Abstract
Objectives
To examine the psychometric properties, adaptations, translations, and applications of the Confusion Assessment Method (CAM), a widely-used instrument and diagnostic algorithm for identification of delirium.
Design
Systematic literature review
Setting
NA
Measurements
Electronic searches of PubMED, EMBASE, PsychINFO, CINAHL, Ageline, and Google Scholar, augmented by reviews of reference listings, were conducted to identify original English-language articles utilizing the CAM from January 1, 1991 to December 31, 2006. Two reviewers independently abstracted key information from each article.
Participants
NA
Results
Of 239 original articles, 10 (4%) were categorized as validation studies, 16 (7%) as adaptations; 12 (5%) as translations, and 222 (93%) as applications. Validation studies evaluated performance of the CAM against a reference standard. Results were combined across 7 high quality studies (n=1071), demonstrating an overall sensitivity of 94% (95% confidence interval, CI, 91–97%), and specificity of 89% (95% CI, 85–94%). CAM has been adapted for use in ICU, emergency, and institutional settings, and for scoring severity and subsyndromal delirium. CAM has been translated into 10 languages where published articles are available. In application studies, CAM-rated delirium is most commonly used as a risk factor or outcome, but also as an intervention or reference standard.
Conclusions
The CAM has helped to improve identification of delirium in clinical and research settings. To optimize performance, the CAM should be scored based on observations made during formal cognitive testing, and training is recommended. Future action is needed to optimize use of the CAM and to improve the recognition and management of delirium.
Keywords: Delirium, systematic review, dementia, older persons, Confusion Assessment Method
Delirium is a common and serious problem affecting older adults, associated with increased mortality, prolonged hospital stays, increased healthcare costs, higher rates of institutionalization, and decreased functional independence (1). High-risk settings for delirium include the hospital, intensive care, emergency, post-operative, institutional, and terminal care settings (2). Delirium increases hospital costs by at least $2,500 per patient, resulting in over $6.9 billion (2004 USD) in hospital costs each year (2). Despite its adverse impact, delirium remains poorly recognized in clinical practice. The Confusion Assessment Method is a delirium instrument published in 1990 (3), which was created to improve the identification of delirium.
The Confusion Assessment Method (CAM) includes an instrument and diagnostic algorithm for identification of delirium (3). Originally developed by literature review and expert consensus, the CAM was validated against the reference standard ratings of geropsychiatrists based on Diagnostic and Statistical Manual for Mental Disorders Third Edition Revised (DSM-IIIR) (4) criteria. The CAM was designed to allow non-psychiatric clinicians to diagnose delirium quickly and accurately following brief formal cognitive testing. The CAM instrument assesses the presence, severity, and fluctuation of 9 delirium features: acute onset, inattention, disorganized thinking, altered level of consciousness, disorientation, memory impairment, perceptual disturbances, psychomotor agitation or retardation, and altered sleep-wake cycle. The CAM diagnostic algorithm is based on four cardinal features of delirium: 1) acute onset and fluctuating course, 2) inattention, 3) disorganized thinking, and 4) altered level of consciousness. A diagnosis of delirium according to the CAM requires the presence of features 1, 2, and either 3 or 4. The CAM demonstrated sensitivities from 94–100%, specificities from 90–95%, positive predictive accuracy of 91– 94%, negative predictive accuracy of 90–100%, interrater reliability ranging from .81–1.00; and convergent agreement with other mental status tests including the Mini-Mental State Examination (MMSE) (5). The Confusion Assessment Method (CAM) Training Manual was developed to facilitate its appropriate use <http://elderlife.med.yale.edu/pdf/The%20Confusion%20Assessment%20Method.pd>. Because of its accuracy, brevity, and ease of use by clinical and lay interviewers, the CAM has become the most widely used standardized delirium instrument for clinical and research purposes over the past 16 years.
The purpose of this article is to provide a systematic review of all original English language articles utilizing the CAM to synthesize its psychometric properties, adaptations, published translations, and clinical and research applications. Strengths and limitations of the articles have been highlighted. Ultimately, it is hoped that this summary will provide a comprehensive overview of the current utility of the CAM, and recommendations for its appropriate use.
Methods
Systematic Literature Review
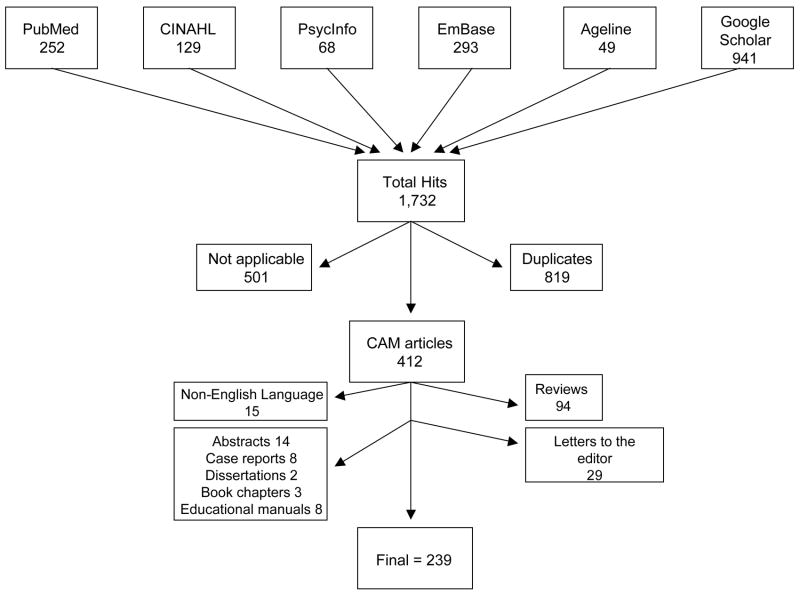
We conducted a comprehensive literature search for all original research articles utilizing the CAM published between January 1, 1991 and December 31, 2006, using PubMED, EMBASE, PsychINFO, CINAHL, Ageline, and Google Scholar. We used full text searches for the search term ‘Confusion Assessment Method’. Applying additional search terms, such as ‘delirium’, ‘acute confusional state’, did not identify additional articles utilizing the CAM. Our inclusion criteria for articles were: 1) original article with either inclusion of primary data or analysis of previously collected data; 2) article indicates use of the CAM instrument and/or diagnostic criteria; 3) articles published in the English language or available as an English language translation (other than for the translations section). The search initially produced 1,732 articles: PubMED (n=252 articles), EMBASE (n=293), CINAHL (n=129), PsychINFO (n=68), Ageline (n=49), and Google Scholar (n=941)(Figure 1). Our search was supplemented with secondary review of the reference listings of the identified articles. We excluded 675 articles that did not meet our inclusion criteria, as follows: 94 review articles, 15 foreign language articles, 8 case reports, 29 letters to the editor, 14 abstracts, 2 dissertations, 3 book chapters, 8 educational manuals, and 501 articles that did not explicitly use the CAM. An additional 819 citations were excluded as duplicates (Figure 1). A total of 239 articles were included in the final review.
Figure 1.
Flow diagram illustrating the selection process of original articles that used the Confusion Assessment Method (CAM).
Article Categorization and Review
Each article was independently reviewed by at least 2 of the authors (LW, ES, MF, SI) to categorize the article and abstract key information. Articles were categorized as a validation, adaptation, translation, or application study, by meeting the specific definitions detailed below; articles could be assigned to more than one category. Validation studies were defined as articles that examined CAM performance characteristics, including sensitivity, specificity, and reliability. Articles that reported only inter-rater reliability were not classified as validation studies. Adaptation studies provided an adaptation of the CAM instrument to be used in a different setting or to refine the diagnosis. Translation studies developed a foreign language version of the CAM. Application studies were those that utilized the CAM (such as to rate delirium as a risk factor or outcome) in an original article.
After categorization, key information was abstracted from each article in standardized tabular format. Two authors abstracted each article independently and blindly, and any discrepancies in information were resolved in a consensus conference of all authors. Information abstracted from each article varied by category, as detailed below. For validation studies, the following information was abstracted: study population and number, study site, cognitive test used prior to CAM, reference standard, sensitivity, specificity, and inter-rater reliability. For adaptation studies, the following information was abstracted: study population and number, study description, changes made, reason for adaptation, and application of the adapted version. For translation studies, published article(s) documenting the translation were required for inclusion and the following information was abstracted: language, instrument translated, reference, the method of translation, and validation of the translation. For application studies, the following information was abstracted: study population and number, study site, study design, delirium prevalence and incidence, and cognitive test used prior to CAM.
In addition, for the validation studies, a quality rating was conducted of each study independently and blindly by two reviewers; discrepancies in ratings were resolved in a consensus conference. Each article was rated on 5 criteria, which were determined as quality standards based on methodologic treatises for validation studies (6). These 5 criteria were: A. Adequacy of the reference standard rating (i.e., comprehensive assessment for delirium); B. Blinded assessment (i.e., no shared information between CAM rater and reference standard); C. Close proximity of assessments between CAM rater and the reference standard assessment (i.e., 8 hours or less); D. Inclusion of false positive challenges (e.g., dementia, depression, and other psychiatric conditions); E. Inclusion of false negative challenges (e.g., patients with normal mental status, without psychiatric conditions). Information to fulfill each criterion needed to be explicitly stated in each article. Each criterion was rated as: 0=not met; 0.5=partially met; 1=fully met, to create an additive scale from 0–5 for each study. Studies with quality ratings of 1.0 or less were excluded, and overall (combined) values of sensitivity and specificity, with their associated 95% confidence intervals, were calculated across the high quality-rated studies. A random effects model, which did not assume homogeneity across studies, was used to estimate the combined results.
Results
Of the 239 final articles, 11 (4.6%) were categorized as validation studies, 16 (6.7%) as adaptations, 12 (5.0%) as translations, and 222 (92.9%) as applications. Some articles fit into multiple categories. Results for each of these categorizations will be further described below.
Validation Studies
Performance characteristics of the CAM were evaluated in 11 studies (Table 1) (3, 7–16). The reference standards used in these studies included expert assessments (geriatrician, psychiatrist, neuropsychologists and advanced practice nurses) applying DSM-III, DSM-IIIR, DSM-IV, or ICD-10 criteria or a consensus diagnosis. The sensitivities are reported from 46–100%. Three studies had sensitivity rates of ≤ 70% (13, 15–16). Unifying reasons for the low sensitivities included nurses or research assistants conducting the ratings with extremely brief cognitive assessments (e.g., attention tasks alone)(15), without formal training in use of the CAM (15–16), or in populations with high rates of dementia (15). In addition, the reference standard assessments were poorly specified in these 3 studies (13, 15–16). The specificities are reported from 63–100%, with overall. The one study (8) with lower specificity (63%) included a large proportion of patients with dementia (43%), depression (15%) and psychosis (4%), which may have confounded delirium recognition. To calculate a combined overall value of sensitivity and specificity, we excluded 4 studies with a quality rating of 1.0 or less (Table 1). Thus, results were combined across 7 studies with a total of 1071 subjects, yielding an overall sensitivity of 94% (95% confidence interval, CI, 91–97%), and specificity of 89% (95% CI, 85–94%). Interrater reliability (.70–1.00) was moderate to high across all studies.
Table 1.
Validation Studies of the CAM
| Study | Study Population (N) * | CAM rated by | Reference standard used (who, what)§ | Sens|| | Spec¶ | Inter-rater reliability** | Quality criteria | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | Score | |||||||
| Gonzalez 2004 (7) | Inpts ≥ 65 y.o. GH (153) | MD | Psychiatrist, DSM-IV | .90 | 1.0 | κ = .89 | 1 | 1 | 1 | 1 | .5 | 4.5 |
| Laurila 2002 (8) | Pts > 70 y.o. GH (81) | MD | Geriatrician, DSM III, III-R, IV and ICD-10 | .81–.86 | .63–.84 | -- | 1 | 1 | 1 | 1 | 0 | 4.0 |
| Fabbri 2001 (9) | Pts ≥ 60 y.o., ED (100) | MD | Psychiatrist, DSM-IV | .94 | .96 | κ = .70 | 0 | 0 | 1 | 0 | 0 | 1.0 |
| Monette 2001 (10) | Pts ≥ 66 y.o., ED (110) | RN | Geriatrician, DSM-IIIR and DSM- IV | .86 | 1.0 | κ = .91 | .5 | 1 | 1 | 1 | 0 | 3.5 |
| Ely 2001a (11) | Ventilated and non- Ventilated ICU, UH (38) | RN, MD | Delirium experts (MD), DSM-IV | .95–1.0 | .89–.93 | κ = .79–.95 | 1 | 1 | 1 | 0 | 0 | 3.0 |
| Ely 2001b (12) | Ventilated ICU pts, UH (111) | RN | Delirium experts (MD, PhD), DSM-IV | .93–1.0 | .98–1.0 | κ = .96 | 1 | 1 | 1 | 0 | 0 | 3.0 |
| Rolfson 1999 (13) | Elderly CABG pts, UH (71) | MD, RN | MD, DSM-IIIR | Overall .701 | Overall 1.002 | -- | 0 | 0 | 0 | 0 | 0 | 0 |
| Zou 1998 (14) | Pts ≥ 65 y.o., GH (87) | RN | Consensus diagnosis | .89 | 1.00 | κ = 0.86 | .5 | 0 | 1 | 0 | 0 | 1.5 |
| Pompei 1995 (15) | Pts ≥ 65 y.o, UH. (432) | RN | MD/PhD., DSM-IIIR | .46 | .92 | -- | 0 | 0 | 0 | .5 | 0 | 0.5 |
| Rockwood1994 (16) | Pts ≥ 65 y.o, UH (434) | RN | MD, DSM-IIIR | .68 | .97 | -- | .5 | 0 | 0 | .5 | 0 | 1.0 |
| Inouye 1990 (3) | Pts ≥ 65 y.o, UH (56) | MD | Psychiatrist, DSM-IIIR | .94–1.0 | .90–.95 | κ = .81–1.0 | 1 | 1 | 1 | 1 | 1 | 5.0 |
CAM = Confusion Assessment Method.
Inpts = inpatients; (N) = number of patients; Pts = patients; y.o. = years old.
ED=emergency department; GH=general hospital (urban or rural); UH=university-affiliated hospital; ICU=intensive care unit; MD=physician; RN=nurse.
DSM= Diagnostic and Statistical Manual Versions III, III-R, IV; ICD-10 = International Classification of Diseases 10th Revision.
Sens = Sensitivity; Spec = Specificity
Average of physician-administered CAM (1.00) and nurse-administered CAM (.13);
Average of physician-administered CAM (1.00) and nurse-administered CAM (1.00).
κ= kappa statistic. Quality criteria (See text for details): A=adequacy of reference standard rating; B=blinded assessment; C=close proximity of assessments; D=inclusion of false positive challenges; E=inclusion of false negative challenges.
An additional study, which did not include a reference standard rating for delirium, demonstrated a high degree of correlation between the CAM and the Delirium Rating Scale (DRS)(r=.92) (17).
These previous studies demonstrate that the accuracy of the CAM rating is improved when formal cognitive testing is used prior to the rating (3, 18). The MMSE is the most widely used cognitive test. Other frequently used tests include the Telephone Interview of Cognitive Status, Short Portable Mental Status Questionnaire, and the Blessed Information-Memory-Concentration test. Studies that compared nurse to physician rating of the CAM found that physician-rated scores had higher sensitivities (13, 16). Appropriate training of the interviewers is also crucial for accurate CAM ratings.
Adaptations
Adaptations of the CAM instrument are presented in Table 2 (11–12, 19–23). Adaptations have been developed to address specific patient populations, such as the CAM-ICU for non-verbal, ventilated patients and adapted versions for the emergency department and nursing home populations. Each of these latter adaptations involved specifying a brief cognitive and/or functional assessment appropriate for the target population to score the four-item CAM algorithm. Notably, the CAM features themselves were not adapted. The CAM has also been adapted for scoring severity and partial (subsyndromal) forms of delirium. Finally, modifications in the scoring of CAM items, wording of some questions, or addition of other questions, have occurred commonly.
Table 2.
CAM Adaptations
| Adaptation | Setting | How Adapted | Validation against Reference Standard | Correlation with other measures assessed |
|---|---|---|---|---|
| CAM-ICU (11–12, 19) | ICU-ventilated patients | • Added nonverbal tasks to rate CAM items | Y | N |
| CAM for ED (20) | ED | • Assess recent history
• Attention tasks |
N | Y |
| MDS Version 3.0 | NH | • Modified CAM items included as part of resident assessment | N | In progress |
| Nursing Home CAM (21) | NH | • Uses MDS criteria to rate CAM | N | Y |
| Delirium Index (22) | All Settings | • Rate severity of 7 delirium symptoms to create severity scale | N | Y |
| One Day Fluctuation Scale (23) | DLB patients | • Rate 7 features of DLB | N | Y |
CAM=Confusion Assessment Method; ICU=intensive care unit; MDS=Minimum Data Set; ED=emergency department; NH=nursing home; DLB=dementia with Lewy bodies; Y=yes; N=no.
Developed specifically for use in mechanically-ventilated intensive care unit (ICU) patients, the CAM-ICU provides a brief non-verbal assessment to score the CAM algorithm. Delirium is a frequent problem in the ICU setting, occurring in up to 82% of patients, and the CAM-ICU is widely used. In two validation studies (11–12), the CAM-ICU was compared with ratings by delirium experts using the DSM-IV, yielding a sensitivity of 95–100%, specificity of 93–98%, and interrater reliability of .79–.95. When the non-verbal ratings on the CAM-ICU were directly compared to verbal ratings (24), CAM-ICU ratings demonstrated lower sensitivity of 73% and lower interrater reliability of .64, but maintained a high specificity of 100%. Thus, standard cognitive tests utilizing verbal responses should be used whenever possible to avoid missing delirium cases. Given the high frequency and poor outcomes of delirium in the ICU (19), the Society of Critical Care Medicine (SCCM) has advised that ICU patients should be monitored regularly for delirium (25).
For rapid evaluation of delirium in the emergency department (ED) setting (20), the assessment for the CAM was modified to add questions to assess the patient’s history of acute mental status change, hallucinations, or dementia. In addition, attention tasks were added, asking the patient to recite the days of the week backward, count backward from 20 and complete a 5-item forward digit span. This adapted version of the CAM was not formally validated, but ratings were compared with ED physician’s diagnosis. The adapted CAM diagnosed delirium in 10% of ED patients, and the ED physicians diagnosed delirium in only 17% of these cases.
An adapted version of the CAM is being included for delirium screening in the ongoing national test of the new version of the Minimum Data Set (MDS Version 3.0) http://www.cms.hhs.gov/NursingHomeQualityInits/25_NHQIMDS30.asp being conducted in 70 community and 20 Veterans Affairs nursing homes. The Minimum Data Set is a standardized resident assessment that is completed on every person admitted to a Medicare certified nursing home to screen for medical and functional problems.
The Nursing Home Confusion Assessment Method (NH-CAM)(21) was created to diagnose delirium in nursing home residents using the items currently in use in the Minimum Data Set (MDS) Resident Assessment Instrument. The NH-CAM uses 9 items from the MDS to create a CAM algorithm rating. Based on this rating, 31.8% of 35,721 residents met criteria for delirium. NH-CAM scores were significant independent predictors of mortality and rehospitalization in this group. The NH-CAM has not been validated against an external reference standard.
The CAM has been adapted to yield a severity score indicating the number and severity of CAM items present. For instance, one study utilized an additive score (26) for the 4 key features of delirium in CAM algorithm (symptom fluctuation, inattention, disorganized thinking, and altered level of consciousness). Each symptom, other than fluctuation, was rated as absent (0 points), mild (1 point), or marked (2 points); symptom fluctuation was rated as absent (0 points) or present (1 point). An additive delirium severity score was created, ranging from 0–7, with higher scores indicating increased severity. In a similar fashion, other studies (27–28) have created additive scales of the number of CAM delirium items present as a severity index. Cases with 1–2 delirium features were identified as partial or subsyndromal delirium in previous studies (27–28). Importantly, these studies have demonstrated that the poor outcomes associated with delirium increased with the number of CAM items present, with the best outcomes with 0 CAM features, intermediate with 1–2 features, and worst with 3–4 features (27–28).
The Delirium Index (DI) (22) was specifically created to rate delirium severity, and adapts several CAM items. The DI assesses the severity of 7 symptoms of delirium: inattention, disorganized thinking, altered levels of consciousness, disorientation, memory impairment, perceptual disturbances, and psychomotor agitation or retardation. Each item is scored on a scale from 0–3, with a maximum possible score of 21. In the original validation study (22), the interrater reliability of the DI ranged from .78–.88 and correlation with the DRS was .84. In another validation study using the CAM as the reference standard (29), the DI had an inter-rater reliability of .98, strong correlations with the Barthel Index, Acute Physiology Score, and Charlson Comorbidity Index, and good internal responsiveness.
The CAM has been adapted to assess fluctuation in patients with Dementia with Lewy Bodies (DLB)(23). This adaptation, the One Day Fluctuation Assessment Scale, consisting of 7 items (falls, fluctuation, drowsiness, attention, disorganized thinking, altered level of consciousness, communication), has been validated against clinician’s diagnoses of DLB.
Other variations in the wording, content, and scoring of the CAM questions have occurred commonly. One study (30) modified the wording to change criterion 1 to “acute onset or fluctuating course (not both)”, criterion 4 (level of consciousness) to be scored on a 0–2 scale, and developed a severity scale. The CAM has been adapted in another study (20) to detect “probable delirium” by changing the first criterion to fulfillment of either acute onset or fluctuating course. The CAM has been adapted to be rated by proxy interview rather than direct patient observation (31). Finally, questions have been added to the CAM to further assess the onset and course of the mental status change (7).
Translations
The CAM has been translated into 10 languages (Table 3) (7–9, 32–40) where published studies are available. The methods used for translation of the CAM in these studies included translation and back-translation in 4, expert panel consensus in 3, and unspecified in 3. Of these translations, 5 have been validated for their performance characteristics against reference standard ratings.
Table 3.
Published Translations of the CAM
| Language | Instrument translated | Reference | Sens | Spec | Inter-rater reliability | Translation Method | Reference Standard for validation |
|---|---|---|---|---|---|---|---|
| Chinese | CAM-ICU | Lin 2004 (32) | Rater 1:.91 Rater 2:.95 | .98 | .91 | Translation and back-translation | Psychiatrist, DSM-IV criteria |
| Dutch | CAM | Lemiengre 2006 (33) | Method 1:.67 Method 2:.24 | Method 1:.91 Method 2:.98 | 1.00 | Translation and back-translation | Prior diagnosis with CAM by trained research nurse |
| Finnish | CAM | Laurila 2002 (8) | .81–.86 | .63–.84 | -- | Expert panel consensus | Geriatrician, DSM-III, IIIR, IV and ICD-10 criteria |
| French | CAM | Laplante 2005 (34) | -- | -- | -- | Translation and back-translation | -- |
| German | CAM | Bickel 2004 (35) | -- | -- | -- | Expert panel consensus | -- |
| Italian | CAM | Grassi 2001 (36) | -- | -- | -- | Not specified | -- |
| Japanese | CAM | Kawaguchi 2006 (37), Kudoh 2004 (38), Shigeta 2001 (39) | -- | -- | -- | Not specified | -- |
| Portuguese | CAM | Fabbri 2001 (9) | .94 | .96 | κ = .70 | Translation and back-translation | Psychiatrist, DSM-IV |
| Spanish | CAM | Gonzalez 2004 (7) | .90 | 1.0 | κ = .89 | Expert panel consensus | Psychiatrist, DSM-IV |
| Turkish | CAM-ICU | Akinci 2005 | -- | -- | -- | Not specified | -- |
Applications
The CAM is widely used in both research and clinical settings. In terms of research applications, the CAM has been applied in at least 222 original studies to date (Reference listing available on line at: [Editor: please insert]). In these studies, delirium prevalence ranged from 2.3% (41) to 66.5% (42) and delirium incidence from 0.6% (43) to 81.7% (19). The research applications of the CAM included: study outcome (n= 117 studies), risk factor or predictor variable (n= 35), reference standard for another instrument (n= 24), or other (e.g., to determine study eligibility, to improve the recognition of delirium, to stratify patients, to establish the reliability of self-report information, and as a covariate in analyses)(n= 46 studies).
CAM-rated delirium was used as a predictor of poor functional outcomes, serious falls, mortality, adverse clinical and post-surgical outcomes, inadequate pain control, prolonged hospital stay, increased sedative/restraint use, and institutionalization. In addition, the CAM was used as the reference standard for delirium in comparison to psychiatrist and emergency department physician diagnosis, nurse assessment of delirium, Delirium Index, Bedside Confusion Scale, NuDESC, CAM-ICU, Clock Drawing Test, serial MMSEs, Bispectral Index, and a chart-based method for identification of delirium
The CAM itself has been incorporated into several interventions, which have been systematically evaluated. Webster et al (44) tested the efficacy of delirium practice guidelines that included the CAM and specialized delirium care teams on the recognition, management, and outcomes of delirious patients. Similarly, Lacko et al (45) implemented an educational program on delirium for nurses, which included the CAM. Hustey et al (46) adopted the CAM as part of routine screening examinations in elderly emergency room patients. Finally, the CAM-ICU was included in routine ICU patient agitation/sedation and delirium monitoring (25,47).
Clinical practice uses for which we have received written requests include use of the CAM as part of electronic medical record systems, admission nursing assessments, training of nursing and physician staff, and screening of patients in multiple clinical settings (emergency room, hospital, intensive care unit, palliative care, geriatric/acute care for the elderly (ACE) units, nursing home, and home care). The CAM is recommended for delirium detection in over 30 published clinical practice guidelines to date, for example, those published by American Psychiatric Association (http://www.psych.org/psych_pract/treatg/pg/prac_guide.cfm), American College of Emergency Physicians (http://www.acep.org/NR/rdonlyres/7C82DA5F-D478-4FA9-B095-5AFC0A66476A/0/cp402100.pdf), Society for Critical Care Medicine (25) (http://www.sccm.org/professional_resources/guidelines/table_of_contents/Documents/Sedatives.pdf), the Royal College of Physicians and the British Geriatrics Society (http://www.rcplondon.ac.uk/pubs/books/pdmd/index.asp), Australian Health Ministers (http://www.health.vic.gov.au/acute-agedcare/delirium-cpg.pdf), Canadian Coalition for Seniors’ Mental Health (http://www.cagp.ca/en/CCSMH%20National%20Delirium%20Guideline%20May%202006.pdf), and 2006 Canadian Cardiovascular Society management guidelines for heart failure (http://www.canadianguidelines.com/landing.asp?topic=19).
Discussion
This article provides a systematic review of the usage of the CAM over the past 16 years. Based on its favorable performance characteristics and ease of use, the CAM has gained widespread usage nationally and internationally. To date, 11 published studies have evaluated the performance characteristics of the CAM compared with reference standard ratings. Based on 7 high quality studies (n=1,071), a combined sensitivity rate has been calculated as 94% (95% CI 91–97%), and combined sensitivity rate of 89% (95% CI 85–94%). Interrater reliability (kappa 0.7–1.0) is generally moderate to high across studies.
Adaptations of the CAM include the CAM-ICU for non-verbal ventilated ICU patients, adaptations for emergency department and nursing home settings (MDS Version 3.0 and the Nursing Home CAM), the Delirium Index for scoring severity, and use of the CAM to identify partial (subsyndromal) forms of delirium. The CAM has been translated into 10 languages where published articles are available. A significant shortcoming of these studies is that not all of the adaptations or translations have been validated against a reference standard to determine their psychometric properties. This will be an important area for future research.
In over 222 application studies, we have documented that the CAM is widely used for both clinical and research applications. While our literature review was comprehensive, some articles may have been missed, particularly those where the term “confusion assessment method” did not appear in the abstract or key search areas or were published in foreign languages.
Based on this review, several recommendations are proposed to optimize the use of the CAM for the identification of delirium. Some training is recommended for optimal use. The Confusion Assessment Method Training Manual is available at http://elderlife.med.yale.edu/pdf/The%20Confusion%20Assessment%20Method.pdf to facilitate this process. Moreover, the CAM was designed to be scored based on observations made during formal cognitive assessment, such as with brief instruments like the MMSE or SPMSQ. Without such formal assessment (or with extremely brief assessments), the sensitivity of the CAM for delirium detection is compromised. For research purposes, use of the full 9-item CAM instrument is recommended to maximize sensitivity for the detection of delirium.
An important caveat about use of the CAM is worthy of comment. Given its imperfect sensitivity, we do not recommend the CAM as the sole means for identification of delirium in the clinical setting. The use of astute clinical judgment combined with other formal cognitive screening measures is required to avoid missing hypoactive, subtle, or atypical cases of delirium.
This systematic review has helped to uncover gaps in our knowledge base regarding the CAM and to define critical areas where further research is needed. Future work should focus on defining the optimal brief assessment to score the CAM. Based on recent studies (48), this assessment is likely to require assessment of sustained attention and executive functioning; nonverbal assessments, such as used for the CAM-ICU, are not ideal in verbal patients (24). In addition, application of combined methods may help to maximize the sensitivity of the CAM for detection of delirium, (e.g., combined assessments (49), medical record review (50). Identification of key features that distinguish delirium from dementia at the bedside may help to improve the specificity of the CAM. Future work is needed to validate the use of CAM summary scores or adaptations to measure delirium severity, and to correlate these scores with outcomes. Finally, testing educational efforts to improve the identification of delirium with the CAM features among physicians and nurses are greatly needed.
Despite use of the CAM, the serious and persistent lack of recognition of delirium in clinical settings remains a fundamental problem. Systematic, widespread changes in our approaches to care of older persons will be needed to make substantial impact on the devastating problem of delirium in this population.
Acknowledgments
The authors thank Ms. Sarah Dowal and Ms. Jasneet Aneja for assistance with manuscript preparation. This paper is dedicated to Ben and Jordan Helfand.
Funding Sources: Funded in part by grants R21AG025193 and K24AG00949 from the National Institute on Aging, and the Aging Brain Center, Institute for Aging Research, Hebrew Senior Life. Dr. Fearing is funded by grant T32 AG023480 from the National Institute on Aging, Beth Israel Deaconess Medical Center, and Harvard Medical School. Dr. Inouye holds the Milton and Shirley F. Levy Family Chair.
Footnotes
Financial Disclosure: The authors have no financial conflicts of interest to disclose.
Sponsors’ Role: The sponsors played no role in design, methods, recruitment, data collection, analysis, interpretation of data, or preparation and review of the manuscript.
References
- 1.Adamis D, Treloar A, Martin FC, et al. Recovery and outcome of delirium in elderly medical inpatients. Arch Gerontol Geriatr. 2006;43:289–98. doi: 10.1016/j.archger.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Inouye SK. Current concepts: delirium in older persons. N Engl J Med. 2006;354:1157–65. doi: 10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- 3.Inouye SK, Van Dyck CH, Alessi CA, et al. Clarifying confusion: the Confusion Assessment Method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–8. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3 rev. Washington, DC: Am Psychiatric Assoc; 1987. pp. 97–124. [Google Scholar]
- 5.Folstein MF, Folstein SE, McHugh PR. Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 6.Feinstein AR. Clinimetrics. New Haven: Yale University Press; 1987. [Google Scholar]
- 7.Gonzalez M, de Pablo J, Fuente E, et al. Instrument for detection of delirium in general hospitals: adaptation of the confusion assessment method. Psychosomatics. 2004;45:426–31. doi: 10.1176/appi.psy.45.5.426. [DOI] [PubMed] [Google Scholar]
- 8.Laurila JV, Pitkala KH, Strandberg TE, et al. Confusion assessment method in the diagnostics of delirium among aged hospital patients: Would it serve better in screening than as a diagnostic instrument? Int J Geriatr Psychiatry. 2002;17:1112–9. doi: 10.1002/gps.753. [DOI] [PubMed] [Google Scholar]
- 9.Fabbri RM, Moreira MA, Garrido R, et al. Validity and reliability of the Portuguese version of the Confusion Assessment Method (CAM) for the detection of delirium in the elderly. Arq Neuropsiquiatr. 2001;59:175–9. doi: 10.1590/s0004-282x2001000200004. [DOI] [PubMed] [Google Scholar]
- 10.Monette J, Galbaud du Fort G, Fung SH, et al. Evaluation of the Confusion Assessment Method (CAM) as a screening tool for delirium in the emergency room. Gen Hosp Psychiatry. 2001;23:20–5. doi: 10.1016/s0163-8343(00)00116-x. [DOI] [PubMed] [Google Scholar]
- 11.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286:2703–10. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 12.Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2001;29:1370–9. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Rolfson DB, McElhaney JE, Jhangri GS, et al. Validity of the confusion assessment method in detecting postoperative delirium in the elderly. Int Psychogeriatr. 1999;11:431–8. doi: 10.1017/s1041610299006043. [DOI] [PubMed] [Google Scholar]
- 14.Zou Y, Cole MG, Primeau FJ, et al. Detection and diagnosis of delirium in the elderly: psychiatrist diagnosis, confusion assessment method, or consensus diagnosis? Int Psychogeriatr. 1998;10:303–8. doi: 10.1017/s1041610298005390. [DOI] [PubMed] [Google Scholar]
- 15.Pompei P, Foreman M, Cassel CK, et al. Detecting delirium among hospitalized older patients. Arch Intern Med. 1995;155:301–7. [PubMed] [Google Scholar]
- 16.Rockwood K, Cosway S, Stolee P, et al. Increasing the recognition of delirium in elderly patients. J Am Geriatr Soc. 1994;42:252–6. doi: 10.1111/j.1532-5415.1994.tb01747.x. [DOI] [PubMed] [Google Scholar]
- 17.Adamis D, Treloar A, MacDonald AJ, et al. Concurrent validity of two instruments (the Confusion Assessment Method and the Delirium Rating Scale) in the detection of delirium among older medical inpatients. Age Ageing. 2005;34:72–5. doi: 10.1093/ageing/afi019. [DOI] [PubMed] [Google Scholar]
- 18.Inouye S, Foreman MD, Mion LC, et al. Nurses’ recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Arch Intern Med. 2001;161:2467–73. doi: 10.1001/archinte.161.20.2467. [DOI] [PubMed] [Google Scholar]
- 19.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–62. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 20.Lewis LM, Miller DK, Morley JE, et al. Unrecognized delirium in ED geriatric patients. Am J Emer Med. 1995;13:142–5. doi: 10.1016/0735-6757(95)90080-2. [DOI] [PubMed] [Google Scholar]
- 21.Dosa D, Intrator O, McNicoll L, et al. Preliminary derivation of a nursing home confusion assessment method based on data from the minimum data set. J Am Geriatr Soc. 2007;55:1099–1105. doi: 10.1111/j.1532-5415.2007.01239.x. [DOI] [PubMed] [Google Scholar]
- 22.McCusker J, Cole M, Bellavance F, Primeau F. Reliability and validity of a new measure of severity of delirium. Int Psychogeriatr. 1998;10:421–33. doi: 10.1017/s1041610298005493. [DOI] [PubMed] [Google Scholar]
- 23.Walker MP, Ayre GA, Cummings JL, et al. The clinician assessment of fluctuation and the one day fluctuation assessment scale. Two methods to assess fluctuating confusion in dementia. Br J Psychiatry. 2000;177:252–6. doi: 10.1192/bjp.177.3.252. [DOI] [PubMed] [Google Scholar]
- 24.McNicoll L, Pisani MA, Ely EW, et al. Detection of delirium in the intensive care unit: comparison of confusion assessment method for the intensive care unit with confusion assessment method ratings. J Am Geriatr Soc. 2005;53:495–500. doi: 10.1111/j.1532-5415.2005.53171.x. [DOI] [PubMed] [Google Scholar]
- 25.Jacobi J, Fraser GL, Coursin DB, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30:119–141. doi: 10.1097/00003246-200201000-00020. [DOI] [PubMed] [Google Scholar]
- 26.Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–76. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- 27.Marcantonio ER, Kiely DK, Simon SE, et al. Outcomes of older people admitted to postacute facilities with delirium. J Am Geriatr Soc. 2005;53:963–9. doi: 10.1111/j.1532-5415.2005.53305.x. [DOI] [PubMed] [Google Scholar]
- 28.Cole M, McCusker J, Dendukuri N, et al. The prognostic significance of subsyndromal delirium in elderly medical inpatients. J Am Geriatr Soc. 2003;51:754–60. doi: 10.1046/j.1365-2389.2003.51255.x. [DOI] [PubMed] [Google Scholar]
- 29.McCusker J, Cole MG, Dendukuri N, Belzile E. The delirium index, a measure of severity of delirium: new findings on reliability, validity, and responsiveness. J Am Geriatr Soc. 2004;52:1744–9. doi: 10.1111/j.1532-5415.2004.52471.x. [DOI] [PubMed] [Google Scholar]
- 30.Milisen K, Foreman MD, Abraham IL, et al. A nurse-led interdisciplinary intervention program for delirium in elderly hip fracture patients. J Am Geriatr Soc. 2001;49:523–32. doi: 10.1046/j.1532-5415.2001.49109.x. [DOI] [PubMed] [Google Scholar]
- 31.Gruber-Baldini AL, Zimmerman S, Morrison RS, et al. Cognitive impairment in hip fracture patients: timing of detection and longitudinal follow-up. J Am Geriatr Soc. 2003;51:1227–36. doi: 10.1046/j.1532-5415.2003.51406.x. [DOI] [PubMed] [Google Scholar]
- 32.Lin SM, Liu CY, Wang CH, et al. The impact of delirium on the survival of mechanically ventilated patients. Crit Care Med. 2004;32:2254–59. doi: 10.1097/01.ccm.0000145587.16421.bb. [DOI] [PubMed] [Google Scholar]
- 33.Lemiengre J, Nelis T, Joosten E, et al. Detection of delirium by bedside nurses using the confusion assessment method. J Am Geriatr Soc. 2006;54:685–9. doi: 10.1111/j.1532-5415.2006.00667.x. [DOI] [PubMed] [Google Scholar]
- 34.Laplante J, et al. Confusion Assessment Method: Validation d’une version française. Perspective Infermière. 2005 [PubMed] [Google Scholar]
- 35.Bickel H, Gradinger R, Kochs E, et al. Incidence and risk factors of delirium after hip surgery [German] Psychiatrische Praxis. 2004;31:360–5. doi: 10.1055/s-2004-828361. [DOI] [PubMed] [Google Scholar]
- 36.Grassi L, Caraceni A, Beltrami E, et al. Assessing delirium in cancer patients. The Italian versions of the delirium rating scale and the memorial delirium assessment scale. J Pain Sympt Manage. 2001;21:59–68. doi: 10.1016/s0885-3924(00)00241-4. [DOI] [PubMed] [Google Scholar]
- 37.Kawaguchi Y, Kanamori M, Ishihara H, et al. Postoperative delirium in spine surgery. Spine J. 2006;6:164–9. doi: 10.1016/j.spinee.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 38.Kudoh A, Takase H, Takahira Y, et al. Postoperative confusion increases in elderly long-term benzodiazepine users. Anesth Analg. 2004;99:1674–8. doi: 10.1213/01.ANE.0000136845.24802.19. [DOI] [PubMed] [Google Scholar]
- 39.Shigeta H, Yasui A, Nimura Y, et al. Postoperative delirium and melatonin levels in elderly patients. Am J Surg. 2001;182:449–54. doi: 10.1016/s0002-9610(01)00761-9. [DOI] [PubMed] [Google Scholar]
- 40.Akinci SB, Rezaki M, Ozdemir H, et al. Validity and reliability of Confusion Assessment Method for the Intensive Care Unit [Turkish] Turk Anesteziyologi ve Reanimasyon Dernegi Dergisi. 2005;33:333–41. [Google Scholar]
- 41.Kalisvaart KJ, Vreeswijk R, de Jonghe JFM, et al. Risk factors and prediction of postoperative delirium in elderly hip-surgery patients: Implementation and validation of a medical risk factor model. J Am Geriatr Soc. 2006;54:817–22. doi: 10.1111/j.1532-5415.2006.00704.x. [DOI] [PubMed] [Google Scholar]
- 42.Kakuma R, du Fort GG, Arsenault L, et al. Delirium in older emergency department patients discharged home: effect on survival. J Am Geriatr Soc. 2003;51:443–50. doi: 10.1046/j.1532-5415.2003.51151.x. [DOI] [PubMed] [Google Scholar]
- 43.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–62. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 44.Webster JR, Chew RB, Mailliard L, et al. Improving clinical and cost outcomes in delirium: use of practice guidelines and a delirium care team. Ann Long-Term Care. 1999;7:128–34. [Google Scholar]
- 45.Lacko L, Dellasega C, Salerno FA, et al. The role of the advanced practice nurse in facilitating a clinical research study. Screening for delirium. Clin Nurse Spec. 2000;14:110–8. doi: 10.1097/00002800-200005000-00005. [DOI] [PubMed] [Google Scholar]
- 46.Hustey FM, Meldon SW, Smith MD, et al. The effect of mental status screening on the care of elderly emergency department patients. Ann Emerg Med. 2003;41:678–84. doi: 10.1067/mem.2003.152. [DOI] [PubMed] [Google Scholar]
- 47.Pun BT, Gordon SM, Peterson JF, et al. Large-scale implementation of sedation and delirium monitoring in the intensive care unit: a report from two medical centers. Crit Care Med. 2005;33:1199–205. doi: 10.1097/01.ccm.0000166867.78320.ac. [DOI] [PubMed] [Google Scholar]
- 48.Rudolph JL, Jones RN, Grande LJ, et al. Impaired executive function is associated with delirium after coronary artery bypass surgery. J Am Geriatr Soc. 2006;54:937–41. doi: 10.1111/J.1532-5415.2006.00735.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Simon SE, Bergmann MA, Jones RN, et al. Reliability of a structured assessment for nonclinicians to detect delirium among new admissions to postacute care. J Am Med Dir Assoc. 2006;7:412–415. doi: 10.1016/j.jamda.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 50.Pisani MA, Araujo KL, VanNess PH, et al. A research algorithm to improve detection of delirium in the intensive care unit. Critical Care. 2006;10:R121. doi: 10.1186/cc5027. [DOI] [PMC free article] [PubMed] [Google Scholar]