Magnetic resonance imaging (MRI) is a non- invasive imaging tool that utilizes a strong Mmagnetic field and radio frequency waves to visualize in great detail organs, soft tissue, and bone. Unlike conventional x-rays (including computed tomography [CT]), there is no exposure to ionizing radiation and at most field strengths (generally below 7 Tesla) the procedure is considered safe for nearly every age group. Because it is non-invasive (i.e., does not break the skin or harm the body) and possesses excellent spatial resolution (down to millimeters), the use of MRI as a research tool has increased exponentially over the past decade. Uses have ranged from add-ons to a clinical study (e.g., after scanning a child who has fallen from a bicycle, the radiologist might do an extra sequence to explore ways of obtaining higher resolution images) to studies of brain development in typically developing children. In addition, a major effort has been made in recent years to use MRI to study brain function (so-called “functional MRI” [fMRI]). Because the clinical utility of fMRI has not yet been realized, fMRI is still considered highly exploratory, and we cannot yet identify incidental findings of a functional (as opposed to structural) nature.
Before discussing the issue of incidental findings (IFs) in MRI brain research, it is worthwhile to review some of the more common uses of MRI in studying both typical and atypical brain structure in children and adults. One such use has been to explore typical brain development across the first two decades of life. For example, the National Institutes of Health (NIH) has supported a contract issued to approximately seven institutions in North America to collect structural data on 0–18-year-olds; the goal of this project is to develop an atlas of the developing brain.1 Similar work is being performed by individual investigators as well. For example, John Gillmore and colleagues at the University of North Carolina have conducted groundbreaking work on infants between zero and one year of age,2 and Jay Giedd and colleagues at the NIH have conducted similar work on children age four and above.3 Perhaps most common has been the use of structural (anatomical) MRI to ground fMRI data; that is, all fMRI investigations require that structural data be obtained as well. In order to know precisely which regions of the brain are activated in a particular task, one must overlay the functional data on the structural (anatomic) data. For example, if the investigator wishes to determine whether the hippocampus is active during memory encoding, it is essential to know precisely where in the brain the hippocampus lies. As a result of this need to acquire structural data, large numbers of structural scans are performed.
Despite its high costs (approximately $1500 for a clinical scan and $500 to $600 for a research scan), MRI has become very popular among those interested in brain development, primarily because it can provide such detailed images of the brain and because the exact same procedure can be used across the entire lifespan to illuminate brain development. Unfortunately, however, relatively little attention has been paid to the issue of IFs, where “an incidental finding is a finding concerning an individual research participant that has potential health or reproductive importance and is discovered in the course of conducting research but is beyond the aims of the study.”4 Although there are now reasonably accurate estimates of the incidence of IFs among adults — more than five percent of scans performed on adults show IFs5 — there are no comparable figures for children among developmental and pediatric investigators. Personal communication with the author among such investigators, however, places the estimate between five and ten percent.6 Of course, clinical intuition and personal anecdote are no substitute for real data, and thus, it would seem imperative for the field to acquire accurate estimates of IFs among children (assuming the figures that are in place for adults are accurate).
Tremendous variation exists among investigators and laboratory sites in their approach to handling IFs. For example, some Institutional Review Boards (IRBs) require a discussion of IFs in their consent form, whereas others do not.7 In addition, some sites and IRBs require that all research scans undergo a clinical read to ascertain whether IFs are present in an individual child, although not all sites do and among those that do, not all are read by a board-certified neuroradiologist. The urgent need for systematic oversight of IFs can be illustrated by the following case study.
The investigators discussed the matter with the university IRB, and were told that they had been in full compliance with procedures then in force, and that this was not an adverse event. Nevertheless, based on the surgeon’s read of the experimental MRI scan, it is not unreasonable to think that if this scan had been read by a neuroradiologist, the tumor would have been spotted earlier. The tumor would still have required removal, but the earlier warning might have been useful, as the student’s unexpected seizure could have been dangerous if she been driving at the time, for example.
This case study illustrates the challenges faced by MRI investigators. Although some IRBs and the NIH now require that all MRI scans be read by a neuroradiologist,8 investigators and sites may still have differing procedures. For example, in some cases the scans are read informally and no report is issued; in others, the scans are formally read and a formal report is prepared and submitted to the principal investigator. In still others, the investigators — often Ph.D.s with no clinical training — read the scans themselves and only refer the scan to a neuroradiologist if something suspicious is detected.
Even among sites where all scans are read clinically, there is variability in who reads the scans and when the scans are read. For example, in queries the author has made to colleagues from around the United States, it appears to be the case that at some sites, scans are batched and read “en masse” at some later point in time, so there might be a delay of weeks or months between when the scan was performed and when it was read.
In addition to whether and when scans are read clinically, there are a number of other issues that must be considered in the context of MRI IFs. First, there has been a proliferation of higher-field scanners; for example, 3 Tesla scanners have, in many places, replaced 1.5 Tesla scanners, and 4 and 7 Tesla scanners are now much more common than they once were. With higher field strength come greater sensitivity and thus, greater likelihood of false positives — that is, detecting a problem when one does not actually exist. Second, many university and research sites use experimental pulse sequences (i.e., different algorithms that permit one to obtain higher resolution data) that may similarly lead to an increase in false positives. Third, as the use of MRI continues to proliferate, and the number of scans being performed increases, it is difficult to predict what the true incidence of IFs will be. Fourth, at many sites, the primary or principal investigator is often a Ph.D. student, postdoctoral fellow, or faculty member with no clinical training in neuroradiology and, very likely, relatively little training in neuroanatomy. If such individuals are the ones to read a scan, the possibility of missing an incidental finding will likely increase. Fifth, in the context of studying brain development, we thus far have only a rudimentary understanding of what typical development looks like. As a result, we do not have a template for what normal brain structure looks like at different ages, which increases the risk of both false positives and false negatives. Sixth, because of the costs involved in having a neuroradiologist read each scan, there is a financial disincentive to having such experts read each scan.
In the early to mid 1990s, a student at a major research university volunteered as an MRI study participant. The study involved being scanned by what was at the time a relatively high-field scanner, 4 Tesla. Because few such scanners existed at that time, the work was considered experimental; in addition, the scan sequence was also exploratory (an example of the structural data obtained at 4 Tesla can be seen in Figure 1). As a result, and because it was not required by the IRB, the investigators did not have the scans read clinically. (In prior consultation with a neuroradiologist, the investigators learned that such scans were far from clinical grade, which would have increased the uncertainty of a clinical read.)
The study itself was unsuccessful, and the findings were never published. A few years later the student experienced an epileptic seizure and was brought by ambulance to a local emergency room. The patient underwent a neurological and neurosurgical evaluation, whereupon a brain tumor was found. The student was admitted to the hospital and surgery was scheduled. The student showed the surgeon a copy of the MRI scan he/she was given by the investigators from a few years earlier. The neurosurgeon studied the MRI scan and identified the tumor, surmising it had likely been present since birth.
Functional MRI
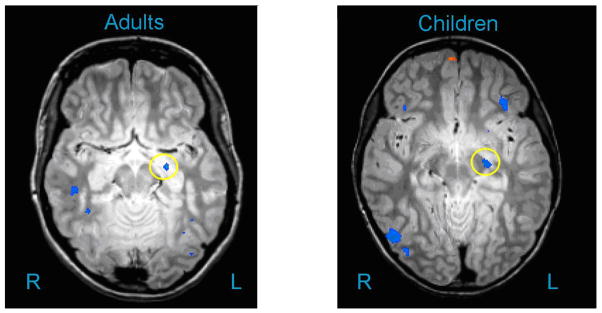
Over and above the challenges of IFs in structural MRI, we must anticipate the exponential growth of functional MRI (an example of fMRI scans of an adult and a child can be seen in Figure 2). Because of its potential to shed light on brain function in real time, and to do so across the lifespan, there has been an enormous increase in the use of this tool across the world. Moreover, it is only a matter of time before fMRI will be used routinely in clinical settings (for example, in localizing particular brain functions before surgery). Leaving aside the structural data obtained during an fMRI procedure (which can certainly produce incidental findings), there exists the potential for identifying incidental findings in the functional data. For example, when investigating the neural source of speech or language or memory, it may become apparent that a given individual’s brain does not show the same pattern of metabolic activity (e.g., increase or decrease in blood flow) as the other participants in the research. Of course, diminished blood flow can mean many things. For example, it could be that the participant has a particularly efficient brain and requires less oxygen to perform a given task; it could also mean that blood flow to that region is diminished because of a vascular abnormality or a tumor that limits or redirects blood flow. The point is simply that at present, we do not have anything like a normal template of brain function, and so cannot reliably identify abnormal incidental findings in the realm of brain function.
Figure 2. Functional MRI Scan in a Child (Right Figure) and an Adult (Left Figure).
The areas circled represent regions of interest identified by the investigator.
Future of Neuroimaging
Aside from MRI-based tools, the future of neuroimaging broadly defined involves a host of other imaging modalities that are currently in use or are being refined and developed. These modalities will raise further issues involving incidental findings, and are discussed below.
Magnetic Encephalography (MEG)
MEG records the minute magnetic activity that is generated by electrically active neurons. It has excellent spatial and temporal resolution. Although very expensive at present (a full MEG system can cost in excess of $2 million) and therefore used in only a handful of places, we are likely to see an increase in its use in coming years.
MEG is often combined with MRI, primarily for the purpose of source localization (i.e., to identify the neural source of the magnetic fields that MEG detects), and as a result, an IF can potentially be found on the structural MRI data. However, of greater concern is that like fMRI, MEG yields poorly understood functional images of the brain, thus increasing the challenge of differentiating what is pathological from what is normal.
High-Density Electroencephalography (EEG)/Event-Related Potentials (ERPs)
In contrast to older methods of recording the brain’s electrical activity, it is now possible to record from a large number of electrodes — in some cases, 256 electrodes. The improved spatial sampling that comes from dense arrays of electrodes brings with it greater sensitivity in detecting abnormal brain activity (e.g., subclinical seizures). However, as is the case with fMRI, the vast majority of investigators using this tool are not neurologists, but rather cognitive neuroscientists or psychologists. As a result, these investigators are not in a position to formally read the EEG to ascertain whether there is abnormal brain activity. Moreover, no atlas of normal EEG development currently exists, and as a result, it is virtually impossible to compare a given participant’s data to a normal template.
Functional Near-Infrared Spectroscopy (fNIRS)
This involves the use of lasers to pass light through the skull; the light is then refracted and detected by an adjacent receiving “optode.” The refraction patterns permit inferences about oxygenated and deoxygenated blood, which is identical to the BOLD (Blood Oxygenated Level Dependent) response obtained in fMRI. The use of fNRIS is presently confined to a small number of labs around the world, but because it has excellent, although limited, spatial resolution (i.e., it can only examine structures that sit on or very close to the cortical surface) and because the technology is relatively inexpensive (a few hundred thousand dollars vs. $3 million for fMRI), we should anticipate greater use in coming years. As is the case with fMRI, fNIRS has the potential to yield important information about blood flow and general metabolic activity, which will likely detect abnormalities. Although again, how an abnormality is defined is unclear, given the lack of a normative template.
Conclusions and Recommendations
MRI and other developing imaging modalities have great potential for revealing the secrets of the brain and brain development, yet they come with the potential cost of identifying IFs. We do not yet have an accurate estimate of the incidence of IFs and as a result, investigators do not know what to expect in any given study. In addition, no systematic reporting of IFs exists; thus, investigators at one site may have no knowledge of what is common at another. When it comes to other imaging modalities, we have virtually no information on what is or is not normal, nor in some cases do we know how to interpret or read an IF (e.g., in the case of fMRI or fNIRS). In this context, I offer some recommendations:
IRBs should come to a consensus regarding what consent forms should say about IFs, and this should be communicated to all investigators using MRI.
Funding agencies, NIH in particular, should be consistent in requiring that all MRI scans undergo a clinical read by a board-certified neuroradiologist, when the scanner being used has a history of clinical use, thus making the scan more interpretable than if the data were collected on an experimental system.
Investigators requesting funding for MRI research should build into their budget provisions for having scans read by a board-certified neuroradiologist.
NIH should fund the development of a national database that would keep track of all IFs discovered in the course of NIH-sponsored MRI research, and all investigators (regardless of funding) should have access to this database.
Research needs to be undertaken that examines the incidence and types of IFs emerging in MRI research on the brain. This information should be freely available to all MRI investigators. Given that some journals currently require all MRI data to be archived, such archived data sets should serve as a rich resource for such an investigation.
Outside of MRI research, other imaging modalities need to be monitored for IFs. At this time, it is premature to analyze IFs in fMRI, MEG, EEG/ERP, and fNIRS research, but it would be wise for investigators to begin to think about the issue. In this context, NIH may wish to support a working group to discuss this matter.
Finally, for all imaging modalities, principal investigators should consider whether their trainees (be they graduate students or postdoctoral fellows) should receive training in the identification of and ethics of IFs. There are, of course, pros and cons to adopting this recommendation. On the pro side are such trainees becoming more aware of the need to consider IFs in MRI research. On the con side, there is the risk of both false positives and false negatives, brought about by having what are essentially lay individuals act as experts (i.e., neuroradiologists).
Figure 1.
Anatomic Image Obtained from a 13-Year-Old Boy, Scanned at 4 Tesla
Acknowledgments
This publication was made possible by National Human Genome Research Institute (NHGRI) grant # R01 HG003178 (PI, S. M. Wolf; Co-Is, J. P. Kahn, F. Lawrenz, C. A. Nelson). Its contents are solely the responsibility of the author and do not necessarily represent the official views of NHGRI.
References
- 1.Almli CR, et al. the the Brain Development Cooperative Group. The NIH MRI Study of Normal Brain Development (Objective-2): Newborns, Infants, Toddlers, and Preschoolers. Neuroimage. 2007;35(1):308–325. doi: 10.1016/j.neuroimage.2006.08.058. [DOI] [PubMed] [Google Scholar]; Waber DP, et al. the Brain Development Cooperative Group. The NIH MRI Study of Normal Brain Development: Performance of a Population Based Sample of Healthy Children Aged 6 to 18 Years on a Neuropsychological Battery. Journal of the International Neuropsychological Society. 2007;13(5):729–746. doi: 10.1017/S1355617707070841. [DOI] [PubMed] [Google Scholar]
- 2.Gilmore JH, et al. 3 Tesla Magnetic Resonance Imaging of the Brain in Newborns. Psychiatry Research. 2004;132(1):81–85. doi: 10.1016/j.pscychresns.2004.04.004. [DOI] [PubMed] [Google Scholar]; Gilmore JH, et al. Imaging Early Childhood Brain Development in Humans. presentation at the Society for Neuroscience; 2006. [Google Scholar]
- 3.Giedd JN, et al. Brain Development during Childhood and Adolescence: A Longitudinal MRI Study. Nature Neuroscience. 1999;2(10):861–863. doi: 10.1038/13158. [DOI] [PubMed] [Google Scholar]
- 4.Wolf SM, et al. Managing Incidental Findings in Human Subjects Research: Analysis and Recommendations. Journal of Law, Medicine & Ethics. 2008;36(2):219–248. doi: 10.1111/j.1748-720X.2008.00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Illes J, et al. Ethical Consideration of Incidental Findings on Adult Brain MRI in Research. Neurology. 2004;62(6):888–890. doi: 10.1212/01.wnl.0000118531.90418.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daniel Pine, personal communication with author, 2006.
- 7.Sobotka S, Lawrenz F. Empirical Analysis of Current Approaches to Incidental Findings. Journal of Law, Medicine & Ethics. 2008;36(2):249–255. doi: 10.1111/j.1748-720X.2008.00267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The author recently had a grant funded by the NIH where the study section reviewing the grant required that all MRIs be read by a neuroradiologist before a notice of grant award was made.