Abstract
Obesity has been strongly implicated as a risk factor for knee osteoarthritis and, in some studies, for osteoarthritis of the hip. Osteoarthritis is the most commonly reported diagnosis for joint replacement patients. In this study, we conducted analyses based on data from the Canadian Joint Replacement Registry (CJRR) to estimate the relationships between overweight and obesity and rates of joint replacement surgery in Canada. Obese persons were over three times as likely and overweight persons were one and a half times more likely to undergo joint replacement surgery, compared to those in the acceptable weight category in 2003–04. This study provides evidence of a clinically relevant association between obesity and joint replacement surgery.
Abstract
L’obésité est souvent citée comme un facteur de risque pour l’ostéoarthrite du genou et, selon certaines études, pour celle de la hanche. L’ostéoarthrite est le diagnostic le plus fréquemment posé chez les patients auxquels on recommande un remplacement articulaire. Dans cette étude, nous analysons des données tirées du Registre canadien des remplacements articulaires (RCRA) pour évaluer les relations entre l’excédent de poids et l’obésité et les taux de chirurgie de remplacement articulaire au Canada. En 2003–04, les personnes obèses étaient trois fois plus susceptibles de subir un remplacement articulaire et celles ayant un excédent de poids étaient une fois et demie plus susceptibles d’en subir une, comparativement aux personnes ayant un poids acceptable. Cette étude fournit des preuves à l’effet qu’il existe une association clinique pertinente entre l’obésité et la chirurgie de remplacement articulaire.
Obesity has been consistently identified as a risk factor for osteoarthritis, particularly of the knee (Felson et al. 1988). The link between obesity and hip osteoarthritis is not as well delineated but has been found in some studies (e.g., Cooper et al. 1998; Marks and Allegrante 2002), including a large prospective cohort study (Karlson et al. 2003). Osteoarthritis is the most commonly reported diagnosis for joint replacement patients (CIHI 2005a).
A large-scale, national survey, which included measurements of the height and weight of Canadians in 2004, classified 23% of the adult population as obese according to international standards, compared to 14% a quarter century ago (Tjepkema 2005). In parallel, joint replacement rates have increased significantly over time. Knee replacement rates increased by 50% in the period from 1994–95 to 2002–03, while hip replacement rates increased by 11% (CIHI 2005a).
In this study, we provide quantitative estimates of the relationships between overweight and obesity and the rates of joint replacement surgery using Canadian data.
Methods
Data source and study population
Patients were identified from the Canadian Joint Replacement Registry (CJRR), which collects demographic, surgical and implant data on hip and knee replacement procedures in Canada. CJRR is managed by the Canadian Institute for Health Information (CIHI). Orthopedic surgeons submit data to the CJRR on a voluntary basis for patients who provide consent to participate. Annually, CJRR includes approximately 54% of all joint replacement surgeries in acute care hospitals (CIHI 2005b).
Approximately 65% (n = 17,244) of patients in the CJRR 2003–04 database were included in this study. These patients had valid height and weight values recorded at the time of surgery and a surgery date between April 1, 2003 and March 31, 2004. Body mass index (BMI) was calculated using weight in kilograms divided by height in metres squared. Patients were assigned to the following internationally accepted BMI categories: less than 18.5 (underweight); 18.5–24.9 (acceptable); 25.0–29.9 (overweight); 30.0 or higher (obese) (Tjepkema 2005; World Health Organization 1995). Data were available for all provinces and territories, with the exception of Yukon and Nunavut, where joint replacement surgery is not routinely performed. Included in the study were total and partial hip and knee replacement surgeries, both primary and revision procedures, as defined by the submitting orthopedic surgeon. Comparative BMI data based on measured height and weight were obtained for a representative sample of the Canadian adult population (by age group and sex) from the Canadian Community Health Survey (Statistics Canada 2005).
Data analysis
In order to characterize CJRR patients, data were analyzed by sex and age group according to the joint on which the procedure was performed. Significance testing was performed at the 0.05 level using the chi-square test. Characteristics of the CJRR sample by BMI category were compared with those of the Canadian adult population based on the Canadian Community Health Survey (Statistics Canada 2005).
In order to estimate the relative risk of obesity as an independent factor for joint replacement surgery, calculations using age–sex standardization were performed. Age and sex distributions were found to be significantly different among BMI groups. Therefore, direct age–sex standardization was employed using Statistics Canada 2004 adult population BMI estimates by age and sex (Statistics Canada 2005) as the standard population. Age–sex-specific joint replacement rates for the study sample were calculated and then multiplied by their respective weights generated from the standard population. The products were summed to total the age–sex standardized rate for each BMI group. The underweight group and cases under the age of 20 were excluded owing to small numbers.
The age–sex standardized rate for the obese group was divided by the age–sex standardized rate for the acceptable weight group in order to derive a rate ratio (RR). A similar rate ratio was derived for the overweight group compared to the acceptable weight group. The 95% confidence intervals (CI) were calculated for each of the rate ratios.
TABLE 1.
Joint replacement patients and Canadian population by BMI category, age group and sex
| JOINT REPLACEMENT PATIENTS (2003–04) |
CANADIAN ADULT POPULATION (2004) |
|||||
|---|---|---|---|---|---|---|
| ACCEPTABLE % |
OVERWEIGHT % |
OBESE % |
ACCEPTABLE % |
OVERWEIGHT % |
OBESE % |
|
| Total | 18.1 | 35.0 | 46.0 | 38.9 | 36.1 | 23.1 |
| Female | 20.2 | 31.4 | 47.2 | 44.1 | 30.2 | 23.2 |
| Male | 15.0 | 40.4 | 44.1 | 33.6 | 42.0 | 22.9 |
| Age | ||||||
| 20–44 | 30.6 | 32.0 | 33.7 | 45.5 | 33.2 | 18.6 |
| Female | 34.9 | 26.1 | 34.1 | 52.7 | 26.2 | 17.8 |
| Male | 26.1 | 38.2 | 33.3 | 38.7 | 39.9 | 19.4 |
| 45–74 | 14.2 | 32.8 | 52.3 | 30.5 | 39.8 | 28.9 |
| Female | 16.5 | 28.7 | 54.0 | 35.5 | 34.1 | 29.2 |
| Male | 11.2 | 38.4 | 49.9 | 25.4 | 45.6 | 28.6 |
| 75+ | 25.2 | 40.2 | 33.3 | 33.0 | 41.2 | 23.6 |
| Female | 26.3 | 37.1 | 35.0 | 34.7 | 36.1 | 26.5 |
| Male | 23.2 | 45.9 | 30.3 | 30.5 | 49.0 | 19.3 |
Source: Canadian Joint Replacement Registry, CIHI; Canadian Community Health Survey, Statistics Canada.
Results
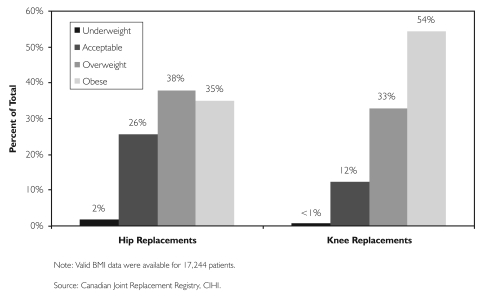
Among hip replacement patients (n = 7,538), 73% were classified as overweight or obese at the time of surgery, compared to 87% of knee replacement patients (n = 9,706) (Figure 1). Females made up 59% of the patients undergoing total hip replacement and 61% of those undergoing total knee replacement. Male patients were more likely to be overweight or obese (85% combined) compared to females (79% combined). Joint replacement patients aged 45 to 74 were more likely to be obese or overweight (85% combined) compared to the other two age groups (66% for those under the age of 45 and 74% for those aged 75 and over).
FIGURE 1.
Hip and knee replacement patients by body mass index (BMI) category, Canada, 2003–04
When compared to the 2004 Canadian adult population (Table 1), 46% of the joint replacement patients (hip and knee) were classified as obese, compared to 23% for Canadian adults in this category. Roughly the same percentage of joint replacement patients and the Canadian adult population were considered overweight – 35% and 36%, respectively. While only 18% of joint replacement patients were considered to have acceptable weights, the Canadian adult population rate for this category was 39%.
When we used direct age–sex standardization to determine risk ratios, we found that persons in the obese category were over three times (RR = 3.12, 95% CI, 2.99–3.25) as likely to undergo joint replacement surgery, and persons in the overweight category were one and a half times (RR = 1.53, 95% CI, 1.46–1.60) more likely, compared to those in the acceptable weight category.
Discussion
Using Canadian data, our study demonstrates a strong cross-sectional relationship between rates of overweight and obesity and joint replacement surgery. This association has also been established in a large, frequency-matched case-control study in the United States (Wendelboe et al. 2003).
To date, however, there is inconclusive evidence available from scientific investigation regarding the influence of obesity on the success of joint replacement surgery from a perioperative or postoperative perspective. For instance, Foran et al. (2004) found that obese knee replacement patients (BMI ≥ 30) had lower Knee Society scores (Insall et al. 1989) postoperatively compared to non-obese patients and those with BMI ≥ 40 had higher revision rates after a minimum follow-up period of five years. Jibodh et al. (2004) found that hip replacement patients with BMI ≥ 40 experienced longer operating times and higher blood loss compared to other BMI groups, but did not differ in terms of functional recovery or hospital resource use. In contrast, Spicer et al. (2001) found no difference in the Knee Society scores of knee replacement patients in differing BMI groups. A 10-year survival analysis (using revision of any component as an endpoint) found that obese and non-obese groups were similar in outcome.
A limitation of this study is the possible bias arising from underreporting of joint replacement procedures, given the voluntary nature of the CJRR (BMI data were available for approximately 35% of all joint replacement procedures performed in Canada). The rate ratios presented in this report are based on the assumption that underreporting in the sample was similar across BMI categories. When we compared our joint replacement sample with the Canadian adult population data, overall geographical BMI patterns were found to be similar and consistent (data not shown).
Conclusion
Unhealthy weights present a complex and challenging problem for individual Canadians and for public health and healthcare delivery practitioners and systems. Based on the knowledge that the determinants of healthy weights encompass a wide range of social, cultural, physical and economic factors, recent Canadian reports suggest that unhealthy weights are best addressed from prevention or treatment perspectives that utilize a multifaceted approach (CIHI 2006; Raine 2004). Our study suggests a relationship between joint replacement and overweight and obesity that is of increasing policy relevance in Canada and other countries. For example, because of financial considerations, NHS trusts in Suffolk in the United Kingdom recently made the decision to deny funding for joint replacement surgery for obese patients (Coombes 2005). Other policy- and decision-makers are endeavouring to understand the relationship between obesity trends and the need for health services in order to facilitate planning and program development.
Contributor Information
Nicole De Guia, Canadian Joint Replacement Registry, Canadian Institute for Health Information (CIHI), Toronto, ON.
Naisu Zhu, Health Services Information – Toronto Canadian Institute for Health Information (CIHI), Ottawa, ON.
Margaret Keresteci, Clinical Registries, Canadian Institute for Health Information (CIHI), Toronto, ON.
Juqing Ellen Shi, Canadian Joint Replacement Registry, Canadian Institute for Health Information (CIHI), Toronto, ON.
References
- Canadian Institute for Health Information (CIHI) Canadian Joint Replacement Registry 2005 Report: Total Hip and Total Knee Replacements in Canada. Toronto: Author; 2005a. [Google Scholar]
- Canadian Institute for Health Information (CIHI) Data Quality Documentation: Canadian Joint Replacement Registry 2003–2004. Toronto: Author; 2005b. [Google Scholar]
- Canadian Institute for Health Information (CIHI) Improving the Health of Canadians: Promoting Healthy Weights. Ottawa: Author; 2006. [Google Scholar]
- Coombes R. Rationing of Joint Replacements Raises Fears of Further Cuts. British Medical Journal. 2005;331(7528):1290. doi: 10.1136/bmj.331.7528.1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper C., Inskip H., Croft P., et al. Individual Risk Factors for Hip Osteoarthritis: Obesity, Hip Injury and Physical Activity. American Journal of Epidemiology. 1998;147(6):516–22. doi: 10.1093/oxfordjournals.aje.a009482. [DOI] [PubMed] [Google Scholar]
- Felson D.T., Anderson J.J., Naimark A., et al. Obesity and Knee Osteoarthritis. The Framingham Study. Annals of Internal Medicine. 1988;109(1):18–24. doi: 10.7326/0003-4819-109-1-18. [DOI] [PubMed] [Google Scholar]
- Foran J.R.H., Mont M.A., Etienne G., et al. The Outcome of Total Knee Arthroplasty in Obese Patients. Journal of Bone and Joint Surgery. 2004;86-A(8):1609–15. doi: 10.2106/00004623-200408000-00002. [DOI] [PubMed] [Google Scholar]
- Insall J.N., Dorr L.D., Scott R.D., et al. Rationale of the Knee Society Clinical Rating System. Clinical Orthopaedics and Related Research. 1989;248:13–14. [PubMed] [Google Scholar]
- Jibodh S.R., Gurkan I., Wenz J.F. In-Hospital Outcome and Resource Use in Hip Arthroplasty: Influence of Body Mass. Orthopedics. 2004;27(6):594–601. doi: 10.3928/0147-7447-20040601-16. [DOI] [PubMed] [Google Scholar]
- Karlson E.W., Mandl L.A., Aweh G.N., et al. Total Hip Replacement Due to Osteoarthritis: The Importance of Age, Obesity, and Other Modifiable Risk Factors. American Journal of Medicine. 2003;114(2):93–98. doi: 10.1016/s0002-9343(02)01447-x. [DOI] [PubMed] [Google Scholar]
- Marks R., Allegrante J.P. Body Mass Indices in Patients with Disabling Hip Osteoarthritis. Arthritis Research. 2002;4(2):112–16. doi: 10.1186/ar387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raine K.D. Overweight and Obesity in Canada: A Population Health Perspective. Ottawa, ON: CIHI; 2004. [Google Scholar]
- Spicer D.D.M., Pomeroy D.L., Badenhausen W.E., et al. Body Mass Index As a Predictor of Outcome in Total Knee Replacement. International Orthopaedics. 2001;25(4):246–49. doi: 10.1007/s002640100255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada. Measured Adult Body Mass Index (BMI), by Age Group and Sex, Household Population Aged 18 and Over Excluding Pregnant Females, Canada. 2005 Retrieved February 17, 2006. http://www.statcan.ca/english/research/82-620-MIE/2005001/tables/t001_en.htm .
- Tjepkema M. Adult Obesity in Canada: Measured Height and Weight. Ottawa: Statistics Canada; 2005. catalogue no. 82-620-MWE. [Google Scholar]
- Wendelboe A.M., Hegmann K.T., Biggs J.J., et al. Relationships between Body Mass Indices and Surgical Replacements of Knee and Hip Joints. American Journal of Preventive Medicine. 2003;25(4):290–95. doi: 10.1016/s0749-3797(03)00218-6. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) Physical Status: The Use and Interpretation of Anthropometry. WHO Technical Report Series. Geneva, Switzerland: Author; 1995. [PubMed] [Google Scholar]