is being developed; and I do not think our goal was to develop the model, but rather it was to develop services, appropriate services, and integrated care. So my feeling was that there was too much emphasis put on that, too much resources and effort put on the Prochaska model and not enough effort put into the concept of integration and provision of services.
The issue here is not the appropriateness of the Prochaska model for framing patient educational activities. What is at issue is how the Prochaska model, which initially was an assessment tool for planning the project, became over time the sole focus of the initiative instead of the integration of healthcare services delivery.
At the level of sentiments and cooperative interactions (i.e., Benson’s “superstructure”), domain and ideological consensus were poorly developed owing to the physicians’ lack of awareness of the interventions to be implemented, and disagreement among members of the clinical team at the community health centre regarding the tasks to be accomplished. A lack of adequate clinical leadership was noted by one member:
The biggest challenge or the biggest problem …, according to what I have seen – I really summarize in general – it is at the time of the group’s meetings, we did not understand each other. We, the providers, we ran on in one way, and the model ran on another one. And this was frustrating as providers. Then if there is no consensus, if we do not start together, if we do not agree, then we lock up everyone together in a room, for three hours, but we leave and we all do not agree.
Work coordination mostly consisted of referrals from physicians to the community health centre, with services being delivered in parallel by each of the care providers involved. Professionals also tended not to value the work done by one another’s organizations. In addition to the historic separation among disciplines, most particularly between physicians and other health professionals, difficult relationships among members of the clinical team at the community health centre were heightened by the hierarchical manner in which the model was implemented. According to one team member:
If we talk about the group’s meetings, we always reviewed nursing first. One can see the hierarchy. The nurse is the first part, the most important. He or she is the link with the physician, the medical part. Then, the dietician. Everyone wanted to see the dietician. This runs together: diet and control. Then, we had foot care. And then, we reviewed social work at the end. … It would have been good to address things more globally.
In summary, a combination of inadequate authority, moderate flow of resources and relatively successful implementation of patient education activities resulted in what Benson would classify as a “low-equilibrium system.” In other words, after one year, the healthcare network retained its balance of fragmentation.
Yet, something beneficial happened at the level of network superstructure. The feedback that physicians received from their patients regarding the services provided at the community health centre, and the observable effects on patients who had adopted healthier lifestyles and gained better control of their disease, convinced physicians that they could no longer work alone when caring for patients with chronic diseases. In Benson’s terms, for the sake of their patients, this initiative mobilized physicians to place greater value on services provided by other health professionals in the local network.
Integrated models of healthcare delivery have attracted attention from researchers and decision-makers for at least the last 15 years. Much work published on the topic concerns theoretical models and expected benefits attributed to integration (in the Canadian context, see, e.g., Leatt et al. 2000; Marriot and Mable 2000). However, as noted by Fleury and Mercier (2002: 69): “The beneficial effects of service integration in the healthcare system are only demonstrated on the basis of a few empirical studies whose findings are mostly contradictory or inconclusive.” Furthermore, empirical research on integration has been dominated by its focus on results, both at a systemic level (e.g., Gillies et al. 1993; Shortell et al. 1996) and at a program level for specific clienteles (see, e.g., Johri et al. 2003 for a review of projects testing integrated models of care for the elderly).
Given such a research context, our work makes a twofold contribution. On the one hand, it departs from the dominant research paradigm – which typically assumes a functional perspective and variance approaches – by adopting Benson’s political economy as a theoretical framework. This framework appears particularly appropriate in this investigation for at least three reasons. First, it constitutes a process theoretical approach, i.e., it helps explain how a phenomenon evolves over time and how it does so in a particular way, whereas a variance theory aims at explaining relationships between dependent and independent variables (Langley 1999); second, it concerns emergent interorganizational networks; and finally, it draws on an empirical study of relationships among human service agencies.
Further, as in any implementation evaluation, this study seeks to provide a comprehensive understanding of the process by which an “ideal” model of integrated care is effectively implemented. As such, and aside from the specific local scope of the project, this investigation provides four intertwined insights to those who seek to integrate primary care networks. First, the supply of new resources appears a necessary but insufficient condition for promoting integration. The great investment that the project’s sponsors made in information technology, with very poor or no results, properly illustrates this point. Second, the lack of adequate clinical leadership and consensus regarding the philosophy of intervention hindered the construction of a truly cooperative interprofessional relationship between physicians and nurses, and precluded the elaboration of a joint disease management plan. Third, implementing integration is an evolutionary process that requires an adequate temporal frame to succeed; stopping the project after only one year constituted a waste of resources and energy. Finally, the project suggests that healthcare integration, whatever form it takes, requires the health professionals involved to give sense to the conceived plan in order to be able to implement it. Put differently, a process of “sensemaking” (Weick 1995) is needed for practitioners to reach an adequate fit between the conceived plan – the vision – and the realized project.
Acknowledgment
This work was supported financially by the Health Transition Fund of the Federal Government of Canada (# QC-433).
Project sponsors included researchers and practitioners from the McGill Department of Family Medicine, the Côte-des-Neiges community health centre, the Montreal Public Health Division and the Multidisciplinary Research Group of Health (GRIS) from the Université de Montréal.
See, for example, the conclusions of the Sinclair Commission in Ontario (December 1999); the Premier’s Health Quality Council in New Brunswick (in progress as of January 2000); the Clair Commission in Quebec (December 2000); the Fyke Commission in Saskatchewan (April 2001); or the federal Romanow Commission (November 2002).
A community organizer is an agent who facilitates social dynamics related to health within a CLSC’s scope of action.
Social capital is the capacity of a collectivity to create and maintain links among its members (see, e.g., Kabanoff 1991; Putnam 1993; Kawachi et al. 1997).
Contributor Information
Charo Rodríguez, Area of Health Services and Policy Research, Department of Family Medicine, McGill University, Montreal, QC.
André-Pierre Contandriopoulos, Département d’administration de la santé, Université de Montréal, Montréal, QC.
Danielle Larouche, Groupe de recherche interdisciplinaire en santé (GRIS), Université de Montréal, Montréal, QC.
References
- American Diabetes Association. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1998;21(Suppl. 1):S5–S19. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- Anderson R.M., Arnold M.M., Funnell M.M., Fitzgerald J.T., Butler P.M., Feste C.C. Patient Empowerment: Results of a Randomized Controlled Trial. Diabetes Care. 1995;18(7):943–49. doi: 10.2337/diacare.18.7.943. [DOI] [PubMed] [Google Scholar]
- Armenakis A.A., Bedeian A.G. Organizational Change: A Review of Theory and Research in the 1990s. Journal of Management. 1999;25(3):293–315. [Google Scholar]
- Baker E.L., Melton R.J., Stange P.V., Fields M.L., Koplan J.P., Guerra F.A., Satcher D. Health Reform and the Health of the Public. Journal of the American Medical Association. 1994;272(16):1276–82. [PubMed] [Google Scholar]
- Bates D.W., Leape L.L., Cullen D.J., Laird N., Petersen L.A., Teich J.M., et al. Effect of Computerized Physician Order Entry and a Team Intervention on Prevention of Serious Medication Errors. Journal of the American Medical Association. 1998;280(15):1311–16. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- Bayless M., Martin C. The Team Approach to Intensive Diabetes Management. Diabetes Spectrum. 1998;11(1):33–37. [Google Scholar]
- Benson J.K. The Interorganizational Network As a Political Economy. Administrative Science Quarterly. 1975;20(2):229–49. [Google Scholar]
- Bergman H., Béland F., Lebel P., Contandriopoulos A.P., Tousignant P., Brunelle Y., et al. Care for the Frail Elderly in Canada: Fragmentation or Integration. Canadian Medical Association Journal. 1997;157(8):1116–21. [PMC free article] [PubMed] [Google Scholar]
- Borgiel A.E.M., Williams J.I., Davis D.A., Dunn E.V., Hobbs N., Hutchison B., et al. Evaluating the Effectiveness of Two Educational Interventions in Family Practice. Canadian Medical Association Journal. 1999;161(8):965–70. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, Primary Prevention Working Group. Primary Prevention of Type 2 Diabetes Mellitus by Lifestyle Intervention: Implications for Health Policy. Annals of Internal Medicine. 2004;140(11):951–58. doi: 10.7326/0003-4819-140-11-200406010-00036. [DOI] [PubMed] [Google Scholar]
- Commission of Study on Health Services and Social Services of Quebec (Clair Commission) Report and Recommendations. Quebec, QC: Ministry of Health, Government of Quebec; 2000. [Google Scholar]
- Contandriopoulos A.P. Journées d’orientation sur la place des unités de courte durée gériatriques et des équipes dans un système en transformation. Montréal: Institut de gériatrie de Montréal; 2000. L’Hôpital face aux nouveaux modèles de prise en charge des personnesâgées vulnérables. [Google Scholar]
- Day J.L., Rayman G., Hall L., Davies P. ‘Learning Diabetes’ – A Multi-media Learning Package for Patients, Carers and Professionals to Improve Chronic Disease Management. Medical Informatics. 1997;22(1):91–104. doi: 10.3109/14639239709089836. [DOI] [PubMed] [Google Scholar]
- Demers M., Brunelle Y. Québec, QC: Ministère de la Santé et des Services Sociaux; 2000. Organisation de l’omnipratique au Québec entre 1994 et 1999. [Google Scholar]
- D’Eramo-Melkus G.A., Wylie-Rosett J., Hagan J.A. Metabolic Impact of Education in NIDDM. Diabetes Care. 1992;15(7):864–69. doi: 10.2337/diacare.15.7.864. [DOI] [PubMed] [Google Scholar]
- Ellrodt G., Cook D.J., Lee J., Cho M., Hunt D., Weingarten S. Evidence-Based Disease Management. Journal of the American Medical Association. 1997;278(20):1687–92. [PubMed] [Google Scholar]
- Etzweiler D.D. Chronic Care: A Need in Search of a System. Diabetes Educator. 1997;23(5):569–73. doi: 10.1177/014572179702300509. [DOI] [PubMed] [Google Scholar]
- Fleury M.J., Mercier C. Integrated Local Networks as a Model for Organizing Mental Health Services. Administration and Policy in Mental Health. 2002;30(1):55–73. doi: 10.1023/a:1021227600823. [DOI] [PubMed] [Google Scholar]
- Gerber D.G., Stewart D.L. Prevention and Control of Hypertension and Diabetes in an Underserved Population through Community Outreach and Disease Management: A Plan of Action. Journal of the Association for Academic Minority Physicians. 1998;9(3):48–52. [PubMed] [Google Scholar]
- Gillies R.R., Shortell S.M., Anderson D.A., Mitchell J.B., Morgan K.L. Conceptualizing and Measuring Integration: Findings from the Health Systems Integration Study. Hospital & Health Services Administration. 1993;38(4):467–89. [PubMed] [Google Scholar]
- Glasgow R.E., Wagner E.H., Kaplan R.H., Vinicor F., Smith L., Norman J. If Diabetes Is a Public Health Problem, Why Not Treat It As One? A Population-Based Approach to Chronic Illness. Annals of Behavioral Medicine. 1999;21(2):159–70. doi: 10.1007/BF02908297. [DOI] [PubMed] [Google Scholar]
- Greenfield S., Kaplan S.H., Ware J.E., Jr., Yano E.M., Frank H.J.L. Patients’ Participation in Medical Care: Effects on Blood Sugar Control and Quality of Life in Diabetes. Journal of General Internal Medicine. 1988;3(5):448–57. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- Greenlink M.R. Educating Physicians for Population-Based Clinical Practice. Journal of the American Medical Association. 1992;267(12):1645–48. [PubMed] [Google Scholar]
- González E.R., Crane V.S. Designing a Disease Management Program: How to Get Started. Formulary. 1995;30:326–40. [PubMed] [Google Scholar]
- Harris M.I. Clinical and Public Health Issues. Diabetes Care. 1993;16(4):642–52. doi: 10.2337/diacare.16.4.642. [DOI] [PubMed] [Google Scholar]
- Hiss R.G. Barriers to Care in Non-insulin Dependant Diabetes Mellitus: The Michigan Experience. Annals of Internal Medicine. 1996;124(1–2):146–48. doi: 10.7326/0003-4819-124-1_part_2-199601011-00012. [DOI] [PubMed] [Google Scholar]
- Hunt D.L., Haynes R.B., Hanna S.E., Smith K. Effects of Computer-Based Clinical Decision Support Systems on Physician Performance and Patient Outcomes. Journal of the American Medical Association. 1998;280(15):1339–46. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- Jiang H.J., Stryer D., Friedman B., Andrews R. Multiple Hospitalizations for Patients with Diabetes. Diabetes Care. 2003;26(5):1421–26. doi: 10.2337/diacare.26.5.1421. [DOI] [PubMed] [Google Scholar]
- Johri M., Béland F., Bergman H. International Experiments in Integrated Care for the Elderly: A Synthesis of the Evidence. International Journal of Geriatric Psychiatry. 2003;18:222–35. doi: 10.1002/gps.819. [DOI] [PubMed] [Google Scholar]
- Kabanoff B. Equity, Equality, Power and Conflict. Academy of Management Review. 1991;16(2):416–41. [Google Scholar]
- Kawachi I., Kennedy B.P., Lochner K., Prothrow-Stith D. Social Capital, Income Inequality, and Mortality. American Journal of Public Health. 1997;87(9):1491–98. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger R.A., Casey M.A. Focus Groups: A Practical Guide for Applied Research (3rd ed.) Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- Langley A. Strategies for Theorizing from Process Data. Academy of Management Review. 1999;24(4):691–710. [Google Scholar]
- Larsen D.L., Cannon W., Towner S. Longitudinal Assessment of a Diabetes Care Management System in an Integrated Health Network. Journal of Managed Care Pharmacy. 2003;9(6):552–58. doi: 10.18553/jmcp.2003.9.6.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leape L.L., Bates D.W., Cullen D.J., Cooper J., Demonaco H.J., Gallivan T., et al. Systems Analysis of Adverse Drug Events. Journal of the American Medical Association. 1995;274(1):35–43. [PubMed] [Google Scholar]
- Leatt P., Pink G.H., Guerriere M. Towards a Canadian Model of Integrated Healthcare. Healthcare Papers. 2000;1(2):13–35. doi: 10.12927/hcpap..17216. [DOI] [PubMed] [Google Scholar]
- Lemieux V., Labrie P. Le Système gouvernetique des CLSC. Recherches Sociographiques. 1979;20(2):149–71. [Google Scholar]
- Marriott J., Mable A.L. Integrated Health Organizations in Canada: Developing the Ideal Model. Healthcare Papers. 2000;1(2):76–87. doi: 10.12927/hcpap.2000.17221. [DOI] [PubMed] [Google Scholar]
- McKinlay J., Marceau L. US Public Health and the 21st Century: Diabetes Mellitus. The Lancet. 2000;356:757–61. doi: 10.1016/S0140-6736(00)02641-6. [DOI] [PubMed] [Google Scholar]
- Meltzer S., Leiter L., Daneman D., Gerstein H.C., Lau D., Ludwig S., et al. 1998 Clinical Practice Guidelines for the Management of Diabetes in Canada. Canadian Medical Association Journal. 1998;159(Suppl. 8):S1–S29. [PMC free article] [PubMed] [Google Scholar]
- Miles M.B., Huberman A.M. An Expanded Sourcebook: Qualitative Data Analysis (2nd ed.) Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- Nasmith L., Moliner P., Rubenstein H., Côté B., Jimenez V., Marchand R., Marleau J. Developing an Integrated Model of Care for Diabetics: The Use of Nominal Groups to Determine the Needs of the Community. Canadian Journal of Diabetes Care. 2001;25(3):157–62. [Google Scholar]
- National Forum on Health. Canada Health Action: Building on the Legacy. The Final Report of the National Forum on Health. Ottawa: Government of Canada; 1997. [Google Scholar]
- O’Brien J.A., Patrick A.R., Caro J. Estimates of Direct Medical Costs for Microvascular and Macrovascular Complications Resulting from Type 2 Diabetes Mellitus in the United States in 2000. Clinical Therapeutics. 2003;25(3):1017–38. doi: 10.1016/s0149-2918(03)80122-4. [DOI] [PubMed] [Google Scholar]
- Orlikowski W.J. Improvising Organizational Transformation over Time: A Situated Change Perspective. Information Systems Research. 1996;7(1):63–92. [Google Scholar]
- Paillé P. De l’analyse qualitative en général et de l’analyse thématique en particulier. Revue de l’Association pour la Recherche Qualitative. 1996;15:179–94. [Google Scholar]
- Patton M.Q. Qualitative Research Methods (3rd ed.) Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Pestotnik S.L., Classen D.C., Evans R.S., Burke J.P. Implementing Antibiotic Practice Guidelines through Computer-Assisted Decision Support: Clinical and Financial Outcomes. Annals of Internal Medicine. 1996;124:884–90. doi: 10.7326/0003-4819-124-10-199605150-00004. [DOI] [PubMed] [Google Scholar]
- Pettigrew A.M. Longitudinal Field Research on Change: Theory and Practice. Organization Science. 1990;1(3):267–92. [Google Scholar]
- Prochaska J.O. Strong and Weak Principles for Progressing from Precontemplation to Action of the Basis of Twelve Problem Behaviors. Health Psychology. 1994;12(1):47–51. doi: 10.1037//0278-6133.13.1.47. [DOI] [PubMed] [Google Scholar]
- Prochaska J.O., DiClemente C.C. Transtheoretical Therapy: Towards a More Integrative Model of Change. Psychotherapy: Theory, Research and Practice. 1982;19(3):276–88. [Google Scholar]
- Putnam R.D. The Prosperous Community: Social Capital and Public Life. American Prospect. 1993;4(13):35–42. [Google Scholar]
- Redhead J., Hussain A., Gedling P., McCulloch A.J. The Effectiveness of a Primary-Care-Based Diabetes Education Service. Diabetic Medicine. 1993;10(7):672–75. doi: 10.1111/j.1464-5491.1993.tb00143.x. [DOI] [PubMed] [Google Scholar]
- Rosnick M. Building Public Health Goals into the Purchasing Process: Managed Care Perspective. American Journal of Preventive Medicine. 1998;14(Suppl. 3):78–83. doi: 10.1016/s0749-3797(97)00041-x. [DOI] [PubMed] [Google Scholar]
- Rubin H.J., Rubin I. Qualitative Interviewing: The Art of Hearing Data. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- Safran M.A., Mukhtar Q., Murphy D.L. Implementing Program Evaluation and Accountability for Population Health: Progress of a National Diabetes Control Effort. Journal of Public Health Management Practice. 2003;9(1):58–65. doi: 10.1097/00124784-200301000-00008. [DOI] [PubMed] [Google Scholar]
- Shortell S.M., Gillies R.R., Anderson D.A., Erickson K.M., Mitchell J.B. Remaking Health Care in America. San Francisco: Jossey–Bass; 1996. [PubMed] [Google Scholar]
- Sylvestry M.F., Marro E.P. Disease Management: Partnering for Better Patient Care. Medical Interface. 1996;9(7):100–04. [PubMed] [Google Scholar]
- Wagner E.H. Population-Based Management of Diabetes Care. Patient Education and Counseling. 1995;26(1–3):225–30. doi: 10.1016/0738-3991(95)00761-n. [DOI] [PubMed] [Google Scholar]
- Wagner E.H., Austin B.T., Von Korff M. Improving Outcomes in Chronic Illness. Managed Care Quarterly. 1996;4(2):12–25. [PubMed] [Google Scholar]
- Weick K.E. Sensemaking in Organizations. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- Weiss K. A Look at Population-Based Medical Care. Part 1. Disease-a-Month. 1998;44(8):353–69. doi: 10.1016/s0011-5029(98)90005-0. [DOI] [PubMed] [Google Scholar]
- Yutchtman E., Seashore S.E. A System Resource Approach to Organizational Effectiveness. American Sociological Review. 1967;32:891–903. [Google Scholar]