Abstract
Patients, policymakers, providers, payers, employers, and others have increasing interest in using personal health records (PHRs) to improve healthcare costs, quality, and efficiency. While organizations now invest millions of dollars in PHRs, the best PHR architectures, value propositions, and descriptions are not universally agreed upon. Despite widespread interest and activity, little PHR research has been done to date, and targeted research investment in PHRs appears inadequate. The authors reviewed the existing PHR specific literature (100 articles) and divided the articles into seven categories, of which four in particular—evaluation of PHR functions, adoption and attitudes of healthcare providers and patients towards PHRs, PHR related privacy and security, and PHR architecture—present important research opportunities. We also briefly discuss other research related to PHRs, PHR research funding sources, and PHR business models. We believe that additional PHR research can increase the likelihood that future PHR system deployments will beneficially impact healthcare costs, quality, and efficiency.
Introduction
Today, an estimated 70 million people in the US have access to some form of personal health record (PHR). Such access in many cases comes through patients' health insurers or healthcare providing institutions, even though most patients may not be aware of it. 1 Patient surveys suggest that patients want to use PHRs and believe that they will be valuable. One survey found that about 75 percent of Americans report they would communicate electronically with their physicians if given the means to do so, 1 while another study found that 60 percent of patients said they would look up test results and track medication use through PHRs if these records were available. 2
Many healthcare information technology vendors and healthcare providers already have the tools available to offer PHRs to their customers and patients. For example, an estimated 50 million patients see healthcare providers who use the EPIC EHR (Electronic Health Record) software system, which includes a tethered PHR product. The EPIC “MyChart” application provides a Web-based portal that allows patients access to a variety of PHR functions, such as reviewing test results and scheduling appointments. The Department of Veterans Affairs (VA), with its approximately 25 million veterans, has a Web-based PHR called MyHealtheVet, which allows US veterans to obtain authoritative health information, link to federal and VA benefits and resources, access a personal health journal and request prescription refills online. 3 A number of health plans and employers also offer or are planning to offer PHRs to their members and employees in the near future. For example, the Blue Cross and Blue Shield Association has teamed up with American's Health Insurance Plans to offer a PHR to the more than 200 million members covered by these organizations by the end of 2008. 4 In the Dossia project, launched in 2006, large employers Intel, Wal-Mart, Applied Materials, British Petroleum, Pitney Bowes, and others, have committed millions of dollars to create a web-based framework that will supply over 5 million of their employees with access to personal health data through a common open-source architecture framework. 5 In the second half of 2007, Microsoft© debuted HealthVault™ which allows anyone with internet access the ability to search for health information, store their own health information, and upload their health information from home health devices. 6
Interest and investment in PHRs can have multiple motivations. Some organizations have implemented PHRs to try to create “stickier” relationships with their patients or enrollees through improved patient satisfaction, 7 while others may be motivated by goals of efficiency, increased patient empowerment, or improved disease management. 8 Almost all the investments in PHRs have focused on product development and implementation, and not on evaluation or research, as demonstrated by the low publication rate in this field. Ultimately, PHRs will succeed if patients use them enough and they provide some combination of improved quality, increased safety, enhanced efficiency, and/or better patient satisfaction both for acute and chronic conditions, along with a reasonable ease of use. These attributes are valued by various healthcare constituencies—patients, providers, payers, employers, and others—and may generate healthcare cost savings to some or all of these parties. The PHRs might conceivably achieve widespread acceptance and use if patients demand and employ them even, if the PHRs do not deliver measurable value. However, under such circumstances, patients might have to pay for PHRs directly. In any case, we believe the lack of evaluation and the current rudimentary understanding of how PHRs can specifically contribute to healthcare quality, safety, efficiency, and patient satisfaction threatens the viability and sustainability of these systems.
In this paper, we propose a research agenda for PHRs, in the same spirit as past frameworks for other areas of clinical informatics. 9,10 If carried out, the suggested research agenda could provide important insights that would increase the likelihood that PHR implementation will lead to better, more efficient healthcare, and improve patient outcomes.
PHR Description
One of the challenges in delineating a PHR research agenda is the absence of a consistent description of what a PHR actually entails. Although many descriptions and definitions exist, for our purposes, we have used a relatively broad description, put forward by the Markle Foundation. A PHR is:
“a set of computer-based tools that allow people to access and coordinate their lifelong health information and make appropriate parts of it available to those who need it”. 2
We recognize that the Markle Foundation description is one of many PHR descriptions, that many definitions are evolving, and that the dominant future PHR description remains unknown. 11
Existing PHR Research
To assess the published research focused on PHRs, we performed a PubMed search of the terms “personal health records” and “PHRs” from 1950 through 2007 and found 100 unique citations related to PHRs. By comparison, an equivalent PubMed search under the terms “clinical decision support” yielded 17,396 citations and under the term “asthma” yielded over 100,000 citations.
We reviewed each of the 100 citations and grouped the citations into seven main categories (▶). Overall, 10% fell into more than one category. Most of the citations fell roughly equally into the PHR adoption and attitudes, PHR function evaluation, and PHR position statements/editorials categories. Of the seven categories, four appear to offer significant research opportunities:
• PHR Function Evaluation
• PHR Adoption and Attitudes
• PHR Privacy and Security
• PHR Architecture
Table 1.
Table 1 Categorization of Existing PHR PubMed Citations
| Category | # of References | % ∗ |
|---|---|---|
| PHR Adoption and Attitudes | 16 (18, 19, 22, 25, 27, 33–43) (44–47) | 24% |
| PHR Architecture | 2 (27, 48, 49) | 3% |
| PHR Function Description (without evaluation) | 4 (13, 22, 44, 50, 51) | 6% |
| PHR Function Evaluation | 15 (12, 14–17, 36, 39, 40, 52–59) | 22% |
| PHR Position Statement/Editorials | 19 (34, 46, 47, 58, 60–96) | 28% |
| PHR Privacy and Security | 8 (26, 97–105) | 12% |
| Other | 10 (106–133) | 15% |
∗ - 10% fell into more then one category.
Approximately 60% (24 of 41) of the citations in these four categories included original primary research (▶).
Table 2.
Table 2 Categorization of Primary Research PHR PubMed Citations
| Category | # of References | % |
|---|---|---|
| PHR Function Evaluation | 10 (12, 14, 15, 17, 36, 39, 40, 52–55, 59) | 8% |
| PHR Adoption and Attitudes | 13 (18, 19, 22, 25, 33, 35–41, 43, 45) | 19% |
| PHR Privacy and Security | 0 | 0% |
| PHR Architecture | 1 (48) | 1% |
PHR Function Evaluation
At this stage of development and deployment, PHR function evaluation may be the most important area of PHR research. Ultimately, PHR functions are likely to drive data, infrastructure, and interoperability requirements, as well as adoption.
The crucial areas for PHR research are better delineation of their functions and of their impact on care. Primary PHR functions fall into four general categories, based on use of information from the patient's perspective:
• Information Collection—PHR functions that help patients to enter their own health information and to retrieve their information from external sources.
• Information Sharing—PHR functions that allow patients to engage in one-way sharing of their health information with others.
• Information Exchange—PHR functions that allow patients to engage in two-way data exchange with others.
• Information Self-Management—PHR functions that allow patients to better manage their own health/healthcare. Examples of PHR functions in this category include those functions that allow patients to record, track, and edit information about their own health/healthcare, as well as obtain relevant patient oriented disease information and decision support.
Based on our literature review, most previous PHR research focused on the areas of information self-management and information exchange. In these areas, PHRs have the potential to dramatically improve the patient-provider relationship, enhance patient and shared decision making, and enable the healthcare system to evolve towards a more personalized medicine model through the integration of more individualized healthcare information in patient care. 12–17
Numerous research opportunities exist to evaluate each area of PHR functionality with respect to the outcomes of healthcare quality, safety, efficiency, cost, and patient and provider satisfaction. The impact of PHRs on care for patients with chronic conditions represents a particularly important research priority given the extremely high associated costs and the potential to improve quality and efficiency. Research should quantify the overall value derived from composite PHR systems—not just the value of individual functions or impact on individual patient-provider pairs.
PHR Adoption and Attitudes
Understanding and addressing attitudinal and physical adoption barriers among patients and healthcare providers represents an important key to achieving widespread implementation and use of PHRs. As noted earlier, patients have expressed willingness to use PHRs, at least for certain functions such as viewing test results and tracking medications. 2 Less information is available about provider attitudes toward PHRs. Nevertheless, some studies suggest that physicians may be more reticent to adopt PHRs than other health professionals, due to concerns about whether adoption of PHRs will create additional work that is not reimbursed. 18–21
Studies of adoption generally show relatively low adoption rates among patients who have been offered access to a PHR, which have typically been free to them. This might be unexpected, given the high reported desire for this technology by patients, but is perhaps not so surprising given the lack of use cases that demonstrate proven value and the lack of proven business models for PHRs. Studies also report low use among providers, 22 and routine, monthly use among patients is generally well below 10% of users who have access to a PHR. 23,24 While it is unclear what benchmarks for PHR use are appropriate, without substantiated PHR use cases for patients, providers, and other constituents, and business models that clearly articulate the value of PHR, PHR adoption will not reach its full potential.
A review of PHRs in cancer care concluded that, while patients welcome PHRs, they do not yet use them effectively. 16 These trends mirror research in paper based PHRs, which show high support for PHRs, but relatively low utilization. 25 This suggests that until PHRs provide valuable functions that improve care on some level, or in other ways promote “stickiness,” adoption rates will remain low.
Research on adoption and attitudes should focus on:
• specific populations, including the underserved, elderly, and patients with chronic illnesses, including what can be done to improve adoption in these populations and what reasonable adoption benchmarks may be, though these will likely vary by population.
• trends in adoption to determine when uptake might be approaching a tipping point.
• factors associated with attitudes, adoption, and use, ranging from basic usability testing to patient-level factors (i.e., age, education, health literacy, accessibility, etc.) to organizational factors (i.e., PHR from providers versus payers) to structural features (i.e., PHRs tied to an EHR versus free-standing PHRs).
• ways to improve provider attitudes toward PHRs, and
• barriers to the use of these systems by patients and providers.
PHR Privacy and Security
Patients' greatest concern about nearly every type of electronic healthcare applications, including PHRs, is security and privacy. Ninety-one percent of people report they are “very concerned” about the privacy and security of their personal health information. 2 While the Health Insurance Portability and Accountability Act (HIPAA) of 1996 outlines the legal protections for PHR privacy and security, it does not address all the issues involved, especially because HIPAA only applies to “covered entities” including health plans, healthcare clearinghouses, and healthcare providers. Organizations like Dossia, Microsoft©, and Google© are not covered entities. Potentially, PHRs (as with EHRs) could protect patient privacy and security in ways that are much more secure than traditional paper-based patient records, such as password protecting and audit tracking. On the other hand, the security provided by paper-based records existing in only a small number of physically accessible places makes the risk of multi-site unauthorized PHR access seem greater. Despite the potential technological privacy and security advantages of PHRs, the general public appears more concerned about these issues for electronic records then for paper-based records. This is not surprising, given a number of recent highly publicized thefts and inadvertent disclosures of personally identifiable electronic information.
Several important issues regarding PHR privacy and security need better evaluation. The first involves who controls sharing and accessing of the information in a PHR. This is critical when many organizations and individuals are sharing data within the PHR. For example, patients may include children or others who do not have legal control over their healthcare information in their PHR record, and patients may want to share their PHR with others not in healthcare. The privacy and security interoperability issues with PHRs have many parallels to privacy and security issues associated with regional health information organizations (RHIOs). Clear tradeoffs exist between privacy, security and access, even for patients.
A second concern is how to optimally design PHR systems in order to allow patients to maximize the security of their PHR. For example, patients may have difficulty remembering or finding their passwords when it is time to use them. If password recovery is too difficult, it may diminish use, while if it is too easy, it increases the likelihood of security breaches. A third related issue of who controls information in a PHR (privacy) and how it is controlled (security) is authentication methods which ensure both privacy and security yet in doing so do not present a major barrier to access. Authentication is vitally important both in terms of people accessing the PHR and data entering the PHR. Although robust authentication methods have been worked out in the financial services sector and other areas, it remains to be seen how well these models will work for PHRs.
PHR issues around control over sharing and access to PHR data present even more complex issues, especially considering a patient controlled PHR and patient proxies. For example, determining appropriate permissions for parents' accesses to their children's records, or for caregivers' access to mentally compromised patient's records, is extremely complex. The perception of PHR privacy and security (and data reliability) will depend on who is hosting the PHR. Many people may think of privacy and security issues differently for a PHR hosted by their provider than for one hosted by their employer, health insurer, or a for-profit corporation. Some PHR designs, such as hardware-based, “pocket” USB PHRs, appear to have inherent privacy and security issues of their own. 26 All of these issues around PHR privacy and security present opportunities for research.
PHR Architecture
As with many other types of health information technology, a PHR consists of three primary components—data, infrastructure, and applications. Data are the types and elements of information that are exchanged, analyzed, and stored by different information technologies. Examples of data include healthcare claims information, laboratory and imaging results, medication history, and lists of patients' medical problems. Infrastructure is the computing platform(s), usually software package(s), functions or websites, which exchange and process healthcare data. Lastly, applications are the capabilities and outputs of health information systems themselves, and are enabled through data and infrastructure. Applications include data exchange and transactional capabilities such as appointment scheduling and medication renewals; analytical capabilities such as patient decision support; and content delivery capabilities such as patient-oriented care guidelines or disease education materials. All three components are critical for effective health information systems and interoperability between health information systems also represents a critical issue. The PHR functions exist in the PHR infrastructure and applications and process data used in the PHR.
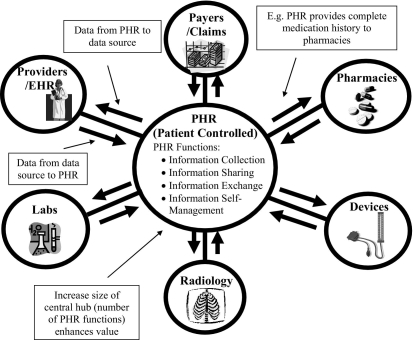
One paradigm for a PHR is to envision a PHR system as a hub and spoke model, with a patient-controlled PHR at the center connected to different stakeholders who exchange data and interact with patients (▶). In this paradigm, the PHR becomes more valuable the bigger the hub (i.e., the more functions the PHR has), the more spokes it has (i.e., the more connected it is to other sources of health information), and the thicker the spokes are (i.e., the more complete the sources of health information are).
Figure 1.
Idealized hub and spoke concept of a PHR system.
This PHR paradigm can be adapted to other PHR models. 27 For example, PHRs tethered to electronic health records (EHRs) might be considered in the hub and spoke model with just one thick spoke. A free standing PHR could be envisioned as a hub without any spokes. A claims-based PHR could have more data than a free standing PHR, but would be unlikely to have as much as a provider-tethered PHR linked to a patient's primary care provider. The relative advantages and disadvantages of different types of PHRs and how a complete hub and spoke PHR system would be developed vary depending on how specific patients receive care and have not been rigorously evaluated from a research perspective. Regardless of the PHR paradigm, as with other types of health information technology, interoperability represents a key component of PHR architecture. Many people see PHRs as an important catalyst toward achieving meaningful health information exchange. Even more so than with EHRs, if PHRs are to be viewed as central data repositories of a patient's data, then interoperability, both in terms of importing information into a PHR and exporting information from a PHR, is critical. The core importance of interoperability poses significant challenges and research opportunities, including assessment of the limitations of specific standards and data reliability.
Research evaluating the relative benefits and costs of different PHR architectural models represents a key research priority. In particular, it is important to determine the relative benefits of free-standing and third-party PHRs, EHR tethered (i.e., provider-tethered) PHRs, and claims or payer-based (i.e., payer-tethered) PHRs, depending on patient-specific circumstances. The value proposition for different PHR architectures may vary based on the type of healthcare delivery system in which a given patient and provider operate in. In addition, how well interoperability works with the various architectures should be examined.
Non-PHR Research Related to PHRs
Although the cumulative research literature on PHRs is modest, other areas of healthcare research may have direct applicability to PHRs. This research generally involves functions and features which were studied outside of a PHR, but which could be incorporated into a PHR. For example, one study showed that secure e-mail between patients and providers improved the ease and quality of communication. 28 Although this study did not use a PHR, email communication is a generally accepted function of many PHRs. Another study showed that computer-mediated medical histories taken directly from patients prior to visits save clinician's time collecting information about family history, personal history, prior immunizations and other important historical data, and may even improve patient candor about sensitive subjects, such as substance abuse and sexual behaviors. 29 Such data are directly applicable to PHRs because patient entered data represent an element in many PHRs. Although data from these studies may extend to PHRs, at least some of these results should be replicated in an actual PHR environment.
PHR Business Case
Another critical issue for PHR research, which must be assessed if PHRs are to be widely adopted, is the business cases for PHRs. Whoever the owner or at least the sponsor of the PHR is must have a valid business case to support it. Each constituency—patients, providers (physicians and non-physicians), payers, pharmacies, labs, etc.—must have sufficient incentives in order for them to be willing to participate in a PHR, either through direct use or data exchange.
For provider groups which develop PHRs, there must be sufficient revenue or other return on investment to justify implementing and providing support for the PHR. Third-party vendors such as Microsoft© and Google© may rely on advertising revenues to generate revenue; it is unclear in this structure what the incentives are for providers to participate, and how information from these PHRs will make its way back to providers. Insurers who develop or sponsor PHRs will have to be able to demonstrate sufficient return on their investment as well.
Overall, many of the incentives for PHRs do not seem well aligned. For example, non-visit care is not generally reimbursed, so strong incentives exist for providers to delay PHR implementation, even if they already have an EHR with PHR functionality. Patients are generally not yet incentivized to use any type of PHR. Legislation may be needed to help create the appropriate incentives, with one example being the proposed Personalized Health Information Act of 2007 (HR 1368) (http://www.govtrack.us/congress/bill.xpd?bill=h110-1368). Key questions include the value to a variety of stakeholders of PHR implementation, and the business case for PHR adoption and use. In considering reimbursement reform, policymakers need additional information about the benefits of non-visit care to determine how best to compensate providers for it.
Although current incentives are not well aligned, consumer demands and needs should also play a major role in the development of PHRs. Because patients are the ultimate end consumers of PHRs, broad demand from consumers could obviously have a dramatic effect on overall PHR adoption and use rates, although this has not occurred to date. For patients to have a significant motivation to adopt PHRs or even catalyze rapid PHR implementation throughout the U.S. health care system, patients must perceive that PHRs provide value to them in some qualitative or quantitative way.
Research Support
To date, private foundations, especially the Markle Foundation (http://www.markle.org/) and the Robert Wood Johnson Foundation (http://www.rwjf.org) have provided the majority of targeted funding for research into PHRs. These foundations have had specific initiatives and funds directed at PHR research. Government funding sources, including the National Library of Medicine, the Agency for Healthcare Research and Quality, and various National Institute of Health institutes have also provided some funding for research related to PHRs. These investigator initiated grants are generally not from PHR designated funds. These investigators compete for their PHR funding with all other investigator initiated grants to these funding sources.
In other clinical research areas, the typical sources of research support include governmental, commercial, and foundation support. Usually, governmental and commercial support constitute upwards of 90% of clinical research funding. 30 This is far from the case for PHRs. In order to ensure that more fundamental PHR research is conducted, both governmental and commercial sources of funding should increase their support of PHR research through programs that designate funds specifically for PHR research. Even though governmental spending on research has been flat, and despite the general woes of the economy, the high costs of healthcare represent a top priority, and PHRs represent one of the areas that should receive top priority for research given their potential for reducing costs and improving care. If funding cannot be increased, at least a portion of existing PHR funding should be directed into the areas highlighted above. Additionally, for PHRs that are already being developed, an evaluation component should be integrated into their development and results from that evaluation should be published and presented.
Several governmental organizations have identified PHRs as a growing priority for research. The National Library of Medicine in its 2006–2016 strategic plan identified PHRs and personal knowledge bases as one of its nine areas of strategic visions. 31 The American Health Informatics Community (AHIC) formed its Personalized Healthcare Workgroup in the fall of 2006, although it has focused primarily on other issues such as standards for genetic test reporting to date. 32 Hopefully, the increasing governmental interest in PHRs will result in increasing funding for PHR research.
Given the relative lack of clarity of many aspects related to PHRs outlined above, additional research investment is warranted to help maximize the return on the enormous investment currently being made into PHRs. This research on PHRs will be challenging, since PHRs have a broad range of functions and implementations, and any individual study may or may not be generalizable to other PHRs. However, today the evidence base about what key features a PHR needs to improve care and deliver value remains remarkably scanty. Because PHRs mostly involve software development costs, as opposed to hardware costs, if benefits are achieved, the returns on this research investment could be great.
Conclusions
We spend nearly $2 trillion annually in healthcare in the US with a high cost per person and an unacceptable variability in the quality of care. It is clear that PHRs have the potential, if designed appropriately and adopted widely, to reduce costs and simultaneously improve quality and safety of care. This potential has led to enormous public enthusiasm for PHRs and large investment. However, the existing knowledge base that underpins this work is surprisingly limited and most of the fundamental issues remain unresolved. For PHRs to realize their future potential, additional research is essential, but it is unlikely to be performed unless substantial additional financial support is committed to PHR research and evaluation, especially from federal and commercial sources. If these additional investments are not made, much time and money may be wasted and the potential value of PHRs will remain unrealized.
Footnotes
Dr. Middleton is a paid member of the US Advisory Board for Intercomponentware, Inc., a PHR vendor. The other authors have no financial or commercial relationships that may pose a conflict of interest.
References
- 1. Few Patients Use or Have Access to Online Services for Communicating with their Doctors, but Most Would Like to. 2006. Wall Street Journal/Harris Interactive.
- 2.The Personal Health Working Group: Markle Foundation 2003.
- 3. My HealtheVet—The Gateway to Veteran Health and Wellness. 2007http://www.myhealth.va.gov/ 2003. Accessed Dec 7, 2007.
- 4.Knowles F. Patients may store health records online 2006. Chicago Sun-Times. 2006 December 25.
- 5.Dossia. 2007http://www.dossia.org 2006. Accessed Dec 7, 2007.
- 6.HealthVault. 2007http://www.healthvault.com/ 2006. Accessed Dec 12, 2007.
- 7.Ralston JD, Carrell D, Reid R, Anderson M, Moran M, Hereford J. Patient web services integrated with a shared medical record: patient use and satisfaction J Am Med Inform Assoc 2007;14(6):798-806Nov–Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grant RW, Wald JS, Poon EG, et al. Design and implementation of a web-based patient portal linked to an ambulatory care electronic health record: patient gateway for diabetes collaborative care Diabetes Technol Ther 2006;8(5):576-586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahern DK, Kreslake JM, Phalen JM. What is eHealth (6): perspectives on the evolution of eHealth research J Med Internet Res 2006;8(1):e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Little DR, Zapp JA, Mullins HC, Zuckerman AE, Teasdale S, Johnson KB. Moving toward a United States strategic plan in primary care informatics: a White Paper of the Primary Care Informatics Working Group, American Medical Informatics Association Inform Prim Care 2003;11(2):89-94. [DOI] [PubMed] [Google Scholar]
- 11. Personalized Healthcare Detailed Use Case March 21, 2008.. 2008. Department of Health and Human Services. Office of the National Coordinator of Health Information Technology. http://www.hhs.gov/healthit/usecases/documents/PHCDetailed.pdf 2003. Accessed Apr 9, 2008.
- 12. Information prescriptions (Ix): bringing internet-based health content into the treatment process; patients to your site Internet Healthc Strateg 2005;7(4):4-8Apr. [PubMed] [Google Scholar]
- 13. New-age PHR comes with decision-support, multiple opportunities for DM Dis Manag Advis 2006;12(12):140-142Dec; 33. [PubMed] [Google Scholar]
- 14.Ayana M, Pound P, Lampe F, Ebrahim S. Improving stroke patients' care: a patient held record is not enough BMC Health Serv Res 2001;1(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cornbleet MA, Campbell P, Murray S, Stevenson M, Bond S. Patient-held records in cancer and palliative care: a randomized, prospective trialt Palliat Med 2002;16(3):205-212. [DOI] [PubMed] [Google Scholar]
- 16.Gysels M, Richardson A, Higginson IJ. Does the patient-held record improve continuity and related outcomes in cancer care: a systematic review Health Expect 2007;10(1):75-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang M, Lau C, Matsen 3rd FA, Kim Y. Personal health information management system and its application in referral management IEEE Trans Inf Technol Biomed 2004;8(3):287-297Sep. [DOI] [PubMed] [Google Scholar]
- 18.Jones R, McConville J, Mason D, Macpherson L, Naven L, McEwen J. Attitudes towards, and utility of, an integrated medical-dental patient-held record in primary care Br J Gen Pract 1999;49(442):368-373May. [PMC free article] [PubMed] [Google Scholar]
- 19.Ayana M, Pound P, Ebrahim S. The views of therapists on the use of a patient-held record in the care of stroke patients Clin Rehabil 1998;12(4):328-337Aug. [DOI] [PubMed] [Google Scholar]
- 20.Kittler AF, Carlson GL, Harris C, et al. Primary care physician attitudes towards using a secure web-based portal designed to facilitate electronic communication with patients Inform Prim Care 2004;12(3):129-138. [DOI] [PubMed] [Google Scholar]
- 21.Kittler AF, Wald JS, Volk LA, et al. The role of primary care non-physician clinic staff in e-mail communication with patients Int J Med Inform 2004;73(4):333-340May. [DOI] [PubMed] [Google Scholar]
- 22.Jeffs D, Harris M. The personal health record. Making it work better for general practitioners. Aust Fam Physician 1993;22(8):1417-1419Aug; 21, 24–7. [PubMed] [Google Scholar]
- 23. Group Health Presentation. Personal Health Records Conference 2006. 2006. Washington DC.
- 24.Wald J. Personal CommunicationCorporate ManagerWellesley, MA: Patient Gateway, Partners IS; 2008.
- 25.Jeffs D, Nossar V, Bailey F, Smith W, Chey T. Retention and use of personal health records: a population-based study J Paediatr Child Health 1994;30(3):248-252Jun. [DOI] [PubMed] [Google Scholar]
- 26.Wright A, Sittig DF. Security threat posed by USB-based personal health records Ann Intern Med 2007;146(4):314-315Feb. [DOI] [PubMed] [Google Scholar]
- 27.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption J Am Med Inform Assoc 2006;13(2):121-126Mar–Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Delbanco T, Sands DZ. Electrons in flight—e-mail between doctors and patients N Engl J Med 2004;350(17):1705-1707. [DOI] [PubMed] [Google Scholar]
- 29.Bachman JW. The patient-computer interview: a neglected tool that can aid the clinician Mayo Clin Proc 2003;78(1):67-78. [DOI] [PubMed] [Google Scholar]
- 30. U.S. Support for Health Research and Development by Source of Funds from 1977 to 1993National Institute of Health; 1993.
- 31. Charting a Course for the 21st Century—NLM's Long Range Plan 2006–2016National Library of Medicine; 2006.
- 32.Personalized Healthcare Workgroup. 2006http://www.hhs.gov/healthit/ahic/index.html 2006. Accessed June 11, 2007.
- 33. Report on attitudes about personal health records Internet Healthc Strateg 2004;6(9):10-11Sep. [PubMed] [Google Scholar]
- 34.Tang PC, Lansky D. The missing link: bridging the patient-provider health information gap Health Aff (Millwood) 2005;24(5):1290-1295Sep–Oct. [DOI] [PubMed] [Google Scholar]
- 35.Lober WB, Zierler B, Herbaugh AL, et al. Barriers to the use of a Personal Health Record by an Elderly Population AMIA Annu Symp Proc 2006:514-518. [PMC free article] [PubMed]
- 36.Kim EH, Wang M, Lau C, Kim Y. Application and evaluation of personal health information management system Conf Proc IEEE Eng Med Biol Soc 2004;5:3159-3162. [DOI] [PubMed] [Google Scholar]
- 37.Kim E, Mayani A, Modi S, Kim Y, Soh C. Evaluation of patient-centered electronic health record to overcome digital divide Conf Proc IEEE Eng Med Biol Soc 2005;2:1091-1094. [DOI] [PubMed] [Google Scholar]
- 38.Liaw ST. Patient and general practitioner perceptions of patient-held health records Fam Pract 1993;10(4):406-415Dec. [DOI] [PubMed] [Google Scholar]
- 39.Liaw ST, Radford AJ, Maddocks I. The impact of a computer generated patient held health record Aust Fam Physician 1998;27(Suppl 1):S39-S43. [PubMed] [Google Scholar]
- 40.Liaw T, Lawrence M, Rendell J. The effect of a computer-generated patient-held medical record summary and/or a written personal health record on patients' attitudes, knowledge and behaviour concerning health promotion Fam Pract 1996;13(3):289-293Jun. [DOI] [PubMed] [Google Scholar]
- 41.Denton IC. Will patients use electronic personal health records?. Responses from a real-life experience. J Healthc Inf Manag 2001;15(3):251-259Fall. [PubMed] [Google Scholar]
- 42.Sprague L. Personal health records: the people's choice? NHPF Issue Brief 2006;30(820):1-3.17146910 [Google Scholar]
- 43.Tobacman JK, Nolan P. Utilization of a personal health record in a general medicine clinic J Gen Intern Med 1996;11(6):370-372. [DOI] [PubMed] [Google Scholar]
- 44.Halamka J, Mandl KD, Tang P. Early Experiences with Personal Health Records J Am Med Inform Assoc 2007. Oct 18. [DOI] [PMC free article] [PubMed]
- 45.Cooke T, Watt D, Wertzler W, Quan H. Patient expectations of emergency department care: phase II—a cross-sectional survey Cjem 2006;8(3):148-157May. [DOI] [PubMed] [Google Scholar]
- 46.Morrissey J. What does the public think?. For consumers to adopt PHRs, they need reasons that hit home. J Ahima 2005;76(10):42-44Nov–Dec. [PubMed] [Google Scholar]
- 47.Smith CP. Helping consumers manage their PHRs J Ahima 2006;77(3):50-51Mar; 3; quiz 7–8. [PubMed] [Google Scholar]
- 48.Moen A, Brennan PF. Health@Home: the work of health information management in the household (HIMH): implications for consumer health informatics (CHI) innovations J Am Med Inform Assoc 2005;12(6):648-656Nov–Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mandl KD, Simons WW, Crawford WC, Abbett JM. Indivo: a personally controlled health record for health information exchange and communication BMC Med Inform Decis Mak 2007;7:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rubel P, Fayn J, Nollo G, et al. Toward personal eHealth in cardiology. Results from the EPI-MEDICS telemedicine project. J Electrocardiol 2005;38(4 Suppl):100-106Oct. [DOI] [PubMed] [Google Scholar]
- 51.Lee M, Delaney C, Moorhead S. Building a personal health record from nursing perspective Stud Health Technol Inform 2006;122:25-29. [PubMed] [Google Scholar]
- 52.Wuerdeman L, Volk L, Pizziferri L, et al. How accurate is information that patients contribute to their Electronic Health Record? AMIA Annu Symp Proc 2005:834-838. [PMC free article] [PubMed]
- 53.Slaughter L, Ruland C, Rotegard AK. Mapping cancer patients' symptoms to UMLS concepts AMIA Annu Symp Proc 2005:699-703. [PMC free article] [PubMed]
- 54.Tobacman JK, Kissinger P, Wells M, et al. Implementation of personal health records by case managers in a VAMC general medicine clinic Patient Educ Couns 2004;54(1):27-33Jul. [DOI] [PubMed] [Google Scholar]
- 55.Kim MI, Johnson KB. Patient entry of information: evaluation of user interfaces J Med Internet Res 2004;6(2):e13May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim MI, Johnson KB. Personal health records: evaluation of functionality and utility J Am Med Inform Assoc 2002;9(2):171-180Mar-Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dorr D, Bonner LM, Cohen AN, et al. Informatics Systems to Promote Improved Care for Chronic Illness: A Literature Review J Am Med Inform Assoc 2007;14(2):156-163March–April. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kimmel Z, Greenes RA, Liederman E. Personal health records J Med Pract Manage 2005;21(3):147-152Nov–Dec. [PubMed] [Google Scholar]
- 59.Hess R, Bryce CL, Paone S, et al. Exploring challenges and potentials of personal health records in diabetes self-management: implementation and initial assessment Telemed J E Health 2007;13(5):509-517Oct. [DOI] [PubMed] [Google Scholar]
- 60.The value of personal health records A joint position statement for consumers of healthcare J Ahima 2006;77(9):24Oct. [PubMed] [Google Scholar]
- 61.Ball MJ, Gold J. Banking on health: Personal records and information exchange J Healthc Inf Manag 2006;20(2):71-83Spring. [PubMed] [Google Scholar]
- 62.Ball MJ, Smith C, Bakalar RS. Personal health records: empowering consumers J Healthc Inf Manag 2007;21(1):76-86Winter. [PubMed] [Google Scholar]
- 63.Burrington-Brown J. The PHR effect J Ahima 2005;76(2):58-59Feb. [PubMed] [Google Scholar]
- 64.Burrington-Brown J, Friedman B. Educating the public about personal health records J Ahima 2005;76(9):94-95Oct. [PubMed] [Google Scholar]
- 65.Rhoads J, Metzger J. Personal health records: prospects and challenges for health plans AHIP Cover 2007;48(1):50Jan–Feb; 3. [PubMed] [Google Scholar]
- 66.Reinke T. Rise of the PHR Manag Care 2007;16(1):40-42Jan. [PubMed] [Google Scholar]
- 67.Neame R. Creating an infrastructure for the productive sharing of clinical information Top Health Inf Manage 2000;20(3):85-91Feb. [PubMed] [Google Scholar]
- 68.Waegemann CP. Closer to reality. Personal health records represent a step in the right direction for interoperability of healthcare IT systems and accessibility of patient data. Health Manag Technol 2005;26(5):16May; 8. [PubMed] [Google Scholar]
- 69.Lowes R. Personal health records: What's the status now? Med Econ 2006;83(4):TCP13-TCP14Feb 17; TCP6. [PubMed] [Google Scholar]
- 70.Clarke JL, Meiris DC, Nash DB. Electronic personal health records come of age Am J Med Qual 2006;21(3 Suppl):5S-15SMay–Jun. [DOI] [PubMed] [Google Scholar]
- 71.Iakovidis I. From electronic medical record to personal health records: present situation and trends in European Union in the area of electronic healthcare records Medinfo 1998;9(suppl):18-22Pt 1. [PubMed] [Google Scholar]
- 72.Iakovidis I. Towards personal health record: current situation, obstacles and trends in implementation of electronic healthcare record in Europe Int J Med Inform 1998;52(1–3):105-115Oct–Dec. [DOI] [PubMed] [Google Scholar]
- 73.Klein-Fedyshin MS. Consumer Health Informatics—integrating patients, providers, and professionals online Med Ref Serv Q 2002;21(3):35-50Fall. [DOI] [PubMed] [Google Scholar]
- 74.Nobel JJ. Health plan sponsored personal health records: a tool for information driven quality improvement AHIP Cover 2005;46(6):14-16Nov–Dec, 8, 20–5. [PubMed] [Google Scholar]
- 75.Sittig DF. Personal health records on the internet: a snapshot of the pioneers at the end of the 20th Century Int J Med Inform 2002;65(1):1-6Apr. [DOI] [PubMed] [Google Scholar]
- 76.Hicks J. Advocating for the PHR: educator's work sets stage for the future J Ahima 2005;76(10):88Nov–Dec. [PubMed] [Google Scholar]
- 77.Readers' perspective Personal health records will be widely used within five years, supplanting the need for regional health information organizations Health Data Manag 2007;15(10):8Oct. [PubMed] [Google Scholar]
- 78. PA partnership publishes IT recommendations Healthcare Benchmarks Qual Improv 2007;14(7):81-83Jul. [PubMed] [Google Scholar]
- 79. The value of personal health records. A joint position statement for consumers of healthcare by the American Health Information Management Association and the American Medical Informatics Association. J Ahima 2007;78(4):22Apr; 4. [PubMed] [Google Scholar]
- 80.Abrahamsen C. From Pong to PHRs: advances in electronic record keeping Nurs Manage 2007;38(8):20-21Aug. [DOI] [PubMed] [Google Scholar]
- 81.Albright B. Prepping for PHRs. The growing trend of consumer empowerment includes the speedy rise of personal health records. Healthc Inform 2007;24(2):44Feb; 6. [PubMed] [Google Scholar]
- 82.Anderson HJ. Managed care plans push PHRs Health Data Manag 2007;15(10):70Oct, 2. [PubMed] [Google Scholar]
- 83.Roop L. Technology. Big business charges ahead with personal health records. Hosp Health Netw 2007;81(2):17Feb. [PubMed] [Google Scholar]
- 84.Robeznieks A. Medicare to test PHRs. CMS will try 18-month pilot of Net-based records. Mod Healthc 2007;37(26):45Jun. [PubMed] [Google Scholar]
- 85.Robeznieks A. Getting personal. Legal liability, patient-data overload among issues making physicians uneasy over emergence of personal health records. Mod Healthc 2007;37(21):40-42May. [PubMed] [Google Scholar]
- 86.Pagliari C, Detmer D, Singleton P. Potential of electronic personal health records Bmj 2007;335(7615):330-333Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Morales Rodriguez M, Casper G, Brennan PF. Patient-centered design. The potential of user-centered design in personal health records. J Ahima 2007;78(4):44-46Apr; quiz 9–50. [PubMed] [Google Scholar]
- 88.Lovis C. Sustainable health care systems. Findings from the section on sustainable health care systems. Methods Inf Med 2007;46(Suppl 1):19-21. [PubMed] [Google Scholar]
- 89.Heubusch K. PHRs for the masses?. Consumers say they are interested in PHRs, but will they use them?. J Ahima 2007;78(4):34Apr, 6. [PubMed] [Google Scholar]
- 90.Greeg C, Buck SL. PHRs and physician practices J Ahima 2007;78(4):71-75Apr. [PubMed] [Google Scholar]
- 91.Foxhall K. Now it's personal. Personal health records may be next on deck for the certification process. Healthc Inform 2007;24(3):30Mar. [PubMed] [Google Scholar]
- 92.Campbell RJ. Getting to the good information. PHRs and consumer health informatics. J Ahima 2005;76(10):46-49Nov–Dec; quiz 51–2. [PubMed] [Google Scholar]
- 93.Friedman RH. Medicaid information technology architecture: an overview Health Care Financ Rev 2006;28(2):1-9Winter. [PMC free article] [PubMed] [Google Scholar]
- 94.Hagland M. Patient to partner. Will PHRs change the physician-patient relationship?. J Ahima 2005;76(10):38-40Nov–Dec. [PubMed] [Google Scholar]
- 95.Kun LG. Homecare and disease prevention: reviewing a decade of evolution-privacy still the biggest hurdle Conf Proc IEEE Eng Med Biol Soc 2006;1:4685. [Google Scholar]
- 96.Pope J. Implementing EHRs requires a shift in thinking. PHRs—the building blocks of EHRs—may be the quickest path to the fulfillment of disease management. Health Manag Technol 2006;27(6):24Jun, 6, 120. [PubMed] [Google Scholar]
- 97.Baker DB, Masys DR. PCASSO: a design for secure communication of personal health information via the internet Int J Med Inform 1999;54(2):97-104May. [DOI] [PubMed] [Google Scholar]
- 98.Blechner B, Butera A. Health Insurance Portability and Accountability Act of 1996 (HIPAA): a provider's overview of new privacy regulations Conn Med 2002;66(2):91-95Feb. [PubMed] [Google Scholar]
- 99.Srinivasan A. Keeping online personal records private: security and privacy considerations for Web-based PHR systems J Ahima 2006;77(1):62-63Jan, 8. [PubMed] [Google Scholar]
- 100.McSherry B. Access to confidential medical records by courts and tribunals: the inapplicability of the doctrine of public interest immunity J Law Med 2006;14(1):15-19Aug. [PubMed] [Google Scholar]
- 101.Conn J. Personal and (maybe) confidential. Questions over privacy, formats and definitions remain, but personal health records are on the way. Mod Healthc 2006;36(27):28-31Jul 3–10. [PubMed] [Google Scholar]
- 102.Harman LB. HIPAA: a few years later Online J Issues Nurs 2005;10(2):3May. [PubMed] [Google Scholar]
- 103.Sax U, Kohane I, Mandl KD. Wireless technology infrastructures for authentication of patients: PKI that rings J Am Med Inform Assoc 2005;12(3):263-268May–Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wright A, Sittig DF. Encryption characteristics of two USB-based personal health record devices J Am Med Inform Assoc 2007;14(4):397-399Jul–Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Fullbrook S. Confidentiality. Part 3: Caldicott guardians and the control of data. Br J Nurs 2007;16(16):1008-1009Sep 13–27. [DOI] [PubMed] [Google Scholar]
- 106. Computerisation of personal health records Health Visit 1978;51(6):227Jun. [PubMed] [Google Scholar]
- 107. Recordkeeping systems: personal health records J Am Med Rec Assoc 1984;55(12):42Dec. [PubMed] [Google Scholar]
- 108.Black D. Personal health records J Med Ethics 1992;18(1):5-6Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mon DT. PHR and EHR: what's the difference?. Records differ in span and legality. J Ahima 2005;76(10):60-61Nov–Dec. [PubMed] [Google Scholar]
- 110.Jossi F. Personal health records Healthc Inform 2006;23(2):52Feb, 4. [PubMed] [Google Scholar]
- 111.Joshi P, Jones KV, Hanson RM, Alperstein G, Fasher B. Personal health records J Paediatr Child Health 1993;29(5):400-401Oct. [DOI] [PubMed] [Google Scholar]
- 112.Endsley S, Kibbe DC, Linares A, Colorafi K. An introduction to personal health records Fam Pract Manag 2006;13(5):57-62May. [PubMed] [Google Scholar]
- 113.Conn J. McKesson deal gives docs new PHR purveyor. Even with acquisition, RelayHealth exec vows vendor neutrality; others dubious. Mod Healthc 2006;36(25):54Jun. [PubMed] [Google Scholar]
- 114.Edlin M. Implementing personal health records AHIP Cover 2006;47(2):14-16Mar–Apr; 9. [PubMed] [Google Scholar]
- 115.Gawthorn EC. Personal health records (PHR) Aust Fam Physician 1983;12(6):466-468Jun. [PubMed] [Google Scholar]
- 116. Annual report of Council, 1985–1986: medical ethics Br Med J (Clin Res Ed) 1986;29(suppl):25-27Mar; 292(6524). [PMC free article] [PubMed] [Google Scholar]
- 117.Schlosser RL, Krackardt B, Weber J, Lerman E. [Impact of Preterm Infants of Less than 30 Weeks Gestation on the Prevalence of Special Education in School Beginners of a German City (Frankfurt/Main).] Klin Padiatr 2007. Aug 21. [DOI] [PubMed]
- 118.Colang JE, Killion JB, Vano E. Patient dose from CT: a literature review Radiol Technol 2007;79(1):17-26Sep–Oct. [PubMed] [Google Scholar]
- 119.Einbinder JS, Bates DW. Leveraging information technology to improve quality and safety Methods Inf Med 2007;46(Suppl 1):22-29. [PubMed] [Google Scholar]
- 120.Celebi S, Acik Y, Deveci SE, et al. Epidemiological features of irritable bowel syndrome in a Turkish urban society J Gastroenterol Hepatol 2004;19(7):738-743Jul. [DOI] [PubMed] [Google Scholar]
- 121.Bashford JA, Warren RM, Brown CA. Use of speech-modulated noise adds strong “bottom-up” cues for phonemic restoration Percept Psychophys 1996;58(3):342-350Apr. [DOI] [PubMed] [Google Scholar]
- 122.Chen X, Yuan H, He W, Hu X, Lu H, Li Y. Construction of a novel kind of expression plasmid by homologous recombination in Saccharomyces cerevisiae Sci China C Life Sci 2005;48(4):330-336Aug. [DOI] [PubMed] [Google Scholar]
- 123.Hellmann H, Davis JM, Thurau K. Blood pressure and indices of glomerular filtration area in hypertensive and normotensive Prague rats Kidney Blood Press Res 2000;23(6):385-392. [DOI] [PubMed] [Google Scholar]
- 124.Kaye JA, Shulman LN. Screening program for colorectal cancer: participation and follow up HMO Pract 1991;5(5):168-170Sep–Oct. [PubMed] [Google Scholar]
- 125.Kim BK, Baldini MG. Glycerol stress and platelet integrity Cryobiology 1986;23(3):209-213Jun. [DOI] [PubMed] [Google Scholar]
- 126.Maciulaitis R, Janusonis T. [Irrational drug use in Siauliai, Panevezys and Utena counties of Lithuania] Medicina (Kaunas) 2003;39(Suppl 2):9-18. [PubMed] [Google Scholar]
- 127.Moore KH, Brouwer KL. High-performance liquid chromatographic evaluation of the effect of heat treatment on trimethoprim and sulfamethoxazole stability in serum Ther Drug Monit 1995;17(4):356-360Aug. [DOI] [PubMed] [Google Scholar]
- 128.Neufeld L, Pelletier DL, Haas JD. The timing hypothesis and body proportionality of the intra-uterine growth retarded infant Am J Hum Biol 1999;11(5):638-646Sep. [DOI] [PubMed] [Google Scholar]
- 129.O'Flaherty S, Jandera E, Llewellyn J, Wall M. Personal health records: an evaluation Arch Dis Child 1987;62(11):1152-1155Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Shah S, Raman S, Moreira C, MacIntyre CR. School immunisation certificates—a review over time in a disadvantaged community Aust N Z J Public Health 2001;25(6):534-538Dec. [DOI] [PubMed] [Google Scholar]
- 131.Zeng-Treitler Q, Kim H, Goryachev S, Keselman A, Slaughter L, Smith CA. Text characteristics of clinical reports and their implications for the readability of personal health records Medinfo 2007;12(Pt 2):1117-1121. [PubMed] [Google Scholar]
- 132.Vogel V, Backer A, Heller J, Kramer HJ. The renal endothelin system in the Prague hypertensive rat, a new model of spontaneous hypertension Clin Sci (Lond) 1999;97(1):91-98Jul. [PubMed] [Google Scholar]
- 133.Smith NL, Maynard C. The burden of diabetes-associated cardiovascular hospitalizations in Veterans Administration (VA) and non-VA medical facilities Diabetes Care 2004;27(Suppl 2):B27-B32. [DOI] [PubMed] [Google Scholar]