Abstract
Background
Caring for a family member with dementia is extremely stressful, contributes to psychiatric and physical illness among caregivers, and increases the risk for caregiver death. Finding better ways to support family caregivers is a major public health challenge.
Objective
To test the effects of a structured multicomponent intervention on quality of life and clinical depression in caregivers and on rates of institutional placement of care recipients in 3 diverse racial or ethnic groups.
Design
Randomized, controlled trial.
Setting
In-home caregivers in 5 U.S. cities.
Participants
212 Hispanic or Latino, 219 white or Caucasian, and 211 black or African-American caregivers and their care recipients with Alzheimer disease or related disorders.
Intervention
Caregivers within each racial or ethnic group were randomly assigned to an intervention or to a control group. The intervention addressed caregiver depression, burden, self-care, and social support and care recipient problem behaviors through 12 in-home and telephone sessions over 6 months. Caregivers in the control group received 2 brief “check-in” telephone calls during the 6-month intervention.
Measurements
The primary outcome was a quality-of-life indicator comprising measures of 6-month caregiver depression, burden, self-care, and social support and care recipient problem behaviors. Secondary outcomes were caregiver clinical depression and institutional placement of the care recipient at 6 months.
Results
Hispanic or Latino and white or Caucasian caregivers in the intervention group experienced significantly greater improvement in quality of life than those in the control group (P < 0.001 and P = 0.037, respectively). Black or African-American spouse caregivers also improved significantly more (P = 0.003). Prevalence of clinical depression was lower among caregivers in the intervention group (12.6% vs. 22.7%; P = 0.001). There were no statistically significant differences in institutionalization at 6 months.
Limitations
The study used only a single 6-month follow-up assessment, combined heterogeneous cultures and ethnicities into a single group, and excluded some ethnic groups.
Conclusions
A structured multicomponent intervention adapted to individual risk profiles can increase the quality of life of ethnically diverse dementia caregivers.
Caring for a family member with dementia is extremely stressful, contributes to psychiatric and physical illness, and increases the risk for death (1, 2). The accumulating evidence on the personal, social, and health effects of dementia caregiving has generated a broad range of intervention studies, including randomized trials aimed at decreasing the burden and stress of caregiving. Several studies have demonstrated statistically significant effects in reducing caregiver burden, lowering caregiver depression, and delaying institutionalization of care recipients (1, 3, 4) through either targeted interventions that treat a specific caregiver problem, such as depression, or broad-based multicomponent interventions that include counseling, case management, and telephone support. Persistent limitations of caregiver intervention research are the paucity of well-controlled randomized trials, the limited range of outcomes examined, small sample sizes and insufficient power, geographic limitations, inadequate racial or ethnic variation, and a scarcity of comprehensive multicomponent interventions (4). Indeed, none of the 41 randomized clinical trials published in the last 5 years met Consolidated Standards of Reporting Trials (CONSORT) recommendations for reporting randomized trials (5), and many have serious methodologic problems that call into question the reported findings (4).
To address these limitations, the National Institute on Aging and the National Institute of Nursing Research funded a multisite research program designed to develop and test an effective caregiver intervention: the Resources for Enhancing Alzheimer's Caregiver Health (REACH) study. We performed the study in 2 phases. In the first phase (REACH I), we tested several different interventions at 6 U.S. sites to identify the most promising approaches to decreasing caregiver burden and depression (6). Results from the study showed that active treatments were superior to control conditions in reducing caregiver burden and that active engagement in skills training statistically significantly reduced caregiver depression (7, 8). The existing literature and findings from REACH I helped guide the design of the REACH II intervention (7, 8). We based the REACH II study on the premise that caregivers can have problems in several areas at varying levels of intensity, and thus, interventions must be responsive to variations in needs among caregivers. The findings from REACH I also suggest that interventions that use active techniques, such as role-playing and interactive practice, are more effective at improving outcomes, such as depression symptoms, compared with more passive methods, such as providing information (7). We based the REACH II intervention on these assumptions and designed the intervention to maximize outcomes by systematically targeting several problem areas, tailored the intervention to respond to the needs of each individual, and actively engaged the caregiver in the intervention process. We hypothesized that participants assigned to the intervention would do better than those in the control group on several indicators of caregiver quality of life, including depression, burden, self-care, and social support and care recipient problem behaviors, and that these differences would be largest among Hispanic or Latino persons because they have lower access to support services (8). In additional analyses, we assessed the effects of treatment on rates of caregiver clinical depression and care recipient institutional placement, as well as the benefits derived from study participation.
Context
Providing care for patients with dementia can pose enormous burdens that may be eased with assistance and support. Needs may differ by race or ethnicity.
Contributions
The investigators randomly assigned Hispanic, black, and white dementia caregivers to receive written educational materials or an intensive intervention to improve caregiver quality of life. The specific interventions were determined by caregivers, were delivered via trained personnel and telephone support groups, and targeted several dimensions of need. The study found that quality of life improved for Hispanic and white caregivers and for black spousal caregivers in the intervention group but not in the control group. The intervention had no detectable effect on the number of care recipients who were institutionalized.
Cautions
The study used only a single 6-month follow-up assessment, combined heterogeneous cultures and ethnicities into 3 groups, and excluded some ethnicities.
Implications
An intensive intervention targeting several dimensions of caregiver need improved caregiver quality of life without an apparent effect on care recipient institutionalization. The effect did not differ by caregiver race or ethnicity.
—The Editors
Methods
Caregivers
Eligibility criteria for caregivers included the following: Hispanic or Latino, white or Caucasian, or black or African-American race or ethnicity; age 21 years or older; living with or sharing cooking facilities with the care recipient; providing care for a relative with diagnosed Alzheimer disease or related disorders for at least 4 hours per day for at least the past 6 months; and reported distress associated with caregiving (reported at least 2 of the following 6 items at baseline assessment: felt overwhelmed, felt like they often needed to cry, were angry or frustrated, felt they were cut off from family or friends, reported moderate to high levels of general stress, or felt their health had declined). We excluded caregivers who were involved in another caregiver intervention study, who had participated in REACH I, or who had an illness that would prevent 6 months of study participation. Other requirements were logistic, including having a telephone, planning to remain in the geographic area for at least 6 months, and competency in either English or Spanish (see Appendix Table 1, available at www.annals.org, for a detailed list of exclusions).
Care Recipients
To be eligible for the study, caregivers had to confirm that their relative had diagnosed Alzheimer disease or related disorders. In addition, we screened care recipients for a history of severe mental illness, head injury, Parkinson disease, or stroke, and we administered the Mini–Mental State Examination (MMSE) (9). We excluded patients who were bedbound with MMSE scores of 0 because we felt that our intervention had little to offer caregivers who were caring for such patients. Moreover, being bedbound is a risk factor for institutional placement or death, and we sought to exclude caregivers who were likely to transition out of the caregiving role within the 6-month study. For patients who scored more than 23 on the MMSE or had other conditions, such as head injury, we required a physician's diagnosis of Alzheimer disease or related disorders.
Procedures
We recruited caregiver and care recipient dyads at 5 sites: Birmingham, Alabama; Memphis, Tennessee; Miami, Florida; Palo Alto, California; and Philadelphia, Pennsylvania. Enrollment began in June 2002, and follow-up ended in August 2004. Recruitment occurred in memory disorder clinics, primary care clinics, social service agencies, physician offices, churches, and community centers and by using professionally designed brochures, public service announcements on radio stations, newspaper articles, television, targeted newsletters, and community presentations.
We translated all intervention materials and assessment instruments into Spanish for the Hispanic or Latino participants by using established techniques for forward-and-back translation and allowing for regional variation in language expression. We used bilingual and bicultural staff at the 3 sites that recruited Hispanic or Latino participants: Palo Alto, Philadelphia, and Miami. At all sites, assessors and interventionists received cultural sensitivity training and were certified before entering the field. Certified assessors were blinded to group assignment of study participants. The institutional review boards of all 5 site institutions and the coordinating center in Pittsburgh, Pennsylvania, approved the study. We obtained written informed consent from all caregivers and from care recipients whenever possible. Caregivers provided consent on behalf of care recipients who could not do so on their own.
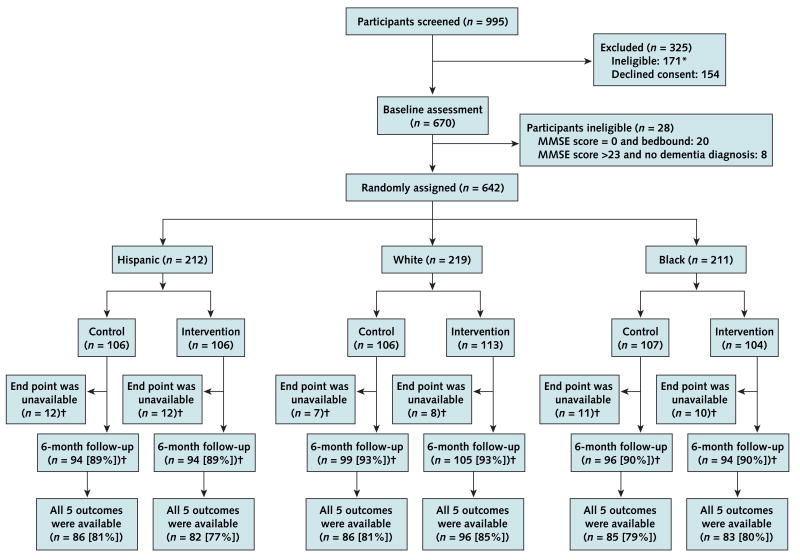
After telephone screening (n = 995) and baseline assessment (n = 670), we randomly assigned participants (n = 642) to the intervention or control group (Figure). We stratified randomization by using a block size of 2 or 4 within strata defined by the 5 intervention sites, 3 racial or ethnic groups (Hispanic or Latino, white or Caucasian, and black or African American), and 2 caregiver–care recipient relationships (spouse or nonspouse). We performed randomization at the coordinating center by using a computer-generated algorithm and a standard protocol for transmitting randomization information between the coordinating center and the study sites. We administered 1 of 3 follow-up batteries, on the basis of care recipient status at follow-up (full follow-up, bereavement battery, or placement battery), to study participants 6 months after randomization when the intervention was completed. To maximize the number of individuals who could be included in the outcome analyses, we ensured that the 3 batteries were as similar as possible. We did not ask caregivers about caregiver burden and care recipient functional status if their care recipients had died; thus, we could not include these caregivers in the primary outcome analysis (10).
Figure. Study flow diagram.
*See Appendix Table 1 (available at www.annals.org) for reasons for ineligibility.
†See Appendix Table 2 (available at www.annals.org) for reasons for unavailable end points and types of 6-month follow-up.
Trial Groups
Intervention
The intervention involved a range of strategies: provision of information, didactic instruction, role playing, problem solving, skills training, stress management techniques, and telephone support groups to reduce risk in the study's 5 target areas by providing caregivers with education, skills to manage troublesome care recipient behaviors, social support, cognitive strategies for reframing negative emotional responses, and strategies for enhancing healthy behaviors and managing stress (Table 1) (11). The intervention was available in English or Spanish, was delivered by certified interventionists with at least a bachelor's degree, occurred over 6 months, and included 12 sessions (9 in-home [1.5 hours each] sessions and 3 telephone [half hour each] sessions) and 5 structured telephone support group sessions. To facilitate the intervention, we supplied participants with resource notebooks with educational materials and telephones with display screens linked to a computer-integrated telephone system to provide information and facilitate group support conference calling. We emphasized the links among the material discussed during the intervention sessions, the features available on the computer-integrated telephone system, and the written educational materials provided to caregivers. The intervention sessions were temporally integrated, such that each session built on and included a review of the material discussed in the previous session.
Table 1. Overview of Intervention*.
| Target Area | Objective | Risk Assessment | Treatment Strategies or Techniques |
|---|---|---|---|
| Depression | Enhance caregiver emotional well-being and skills for mood management. | High risk was defined as a score >4 on the CES-D or responding “often” to 4 items on the RA instrument, indicating feeling depressed, sad, or angry or not having time for enjoyable activities. Moderate risk was defined as responding “sometimes” to these 4 items. | 1) Provide education about importance of pleasant events and emotional well-being (caregiver notebook); 2) teach and practice strategies for engaging in pleasant events; 3) teach and role-play strategies for mood management and use of thought record; 4) establish schedule of pleasant events. |
| Burden | Increase caregiver knowledge about consequences of stress and enhance caregiver skills and strategies for managing burden of care. | High risk was defined as responding “often” to 8 RA items, indicating stress or difficulty with caregiving tasks (e.g., get chores done, take care of care recipient toileting). Moderate risk was defined as responding “sometimes” to these RA items. | 1) Provide educational materials on safety, caregiving, and stress (caregiver notebook); 2) teach and practice 3 stress management techniques (breathing exercises, music, stretching exercises); 3) refer to stress management feature on computerized telephone system. |
| Self-care and healthy behaviors | Enhance caregiver physical well-being and self-care behaviors. | High risk was defined as responding “yes” to 3 RA items about missing physician appointments, weight loss, or decrease in physical activity; “no” to 9 items about routine check-ups (e.g., getting a flu shot, visiting a dentist); or “often” to 6 items about health problems, sleeping problems, or poor nutritional habits. Moderate risk was defined as responding “sometimes” to 6 items on health, sleeping, or eating problems. | 1) Provide educational materials on self-care and preventive health practices (health passport, caregiver notebook); 2) demonstrate and review use of health passport; 3) teach healthy behaviors (e.g., nutrition, remembering medical appointments, adhering to medication schedule; 4) refer to healthy living feature of computerized telephone system. |
| Social support | Enhance caregiver emotional and social support and support with caregiving activities. | High risk was defined as responding “never” to 3 RA items assessing the availability of someone to talk to about important decisions, to provide comfort, or to provide a break from care or “often” to 3 items, indicating difficulty obtaining instrumental support or feeling isolated from family or friends. Moderate risk was defined as responding “sometimes” to these items. | 1) Provide education about importance of social support (caregiver notebook); 2) teach how to access community resources; 3) practice role-play strategies to enhance communication with health care providers and family members; 4) reinforce participation in telephone support groups; 5) refer to resource guide and communication and respite features of computerized telephone system. |
| Problem behaviors | Enhance caregiver ability to manage ADL or instrumental ADL and behavioral problems. | High risk was defined as responding “very much” or “extremely” upset to any of the 25 memory, behavior, or mood problems listed on the RMBPC (i.e., ask same questions over and over, verbally aggressive, express feelings of hopelessness), regardless of frequency of occurrence. Moderate risk was defined as being “moderately” bothered by any of the 25 memory, behavior, or mood problems that occurred daily or 3 to 6 times per week. | 1) Provide educational materials on symptoms of dementia and managing behaviors (caregiver notebook); 2) engage in structured problem solving and brainstorming of strategies; 3) provide a written behavioral prescription that specifies step-by-step strategies to manage troublesome behaviors; 4) demonstrate and practice specific strategies using role-play; 5) refer to problem behavior feature of computerized telephone system. |
ADL = activities of daily living; CES-D = Center for Epidemiologic Studies Depression Scale; RA = risk assessment; RMBPC = Revised Memory and Behavior Problems Checklist.
Because of the variability inherent in the caregiving situation, the intervention allowed for tailoring to meet the specific needs of the individual. We based the tailoring of the intervention on individual risk profiles obtained from the baseline assessment. We used items that assessed depression, burden, physical health and health behaviors, social support, and knowledge to classify individuals who were at high or moderate risk within each category addressed by the intervention. High-risk status within a category triggered the most active treatment strategies and techniques within a target area. Table 1 shows the criteria for determining risk level.
We structured the initial 2 in-home sessions to orient participants to the study, educational materials, computer-integrated telephone system, and support group calls and to begin tailoring the intervention. We interactively reviewed the caregiver's concerns on the basis of the risk profile to identify particular problems to target during the intervention. We also reviewed basic information on the importance of self-care and taught techniques to improve healthy behaviors. Caregivers received a “health passport,” a booklet that provided reminder information about health maintenance activities (such as annual physical examinations) and a tool to record health information and health appointments for both themselves and the care recipients.
A goal of the remaining intervention visits was to develop the caregiver's ability to assess and manage care recipient problem behaviors and manage their own stress and emotional well-being. The interventionist and caregiver jointly engaged in a problem-solving process (including defining problems in specific and objective terms, translating problems into objective goals, and generating specific action-oriented steps to solve the problems) to find effective and workable solutions to problem behaviors identified (such as repeated questioning). The outcome of each problem-solving process was a written, structured behavioral prescription that outlined strategies for managing the targeted behavior problems that were responsive to the caregiver's needs but were concrete and realistic within the caregiver's situation. We reviewed the prescriptions with the caregiver and actively practiced the techniques, such as role-playing. In subsequent sessions, caregivers reported on their use of the behavioral strategies to allow modification of the prescription. We targeted a maximum of 3 jointly negotiated problems during the intervention.
We also integrated skills training for managing burden of care, emotional well-being, and social support into the sessions. We taught and actively practiced strategies to help caregivers reduce the burden of care (for example, taking a break from caregiving activities) and techniques for stress management, including breathing exercises, listening to music, and stretching exercises. Caregivers also received training and practice in mood management techniques and strategies for increasing involvement in pleasant events.
The social support component focused on helping caregivers receive support for decision making, managing caregiving tasks, and reducing problems with social isolation. We gave caregivers information on how to access community resources and instructed them about strategies or skills related to social support and communication. We designed the 5 telephone-based support group sessions to reinforce the information or training presented during the one-on-one intervention sessions and to provide caregivers with an opportunity to interact with other caregivers and express their feelings and concerns.
Control
We mailed caregivers in the control group a packet of educational materials and provided 2 brief (<15 minute) telephone “check-in” calls at 3 months and 5 months after randomization. The educational materials, which were available in English or Spanish, included basic information about dementia and Alzheimer disease, caregiving, safety, and community resources. We also invited caregivers to participate in a workshop on dementia and caregiving at the end of the study after the 6-month assessment.
Intervention Implementation
Interventionists received intensive training, including reading materials, structured role-play, and practice opportunities. Interventionists also submitted an audiotape of their first treatment session for review and received feedback from a monitoring committee, which included a representative from each site, and the coordinating center as part of the certification process. We monitored and maintained intervention implementation through weekly supervision meetings at each site and monthly conference call meetings that involved interventionists from all sites. Interventionists also submitted taped treatment sessions throughout the study, which the monitoring committee reviewed. In addition, a delivery assessment form was completed after each contact with a caregiver. The coordinating center and the monitoring committee reviewed these forms to ensure adherence to the intervention protocol.
Primary Outcome
The primary outcome comprised standardized differences between baseline and 6-month follow-up for each of 5 measures that were central to caregiver quality of life and were closely linked to components of the intervention. The measures have been widely used in caregiving studies, have been validated with diverse cultural groups, and are relatively brief (10). Improvements of 0.5 SD on these measures are considered clinically meaningful effects and represent the upper end of the distribution of effect sizes that are reported in the caregiver intervention literature (12, 13).
Depression
We used the 10-item version of the Center for Epidemiologic Studies Depression Scale (CES-D) (14, 15) to assess depression. We computed total depression scores by summing scores for all items (after recoding responses so that all scores are in the same direction). For each statement, respondents indicated how often they felt that way during the past week using a scale from 0 (rarely or never) to 3 (most or all of the time). Scores could range from 0 through 30, with higher scores indicating increased presence of depression symptoms. A score of 15 (equivalent to 30 on the full 20-item scale) reflects extremely high levels of depression symptoms, and we used this score as an alert value for reporting to the data safety monitoring board and for designating individuals with clinical depression (15, 16).
Caregiver Burden
We used the brief (12-item) version of the Zarit Caregiver Burden Interview (17, 18). However, because 1 of the questions was not appropriate for caregivers of persons who were institutionalized at the 6-month follow-up (that is, “Do you feel that you don't have as much privacy as you would like because of [care recipient's name]”?), we based caregiver burden on the sum of 11 questions (for example, “Feel stressed between caring for [the care recipient] and meeting other responsibilities?”). Caregivers rated each item on a 5-point scale from 0 (never) to 4 (nearly always), yielding a possible range of 0 to 44. Higher values indicated greater levels of caregiver burden.
Self-Care
We assessed the caregiver's diligence in looking after his or her own health by using 11 questions, such as whether he or she was getting enough rest when sick, seeing a physician when needed, and adhering to a medication schedule. We scored all items with 0 or 1 (no or yes), yielding a range from 0 to 11. Higher scores indicated increased attention to one's health and well-being.
Social Support
We assessed social support by using 10 items that assessed 3 domains of support: received support (3 items) (19, 20), satisfaction with support (3 items) (20, 21), and negative interactions or support (4 items) (20). All items required respondents to use a 4-point scale that ranged from 0 (never) to 3 (very often). We computed total social support scores by summing the scores for all items after recoding responses. Higher scores indicated increased social support for each item. Scores could range from 0 through 30, with higher scores indicating increased social support.
Problem Behaviors
We used 3 questions that assessed the primary domains of the Revised Memory and Behavior Problem Checklist (that is, memory, depression, and disruption) (22) to assess change in problem behaviors of care recipients at baseline and at follow-up. We scored responses on 5-point scales ranging from 1 (substantial improvement) to 5 (substantial decline). Thus, total scores for the 3 questions ranged from 3 to 15, with higher scores indicating greater decline.
Because higher scores indicated worse outcomes for the depression, caregiver burden, and problem behavior measures but better outcomes for the self-care and social support measures, we recoded the latter measures by subtracting the score from the maximum possible value for that measure. We obtained standardized values of the difference between baseline and follow-up by dividing the difference score for each participant by the common SD of that difference score across all participants.
Secondary Outcomes
Secondary outcomes were the prevalence of caregiver clinical depression and institutional placement of care recipients at 6-month follow-up. These measures are frequently used to assess the public health significance of caregiver interventions (23). Caregivers with scores of 15 or higher on the 10-item CES-D had symptoms that we judged to be at a level requiring clinical intervention (15, 16). We carefully coded institutionalization to include only cases in which the caregiver indicated that the patient was permanently institutionalized, and we confirmed that the patient was institutionalized at the final assessment point.
At the conclusion of the study, we asked all caregivers 7 questions about ways in which they benefited from participating in the study (for example, whether it helped improve the care recipient's life, keep the care recipient at home, and make the caregiver's life easier). The response options for each question were “not at all,” “some,” and “a great deal.”
Data Safety Monitoring
A data safety monitoring board, which was appointed by the National Institute on Aging and the National Institute of Nursing Research, monitored the study. Baseline safety alerts reported to the committee included high caregiver depression scores and care recipient safety issues (access to a gun or dangerous weapon, driving, repeatedly threatening to hurt himself or herself or others, and suicidal statements). We gave information and strategies about dealing with alerts identified at baseline to caregivers in both study groups. Additional potential adverse events throughout the 6-month intervention period were caregiver and care recipient deaths, hospitalizations, emergency department visits, severe medical problems, and care recipient institutionalization.
Statistical Analysis
For the primary outcome, we fitted generalized estimating equation (GEE) models with robust (sandwich) SEs and performed global tests to evaluate whether the intervention statistically significantly differed from the control, taking into account correlations among the outcome's 5 domains (24). We fitted models adjusted for caregiver–care recipient relationship (spouse or nonspouse) separately for each ethnicity or race group to reflect study design. We examined the interactions of intervention and the caregiver–care recipient relationship in an exploratory analysis for each racial or ethnic group. The models also included covariates for significant baseline differences between groups (P < 0.05 for education for Hispanic or Latino participants). Using this approach, we initially tested the assumption of a common effect of intervention for each measure (homogeneity) by using a score test on the standardized difference measures (24). We also used GEE models to examine whether an outcome statistically significantly changed within the control group alone. For all GEE analyses, we used an unstructured working correlation matrix.
We used simple and multiple linear regression to test for intervention effects on the changes (baseline to 6 months) within each domain separately. To assess clinical significance within domains, we used the criterion of 0.5-SD improvement from baseline to follow-up. This is consistent with our study design, which used 0.5 SD for sample size calculation, and represents the upper end of the distribution of effect sizes reported in the literature (12, 13). Within each racial or ethnic group and treatment group for each domain, we calculated the number of individuals who improved by at least 0.5 SD from baseline to follow-up and subtracted the number of individuals who worsened by at least 0.5 SD, yielding a net improvement score. Using the same strategy, we also calculated the number of different outcomes showing net improvement versus no change or decline by intervention and control condition within each racial or ethnic group. By using the bootstrap method (25), we estimated the 95% CIs of the differences in number (Δn) and percentage (Δ%) of participants between the groups. We used selection with equal probability and with replacement to create 1000 bootstrap samples, from which we obtained the 95% CIs based on the percentile of distributions of Δn and Δ%.
For the secondary outcomes of care recipient institutionalization and caregiver clinical depression (CES-D score ≥15), we calculated and compared proportions between treatment groups using exact tests for differences of proportions for each racial or ethnic group. We used Pearson chi-square tests to assess differences across racial or ethnic groups. We also used a logistic regression model to assess the relationship between treatment groups and 6-month clinical depression, controlling for baseline clinical depression for each racial or ethnic group. We assessed whether the benefits of participating in the study differed significantly between the intervention and control groups by using trend tests.
Sample Size and Power
The sample size for REACH II provided 80% power to detect an effect size of 0.50 (26) by using Student t-tests for comparing changes between baseline and 6 months in intervention groups. Because REACH II was designed as 3 separate studies (for white or Caucasian, black or African-American, and Hispanic or Latino participants), we calculated the sample size with a 2-sided α level of 0.0167, using a conservative Bonferroni adjustment. This yielded sample sizes of 170 caregivers in each study. We estimated that follow-up data would be unavailable for 15% of the sample, so we aimed to recruit 200 persons per racial or ethnic group. Note that the sample size required for the multivariate global test is no greater than the smallest size required for any corresponding univariate test (27–29).
Role of the Funding Sources
The National Institute on Aging and the National Institute of Nursing Research funded the study. Staff from the funding sources participated in the study design, implementation, and analyses and had a role in the decision to submit the manuscript for publication.
Results
Of the 995 caregivers screened, 171 (17%) were ineligible and 154 (15%) withheld consent. Of the remaining 670 who underwent a baseline assessment, 642 (96%) were randomly assigned (Figure).
Demographic Characteristics and Baseline Scores
Within each racial or ethnic group, caregivers in both groups had similar demographic and relationship characteristics at baseline, and care recipients in the 2 groups had similar demographic characteristics, functional and cognitive status, and problem behaviors (Table 2). Hispanic or Latino care recipients in the intervention group were significantly more likely to have been educated beyond high school (P = 0.024). We used this variable as a covariate in the primary outcome analysis for Hispanic or Latino caregivers.
Table 2. Caregiver and Care Recipient Characteristics by Ethnicity or Race and Treatment Group*.
| Variable | Hispanic or Latino | White or Caucasian | Black or African American | |||
|---|---|---|---|---|---|---|
| Control (n = 86) | Intervention (n = 82) | Control (n = 86) | Intervention (n = 96) | Control (n = 85) | Intervention (n = 83) | |
| Caregiver | ||||||
| Relationship to care recipient, n (%) | ||||||
| Spouse | 34 (39.5) | 36 (43.9) | 47 (54.7) | 57 (59.4) | 24 (28.2) | 26 (31.3) |
| Nonspouse | 52 (60.5) | 46 (56.1) | 39 (45.3) | 39 (40.6) | 61 (71.8) | 57 (68.7) |
| Child | 43 (82.7) | 41 (89.1) | 35 (89.7) | 36 (92.3) | 48 (78.7) | 43 (75.4) |
| Sibling | 6 (11.5) | 1 (2.2) | 2 (5.1) | 0 (0.0) | 0 (0.0) | 5 (8.8) |
| Other | 3 (5.8) | 4 (8.7) | 2 (5.1) | 3 (7.7) | 13 (21.3) | 9 (15.8) |
| Age, y | ||||||
| Mean (SD) | 59.0 (13.6) | 59.7 (14.3) | 63.2 (12.8) | 63.5 (11.7) | 57.1 (12.8) | 60.9 (12.9) |
| Median (IQR) | 61.9 (48–70) | 60.6 (50–69) | 63.2 (53–74) | 62.1 (55–72) | 55.0 (48–66) | 59.5 (51–71) |
| Men, n (%) | 14 (16.3) | 16 (19.5) | 16 (18.6) | 19 (19.8) | 10 (11.8) | 13(15.7) |
| Education, n (%) | ||||||
| <High school | 38 (44.2) | 28 (34.1) | 7 (8.1) | 10 (10.4) | 5 (5.9) | 9 (10.8) |
| High school | 19 (22.1) | 16 (19.5) | 15 (17.4) | 16 (16.7) | 30 (35.3) | 26 (31.3) |
| >High school | 29 (33.7) | 38 (46.3) | 64 (74.4) | 70 (72.9) | 50 (58.8) | 48 (57.8) |
| Marital status, n (%) | ||||||
| Married | 55 (64.0) | 51 (62.2) | 66 (76.7) | 82 (85.4) | 43 (50.6) | 53 (63.9) |
| Not married | 31 (36.0) | 31 (37.8) | 20 (23.3) | 14 (14.6) | 42 (49.4) | 30 (36.1) |
| Care recipient annual income, n (%) | ||||||
| <$20 000 | 49 (57.6) | 46 (58.2) | 7 (8.4) | 16 (17.4) | 31 (37.8) | 30 (39.0) |
| $20 000–$39 999 | 26 (30.6) | 19 (24.1) | 29 (34.9) | 26 (28.3) | 27 (32.9) | 26 (33.8) |
| ≥$40 000 | 10 (11.8) | 14 (17.7) | 47 (56.6) | 50 (54.3) | 24 (29.3) | 21 (27.3) |
| Years living with care recipient, y | ||||||
| Mean (SD) | 23.2 (21.2) | 24.0 (20.5) | 26.1 (22.5) | 25.8 (21.9) | 16.6 (20.1) | 18.5 (20.1) |
| Median (IQR) | 13.5 (3–42) | 19.0 (3–44) | 20.5 (4–44) | 23.0 (4–48) | 5.0 (2–33) | 7.0 (3–37) |
| Employed, n (%) | ||||||
| Full- or part-time | 24 (27.9) | 28 (34.1) | 28 (32.6) | 26 (27.1) | 35 (41.2) | 28 (33.7) |
| Retired | 23 (26.7) | 24 (29.3) | 42 (48.8) | 39 (40.6) | 24 (28.2) | 35 (42.2) |
| Unemployed | 39 (45.3) | 30 (36.6) | 16 (18.6) | 31 (32.3) | 26 (30.6) | 20 (24.1) |
| Care recipient | ||||||
| Age, y | ||||||
| Mean (SD) | 77.6 (9.9) | 77.9 (9.3) | 78.6 (9.3) | 77.5 (8.8) | 80.0 (8.5) | 80.8 (8.6) |
| Median (IQR) | 79.4 (71–84) | 78.3 (73–83) | 79.5 (75–84) | 79.0 (73–84) | 80.4 (73–85) | 82.1 (74–85) |
| Men, n (%) | 31 (36.0) | 28 (34.1) | 39 (45.3) | 52 (54.2) | 33 (38.8) | 26 (31.3) |
| Education, n (%) | ||||||
| <High school | 58 (69.9) | 59 (73.8) | 20 (23.8) | 29 (30.2) | 45 (56.3) | 41 (53.2) |
| High school | 16 (19.3) | 6 (7.5) | 24 (28.6) | 27 (28.1) | 12 (15.0) | 17 (22.1) |
| >High school | 9 (10.8) | 15 (18.8) | 40 (47.6) | 40 (41.7) | 23 (28.8) | 19 (24.7) |
| ADL limitations at baseline (range, 0–6) | ||||||
| Mean (SD) | 3.1 (2.2) | 3.6 (2.0) | 3.3 (2.0) | 3.1 (2.0) | 3.3 (2.0) | 3.3 (2.0) |
| Median (IQR) | 3.5 (1–5) | 4.0 (2–5) | 3.0 (1–5) | 3.0 (1–5) | 4.0 (1–5) | 4.0 (2–5) |
| Instrumental ADL limitations at baseline (range, 0–8) | ||||||
| Mean (SD) | 6.9 (1.6) | 6.9 (1.8) | 7.0 (1.6) | 6.8 (1.7) | 7.0 (1.4) | 6.6 (1.9) |
| Median (IQR) | 8.0 (6–8) | 8.0 (7–8) | 8.0 (7–8) | 7.0 (6–8) | 7.0 (6–8) | 7.0 (6–8) |
| MMSE score at baseline (range, 0–30) | ||||||
| Mean (SD) | 12.7 (7.4) | 11.1 (6.7) | 13.7 (8.0) | 15.3 (7.1) | 11.3 (6.8) | 12.7 (7.1) |
| Median (IQR) | 13.0 (7–19) | 10.0 (6–18) | 15.0 (6–20) | 15.0 (11–22) | 11.0 (6–16) | 14.0 (7–19) |
| RMBPC behavior frequency score at baseline (range, 0–72) | ||||||
| Mean (SD) | 22.3 (9.7) | 25.2 (11.1) | 23.9 (9.3) | 21.3 (8.8) | 20.7 (10.7) | 20.3 (9.7) |
| Median (IQR) | 21.0 (16–28) | 24.5 (18–32) | 23.5 (18–30) | 21.0 (15–28) | 19.8 (13–25) | 19.8 (13–28) |
Limited to those included in outcomes analysis. ADL = activities of daily living; IQR = interquartile range; MMSE = Mini-Mental State Examination; RMBPC = Revised Memory and Behavior Problem Checklist.
Treatment Implementation
Of the 323 caregivers who were randomly assigned to the intervention group, 60% completed all 12 sessions (9 in-home and 3 telephone sessions) and 5% did not complete any session (Appendix Table 3, available at www.annals.org). The treatment dose, measured in minutes of treatment time, did not statistically significantly differ among the racial or ethnic groups. In the control group, 90% of the 319 caregivers received both telephone contacts and 3% (4% Hispanic or Latino, 2% white or Caucasian, and 5% black or African American) did not receive either telephone contact. Following intention-to-treat principles, we included participants in the outcome analyses regardless of the level of exposure to treatment.
Primary Outcomes
We based primary outcome analyses on all participants with available data (see Appendix, available at www.annals.org, for details on nonresponders and missing data). Although tests for homogeneity indicated that the intervention effects were similar within each racial or ethnic group (P = 0.158 for Hispanic or Latino, P = 0.619 for white or Caucasian, and P = 0.862 for black or African American), we observed significantly greater improvements among Hispanic or Latino participants (coefficient, −0.3 [95% CI, −0.5 to −0.1]; P < 0.001) and white or Caucasian participants (coefficient, −0.2 [CI, −0.4 to 0.0]; P = 0.032) but not among black or African-American participants (coefficient, −0.1 [CI, −0.3 to 0.1]; P = 0.23) in the intervention group (Appendix Table 4, available at www.annals.org). In other words, the 5 outcomes improved 0.3 SD more in Hispanic or Latino participants and 2.0 more in white or Caucasian participants in the intervention group compared with those in the control group. Overall, participants in the control group also improved by approximately 0.1 SD. Adjustment for study site and baseline scores of the dependent variables did not affect the pattern of reported findings.
Exploratory analyses showed a significant interaction between caregiver–care recipient relationship and intervention among black or African-American participants (intervention × spouse interaction term, −0.5 [CI, −0.9 to −0.1]; P = 0.008). Spouses in the intervention group showed statistically significantly greater improvement than spouses in the control group (coefficient, −0.5 [CI, −0.8 to −0.1]). The intervention effect for nonspouses was not statistically significant. We found no other statistically significant effects for caregiver–care recipient relationship.
Table 3 shows the proportion of participants with clinically significant changes of 0.5 SD or more for each domain and all domains combined. Among Hispanic participants, net improvement across all 5 domains was greater in the intervention group than in the control group (45.1% vs. 6.9%; difference, 38.2% [CI, 11.2% to 64.4%]). Differences in net improvement between the groups favored the intervention for both depression and problem behaviors. Thirty-two of 82 participants in the intervention group lowered their depression scores by a clinically meaningful 2.6 points (SD, 0.5 [pooled across control and intervention groups]) compared with 0 of 86 participants in the control group. A reduction of 2.6 points is approximately equivalent to the individual changing from being at risk for clinical depression (CES-D score, 8) to being within the normative range (CES-D score, 5) for depression symptoms when at-risk status is used as the starting point. We found similar results for problem behavior score among intervention Hispanic or Latino participants whose net improvement was 31.7 percentage points. This indicates that 26 of 82 intervention caregivers experienced at least a 1.5-point net decrease in problem behaviors compared with 4 of 86 control caregivers who reported a net increase in problem behaviors (difference in net improvement, 36.3 percentage points [CI, 13.2 to 56.7 percentage points]). A change of 1.5 points in problem behavior score is approximately equivalent to the individual reporting substantial improvement versus minimal improvement or, alternatively, reporting minimal decline versus substantial decline. Among white persons, the overall difference in net improvement between the groups was 24.5 percentage points (CI, −3.4 to 51.6 percentage points). We found a clinically meaningful effect favoring the intervention for social support (difference in net improvement, 24.1 percentage points [CI, 3.0 to 46.4 percentage points]). We found no overall clinically significant effects for black or African-American persons; however, exploratory analysis of caregiver–care recipient relationship showed clinically meaningful differences that favored the intervention for black or African-American spouses when all domains were combined (difference in net improvement, 62.7 percentage points [CI, 17.6 to 109.9 percentage points]) and for 2 of the 5 domains (burden and self-care) (data not shown in Table 3).
Table 3. Summary of Clinically Significant Changes in Primary Outcome Measure*.
| Variable | Intervention | Control | Difference in Net Improvement‡ | |||||
|---|---|---|---|---|---|---|---|---|
| Improved, n (%) | Worsened, n (%) | Net Improvement, n (percentage points)† | Improved, n (%) | Worsened, n (%) | Net Improvement, n (percentage points)† | Δn (95% CI) | Δ% (95% CI) | |
| Hispanic or Latino (82 intervention; 86 control) | ||||||||
| Burden | 27 (32.9) | 14 (17.1) | 13 (15.8) | 30 (34.9) | 20 (23.3) | 10 (11.6) | 3 (−15 to 21) | 4.2 (−16.9 to 25.7) |
| Depression | 43 (52.4) | 11 (13.4) | 32 (39.0) | 24 (27.9) | 24 (27.9) | 0 (0.0) | 32 (12 to 49) | 39.0 (15.5 to 59.6) |
| Self-care | 29 (35.4) | 15 (18.3) | 14 (17.1) | 19 (22.1) | 15 (17.4) | 4 (4.7) | 10 (−8 to 29) | 12.4 (−8.7 to 35.0) |
| Social support | 38 (46.3) | 19 (23.2) | 19 (23.1) | 29 (33.7) | 19 (22.1) | 10 (11.6) | 9 (−11 to 28) | 11.5 (−12.3 to 34.2) |
| Problem behavior | 37 (45.1) | 11 (13.4) | 26 (31.7) | 20 (23.3) | 24 (27.9) | −4 (−4.6) | 30 (11 to 47) | 36.3 (13.2 to 56.7) |
| Across 5 domains§ | 56 (68.3) | 19 (23.2) | 37 (45.1) | 37 (43.0) | 31 (36.1) | 6 (6.9) | 31 (8 to 53) | 38.2 (11.2 to 64.4) |
| White or Caucasian (96 intervention; 86 control) | ||||||||
| Burden | 31 (32.3) | 22 (22.9) | 9 (9.4) | 25 (29.1) | 13 (15.1) | 12 (14.0) | −3 (−21 to 16) | −4.6 (−23.7 to 15.4) |
| Depression | 45 (46.9) | 18 (18.7) | 27 (28.2) | 36 (41.9) | 16 (18.6) | 20 (23.3) | 7 (−13 to 26) | 4.9 (−16.9 to 26.1) |
| Self-care | 42 (43.8) | 29 (30.2) | 13 (13.6) | 31 (36.1) | 31 (36.1) | 0 (0.0) | 13 (−9 to 36) | 13.6 (−10.4 to 39.0) |
| Social support | 40 (41.7) | 18 (18.8) | 22 (22.9) | 24 (27.9) | 25 (29.1) | −1 (−1.2) | 23 (4 to 43) | 24.1 (3.0 to 46.4) |
| Problem behavior | 31 (32.3) | 19 (19.8) | 12 (12.5) | 22 (25.6) | 23 (26.7) | −1 (−1.1) | 13 (−5 to 33) | 13.6 (−6.3 to 35.3) |
| Across 5 domains§ | 62 (64.6) | 24 (25.0) | 38 (39.6) | 41 (47.7) | 28 (32.6) | 13 (15.1) | 25 (0 to 49) | 24.5 (−3.4 to 51.6) |
| Black or African American (83 intervention; 85 control) | ||||||||
| Burden | 38 (45.8) | 12 (14.5) | 26 (31.3) | 28 (32.9) | 21 (24.7) | 7 (8.2) | 19 (0 to 38) | 23.1 (0.6 to 45.7) |
| Depression | 30 (36.1) | 12 (14.5) | 18 (21.6) | 24 (28.2) | 15 (17.7) | 9 (10.5) | 9 (−9 to 26) | 11.1 (−10.3 to 31.2) |
| Self-care | 36 (43.4) | 28 (33.7) | 8 (9.7) | 34 (40.0) | 28 (32.9) | 6 (7.1) | 2 (−20 to 24) | 2.6 (−23.6 to 26.6) |
| Social support | 36 (43.4) | 13 (15.7) | 23 (27.7) | 31 (36.5) | 19 (22.4) | 12 (14.1) | 11 (−7 to 29) | 13.6 (−8.1 to 34.8) |
| Problem behavior | 22 (26.5) | 27 (32.5) | −5 (−6.0) | 21 (24.7) | 23 (27.1) | −2 (−2.4) | −3 (−21 to 14) | −3.6 (−25.2 to 16.7) |
| Across 5 domains§ | 49 (59.0) | 26 (31.3) | 23 (27.7) | 40 (47.1) | 29 (34.1) | 11 (13.0) | 12 (−10, 34) | 14.7 (−11.3 to 40.9) |
Clinically significant improvement and worsening was defined as an unadjusted standardized change of ± 0.5 SD or more from baseline to follow-up.
Net improvement = participants who improved – participants who worsened.
Intervention group – control group. Δn = difference in number; Δ% = difference in percentage.
The participant improved when there were more improved domains than worsened domains (i.e., more domains improved >0.5 SD than worsened >0.5 SD). The participant worsened when there were less improved domains than worsened domains (i.e., fewer domains improved >0.5 SD than worsened >0.5 SD).
Secondary Outcomes
The overall prevalence of clinical depression at follow-up was significantly greater among caregivers in the control group than among those in the intervention group (22.7% vs. 12.6%; P = 0.001) (Table 4). The difference remained significant after adjustment for race or ethnicity and baseline clinical depression (odds ratio, 0.46 [CI, 0.28 to 0.76]; P = 0.002). Prevalence differed for white or Caucasian caregivers (24.5% [control] vs. 10.5% [intervention]; P = 0.008) but not for Hispanic or Latino caregivers (26.9% vs. 19.2%; P = 0.21) or black or African-American caregivers (16.8% vs. 8.5%; P = 0.086). Adjustment for baseline clinical depression did not qualitatively affect the within-group findings for white or Caucasian caregivers (odds ratio, 0.4 [CI, 0.2 to 1.0]; P = 0.045), Hispanic or Latino caregivers (odds ratio, 0.5 [CI, 0.2 to 1.2]; P = 0.129), or black or African-American caregivers (odds ratio, 0.4 [CI, 0.2 to 1.0]; P = 0.060).
Table 4. Clinical Depression of Caregivers and Institutional Placement of Care Recipients at 6-Month Follow-up*.
| Variable | Hispanic or Latino | White or Caucasian | Black or African American | Combined | ||||
|---|---|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | Control | Intervention | Control | Intervention | |
| Caregivers at follow-up, n | 94† | 94 | 99† | 105 | 96† | 94 | 289‡ | 293 |
| Caregivers with clinical depression at follow-up, n (%) | 25 (26.9) | 18 (19.2) | 24 (24.5) | 11 (10.5)§ | 16 (16.8) | 8 (8.5) | 65 (22.7) | 37 (12.6)‖ |
| Care recipient randomization, n | 106 | 106 | 106 | 113 | 107 | 104 | 319 | 323 |
| Care recipients institutionalized, n (%) | 6 (5.7) | 1 (0.9) | 13 (12.3) | 7 (6.2) | 4 (3.7) | 6 (5.8) | 23 (7.2) | 14 (4.3) |
Clinical depression was defined as a CES-D score ≥15, and care recipients were institutionalized permanently at last available assessment. CES-D = Center for Epidemiologic Studies Depression Scale.
1 participant was missing CES-D score.
3 participants were missing CES-D scores.
P = 0.008.
P = 0.0014.
The number of care recipients who were institutionalized did not differ statistically significantly between groups (7.2% [control] vs. 4.3% [intervention]; P = 0.118). Twenty of 37 institutionalized care recipients were white or Caucasian. An exact test indicated no significant differences between the groups for institutionalization within 6 months in any racial or ethnic group (P = 0.119 for Hispanic or Latino, P = 0.159 for white or Caucasian, and P = 0.53 for black or African American).
We found statistically significant treatment differences favoring the intervention group for all 7 items assessing the benefits of study participation (Appendix Table 5, available at www.annals.org).
Adverse Events
The only prespecified adverse event reported for the 642 caregivers at baseline was high levels of depression symptoms (n = 144 of 145 events). The most common care recipient events at baseline were suicidal thoughts (n = 56), access to a gun or dangerous weapon (n = 39), and driving (n = 37). During the intervention, the most common events among caregivers were evidence of high levels of depression symptoms (n = 93), hospitalization (n = 34), emergency department visits (n = 21), and severe medical problems (n = 14). Among care recipients, the most common events during the intervention were hospitalization (n = 111), death (n = 46), institutionalization (n = 45), suicidal thoughts (n = 32), emergency department visits (n = 27), driving (n = 22), access to a gun or dangerous weapon (n = 18), and severe medical problems (n = 13). No adverse event was attributed to the intervention.
Discussion
Family caregiving for patients with dementia is characterized by several challenges that seriously compromise the quality of life for millions of family members in the United States. We believe that our study is the first to systematically assess the efficacy for a multicomponent caregiver intervention compared with a control group in ethnically diverse populations. Compared with minimal support, a multicomponent intervention led to statistically significantly greater improvements in quality of life (as measured by indicators of depression, burden, social support, self-care, and patient problem behaviors) for white or Caucasian and Hispanic or Latino caregivers but not for black or African-American caregivers. We did observe, however, statistically significant quality-of-life changes for black or African-American spouse caregivers. Although the improvement in treatment conditions compared with control conditions on our multivariate outcome was modest (approximately 0.3 SD among Hispanic or Latino participants and 0.2 SD among white or Caucasian participants), we found clinically meaningful differences for specific components of our multivariate outcome. Among Hispanic or Latino persons, caregivers in the intervention group were more likely to report improvement in depression symptoms and problem behaviors. White or Caucasian caregivers in the intervention group reported higher levels of social support. We also found that the rate of clinical depression among caregivers in the intervention group was statistically significantly lower than that of the control group. Institutionalization of care recipients did not statistically significantly differ, although rates of placement were higher in the control group than in the intervention group. Caregivers in the intervention group reported that study participation helped them feel more confident in dealing with the care recipient, made life easier for them, improved their ability to care for the care recipient, improved the care recipient's life, and helped them keep the care recipient at home. Of note, many participants in the control group reported that they benefited “some” or “a great deal” from participating in the study, suggesting that even minimal support and attention may have positive effects on caregivers.
Our study has several limitations. First, we had only 1 follow-up assessment available, which makes the long-term effect of the intervention difficult to assess. Assessing the effects of the intervention on institutional placement, for example, typically requires follow-up of 1 year or longer. Second, although our study is unusual in that we included many ethnic minorities, all 3 ethnic or racial groups are quite heterogeneous. For example, the Hispanic or Latino sample includes both Mexican-American and Cuban-American persons—2 groups with very different cultural backgrounds. Other minority groups, such as Asian-American persons, were left out altogether. Finally, some researchers might question our choice of the control condition. The most appropriate control condition for the type of intervention that we used is under considerable debate. Options include treatment as usual, minimal support, or attention control. For ethical reasons and to motivate control participants to remain in the study, we offered participants something minimal but meaningful, and we thus opted for a minimal support control condition in which caregivers received basic written educational material and 2 brief telephone calls. We had also considered an attention control condition that would engage participants in an activity unrelated to the goals of the intervention but decided against this because we could not identify an activity that would be both meaningful and distinct from the intervention.
Making the intervention available in Spanish for Hispanic or Latino caregivers who may have had limited access to community resources probably contributed to the relatively larger effects obtained for this group. We designed the intervention to be culturally sensitive, flexible, and modularized to facilitate easy transfer to applied settings. Inasmuch as many of the health-related problems of late life present several interrelated challenges, this approach to intervention may also be effective in other contexts and could be useful in reducing physical and mental health disparities among individuals from different cultural groups (30).
The materials and protocols developed for our study can feasibly be adapted for widescale implementation in community settings. Learning the intervention requires approximately 80 hours of training, and it can be delivered by an individual with a bachelor's degree in psychology, social work, nursing, occupational therapy, or other related disciplines. Future research should focus on ways in which multicomponent interventions, such as REACH II, can be implemented at the community level within the existing health and aging services networks.
Because of their frequent contact with patients with dementia and their family members, health professionals are in a unique position to identify family members whose quality of life has been seriously compromised by caregiving demands. Future availability of community-based intervention services modeled after the REACH II intervention would be a valuable referral resource for family caregivers. Although multifaceted programs are currently not available, referral to community resources, such as local area agencies on aging or the Alzheimer's Association, may be beneficial to some caregivers.
Supplementary Material
Acknowledgments
Grant Support: In part by the National Institute on Aging and the National Institute of Nursing Research (AG13305, AG13289, AG13313, AG20277, AG13265, and NR004261).
Footnotes
Note: A detailed description of the REACH II study design, methods, assessment instruments, and original de-identified data are available to the public at the National Archive of Computerized Data on Aging (http://webapp.icpsr.umich.edu/cocoon/NACDA-Study/04354.xml). The Study Manual of Operations, which contains detailed information about the intervention, including resource and training materials, is also available at www.edc.pitt.edu/reach2/public/manuals.html.
Potential Financial Conflicts of Interest: None disclosed.
References
- 1.Schulz R, Martire LM. Family caregiving of persons with dementia: prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004;12:240–9. PMID: 15126224. [PubMed] [Google Scholar]
- 2.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282:2215–9. doi: 10.1001/jama.282.23.2215. PMID: 10605972. [DOI] [PubMed] [Google Scholar]
- 3.Brodaty H, Green A, Koschera A. Meta-analysis of psychosocial interventions for caregivers of people with dementia. J Am Geriatr Soc. 2003;51:657–64. doi: 10.1034/j.1600-0579.2003.00210.x. PMID: 12752841. [DOI] [PubMed] [Google Scholar]
- 4.Schulz R, Martire LM, Klinger JN. Evidence-based caregiver interventions in geriatric psychiatry. Psychiatr Clin North Am. 2005;28:1007–38. doi: 10.1016/j.psc.2005.09.003. x. [PMID: 16325738] [DOI] [PubMed] [Google Scholar]
- 5.Moher D, Schulz KF, Altman D. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001;285:1987–91. doi: 10.1001/jama.285.15.1987. PMID: 11308435. [DOI] [PubMed] [Google Scholar]
- 6.Wisniewski SR, Belle SH, Coon DW, Marcus SM, Ory MG, Burgio LD, et al. The Resources for Enhancing Alzheimer's Caregiver Health (REACH): project design and baseline characteristics. Psychol Aging. 2003;18:375–84. doi: 10.1037/0882-7974.18.3.375. PMID: 14518801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belle SH, Czaja SJ, Schulz R, Zhang S, Burgio LD, Gitlin LN, et al. Using a new taxonomy to combine the uncombinable: integrating results across diverse interventions. Psychol Aging. 2003;18:396–405. doi: 10.1037/0882-7974.18.3.396. PMID: 14518803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gitlin LN, Belle SH, Burgio LD, Czaja SJ, Mahoney D, Gallagher-Thompson D, et al. Effect of multicomponent interventions on caregiver burden and depression: the REACH multisite initiative at 6-month follow-up. Psychol Aging. 2003;18:361–74. doi: 10.1037/0882-7974.18.3.361. PMID: 14518800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. PMID: 1202204. [DOI] [PubMed] [Google Scholar]
- 10.Ann Arbor: National Archive of Computerized Data; [7 September 2006]. National Archive of Computerized Data on Aging search holdings. Accessed at www.icpsr.umich.edu/NACDA/archive.html. [Google Scholar]
- 11.Pittsburgh, PA: University of Pittsburgh Epidemiology Data Center; [7 September 2006]. REACH II: Resources for Enhancing Alzheimer's Caregiver Health. Accessed at www.edc.pitt.edu/reach2/public. [Google Scholar]
- 12.Sörensen S, Pinquart M, Duberstein P. How effective are interventions with caregivers? An updated meta-analysis. Gerontologist. 2002;42:356–72. doi: 10.1093/geront/42.3.356. PMID: 12040138. [DOI] [PubMed] [Google Scholar]
- 13.Brodaty H, Green A, Koschera A. Meta-analysis of psychosocial interventions for caregivers of people with dementia. J Am Geriatr Soc. 2003;51:657–64. doi: 10.1034/j.1600-0579.2003.00210.x. PMID: 12752841. [DOI] [PubMed] [Google Scholar]
- 14.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 15.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Arch Intern Med. 1999;159:1701–4. doi: 10.1001/archinte.159.15.1701. PMID: 10448771. [DOI] [PubMed] [Google Scholar]
- 16.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10:77–84. PMID: 8037935. [PubMed] [Google Scholar]
- 17.Zarit SH, Orr NK, Zarit JM. The Hidden Victims of Alzheimer's Disease: Families under Stress. New York: New York Univ Pr; 1985. [Google Scholar]
- 18.Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, O'Donnell M. The Zarit Burden Interview: a new short version and screening version. Gerontologist. 2001;41:652–7. doi: 10.1093/geront/41.5.652. PMID: 11574710. [DOI] [PubMed] [Google Scholar]
- 19.Barrera M, Sandler I, Ramsay T. Preliminary development of a scale of social support: studies on college students. American Journal of Community Psychology. 1981;9:435–41. [Google Scholar]
- 20.Krause N. Negative interaction and satisfaction with social support among older adults. J Gerontol B Psychol Sci Soc Sci. 1995;50:P59–73. doi: 10.1093/geronb/50b.2.p59. PMID: 7757834. [DOI] [PubMed] [Google Scholar]
- 21.Krause N, Markides K. Measuring social support among older adults. Int J Aging Hum Dev. 1990;30:37–53. doi: 10.2190/CY26-XCKW-WY1V-VGK3. PMID: 2407665. [DOI] [PubMed] [Google Scholar]
- 22.Teri L, Truax P, Logsdon R, Uomoto J, Zarit S, Vitaliano PP. Assessment of behavioral problems in dementia: the revised memory and behavior problems checklist. Psychol Aging. 1992;7:622–31. doi: 10.1037//0882-7974.7.4.622. PMID: 1466831. [DOI] [PubMed] [Google Scholar]
- 23.Schulz R, O'Brien A, Czaja S, Ory M, Norris R, Martire LM, et al. Dementia caregiver intervention research: in search of clinical significance. Gerontologist. 2002;42:589–602. doi: 10.1093/geront/42.5.589. PMID: 12351794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bull SB. Regression models for multiple outcomes in large epidemiologic studies. Stat Med. 1998;17:2179–97. doi: 10.1002/(sici)1097-0258(19981015)17:19<2179::aid-sim921>3.0.co;2-l. PMID: 9802177. [DOI] [PubMed] [Google Scholar]
- 25.Davison AC, Hinkley DV. Bootstrap Methods and Their Application. Cambridge, United Kingdom: Cambridge Univ Pr; 1997. Cambridge Series in Statistical and Probabilistic Mathematics; No. 1. [Google Scholar]
- 26.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1987. [Google Scholar]
- 27.Tang DI, Gnecco C, Geller NL. Design of group sequential clinical trials with multiple end points. Journal of the American Statistical Association. 1989;84:776–9. [Google Scholar]
- 28.Diggle PJ, Liang K, Zeger SL. Analysis of Longitudinal Data. Oxford, United Kingdom: Oxford Univ Pr; 1994. Oxford Statistical Science Series; No. 13. [Google Scholar]
- 29.Jennison C, Turnbull BW. Group Sequential Methods with Applications to Clinical Trials. Boca Raton, FL: Chapman and Hall and CRC Pr; 1999. Multiple endpoints; pp. 299–316. [Google Scholar]
- 30.Whitfield KE, editor. Closing the Gap: Improving the Health of Minority Elders in the New Millennium. Washington, DC: Gerontological Society of America; 2004. [Google Scholar]
- 31.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–41. doi: 10.1111/j.1532-5415.1975.tb00927.x. PMID: 1159263. [DOI] [PubMed] [Google Scholar]
- 32.Schulz R, Mendelsohn AB, Haley WE, Mahoney D, Allen RS, Zhang S, et al. End-of-life care and the effects of bereavement on family caregivers of persons with dementia. N Engl J Med. 2003;349:1936–42. doi: 10.1056/NEJMsa035373. PMID: 14614169. [DOI] [PubMed] [Google Scholar]
- 33.Schulz R, Belle SH, Czaja SJ, McGinnis KA, Stevens A, Zhang S. Long-term care placement of dementia patients and caregiver health and well-being. JAMA. 2004;292:961–7. doi: 10.1001/jama.292.8.961. PMID: 15328328. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.