Abstract
Background:
Much of the current evidence regarding timely access to healthcare services focuses on the duration of the waiting time as the principal determinant of wait time acceptability. We conducted the first national-level analysis of wait time acceptability in Canada to identify the determinants of unacceptable waits for specialized healthcare services, including selected demographic and socio-economic variables.
Methods:
We analyzed data reported by respondents to a national survey on access to healthcare services who accessed specialized services (i.e., specialist visits, non-emergency surgery and selected diagnostic tests) during a 12-month period. We used univariate analyses and weighted logistic regression to examine the relation between wait time acceptability and selected demographic, socio-economic and health status factors for each specialized service.
Results:
Between 17% and 29% of patients who waited for a specialized service declared that their waiting time was unacceptable. Most individuals reported waiting less than 3 months for their services. Between 10% and 19% of those who waited indicated that waiting for care affected their lives. Results of the logistic regression analyses showed that longer waits and adverse experiences during the waiting period were significantly associated with higher odds of reporting an unacceptable waiting time for all three types of specialized services. The role of socio-economic and demographic factors on wait time acceptability was varied. Individuals with lower education were consistently less likely to consider their waiting times unacceptable. Patients less than 65 years of age were more likely to consider their waiting times unacceptable for specialist visits and diagnostic tests.
Interpretation:
Our study shows that the primary determinants of waiting time acceptability are the length of the waiting time and the effects of waiting on the patient’s life. In addition, some patient characteristics, such as age and education, may play a role, pointing to the potential role of patient expectations in determining the acceptability of waits for specialized services.
Abstract
Contexte :
Une bonne partie des preuves actuelles concernant l’accès en temps opportun aux services de santé met l’accent sur la durée de l’attente comme principal facteur déterminant de l’acceptabilité des temps d’attente. Nous avons effectué la toute première analyse d’envergure nationale de l’acceptabilité des temps d’attente au Canada afin de cerner les facteurs déterminants des temps d’attente inacceptables pour l’obtention de services de santé spécialisés, y compris des variables démographiques et socio-économiques sélectionnées.
Méthodes :
Nous avons analysé des données recueillies dans le cadre d’un sondage national sur l’accès aux services de santé auprès de répondants qui ont cherché à obtenir des services spécialisés (c.-à-d. consultation de spécialistes, chirurgies non urgentes et tests diagnostiques sélectionnés) sur une période de 12 mois. Nous avons utilisé des analyses univariées et une régression logique pondérée pour examiner la relation entre l’acceptabilité du temps d’attente et des facteurs démographiques, socio-économiques et de santé sélectionnés pour chaque service spécialisé.
Résultats :
Entre 17 % et 29 % des patients qui ont dû attendre pour recevoir un service spécialisé ont déclaré que le temps d’attente était inacceptable. La plupart des répondants ont dit avoir attendu moins de trois mois pour obtenir les services. Entre 10 % et 19 % de ceux qui ont attendu ont indiqué que l’attente a eu une incidence sur leur vie. Les résultats des analyses de régression logistique ont révélé que des temps d’attente plus longs et des expériences négatives pendant l’attente étaient associés de manière significative à une probabilité accrue de déclarer un temps d’attente inacceptable pour les trois types de services spécialisés. Les facteurs socio-économiques et démographiques n’ont joué qu’un rôle limité dans l’acceptabilité des temps d’attente. Les personnes ayant un niveau d’instruction moins élevé étaient constamment moins susceptibles de considérer leurs temps d’attente comme inacceptables. Les patients âgés de moins de 65 ans étaient plus susceptibles de considérer leurs temps d’attente pour consulter des spécialistes et obtenir des tests diagnostiques comme inacceptables.
Interprétation :
Notre étude montre que les principaux facteurs déterminants de l’acceptabilité des temps d’attente sont la durée de l’attente et les effets de cette dernière sur la vie du patient. Certaines caractéristiques des patients, telles que l’âge et le niveau d’instruction, peuvent également influer sur l’acceptabilité, ce qui laisse à penser que les attentes des patients jouent peut-être un rôle dans la détermination de l’acceptabilité des temps d’attente pour l’obtention de services spécialisés.
Waiting times for medical services such as specialist visits and surgery continue to be an issue in most countries with publicly funded healthcare systems, particularly in Canada, where timely access to healthcare services is at the top of the health policy agenda (Romanow 2002). In this country, long waits are routinely identified as the leading barrier to care (Sanmartin et al. 2002). Waiting for care, however, is only problematic when patients consider their waiting times unacceptable (Martin et al. 2003). To address the issue of unacceptable waits for care, it is important to understand the factors contributing to patients’ assessment of the acceptability of their waiting times.
Much of the evidence to date focuses on the duration of the waiting time as the principal determinant of wait time acceptability, often with little to no regard for other factors that may influence patients’ views on waiting times (Sanmartin 2001; Llewellyn-Thomas et al. 1998; Conner-Spady et al. 2004). In Ontario, Ho and colleagues (1994) asked patients who underwent knee replacement about the acceptability of their waiting times. Patients who considered their waiting times acceptable reported a median waiting time of 8 weeks from consultation to surgery as compared with the median of 32 weeks reported by those who considered their waits unacceptable (Ho et al. 1994). In a subsequent study, the duration of the wait was identified as a primary determinant of wait time acceptability (Coyte et al. 1994). A similar approach was used by Dunn and associates (1997) among cataract patients in Manitoba, where the majority of patients agreed that 3 months or less was a reasonable wait for surgery (Dunn et al. 1997).
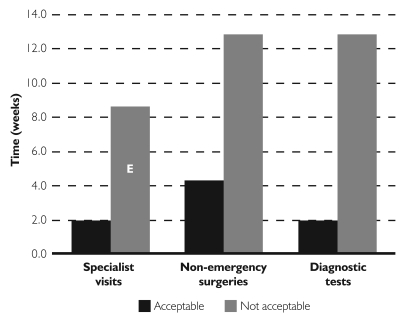
Recent results from a national study on access to care in Canada revealed that individuals who considered their waiting times unacceptable waited an average of between 9 weeks (for specialist visits) and 13 weeks (for non-emergency surgery) for specialized services, which was three to four times longer than the wait for those who did not consider their wait unacceptable (Figure 1). These individuals were also more likely to report that waiting for care affected their lives (Sanmartin et al. 2004).
FIGURE 1.
Median waiting times for specialized services by reported acceptability, Canada, 2003
Although current evidence provides some insight regarding patients’ experiences waiting for care, considerably less information exists about other factors that may affect wait time acceptability, such as patient demographics and socio-economic status. The purpose of this study, therefore, was to analyze national data on waiting for care to identify the key determinants associated with unacceptable waiting times. Specifically, the study focuses on three specialized services: specialist visits, non-emergency (or elective) surgery and diagnostic tests.
Methods
Data
This study is based on self-reported cross-sectional data collected in 2003 through the Health Services Access Survey (HSAS). The HSAS was designed to collect information regarding patients’ experiences accessing healthcare services, including waiting times and acceptability of waiting times. The HSAS was conducted by Statistics Canada as a supplement to the 2003 Canadian Community Health Survey (CCHS). The CCHS is a cross-sectional survey that gathers self-reported information on health status, healthcare use and health determinants for the Canadian population. The CCHS collects responses from persons aged 12 or older living in private households, excluding those living on Indian reserves and on Crown lands, residents of institutional dwellings, full-time members of the Canadian Armed Forces and residents of certain remote regions. More details regarding the CCHS have been documented elsewhere (Béland 2002). A subsample of CCHS respondents aged 15 and over from all 10 provinces were contacted (n=36,731) to participate in the HSAS. Telephone interviews were conducted between January and December 2003. The response rate was 87%, resulting in a final sample size of 32,005 (Béland 2002).
The study sample includes all persons who accessed one of the following specialized services in the 12 months before the survey: a specialist visit for a new illness or condition (n=3,616), elective surgery (n=1,911) or selected diagnostic tests such as MRI, CT scan or angiography (n=2,297). Respondents may have received more than one specialized service, and therefore would be represented in multiple groups. The services were received for a range of conditions, including cardiac disease, cancer, joint replacements, cataracts and other medical conditions. Respondents were asked for information about their experiences waiting for care, including (1) how long they waited for the specialized service, (2) whether the waiting time was acceptable (yes/no) and (3) whether waiting for care affected their lives (yes/no), and if so, how they were affected (e.g., worry, stress, anxiety, pain, etc.). The latter was an open-ended question with responses coded by the interviewer to a list of predetermined responses with an “other” category to capture additional information. The effects of waiting for care were categorized in the following groups: psychological effects (worry, stress and anxiety), physical effects (pain, activity limitation and deteriorating health status), effects on family and friends (worry, stress and increased dependency) and other effects (including loss of work and income).
Waiting time was defined as the time between the decision to treat (i.e., when the respondent and the physician decided the service was needed) and when the service was provided. Respondents could provide this information in terms of days, weeks or months. Waiting time data were converted to days and then grouped into the following categories: <1 month, 1–3 months, >3 months.
The HSAS data were linked to the CCHS data to obtain additional respondent information. The demographic and socio-economic information derived from the CCHS included age, sex, province of residence, rural or urban residence, education and income. Education information represents the highest level of education attained by the respondent, according to the following categories: less than secondary school graduation; secondary school graduation but no post-secondary education; some post-secondary education; and post-secondary degree or diploma. Income quartiles were calculated using total household income.
Health information was also obtained from the CCHS data. Respondents were asked to describe their overall general health status as excellent, very good, good, fair or poor. Responses were collapsed into three categories: fair/poor, good and excellent/very good health. As a more precise mobility measure, we included the concept of activity limitation. Individuals were asked whether or not they required assistance with a range of activities, such as preparing meals or shopping for groceries or other necessities, owing to health reasons.
Analysis
Descriptive statistics are used to provide information on the study population. We used multivariate logistic regression to examine the relation between wait time acceptability and a range of waiting time, demographic, socio-economic and health status factors. We developed regression models separately for each specialized service (i.e., specialist visits, non-emergency surgery and diagnostic tests). A broad range of conditions and procedures are represented within each service group. Within the non-emergency surgery group, for example, procedures include cancer-related surgery, cardiac surgery, hip and knee replacements and cataract surgery. Since the type of non-emergency surgery may also be related to other variables in the model, such as length of waiting time, age and sex, the models for specialist visits and diagnostic tests were adjusted for type of condition and the non-emergency surgery model was adjusted for type of procedure to remove potential confounding effects.
In order to obtain unbiased point estimates of the odds ratios, all regression analyses were weighted using standardized or normalized CCHS sampling weights, which account for such factors as unequal probability of selection. Further, the bootstrap technique was used to determine the significance of the odds ratios (ORs) and to estimate the 95% confidence intervals (CIs). This technique fully accounts for the design effects of the survey (Davison and Hinkley 1997).
Results
Respondent characteristics are presented in Table 1. The majority of individuals who accessed a specialized service were more likely to be between the ages of 35 and 64, have some post-secondary education and be in the upper-middle to highest income quartile. The majority of individuals waited less than 1 month for a specialist visit (48%) or diagnostic test (58%), whereas those who had non-emergency surgery were more likely to wait longer than 1 month. The proportion of individuals who reported that waiting for care affected their lives was 19% for specialist visits, 10% for non-emergency surgery and 14% for diagnostic tests. Between 60% and 72% of these individuals reported that they experienced worry, stress and anxiety (Table 2). Over half the patients whose lives were affected by waiting indicated that they experienced physical effects such as pain, problems with activities of daily living or deterioration of overall health. In some cases, waiting for care also affected respondents’ families and friends. Between 25% (for diagnostic tests) and 37% (for non-emergency surgery) of those whose lives were affected reported that their family and friends experienced stress and worry or that they became increasingly dependent on them.
TABLE 1.
Characteristics of patients accessing specialized healthcare services
| SPECIALIST VISITS (N=3,616) (%) |
ELECTIVE SURGERY (N=1,911) (%) |
DIAGNOSTIC TESTS (N=2,297) (%) |
|
|---|---|---|---|
| Waiting time unacceptable | |||
| Yes | 29.4 | 17.3 | 21.5 |
| No | 70.6 | 82.7 | 78.5 |
| Gender | |||
| Female | 60.2 | 56.5 | 51.7 |
| Male | 39.8 | 43.5 | 48.3 |
| Age group | |||
| <35 | 26.7 | 24.0 | 17.2 |
| 34–64 | 57.1 | 51.8 | 60.2 |
| 65+ | 16.2 | 24.2 | 22.6 |
| Region | |||
| East | 8.5 | 10.0 | 9.2 |
| Quebec | 20.2 | 16.9 | 19.3 |
| Ontario | 39.6 | 39.5 | 42.6 |
| West | 31.7 | 33.6 | 29.0 |
| Residence | |||
| Rural | 17.6 | 18.6 | 17.2 |
| Urban | 82.4 | 81.4 | 82.8 |
| Education | |||
| Less than high school | 16.5 | 20.9 | 20.6 |
| High school/some post-secondary | 24.7 | 28.3 | 27.1 |
| Post-secondary degree/diploma | 58.8 | 50.8 | 52.3 |
| Income | |||
| Lowest quartile | 5.6 | 8.9 | 8.5 |
| Lower-middle quartile | 16.0 | 16.5 | 18.0 |
| Upper-middle quartile | 32.5 | 29.1 | 30.1 |
| Highest quartile | 34.8 | 30.0 | 27.1 |
| Missing | 11.1 | 15.5 | 16.3 |
| Health status | |||
| Fair/poor | 18.0 | 18.4 | 27.3 |
| Good | 31.0 | 31.3 | 37.2 |
| Excellent/very good | 51.0 | 50.3 | 35.5 |
| Some restriction | |||
| Yes | 21.7 | 21.4 | 32.4 |
| No | 78.3 | 78.6 | 67.6 |
| Waiting time | |||
| <1 month | 47.9 | 17.4 | 57.5 |
| 1–3 months | 40.7 | 42.0 | 31.0 |
| >3 months | 11.4 | 40.6 | 11.5 |
| Waiting affected life | |||
| Yes | 18.5 | 9.8 | 14.0 |
| No | 81.5 | 90.2 | 86.0 |
TABLE 2.
Effects of waiting for care reported by patients whose lives were affected by waiting
| SPECIALIST VISITS (N=663) (%) |
ELECTIVE SURGERY (N=187) (%) |
DIAGNOSTIC TESTS (N=319) (%) |
|
|---|---|---|---|
| Psychological effects | 71.7 | 60.2 | 60.5 |
| Physical effects | 57.3 | 68.4 | 63.5 |
| Effects on family and friends | 30.6 | 36.7 | 25.1 |
| Other effects | 20.5 | 24.6 | 17.3 |
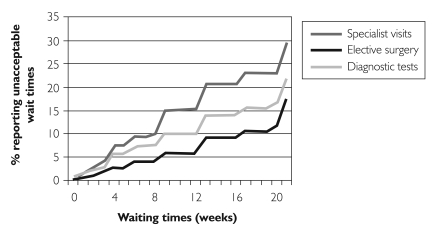
The proportion of individuals who considered their waiting times unacceptable was 29.4% for specialist visits, 17.3% for non-emergency surgery and 21.5% for diagnostic tests (Table 1). Unacceptable waits were reported at all waiting time periods, with the proportion increasing with longer waiting times (Figure 2). The cumulative distribution of patients reporting unacceptable waits varied across procedure groups. At 8 weeks, for example, the proportion of patients reporting unacceptable waiting times was 10% for specialist visits, 8% for diagnostic tests and 4% for non-emergency surgery.
FIGURE 2.
Cumulative distribution of unacceptable waiting times for each specialized service
Determinants of unacceptable waits
Results of the logistic regression analyses indicated that the waiting time and the effect of waiting on a person’s life were the most significant determinants of unacceptable waits (Table 3). Longer waits and adverse experiences during the waiting period were associated with higher odds of reporting an unacceptable waiting time for all three service types.
TABLE 3.
Results of multivariate logistic regressiona
| SPECIALIST VISITS (N=3,729) |
ELECTIVE SURGERY (N=1,957) |
DIAGNOSTIC TESTS (N=2,416) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||||
| Gender | |||||||||
| Female | 0.74 | 0.52 | 1.04 | 0.76 | 0.44 | 1.33 | 0.73 | 0.43 | 1.22 |
| Male | 1 | 1 | 1 | ||||||
| Age group | |||||||||
| <35 | 1.14 | 0.65 | 1.98 | 0.93 | 0.40 | 2.20 | 2.78* | 1.19 | 6.47 |
| 34–64 | 1.67* | 1.02 | 2.73 | 1.28 | 0.63 | 2.60 | 1.36 | 0.74 | 2.50 |
| 65+ | 1 | 1 | 1 | ||||||
| Region | |||||||||
| East | 0.76 | 0.50 | 1.16 | 1.03 | 0.54 | 1.97 | 0.66 | 0.39 | 1.10 |
| Quebec | 0.60* | 0.36 | 0.99 | 0.86 | 0.35 | 2.13 | 0.54 | 0.23 | 1.25 |
| Ontario | 0.97 | 0.65 | 1.44 | 0.57 | 0.31 | 1.05 | 0.48* | 0.27 | 0.86 |
| West | 1 | 1 | 1 | ||||||
| Residence | |||||||||
| Rural | 0.59* | 0.36 | 0.94 | 0.44* | 0.22 | 0.88 | 1.31 | 0.66 | 2.60 |
| Urban | 1 | 1 | 1 | ||||||
| Education | |||||||||
| Less than high school | 0.55* | 0.32 | 0.94 | 0.39* | 0.20 | 0.77 | 0.47* | 0.26 | 0.85 |
| High school/some post-secondary | 0.93 | 0.62 | 1.37 | 0.83 | 0.46 | 1.49 | 0.64 | 0.35 | 1.15 |
| Post-secondary degree/diploma | 1 | 1 | 1 | ||||||
| Income | |||||||||
| Lowest quartile | 0.85 | 0.43 | 1.67 | 0.85 | 0.32 | 2.23 | 1.32 | 0.62 | 2.82 |
| Lower-middle quartile | 0.92 | 0.48 | 1.74 | 0.54 | 0.23 | 1.30 | 1.71 | 0.78 | 3.75 |
| Upper-middle quartile | 0.84 | 0.56 | 1.26 | 0.91 | 0.45 | 1.81 | 1.52 | 0.81 | 2.83 |
| Highest quartile | 1 | 1 | 1 | ||||||
| Health status | |||||||||
| Fair/poor | 1.05 | 0.65 | 1.70 | 1.69 | 0.81 | 3.56 | 0.97 | 0.47 | 2.01 |
| Good | 1.16 | 0.79 | 1.71 | 1.32 | 0.67 | 2.61 | 0.94 | 0.50 | 1.79 |
| Excellent/very good | 1 | 1 | 1 | ||||||
| Some restriction | |||||||||
| Yes | 1.08 | 0.68 | 1.68 | 1.32 | 0.65 | 2.65 | 1.33 | 0.78 | 2.26 |
| No | 1 | 1 | 1 | ||||||
| Waiting time | |||||||||
| <1 month | 1 | 1 | 1 | ||||||
| 1–3 months | 6.47* | 4.28 | 9.76 | 3.73* | 1.64 | 8.53 | 8.64* | 4.92 | 15.19 |
| >3 months | 33.14* | 18.79 | 58.46 | 20.22* | 8.53 | 47.93 | 27.29* | 11.14 | 66.83 |
| Waiting affected life | |||||||||
| Yes | 23.24* | 14.40 | 37.51 | 23.18* | 11.38 | 47.22 | 11.19* | 5.54 | 22.59 |
| No | 1 | 1 | 1 | ||||||
p>0.05
Models adjusted for type of condition
For each type of specialized service, there was a clear dose–response effect for waiting times, with the odds of reporting an unacceptable wait increasing with the length of the waiting time. Compared with patients who waited less than 1 month, the ORs for reporting an unacceptable wait among those who waited 1 to 3 months ranged from 3.7 (95% CI: 1.6, 8.5) for non-emergency surgery to 8.6 (95% CI: 4.9, 15.2) for diagnostic tests. Among those who waited more than 3 months, the ORs increased significantly ranging from 20.2 (95% CI: 8.5, 47.9) to 33.1 (95% CI: 18.8, 58.5) (Table 3).
Respondents who indicated that waiting for care affected their lives were more likely to report unacceptable waiting times than were unaffected respondents. The finding was consistent across all three types of services. The significant ORs ranged from 11.2 (95% CI: 5.5, 22.6) for diagnostic tests to 23.2 for both specialist visits (95% CI: 14.4, 37.5) and non-emergency surgery (95% CI: 11.4, 47.2) (Table 3).
Education was significantly associated with wait time acceptability. For all three types of specialized services, individuals with less than high school education were consistently less likely to consider their waits unacceptable compared with those who had completed post-secondary education. The ORs ranged from 0.39 (95% CI: 0.2, 0.77) for non-emergency surgery to 0.55 (95% CI: 0.3, 0.9) for specialist visits.
Overall, the associations between wait time acceptability and several demographic factors were limited and varied across the types of services considered. Respondents younger than 65 years of age were more likely to report unacceptable waits for specialist visits and diagnostic tests compared with those aged 65 and over; however, the results varied by procedure type. Among patients who accessed a specialist visit, those aged 35 to 64 years were more likely to report unacceptable waits (OR: 1.67; 95% CI: 1.02, 2.7). For diagnostic tests, patients younger than 35 years of age were more than 2.5 times more likely than were seniors to consider their waiting time unacceptable (OR: 2.8; 95% CI: 1.2, 6.5).
We noted some regional variations for two of the specialized service types. For specialist visits, residents of Quebec were less likely to consider their waiting time unacceptable (OR: 0.6; 95% CI: 0.4, 0.99) compared with those living in the western provinces. Individuals living in Ontario were half as likely to report unacceptable waits for diagnostic tests (OR: 0.5; 95% CI: 0.3, 0.9) compared with those living in western Canada. Similarly, individuals living in rural areas were significantly less likely to report unacceptable waits for specialist visits (OR: 0.6; 95% CI: 0.4, 0.9) and non-emergency surgery (OR: 0.4; 95% CI: 0.2, 0.9) compared with urban dwellers.
Interpretation
The initial descriptive component of this study yielded a number of informative findings. First, although the majority of respondents reported that they waited less than 3 months for specialized services, between 17% and 29% indicated that the waiting time was unacceptable. Patients who waited for non-emergency surgery appear to have a higher tolerance for waiting, with patients waiting for specialist visits and diagnostic tests being more likely to report unacceptable waits earlier in the waiting period. These differences are likely attributable to the fact that relative to those waiting for non-emergency surgery, patients anticipating diagnostic tests and specialist visits are more uncertain about their future health and need for treatment; in other words, non-emergency surgery patients are perhaps able to see more “light at the end of the tunnel.” Second, fewer than one in five patients reported that waiting for care affected their life, and the majority of these reported physical or psychological effects, or both. Psychological effects were predominantly reported by those who waited for a specialist visit. Similar to the point made above, this result was likely due to patients having to wait in a state of “not knowing” and experiencing the stress and anxiety of waiting for a diagnosis to be established.
A number of interesting results also emerged from the multivariate logistic regression models of wait time acceptability. These analyses clearly demonstrated that, in patients’ experiences of waiting for care, the length of time they waited and the effects of waiting were the primary determinants of waiting time acceptability. Although there were individuals in all waiting time categories who considered their waits for specialized services to be unacceptable, the odds of reporting an unacceptable wait increased with longer waits. Similar results were reported in a multivariate analysis of wait time acceptability among Swedish orthopaedic patients. Patients who waited longer were significantly more likely to consider their waiting times unacceptable (Lofvendahl et al. 2005).
The results of our study also indicate that patients whose lives were affected by waiting for care were significantly more likely than unaffected patients to consider their waits unacceptable. A substantial amount of prior research has shown that patients can experience a variety of adverse effects while waiting for care, including pain and limited mobility (Williams et al. 1997; Mahon et al. 2002; Hajat et al. 2002) as well as stress and anxiety (Jonsdottir and Baldursdottir 1998; Bengston et al. 1994), which often lead to dissatisfaction with the waiting experience. Our results contribute to this body of work, showing that the impact of waiting on patients’ lives is a salient predictor of wait time acceptability. Therefore, these findings further highlight for policy makers the potential attitudinal consequences of negative experiences while waiting for care, as well as suggest areas for possible improvement in service delivery, such as the development of strategies aimed at alleviating any mental and physical burden encountered while waiting.
Our results also point to the role of demographic and socio-economic factors, namely age and education, in patients’ determination of wait time acceptability. Individuals with less than high school education were consistently less likely to report unacceptable waits for all three types of specialized services, as were those older than 65 years of age who waited for specialist visits and diagnostic tests. In general, older patients and those with lower levels of education are less likely to be dissatisfied with their healthcare services compared with younger or more highly educated patients (Sitzia and Wood 1997). The results of our study confirm that they are also less likely to consider their waits unacceptable. This finding may be due to an overall higher level of satisfaction with healthcare services in general, or more specifically, it may be the result of differing expectations regarding how long patients ought to wait for care.
Patient expectations regarding service provision is a key determinant of satisfaction with the delivery of healthcare services and the timeliness of care (Thompson and Yarnold 1995). Patients who wait longer for care than they expect are less likely to be satisfied with the healthcare service (Levesque et al. 2000; Thompson et al. 1996). The role of patient expectations among those currently younger than 65 years of age will likely be increasingly important as this cohort ages, becoming the primary recipients of services such as joint replacements and cataract surgery, procedures that currently entail long wait times in Canada. Thus, monitoring attitudes towards wait time acceptability, specifically among this age group, will continue to be important.
Finally, the significant findings regarding patients’ place of residence highlight the potential role of contextual factors in an individual’s determination of unacceptable waiting times. Some evidence suggests that waiting times for specific types of specialized services vary across the country (Sanmartin 2003). Actual waiting times at the local or provincial level may influence an individual’s assessment of whether his or her waiting time was unacceptable. Thus, one possible objective of future research might be to determine the extent of patient knowledge regarding such “standards,” and following this, the degree to which patients actually use them as anchors or reference points when formulating judgments about their own waiting times.
Limitations
Some methodological limitations of the present work should be noted. Our study is based on self-reported waiting time data for individuals who completed their waiting period and received care. The data may be subject to recall bias because all respondents were asked about their experiences over the previous 12 months. Respondents were permitted to report the length of their wait in days, weeks or months, and our data suggest that their responses were subject to rounding. Furthermore, to ensure adequate sample sizes, we conducted analyses for each type of specialized service for a range of conditions. The results, therefore, are generalizable to the specialized services overall (e.g., non-emergency surgery) but may not reflect the same determinants for specific types of conditions (e.g., cardiac surgery, hip and knee replacement surgery).
Strengths
Despite these limitations, the current findings are encouraging from both a knowledge and a policy perspective. This study represents the first national-level analysis of wait time acceptability in Canada and is one of the few studies considering a broad range of potential factors affecting individuals’ views regarding the acceptability of their waiting times. Clearly, for some individuals, the length of time they have to wait for specialized services is unacceptable. Our results are consistent with much prior research focusing on length of waiting time as a key determinant of unacceptable waits for care; at the same time, they broaden understanding of additional determinants. The links between the duration and effects of waiting for care, education and wait time acceptability provide further insight regarding the importance of patients’ experiences waiting for care, as well as the role of patient expectations. Shedding more light on the determinants of unacceptable waiting times also increases the number of potential targets for policies aimed at minimizing the burden of waiting.
In addition to efforts directed solely towards reducing the length of waits, other types of strategies focusing on ameliorating the actual experience of waiting might be useful. For example, given the robust association found here between the effects of waiting and perceptions of wait time acceptability, interventions geared towards maintaining and improving the health-related quality of life of those waiting for medical services may be warranted.
Future studies
Further investigation is required to better understand the differential effects of the various determinants of wait time acceptability, specifically, the role of patient expectations. Such work may involve directly measuring patient expectations (and other closely related psychological constructs such as patient satisfaction), as well as examining a more complex system of causal pathways among the different determinants of unacceptable waiting times, to clarify the processes by which patients come to judge their waiting times as unacceptable. The results of such analyses could help in developing a more comprehensive and unified conceptual framework for guiding policy action on the waiting times issue in Canada and elsewhere.
Acknowledgment
This paper was funded by Statistics Canada.
Contributor Information
Claudia Sanmartin, Health Analysis and Measurement Group, Statistics Canada, Ottawa, ON.
Jean-Marie Berthelot, Canadian Institute for Health Information; Department of Epidemiology and Biostatics, McGill University.
Cameron N. Mcintosh, Health Analysis and Measurement Group, Statistics Canada, Ottawa, ON.
References
- Béland Y. Canadian Community Health Survey – Methodological Overview. Health Reports. 2002;13:9–14. [PubMed] [Google Scholar]
- Bengston A., Herlitz J., Karlsson T., Hjalmarson A. The Epidemiology of a Coronary Waiting List: A Description of All Patients. Journal of Internal Medicine. 1994;235:263–69. doi: 10.1111/j.1365-2796.1994.tb01070.x. [DOI] [PubMed] [Google Scholar]
- Conner-Spady B., Estey A., Arnett G., Ness K., McGurran J., Bear R., et al. Prioritization of Patients on Waiting Lists for Hip and Knee Replacement: Validation of a Priority Criteria Tool. International Journal of Technological Assessment in Health Care. 2004;20:509–15. doi: 10.1017/s0266462304001436. [DOI] [PubMed] [Google Scholar]
- Coyte P.C., Wright J.G., Hawker G.A., Bombardier C., Dittus R.S., Paul J.E., et al. Waiting Times for Knee-Replacement Surgery in the United States and Ontario. New England Journal of Medicine. 1994;331(16):1068–71. doi: 10.1056/NEJM199410203311607. [DOI] [PubMed] [Google Scholar]
- Davison A.C., Hinkley D.V. Bootstrap Methods and Their Application. Cambridge Series in Statistical and Probabilistic Mathematics. Cambridge, UK: Cambridge University Press; 1997. [Google Scholar]
- Dunn E., Black C., Alonso J., Norregaard J.C., Anderson G.F. Patients’ Acceptance of Waiting for Cataract Surgery: What Makes a Wait Too Long? Social Science and Medicine. 1997;44:1603–10. doi: 10.1016/s0277-9536(96)00251-1. [DOI] [PubMed] [Google Scholar]
- Hajat S., Fitzpatrick R., Morris R., Reeves B., Rigge M., Williams O., et al. Does Waiting for Total Hip Replacement Matter? Prospective Cohort Study. Journal of Health Services Research and Policy. 2002;7(1):19–25. doi: 10.1258/1355819021927638. [DOI] [PubMed] [Google Scholar]
- Ho E., Coyte P.C., Bombardier C., Hawker G., Wright J.G. Ontario Patients’ Acceptance of Waiting Times for Knee Replacements. Journal of Rheumatology. 1994;21:2101–5. [PubMed] [Google Scholar]
- Jonsdottir H., Baldursdottir L. The Experience of People Awaiting Coronary Artery Bypass Graft Surgery: The Icelandic Experience. Journal of Advanced Nursing. 1998;27:68–74. doi: 10.1046/j.1365-2648.1998.00497.x. [DOI] [PubMed] [Google Scholar]
- Levesque J., Bogoch E.R., Cooney B., Johnston B., Wright J.G. Improving Patient Satisfaction with Time Spent in an Orthopedic Outpatient Clinic. Canadian Journal of Surgery. 2000;43:431–36. [PMC free article] [PubMed] [Google Scholar]
- Llewellyn-Thomas H.A., Arshinoff R., Bell M., Williams J.I., Naylor C.D. In the Queue for Total Joint Replacement: Patients’ Perspectives on Waiting Times. Ontario Hip and Knee Replacement Project Team. Journal of Evaluative Clinical Practice. 1998;4:63–74. doi: 10.1046/j.1365-2753.1998.t01-1-00006.x. [DOI] [PubMed] [Google Scholar]
- Lofvendahl S., Eckerlund I., Hansag H., Malmqvist B., Resch S., Hanning M. Waiting for Orthopaedic Surgery: Factors Associated with Waiting Time and Patients’ Opinions. International Journal of Quality Health Care. 2005;17:133–40. doi: 10.1093/intqhc/mzi012. [DOI] [PubMed] [Google Scholar]
- Mahon J.L., Bourne R.B., Rorabeck C.H., Feeny D.H., Stitt L., Webster-Bogaert S. Health-Related Quality of Life and Mobility of Patients Awaiting Elective Total Hip Arthroplasty: A Prospective Study. Canadian Medical Association Journal. 2002;167(10):1115–21. [PMC free article] [PubMed] [Google Scholar]
- Martin R.M., Sterne J.A.C., Gunnell D., Ebrahim S., Smith G.D., Frankel S. NHS Waiting Lists and Evidence of National or Local Failure: Analysis of Health Service Data. British Medical Journal. 2003;326(7382):188. doi: 10.1136/bmj.326.7382.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romanow R.J. Building on Values: The Future of Health Care in Canada – Final Report. Ottawa: Commission on the Future of Health Care; 2002. [Google Scholar]
- Sanmartin C. Establishing Acceptable Waiting Times for Medical Services: A Review of the Evidence and Proposed Methods. Calgary: Western Canada Wait List Project; 2001. [Google Scholar]
- Sanmartin C., Gendron F., Berthelot J.M., Murphy K. Access to Health Care Services in Canada, 2003. Ottawa: Statistics Canada; 2004. Cat. no. 82-575-XIE. [Google Scholar]
- Sanmartin C., Houle C., Tremblay S., Berthelot M. Changes in Unmet Health Care Needs. Health Reports. 2002;13(3):15–21. [PubMed] [Google Scholar]
- Sitzia J., Wood N. Patient Satisfaction: A Review of Issues and Concepts. Social Science and Medicine. 1997;45:1829–43. doi: 10.1016/s0277-9536(97)00128-7. [DOI] [PubMed] [Google Scholar]
- Thompson D.A., Yarnold P.R. Relating Patient Satisfaction to Waiting Time Perceptions and Expectations: The Disconfirmation Paradigm. Academy of Emergency Medicine. 1995;2:1057–62. doi: 10.1111/j.1553-2712.1995.tb03150.x. [DOI] [PubMed] [Google Scholar]
- Thompson D.A., Yarnold P.R., Williams D.R., Adams S.L. Effects of Actual Waiting Time, Perceived Waiting Time, Information Delivery and Expressive Quality on Patient Satisfaction in the Emergency Department. Annals of Emergency Medicine. 1996;28:657–65. doi: 10.1016/s0196-0644(96)70090-2. [DOI] [PubMed] [Google Scholar]
- Williams J.I., Llewellyn-Thomas H., Arshinoff R., Young N., Naylor C.D. The Burden of Waiting for Hip and Knee Replacement in Ontario. Journal of Evaluative Clinical Practice. 1997;3:59–68. doi: 10.1111/j.1365-2753.1997.tb00068.x. [DOI] [PubMed] [Google Scholar]