Abstract
Background
The African population is composed of a variety of ethnic groups, which differ considerably from each other. Some studies suggest that ethnic variation may influence dating. The aim of the present study was to establish reference values for fetal age assessment in Cameroon using two different ethnic groups (Fulani and Kirdi).
Methods
This was a prospective cross sectional study of 200 healthy pregnant women from Cameroon. The participants had regular menstrual periods and singleton uncomplicated pregnancies, and were recruited after informed consent. The head circumference (HC), outer-outer biparietal diameter (BPDoo), outer-inner biparietal diameter and femur length (FL), also called femur diaphysis length, were measured using ultrasound at 12–22 weeks of gestation. Differences in demographic factors and fetal biometry between ethnic groups were assessed by t- and Chi-square tests.
Results
Compared with Fulani women (N = 96), the Kirdi (N = 104) were 2 years older (p = 0.005), 3 cm taller (p = 0.001), 6 kg heavier (p < 0.0001), had a higher body mass index (BMI) (p = 0.001), but were not different with regard to parity. Ethnicity had no effect on BPDoo (p = 0.82), HC (p = 0.89) or FL (p = 00.24). Weight, height, maternal age and BMI had no effect on HC, BPDoo and FL (p = 0.2–0.58, 0.1–0.83, and 0.17–0.6, respectively).
When comparing with relevant European charts based on similar design and statistics, we found overlapping 95% CI for BPD (Norway & UK) and a 0–4 day difference for FL and HC.
Conclusion
Significant ethnic differences between mothers were not reflected in fetal biometry at second trimester. The results support the recommendation that ultrasound in practical health care can be used to assess gestational age in various populations with little risk of error due to ethnic variation.
Background
Maternal and perinatal mortalities in sub-Saharan countries are among the highest in the world. In Cameroon the maternal mortality rate is 430 per 100 000 live births and the infant mortality rate 87 per 1000 under one year) [1]. Gestational age (GA) has emerged as one of the most important predictors of perinatal mortality and morbidity [2]. By combining GA and fundal height of the uterus, complications such as intra-uterine growth restriction (IUGR), oligohydramnion, macrosomia, multiple pregnancy and polyhydramnion may be identified [3]. Knowledge of GA is also a prerequisite in the management of conditions such as premature rupture of membranes, preterm labour, post dates, antepartum bleeding, preeclampsia etc.
Last menstrual period (LMP) is simple and the most common method of calculating GA. However, 45–68% of pregnant women have been reported to have irregular periods or uncertain information regarding their LMP. The ultrasonographic measurements of the fetal BPD is a more reliable method, predicting date of spontaneous delivery with greater certainty than even a certain LMP [4-7]. Ultrasound is particularly useful in parts of the world where women often cannot account for their LMP [8,9]. In Cameroon the illiteracy rate is 68% among people older than 15 years [1], and many of the pregnant women who attend hospital clinics do not know the exact date of their LMP, but they count completed months.
Biparietal diameter (BPD) is the most commonly used ultrasound measurement for fetal age assessment. Fetal age assessment in the second trimester can also be based on head circumference (HC) and femur length (FL). These methods are less influenced by maternal and fetal factors such as parity, age and fetal gender [10-15].
The African population is composed of a variety of ethnic groups, differing considerably from each other. Some studies suggest that population differences in fetal biometry are negligible and that separate studies are not essential [16,17]. Other studies however demonstrate morphometric variation among different population groups around the world [18-20] suggesting that ethnic variation may influence dating.
The aim of the present study was therefore to establish reference values for fetal age assessment in Cameroon using two different ethnic groups. We also wanted to determine the effect of maternal morphometry on the age assessment and to compare these new reference charts with other relevant charts.
Methods
This was a prospective cross sectional study of 200 pregnant women belonging to two different ethnic groups in the northern part of Cameroon: the Fulani people who are slender, and the Kirdi people who are in general stocky (Table 1). The participants were recruited from an antenatal clinic when they attended their routine prenatal care at 12–22 weeks of gestation. About 20 participants were recruited for each gestational week. The women were healthy with regular menstrual periods and certain information about LMP. They participated voluntarily after informed consent according to a protocol acknowledged by the hospital committee of Medical Research Ethics.
Table 1.
Comparison between Fulani (N = 96) and Kirdi (N = 104) according to height, weight, body mass index (BMI), maternal age (A = ANOVA test).
| Height | Mean | 95% Confidence Interval | p = 0.001 | |
| Fulani | 1.57 | 1.56 | 1.58 | |
| Kirdi | 1.595 | 1.585 | 1.605 | |
| Total | 1.58 | 1.57 | 1.59 | |
| Weight | Mean | 95% Confidence Interval | p < 0.0001 | |
| Fulani | 59.93 | 57.90 | 61.95 | |
| Kirdi | 65.87 | 63.93 | 67.82 | |
| Total | 62.90 | 61.50 | 64.30 | |
| BMI | Mean | 95% Confidence Interval | p = 0.001 | |
| Fulani | 24.03 | 23.26 | 24.80 | |
| Kirdi | 25.83 | 25.09 | 26.57 | |
| Total | 24.93 | 24.40 | 25.46 | |
| Age | Mean | 95% Confidence Interval | p = 0.005 | |
| Fulani | 25.32 | 24.19 | 26.45 | |
| Kirdi | 27.59 | 26.50 | 28.67 | |
| Total | 26.46 | 26.67 | 27.24 | |
One investigator (DS) trained at a Norwegian university hospital did all the ultrasound examinations using Shimasonic (Shimadzu) SDL-300, Japan, with a 3.5 MHz curvilinear probe.
Fetal head measurements were obtained in a horizintal section at the level of the thalamus and the cavum septi pellucidi [21]. Measurements of the biparietal diameter were obtained by placing the callipers at the outer border of the cranium on both sides (BPD outer-outer, BPDoo) and at the leading edges (BPD outer-inner, BPDoi). The occipital-frontal diameter (OFD) was measured between the leading edge of the frontal bone and the outer border of the occiput. Head circumference (HC) was estimated from the measurement of the OFD and the BPDoo using the formula π(BPD+OFD)/2 [21]. The fetal femur length (FL) was obtained in a longitudinal section by placing the calliper at the end of the diaphysis on both sides [22], also called the femur diaphysis length (FDL) [23]. For each parameter three measurements were used to calculate a mean.
Gestational age was calculated from the first day of the last menstrual period, and corrected for cycle length; i.e. corresponding number of days were added or subtracted according to menstrual cycle length shorter or longer than 28 days, respectively.
Statistics
The sample size was determined based on the power calculation and design of a corresponding previous study [24]. Fractional polynomial regression models were fitted to the data in order to construct the mean [24]. To construct the 2.5th, 5th, 10th, 25th, 75th, 90th, 95th, and 97.5th centiles, the method of scaled absolute residuals was applied [25]. Differences in demographic factors and fetal biometry between ethnic groups were assessed by t- and Chi-square tests. Continuous dependent variables were power transformed to normality were necessary. Intra-observer coefficient of variation was calculated based on the three repeat measurements of each parameter in all participants. The intra-observer variation was also analyzed as the intra-class correlation. The SPSS statistical package (SPSS, Chicago, IL, USA) was used, except for the intra-observer coefficient of variation, which was carried out according to the 'logarithmic method' of Bland [26].
Results
Table 1 and Table 2 show the characteristics of the total population and the comparison between the 96 Fulani and 104 Kirdi with regard to maternal age, height, weight, BMI and parity. Compared with the Fulani women, the Kirdi were two years older (p = 0.005), three cm taller (p = 0.001), six kg heavier (p < 0.0001), had a higher BMI (p = 0.001), but were not different with regard to parity. Seventy (35%) of all the women had never been to school and 162 (81%) of them were housewives, while only one (0.5%) of their husbands was unemployed. All the women were married.
Table 2.
Comparison between Fulani (N = 96) and Kirdi (N = 104) according to parity (B= Chi-square test)
| Parity | Fulani | Kirdi | Total | ||||
| n | % | N | % | n | % | ||
| 0 | 22 | 22.92 | 24 | 23.08 | 46 | 24.21 | Chi-square test: |
| 1 | 24 | 25.00 | 26 | 25.00 | 50 | 26.32 | P = 0.9 |
| 2 | 14 | 14.58 | 15 | 14.42 | 29 | 15.26 | |
| 3 | 13 | 13.54 | 10 | 9.62 | 23 | 12.11 | |
| 4 | 9 | 9.38 | 9 | 8.65 | 18 | 9.47 | |
| 5 | 14 | 14.58 | 20 | 19.23 | 34 | 17.90 |
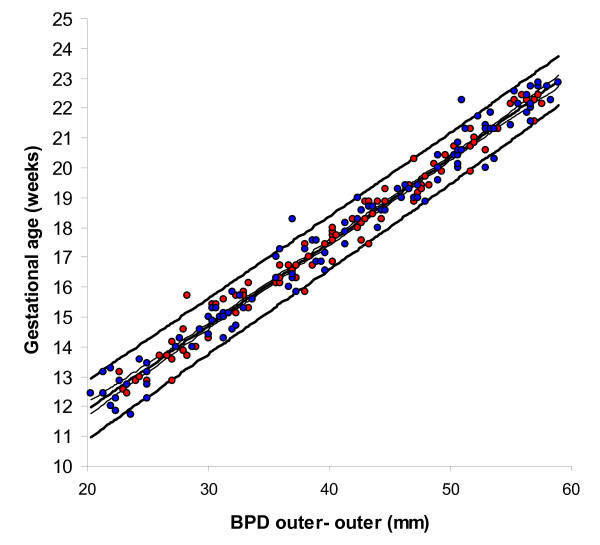
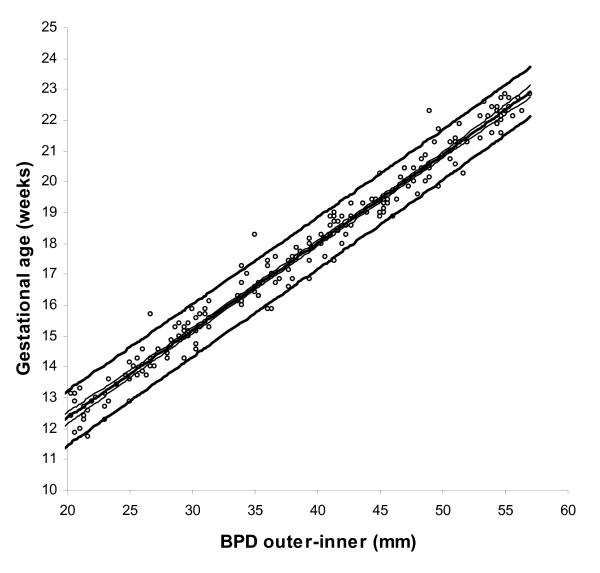
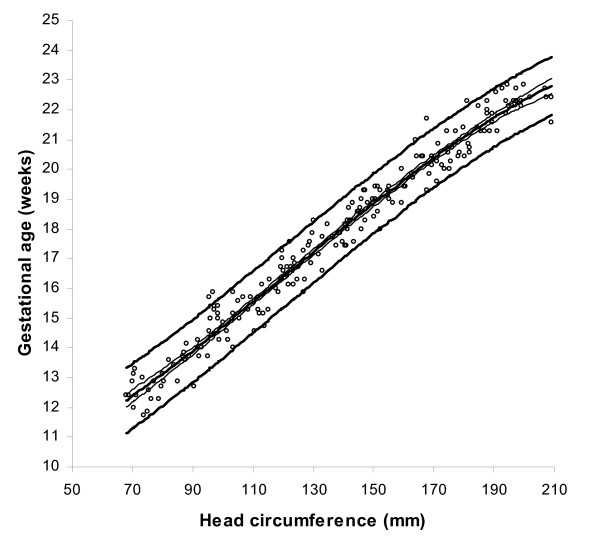
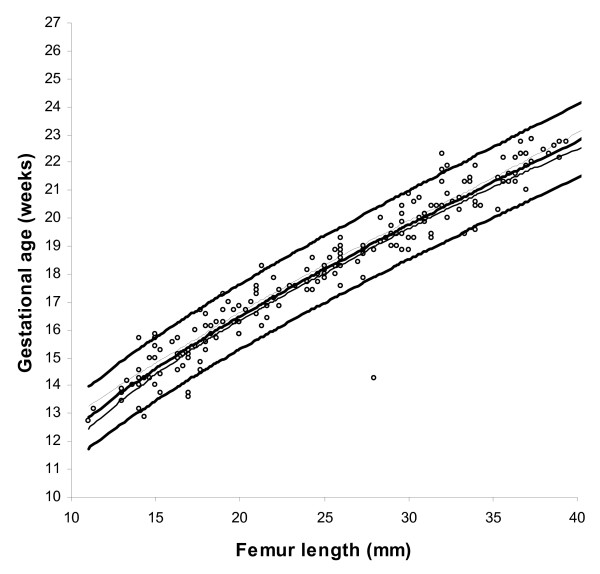
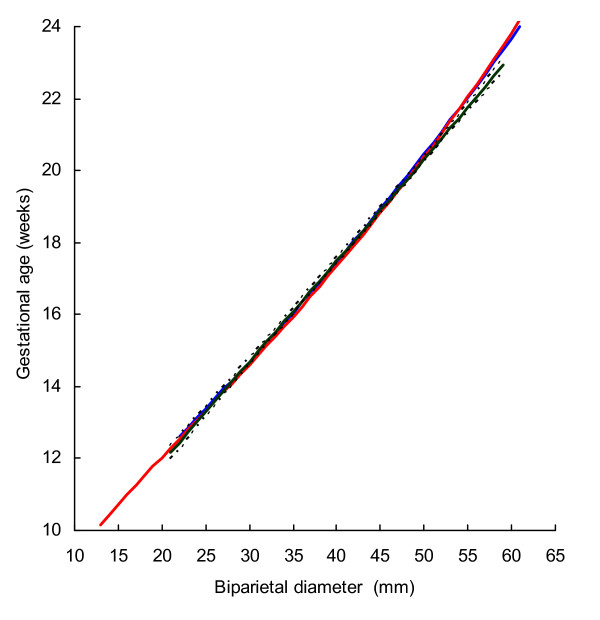
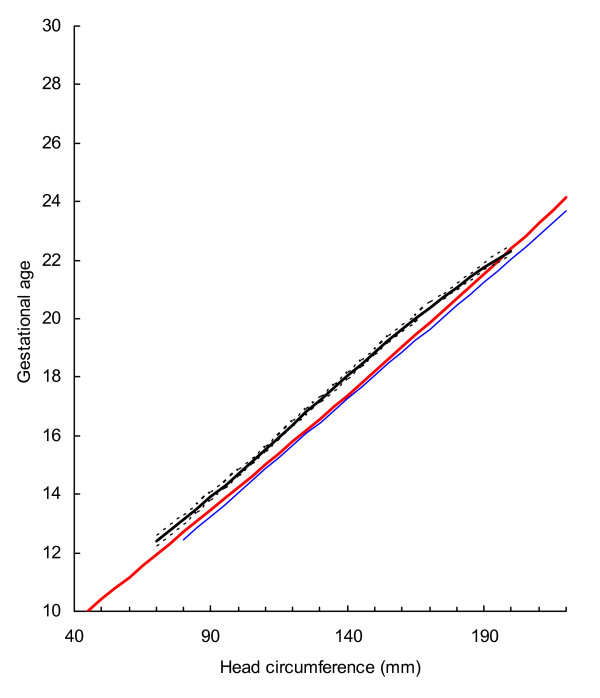
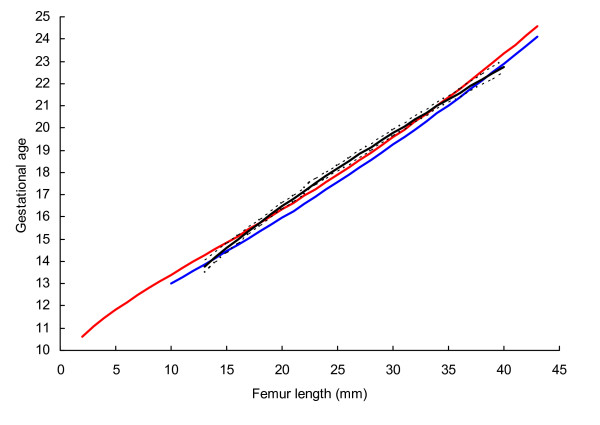
BPD, OFD and HC were successfully determined in all participants, while in 18 cases visualisation of the FL was not possible during early pregnancy. For the ethnic groups combined, raw data with fitted 2.5th, 50th and 97.5th centiles and 95% CI for mean gestational age as functions of BPDoo, BPDoi, HC and FL are presented in Figures 1, 2, 3, 4 and the corresponding charts for GA assessment according to biometrical measurements in Tables 3, 4, 5 and 6. Mean gestational age and standard deviation (SD) as functions of the anatomical parameters were: Mean gestational age (weeks)1.255 = 9.2309763061 + 0.6491253792 BPDoo (mm) + 0.0000166409 BPDoo3, SD = 1.1891063079 - 0.0000676577 BPDoo; mean gestational age (weeks)1.255 = 9.9633718109 + 0.6655891074 BPDoi (mm) + 0.0000165695 BPDoi3, SD = 1.0450011947 + 0.0018760334 BPDoi; mean gestational age (weeks)1.255 = 16.8857174784 + 0.0016547829 HC (mm)2 - 0.0000042242 HC3, SD = 1.2876967006 + 0.0004840074 HC and mean gestational age (weeks)1.255 = 1.2653359275 + 6.9440971709 FL (mm)0.5 + 0.0033225118 FL2, SD = 1.1872945587 + 0.0170042678 FL.
Figure 1.
Raw data with fitted centiles of gestational age (2.5th, 50th and 97.5th) by biparietal diameter (outer-outer) and 95% CI for the mean. Red dots are Fulani and blue dots Kirdi.
Figure 2.
Raw data with fitted centiles of gestational age (2.5th, 50th and 97.5th) by biparietal diameter (outer-inner)) and 95% CI for the mean.
Figure 3.
Raw data with fitted centiles of gestational age (2.5th, 50th and 97.5th) by head circumference and 95% CI for the mean.
Figure 4.
Raw data with fitted centiles of gestational age (2.5th, 50th and 97.5%) by femur length and 95% CI for the mean.
Table 3.
Gestational age assessment by biparietal diameter outer-outer (BPDoo)
| Centiles | ||||||
| 50th | 2.5th | 97.5th | ||||
| BPDoo (mm) | weeks | days | weeks | days | weeks | days |
| 20 | 11 | 6 | 10 | 6 | 12 | 6 |
| 21 | 12 | 1 | 11 | 1 | 13 | 0 |
| 22 | 12 | 3 | 11 | 3 | 13 | 2 |
| 23 | 12 | 5 | 11 | 5 | 13 | 4 |
| 24 | 13 | 0 | 12 | 0 | 13 | 6 |
| 25 | 13 | 2 | 12 | 2 | 14 | 1 |
| 26 | 13 | 4 | 12 | 4 | 14 | 3 |
| 27 | 13 | 5 | 12 | 6 | 14 | 5 |
| 28 | 14 | 0 | 13 | 1 | 15 | 0 |
| 29 | 14 | 2 | 13 | 3 | 15 | 2 |
| 30 | 14 | 4 | 13 | 5 | 15 | 4 |
| 31 | 14 | 6 | 14 | 0 | 15 | 6 |
| 32 | 15 | 1 | 14 | 2 | 16 | 1 |
| 33 | 15 | 3 | 14 | 4 | 16 | 3 |
| 34 | 15 | 5 | 14 | 6 | 16 | 5 |
| 35 | 16 | 0 | 15 | 1 | 16 | 6 |
| 36 | 16 | 2 | 15 | 3 | 17 | 1 |
| 37 | 16 | 4 | 15 | 5 | 17 | 3 |
| 38 | 16 | 6 | 16 | 0 | 17 | 5 |
| 39 | 17 | 1 | 16 | 2 | 18 | 0 |
| 40 | 17 | 3 | 16 | 4 | 18 | 2 |
| 41 | 17 | 5 | 16 | 6 | 18 | 4 |
| 42 | 18 | 0 | 17 | 1 | 18 | 6 |
| 43 | 18 | 2 | 17 | 3 | 19 | 1 |
| 44 | 18 | 4 | 17 | 5 | 19 | 3 |
| 45 | 18 | 6 | 18 | 0 | 19 | 5 |
| 46 | 19 | 1 | 18 | 2 | 20 | 0 |
| 47 | 19 | 3 | 18 | 4 | 20 | 2 |
| 48 | 19 | 5 | 18 | 6 | 20 | 4 |
| 49 | 20 | 0 | 19 | 1 | 20 | 6 |
| 50 | 20 | 2 | 19 | 3 | 21 | 1 |
| 51 | 20 | 4 | 19 | 5 | 21 | 3 |
| 52 | 20 | 6 | 20 | 0 | 21 | 5 |
| 53 | 21 | 1 | 20 | 2 | 22 | 0 |
| 54 | 21 | 3 | 20 | 4 | 22 | 2 |
| 55 | 21 | 5 | 20 | 6 | 22 | 4 |
| 56 | 22 | 0 | 21 | 1 | 22 | 6 |
| 57 | 22 | 2 | 21 | 3 | 23 | 1 |
| 58 | 22 | 4 | 21 | 5 | 23 | 3 |
Table 4.
Gestational age asssessment by biparietal diameter outer-inner (BPDoi)
| Centiles | ||||||
| 50th | 2.5th | 97.5th | ||||
| BPDoi (mm) | weeks | days | weeks | days | weeks | days |
| 20 | 12 | 2 | 11 | 3 | 13 | 1 |
| 21 | 12 | 4 | 11 | 5 | 13 | 3 |
| 22 | 12 | 6 | 12 | 0 | 13 | 5 |
| 23 | 13 | 1 | 12 | 2 | 14 | 0 |
| 24 | 13 | 3 | 12 | 4 | 14 | 2 |
| 25 | 13 | 5 | 12 | 6 | 14 | 4 |
| 26 | 14 | 0 | 13 | 1 | 14 | 6 |
| 27 | 14 | 2 | 13 | 3 | 15 | 1 |
| 28 | 14 | 4 | 13 | 5 | 15 | 3 |
| 29 | 14 | 6 | 14 | 0 | 15 | 5 |
| 30 | 15 | 1 | 14 | 2 | 16 | 0 |
| 31 | 15 | 3 | 14 | 4 | 16 | 2 |
| 32 | 15 | 5 | 14 | 6 | 16 | 4 |
| 33 | 16 | 0 | 15 | 1 | 16 | 6 |
| 34 | 16 | 2 | 15 | 3 | 17 | 1 |
| 35 | 16 | 4 | 15 | 5 | 17 | 3 |
| 36 | 16 | 6 | 16 | 0 | 17 | 5 |
| 37 | 17 | 1 | 16 | 2 | 17 | 6 |
| 38 | 17 | 3 | 16 | 4 | 18 | 1 |
| 39 | 17 | 5 | 16 | 6 | 18 | 3 |
| 40 | 18 | 0 | 17 | 1 | 18 | 5 |
| 41 | 18 | 2 | 17 | 3 | 19 | 0 |
| 42 | 18 | 4 | 17 | 5 | 19 | 2 |
| 43 | 18 | 6 | 18 | 0 | 19 | 4 |
| 44 | 19 | 1 | 18 | 2 | 19 | 6 |
| 45 | 19 | 3 | 18 | 4 | 20 | 1 |
| 46 | 19 | 5 | 18 | 6 | 20 | 3 |
| 47 | 20 | 0 | 19 | 1 | 20 | 5 |
| 48 | 20 | 2 | 19 | 3 | 21 | 0 |
| 49 | 20 | 4 | 19 | 5 | 21 | 2 |
| 50 | 20 | 6 | 20 | 0 | 21 | 4 |
| 51 | 21 | 1 | 20 | 2 | 21 | 6 |
| 52 | 21 | 3 | 20 | 4 | 22 | 1 |
| 53 | 21 | 5 | 20 | 6 | 22 | 3 |
| 54 | 22 | 0 | 21 | 1 | 22 | 5 |
| 55 | 22 | 2 | 21 | 3 | 23 | 1 |
| 56 | 22 | 4 | 21 | 5 | 23 | 3 |
| 57 | 22 | 6 | 22 | 0 | 23 | 5 |
| 58 | 23 | 1 | 22 | 2 | 24 | 0 |
Table 5.
Gestational age ssessment by head circumference (HC)
| Centiles | Centiles | ||||||||||||
| 50th | 2.5th | 97.5th | 50th | 2.5th | 97.5th | ||||||||
| HC (mm) | weeks | days | weeks | days | weeks | days | HC (mm) | weeks | days | weeks | days | weeks | days |
| 70 | 12 | 2 | 11 | 2 | 13 | 3 | 140 | 18 | 0 | 17 | 0 | 19 | 0 |
| 72 | 12 | 3 | 11 | 3 | 13 | 4 | 142 | 18 | 1 | 17 | 1 | 19 | 1 |
| 74 | 12 | 4 | 11 | 4 | 13 | 5 | 144 | 18 | 2 | 17 | 2 | 19 | 2 |
| 76 | 12 | 5 | 11 | 5 | 13 | 6 | 146 | 18 | 3 | 17 | 3 | 19 | 3 |
| 78 | 12 | 6 | 11 | 6 | 14 | 0 | 148 | 18 | 4 | 17 | 4 | 19 | 4 |
| 80 | 13 | 0 | 12 | 0 | 14 | 1 | 150 | 18 | 5 | 17 | 5 | 19 | 5 |
| 82 | 13 | 1 | 12 | 1 | 14 | 2 | 152 | 19 | 0 | 17 | 6 | 20 | 0 |
| 84 | 13 | 3 | 12 | 2 | 14 | 3 | 154 | 19 | 1 | 18 | 1 | 20 | 1 |
| 86 | 13 | 4 | 12 | 3 | 14 | 4 | 156 | 19 | 2 | 18 | 2 | 20 | 2 |
| 88 | 13 | 5 | 12 | 4 | 14 | 5 | 158 | 19 | 3 | 18 | 3 | 20 | 3 |
| 90 | 13 | 6 | 12 | 5 | 14 | 6 | 160 | 19 | 4 | 18 | 4 | 20 | 4 |
| 92 | 14 | 0 | 12 | 6 | 15 | 0 | 162 | 19 | 5 | 18 | 5 | 20 | 5 |
| 94 | 14 | 1 | 13 | 1 | 15 | 1 | 164 | 19 | 6 | 18 | 6 | 20 | 6 |
| 96 | 14 | 2 | 13 | 2 | 15 | 3 | 166 | 20 | 0 | 19 | 0 | 21 | 0 |
| 98 | 14 | 3 | 13 | 3 | 15 | 4 | 168 | 20 | 1 | 19 | 1 | 21 | 1 |
| 100 | 14 | 5 | 13 | 4 | 15 | 5 | 170 | 20 | 2 | 19 | 2 | 21 | 2 |
| 102 | 14 | 6 | 13 | 5 | 15 | 6 | 172 | 20 | 3 | 19 | 3 | 21 | 3 |
| 104 | 15 | 0 | 13 | 6 | 16 | 0 | 174 | 20 | 4 | 19 | 4 | 21 | 4 |
| 106 | 15 | 1 | 14 | 1 | 16 | 1 | 176 | 20 | 5 | 19 | 5 | 21 | 5 |
| 108 | 15 | 2 | 14 | 2 | 16 | 2 | 178 | 20 | 6 | 19 | 6 | 21 | 6 |
| 110 | 15 | 3 | 14 | 3 | 16 | 4 | 180 | 21 | 0 | 20 | 0 | 22 | 0 |
| 112 | 15 | 4 | 14 | 4 | 16 | 5 | 182 | 21 | 1 | 20 | 1 | 22 | 1 |
| 114 | 15 | 6 | 14 | 5 | 16 | 6 | 184 | 21 | 2 | 20 | 2 | 22 | 2 |
| 116 | 16 | 0 | 15 | 0 | 17 | 0 | 186 | 21 | 3 | 20 | 3 | 22 | 3 |
| 118 | 16 | 1 | 15 | 1 | 17 | 1 | 188 | 21 | 4 | 20 | 4 | 22 | 4 |
| 120 | 16 | 2 | 15 | 2 | 17 | 2 | 190 | 21 | 5 | 20 | 5 | 22 | 4 |
| 122 | 16 | 3 | 15 | 3 | 17 | 3 | 192 | 21 | 5 | 20 | 6 | 22 | 5 |
| 124 | 16 | 5 | 15 | 4 | 17 | 5 | 194 | 21 | 6 | 20 | 6 | 22 | 6 |
| 126 | 16 | 6 | 15 | 5 | 17 | 6 | 196 | 22 | 0 | 21 | 0 | 23 | 0 |
| 128 | 17 | 0 | 16 | 0 | 18 | 0 | 198 | 22 | 1 | 21 | 1 | 23 | 1 |
| 130 | 17 | 1 | 16 | 1 | 18 | 1 | 200 | 22 | 2 | 21 | 2 | 23 | 2 |
| 132 | 17 | 2 | 16 | 2 | 18 | 2 | 202 | 22 | 3 | 21 | 3 | 23 | 2 |
| 134 | 17 | 3 | 16 | 3 | 18 | 3 | 204 | 22 | 3 | 21 | 3 | 23 | 3 |
| 136 | 17 | 4 | 16 | 4 | 18 | 5 | 206 | 22 | 4 | 21 | 4 | 23 | 4 |
| 138 | 17 | 6 | 16 | 6 | 18 | 6 | 208 | 22 | 5 | 21 | 5 | 23 | 5 |
| 210 | 22 | 5 | 21 | 6 | 23 | 5 | |||||||
Table 6.
Gestational age assessment by femur length (FL)
| Centiles | ||||||
| 50th | 2.5th | 97.5th | ||||
| FL (mm) | weeks | days | Weeks | days | weeks | days |
| 11 | 11 | 5 | 12 | 0 | 13 | 6 |
| 12 | 12 | 1 | 12 | 4 | 14 | 3 |
| 13 | 12 | 4 | 13 | 0 | 14 | 6 |
| 14 | 13 | 0 | 13 | 3 | 15 | 2 |
| 15 | 13 | 3 | 13 | 5 | 15 | 5 |
| 16 | 13 | 5 | 14 | 1 | 16 | 0 |
| 17 | 14 | 1 | 14 | 4 | 16 | 3 |
| 18 | 14 | 4 | 14 | 6 | 16 | 6 |
| 19 | 14 | 6 | 15 | 2 | 17 | 1 |
| 20 | 15 | 2 | 15 | 4 | 17 | 4 |
| 21 | 15 | 4 | 16 | 0 | 17 | 6 |
| 22 | 15 | 6 | 16 | 2 | 18 | 2 |
| 23 | 16 | 2 | 16 | 5 | 18 | 4 |
| 24 | 16 | 4 | 17 | 0 | 19 | 0 |
| 25 | 16 | 6 | 17 | 2 | 19 | 2 |
| 26 | 17 | 1 | 17 | 4 | 19 | 4 |
| 27 | 17 | 4 | 18 | 0 | 20 | 0 |
| 28 | 17 | 6 | 18 | 2 | 20 | 2 |
| 29 | 18 | 1 | 18 | 4 | 20 | 4 |
| 30 | 18 | 3 | 18 | 6 | 20 | 6 |
| 31 | 18 | 5 | 19 | 1 | 21 | 2 |
| 32 | 19 | 0 | 19 | 3 | 21 | 4 |
| 33 | 19 | 2 | 19 | 5 | 21 | 6 |
| 34 | 19 | 4 | 20 | 1 | 22 | 1 |
| 35 | 19 | 6 | 20 | 3 | 22 | 3 |
| 36 | 20 | 2 | 20 | 5 | 22 | 5 |
| 37 | 20 | 4 | 21 | 0 | 23 | 1 |
| 38 | 20 | 6 | 21 | 2 | 23 | 3 |
| 39 | 21 | 1 | 21 | 4 | 23 | 5 |
| 40 | 21 | 3 | 21 | 6 | 24 | 0 |
In supplementary analyzes, we compared z-scores of gestational age in the two ethnical groups. For both groups, mean z-scores for each anatomical parameter was non-different from zero (General Linear Models, SPSS). Nor did inclusion of ethnicity as an independent variable in the functions, which describe the estimated mean gestational age, reveal significant effects. Mean z-scores of gestational age as function of HC in Fulani and Kirdi women were -0.02 (95% CI: -0.22, 0.18), SD 0.98, and 0.02 (95% CI: -0.19, 0.22), SD 1.05, respectively. Correspondingly, mean z-scores of gestational age according to BPDoo in Fulani and Kirdi were 0.00 (95% CI: -0.19, 0.19), SD 0.92, and 0.00 (95% CI: -0.22, 0.23), SD 1.15, respectively. For BPDoo mean gestational age z-scores in Fulani and Kirdi women were -0.02 (95% CI: -0.21, 0.17), SD 0.94 and 0.02 (95% CI: -0.21, 0.25), SD 1.18, respectively. For FL mean gestational age z-scores in Fulani and Kirdi women were -0.12 (95% CI: -0.39, 0.15), SD 1.30 and 0.12 (95% CI: -0.08, 0.32), SD 0.97, respectively.
Prediction of gestational age from BPD (22–59 mm) was fairly similar in three studies using outer-outer measurement technique (Fig 5). In practical terms, differences in predicted gestational age between the British and the Norwegian studies compared with the present study ranged from -0.03 to 0.4 weeks and -0,2 to 0.5 weeks, respectively. The 95% CI for the mean in the present study generally overlapped with the means of the other two studies. Predicted gestational age in the present study from HC (80–200 mm) was generally higher than those in the British and the Norwegian (Fig. 6). The difference from the British and the Norwegian studies ranged from -0.7 to -0.3 and -0.7 to 0.07 weeks, respectively. Predictions of gestational age from FL (13–40 mm) in the present and the Norwegian studies were similar and the difference ranged from -0.3 to 0.6 weeks (Fig. 7). However, predicted gestational age in the British study was generally lower than in the present (difference -0.6 to -0.1 weeks). The 95% CI for the mean in the present study generally overlapped with the mean in the Norwegian study. Design and statistical methods are comparable in these three studies. The 5th and 95th centiles were used to reflect uncertainty of gestational age estimation in the three methods (Table 7).
Figure 5.
The 50th centile for biparietal diameter (outer-outer) with 95% confidence interval in the present study compared with those of Altman and Chitty (blue line)[10]and Johnsen et al (red line)[14].
Figure 6.
The 50th centile for head circumference with 95% confidence interval in the present study compared with those of Altman and Chitty (blue line)[10]and Johnsen et al (red line)[14].
Figure 7.
The 50th centile for femur length with 95% confidence interval in the present study compared with those of Altman and Chitty (blue line)[10]and Johnsen et al (red line)[15].
Table 7.
Uncertainty of gestational age assessment, expressed as the distance between the 5th and 95th centile, when using outer-outer biparietal diameter (BPDoo), head circumference (HC) and femur length (FL) based on the present study, the study of Altman and Chitty [10] and that of Johnsen et al. [14]
| Present study | Altman and Chitty | Johnsen et al | |||||
| Measurement | 50th centile | Uncertainty | 50th centile | Uncertainty | 50th centile | Uncertainty | |
| (mm) | (weeks + days) | (± days) | (weeks + days) | (± days) | (weeks + days) | (± days) | |
| BPDoo | 22 | 12 + 3 | 6 | 12 + 4 | 7 | 12 + 3 | 6 |
| 50 | 20 + 2 | 5 | 20 + 3 | 13 | 20 + 2 | 9 | |
| HC | 90 | 13 + 6 | 6 | 13 + 2 | 5 | 13 + 3 | 6 |
| 180 | 21 + 0 | 6 | 20 + 5 | 10 | 20 + 4 | 8 | |
| FL | 14 | 14 + 1 | 7 | 14 + 1 | 7 | 14 + 3 | 6 |
| 32 | 20 + 2 | 8 | 20 + 0 | 11 | 20 + 2 | 8 | |
In Tables 8, 9 and 10 the effects of maternal characteristics on fetal age assessment are presented. There was no significant effect of weight, height, maternal age or BMI on fetal biometry, but parity seemed to increase fetal BPDoo for the first three babies (p = 0.01), but not for HC or FL (p = 0.01, 0.27 and 0.11, respectively).
Table 8.
Effects of maternal ethnicity, weight, height, body mass index (BMI), parity, and age on biparietal diameter outer – outer (BPDoo)
| Maternal factor | Mean | 95%CI | SD | p-value | |
| Ethnicity | 0.82 | ||||
| Fulani | 40.52 | 40.19 | 40.85 | 9.8 | |
| Kirdi | 40.47 | 40.15 | 40.78 | 11.2 | |
| Weight (centiles) | 0.39 | ||||
| < 10 | 40.30 | 39.64 | 40.97 | 10.1 | |
| 10–90 | 40.44 | 40.18 | 40.69 | 10.6 | |
| 90+ | 41.11 | 40.40 | 41.83 | 10.6 | |
| Height (centiles) | 0.83 | ||||
| < 10 | 40.47 | 39.77 | 41.17 | 9.7 | |
| 10–90 | 40.54 | 40.27 | 40.80 | 10.7 | |
| 90+ | 40.25 | 39.64 | 40.86 | 10.6 | |
| BMI (centiles) | 0.33 | ||||
| < 10 | 40.47 | 39.74 | 41.19 | 8.5 | |
| 10–90 | 40.44 | 40.19 | 40.69 | 10.7 | |
| 90+ | 40.91 | 40.19 | 41.63 | 10.7 | |
| Parity | 0.01 | ||||
| 0 | 38.67 | 37.97 | 39.38 | 11.4 | |
| 1 | 39.04 | 38.39 | 39.69 | 10.1 | |
| 2 | 39.70 | 38.85 | 40.55 | 11.2 | |
| 3 | 40.41 | 39.55 | 41.27 | 11.5 | |
| 4 | 39.45 | 38.51 | 40.40 | 10.3 | |
| 5+ | 39.99 | 39.12 | 40.87 | 9.3 | |
| Age | 0.10 | ||||
| -19 | 40.25 | 39.16 | 41.35 | 12.3 | |
| 20–24 | 39.98 | 39.37 | 40.58 | 10.4 | |
| 25–29 | 39.53 | 39.01 | 40.06 | 10.0 | |
| 30–34 | 38.55 | 37.81 | 39.28 | 11.9 | |
| 35+ | 39.41 | 38.28 | 40.55 | 9.7 | |
Table 9.
Effects of maternal ethnicity, weight, height, body mass index (BMI), parity, and age on head circumference (HC)
| Maternal factor | Mean | 95%CI | SD | p-value | |
| Ethnicity | 0.89 | ||||
| Fulani | 136.59 | 135.21 | 137.97 | 36.6 | |
| Kirdi | 136.46 | 135.13 | 137.78 | 40.4 | |
| Weight (centiles) | 0.22 | ||||
| < 10 | 135.47 | 132.66 | 138.27 | 39.4 | |
| 10–90 | 136.30 | 135.23 | 137.37 | 38.2 | |
| 90+ | 139.45 | 136.43 | 142.46 | 39.0 | |
| Height (centiles) | 0.58 | ||||
| < 10 | 136.10 | 133.17 | 139.03 | 37.5 | |
| 10–90 | 137.05 | 135.95 | 138.14 | 39.6 | |
| 90+ | 134.00 | 131.46 | 136.55 | 39.6 | |
| BMI (centiles) | 0.20 | ||||
| < 10 | 135.68 | 132.62 | 138.73 | 32.9 | |
| 10–90 | 136.42 | 135.35 | 137.49 | 38.8 | |
| 90+ | 138.19 | 135.16 | 141.22 | 38.1 | |
| Parity | 0.27 | ||||
| 0 | 132.01 | 129.21 | 134.81 | 41.8 | |
| 1 | 131.25 | 128.68 | 133.82 | 36.3 | |
| 2 | 132.64 | 129.26 | 136.02 | 40.9 | |
| 3 | 135.78 | 132.38 | 139.17 | 40.8 | |
| 4 | 132.05 | 128.30 | 135.81 | 40.0 | |
| 5+ | 134.50 | 131.04 | 137.97 | 34.0 | |
| Age | 0.34 | ||||
| -19 | 134.81 | 130.45 | 139.16 | 45.6 | |
| 20–24 | 134.26 | 131.85 | 136.66 | 38.1 | |
| 25–29 | 132.09 | 130.00 | 134.17 | 36.7 | |
| 30–34 | 132.44 | 129.52 | 135.36 | 43.1 | |
| 35+ | 131.60 | 127.09 | 136.11 | 33.9 | |
Analysis of variance (ANOVA), adjustments for gestational age.
Parity and age were adjusted for each other.
Table 10.
Effects of maternal ethnicity, weight, height, body mass index (BMI), parity, and age on fetal femur length (FL)
| Maternal factor | Mean | 95%CI | SD | p-value | |
| Ethnicity | 0.24 | ||||
| Fulani | 24.53 | 22.89 | 26.17 | 7.7 | |
| Kirdi | 25.79 | 24.18 | 27.41 | 8.0 | |
| Weight (centiles) | 0.20 | ||||
| < 10 | 23.33 | 19.95 | 26.72 | 8.4 | |
| 10–90 | 25.26 | 23.96 | 26.57 | 7.8 | |
| 90+ | 26.53 | 22.97 | 30.08 | 7.8 | |
| Height (centiles) | 0.22 | ||||
| < 10 | 24.05 | 20.66 | 27.44 | 8.4 | |
| 10–90 | 25.18 | 23.84 | 26.52 | 7.8 | |
| 90+ | 26.04 | 22.99 | 29.09 | 7.6 | |
| BMI (centiles) | 0.60 | ||||
| < 10 | 21.61 | 17.99 | 25.24 | 7.3 | |
| 10–90 | 25.45 | 24.17 | 26.73 | 7.7 | |
| 90+ | 26.42 | 22.89 | 29.95 | 8.3 | |
| Parity | 0.11 | ||||
| 0 | 23.95 | 23.02 | 24.88 | 8.7 | |
| 1 | 24.21 | 23.37 | 25.05 | 7.7 | |
| 2 | 24.77 | 23.62 | 25.92 | 7.7 | |
| 3 | 23.88 | 22.77 | 24.99 | 5.6 | |
| 4 | 24.63 | 23.40 | 25.86 | 8.2 | |
| 5+ | 25.63 | 24.53 | 26.73 | 7.4 | |
| Age | 0.17 | ||||
| -19 | 25.32 | 23.91 | 26.74 | 8.6 | |
| 20–24 | 24.91 | 24.15 | 25.66 | 7.8 | |
| 25–29 | 24.62 | 23.98 | 25.27 | 7.9 | |
| 30–34 | 23.99 | 23.03 | 24.96 | 8.3 | |
| 35+ | 23.71 | 22.27 | 25.15 | 7.1 | |
Analysis of variance (ANOVA), adjustments for gestational age.
Parity and age were adjusted for each other.
The intra-observer variation, calculated as the coefficient of variation for BPDoo, BPDoi, HC and FL was 2.7 (95% CI 2.5–2.9), 2.7 (2.6–2.9), 3.8 (2.8–3.3) and 3.1 (2.8–3.3), respectively. The corresponding intra-class correlation was 99.1% (95% CI 98.9–99.3), 99.2 (99.0–99.4), 98.4 (97.9–98.7) and 99.3 (99.11–99.4), respectively.
Discussion
We have established reference charts for gestational age assessment using three fetal ultrasonographic measurements in an African population composed of two different ethnic groups. We have shown that significant morphometric ethnic differences had no significant influence on gestational age assessment. The charts are in agreement with European charts based on corresponding design and statistics.
Although ethnic groups (Kirdi and Fulani) differed significantly with respect to maternal age, height, weight and BMI (Table 1) we found no significant impact of ethnicity on fetal size at 12–22 weeks of gestation (Tables 8, 9 and 10). Additionally, supplementary analyses revealed no significant difference in distributions of z-scores of BPD, HC, or FL. Nor did we find any significant effects of ethnicity on predicted gestational age. These findings are very helpful in a country such as Cameroon, which has a variety of ethnic groups. It would be impractical to use different charts for all these groups. However, other studies [18-20] report clinically significant inter-ethnic morphometric differences, and a study among a multi-ethnic population in USA suggested accordingly that ethnicity and sex difference should be take into consideration to improve the accuracy of ultrasound estimation of GA [19]. However, we compared our new charts with those established for a Caucasian population and a mixed population in Europe [10,14,15] (Figures 5, 6 and 7) and found agreement for BPDoo-charts, the most commonly used measurement for this purpose. The method of assessing HC was different in Cameroon compared to the European studies (estimating circumference based on BPD and OFD compared to tracing or adjusting an ellipse to the fetal skull), which may explain some of the variance (Fig 6). The slightly different curvature of the means (Figures 6 and 7) may reflect that the fitted regression line would be different for the short time span of the present data compared the longer span of the other two studies.
As for FL there was no difference compared with the Norwegian study (95% CI overlapped). These two studies used identical insonation and measurement techniques as all ultrasound operators had been trained in the same unit, but then applied this technique using different machines in different countries. In general, FL charts vary more from study to study than the fetal head biometry, which probably reflects an uncertainty in defining the landmarks for the femoral diaphysis. We believe the small differences compared with the British charts are due to measurement technique, since study design and statistical methods were otherwise identical.
We have previously shown that morphometric differences at 18 weeks of gestation are related to body composition at birth [27]. Here we show that the ethnic impact on fetal morphometry at this stage of pregnancy is insignificant in the context of assessing gestational age. We acknowledge that ethnic differences are expressed during fetal development, but then mainly during the latter half of pregnancy. However, ethnical differences in mid gestation have been found for femur measurements in some studies [10,18-20], and we therefore recommend fetal age assessment in the second trimester to be based primarily on fetal head-measurements.
The impact of weight, height, maternal age, and BMI on fetal biometry, was non-existent in the present study or so small that it can be ignored before 22 weeks of gestation. There was a significant effect of parity on BPDoo, but since there was no effect on HC and FL it may well be due to chance. A study of normal pregnancies in Papua New Guinea found that fetal biometry was hardly affected by socio-demographic characteristics, weight gain during pregnancy or the height of the mother [3]; which is in line with the present findings.
In the present study all participants were married and lived with their husband, a sign of couple's stability. Although most of the women were housewives and dependent on their husbands, at least one member of the couple had income. This does not reflect the general population where more than 30% are believed to be unemployed, and this suggests that our study population was skewed. The fact that we included only women who knew their LMP probably augmented this skewed distribution as destitute pregnant women tend not to know their LMP and are therefore more likely to be excluded from the study. Recently established WHO standards for infant growth included children from optimal socioeconomic backgrounds at different locations around the world[28]. The present study should then be in line with such guidelines.
This study can be criticised for lacking perinatal data. We could not collect the outcomes of pregnancy as this would have necessitated the investigator's presence at the study site for a longer period. Home birth is common and would have resulted in numerous dropouts. Secondly, if growth deviation or other complications had occurred, we would not have excluded these participants [24]. Constructing reference charts by excluding participants for complications occurring after enrolment is not considered prudent, and carries the risk of constructing "supernormal" reference charts that are not applicable for women with complications.
Conclusion
In countries such as Cameroon where the illiteracy is very high (68%) [1], only a few women know the date of their LMP. In general, even when educated, many women do not remember, or are uncertain of the date of their LMP [29]. Most pregnant women come to their first consultation around three months of gestation or later. GA assessed at this stage forms the base for growth assessment during the rest of the pregnancy and prediction of expected date of delivery. This study provides the tool for assessing GA by fetal biometry and makes it possible to determine IUGR and prematurity in Cameroon and other African populations. Although ultrasound machines are not readily available in antenatal care in developing countries, we believe that accurately assessed GA in risk groups would be important information at a time when ultrasound becomes increasingly available in these countries.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
DS contributed to conception and design of the study, acquisition of data, interpretation of data, revision of the manuscript, and approved the final version. TK contributed to conception and design of the study, analysis and interpretation of data, helped to draft the manuscript, and approved the final version. SR contributed to conception and design of the study, analysis and interpretation of data, helped to draft the manuscript, and approved the final version. SLJ contributed to analysis and interpretation of data, drafted the manuscript, and approved the final version.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
The Centre for International Health and the Norwegian State Loan Fund for Education funded Daniel Salpou's research fellowship.
Svein Rasmussen and Torvid Kiserud were under their institutional payrolls.
Western Norway Regional Health Authority funded Synnøve Lian Johnsen's research fellowship.
Department of Obstetrics and Gynecology at Haukeland University Hospital provided office facilities, equipment and clerical support.
Contributor Information
Daniel Salpou, Email: danielsalpou@yahoo.fr.
Torvid Kiserud, Email: torvid.kiserud@kk.uib.no.
Svein Rasmussen, Email: svein.rasmussen@mfr.uib.no.
Synnøve Lian Johnsen, Email: synnove.johnsen@helse-bergen.no.
References
- Statistics in Cameroon. 2005. http://www.unicef.org/infobycountry/cameroon_statistics.html
- Markestad T, Kaaresen PI, Ronnestad A, Reigstad H, Lossius K, Medbo S, Zanussi G, Engelund IE, Skjaerven R, Irgens LM. Early death, morbidity, and need of treatment among extremely premature infants. Pediatrics. 2005;115:1289–1298. doi: 10.1542/peds.2004-1482. [DOI] [PubMed] [Google Scholar]
- Amoa AB, Wapi J, Klufio CA. Longitudinal fetal biometry of normal pregnant Melanesian Papua New Guineans to construct standards of reference for Papua New Guinea. P N G Med J. 1993;36:219–227. [PubMed] [Google Scholar]
- Waldenstrom U, Axelsson O, Nilsson S. A comparison of the ability of a sonographically measured biparietal diameter and the last menstrual period to predict the spontaneous onset of labor. Obstet Gynecol. 1990;76:336–338. [PubMed] [Google Scholar]
- Tunon K, Eik-Nes SH, Grottum P. A comparison between ultrasound and a reliable last menstrual period as predictors of the day of delivery in 15,000 examinations. Ultrasound Obstet Gynecol. 1996;8:178–185. doi: 10.1046/j.1469-0705.1996.08030178.x. [DOI] [PubMed] [Google Scholar]
- Nguyen TH, Larsen T, Engholm G, Moller H. Evaluation of ultrasound-estimated date of delivery in 17,450 spontaneous singleton births: do we need to modify Naegele's rule? Ultrasound Obstet Gynecol. 1999;14:23–28. doi: 10.1046/j.1469-0705.1999.14010023.x. [DOI] [PubMed] [Google Scholar]
- Mongelli M, Wilcox M, Gardosi J. Estimating the date of confinement: ultrasonographic biometry versus certain menstrual dates. Am J Obstet Gynecol. 1996;174:278–281. doi: 10.1016/S0002-9378(96)70408-8. [DOI] [PubMed] [Google Scholar]
- Okupe RF, Coker OO, Gbajumo SA. Assessment of fetal biparietal diameter during normal pregnancy by ultrasound in Nigerian women. Br J Obstet Gynaecol. 1984;91:629–632. doi: 10.1111/j.1471-0528.1984.tb04821.x. [DOI] [PubMed] [Google Scholar]
- Mounanga M, Ngou-Mve-Ngou JP, Desrentes M, Zinsou RD. [Ultrasonics and fetal growth in Gabon] J Gynecol Obstet Biol Reprod (Paris) 1988;17:37–43. [PubMed] [Google Scholar]
- Altman DG, Chitty LS. New charts for ultrasound dating of pregnancy. Ultrasound Obstet Gynecol. 1997;10:174–191. doi: 10.1046/j.1469-0705.1997.10030174.x. [DOI] [PubMed] [Google Scholar]
- Chervenak FA, Skupski DW, Romero R, Myers MK, Smith-Levitin M, Rosenwaks Z, Thaler HT. How accurate is fetal biometry in the assessment of fetal age? Am J Obstet Gynecol. 1998;178:678–687. doi: 10.1016/S0002-9378(98)70477-6. [DOI] [PubMed] [Google Scholar]
- Hadlock FP, Deter RL, Harrist RB, Park SK. Fetal head circumference: relation to menstrual age. AJR Am J Roentgenol. 1982;138:649–653. doi: 10.2214/ajr.138.4.649. [DOI] [PubMed] [Google Scholar]
- Law RG, MacRae KD. Head circumference as an index of fetal age. J Ultrasound Med. 1982;1:281–288. doi: 10.7863/jum.1982.1.7.281. [DOI] [PubMed] [Google Scholar]
- Johnsen SL, Rasmussen S, Sollien R, Kiserud T. Fetal age assessment based on ultrasound head biometry and the effect of maternal and fetal factors. Acta Obstet Gynecol Scand. 2004;83:716–723. doi: 10.1111/j.0001-6349.2004.00485.x. [DOI] [PubMed] [Google Scholar]
- Johnsen SL, Rasmussen S, Sollien R, Kiserud T. Fetal age assessment based on femur length at 10–25 weeks of gestation, and reference ranges for femur length to head circumference ratios. Acta Obstet Gynecol Scand. 2005;84:725–733. doi: 10.1111/j.0001-6349.2005.00691.x. [DOI] [PubMed] [Google Scholar]
- Borgida AF, Zelop C, Deroche M, Bolnick A, Egan JF. Down syndrome screening using race-specific femur length. Am J Obstet Gynecol. 2003;189:977–979. doi: 10.1067/S0002-9378(03)00657-4. [DOI] [PubMed] [Google Scholar]
- Ruvolo KA, Filly RA, Callen PW. Evaluation of fetal femur length for prediction of gestational age in a racially mixed obstetric population. J Ultrasound Med. 1987;6:417–419. doi: 10.7863/jum.1987.6.8.417. [DOI] [PubMed] [Google Scholar]
- Kovac CM, Brown JA, Apodaca CC, Napolitano PG, Pierce B, Patience T, Hume RF, Jr, Calhoun BC. Maternal ethnicity and variation of fetal femur length calculations when screening for Down syndrome. J Ultrasound Med. 2002;21:719–722. doi: 10.7863/jum.2002.21.7.719. quiz 724-715. [DOI] [PubMed] [Google Scholar]
- Davis RO, Cutter GR, Goldenberg RL, Hoffman HJ, Cliver SP, Brumfield CG. Fetal biparietal diameter, head circumference, abdominal circumference and femur length. A comparison by race and sex. J Reprod Med. 1993;38:201–206. [PubMed] [Google Scholar]
- Shipp TD, Bromley B, Mascola M, Benacerraf B. Variation in fetal femur length with respect to maternal race. J Ultrasound Med. 2001;20:141–144. doi: 10.7863/jum.2001.20.2.141. [DOI] [PubMed] [Google Scholar]
- Campbell S, Thoms A. Ultrasound measurement of the fetal head to abdomen circumference ratio in the assessment of growth retardation. Br J Obstet Gynaecol. 1977;84:165–174. doi: 10.1111/j.1471-0528.1977.tb12550.x. [DOI] [PubMed] [Google Scholar]
- Goldstein RB, Filly RA, Simpson G. Pitfalls in femur length measurements. J Ultrasound Med. 1987;6:203–207. doi: 10.7863/jum.1987.6.4.203. [DOI] [PubMed] [Google Scholar]
- Deter RL, Rossavik IK, Hill RM, Cortissoz C, Hadlock FP. Longitudinal studies of femur growth in normal fetuses. J Clin Ultrasound. 1987;15:299–305. doi: 10.1002/jcu.1870150502. [DOI] [PubMed] [Google Scholar]
- Altman DG, Chitty LS. Charts of fetal size: 1. Methodology. Br J Obstet Gynaecol. 1994;101:29–34. doi: 10.1111/j.1471-0528.1994.tb13006.x. [DOI] [PubMed] [Google Scholar]
- Royston P, Wright EM. How to construct 'normal ranges' for fetal variables. Ultrasound Obstet Gynecol. 1998;11:30–38. doi: 10.1046/j.1469-0705.1998.11010030.x. [DOI] [PubMed] [Google Scholar]
- How should I calculate a within-subject coefficient of variation? http://www-users.york.ac.uk/~mb55/meas/cv.htm
- Rasmussen S, Kiserud T, Albrechtsen S. Foetal size and body proportion at 17–19 weeks of gestation and neonatal size, proportion, and outcome. Early Human Development. 2006;82:683–690. doi: 10.1016/j.earlhumdev.2006.01.010. [DOI] [PubMed] [Google Scholar]
- Who Multicentre Growth Reference Study Group Enrolment and baseline characteristics in the WHO Multicentre Growth Reference Study. Acta pædiatrica Supplement. 2006;7:7. doi: 10.1111/j.1651-2227.2006.tb02371.x. [DOI] [PubMed] [Google Scholar]
- Geirsson RT, Busby-Earle RM. Certain dates may not provide a reliable estimate of gestational age. Br J Obstet Gynaecol. 1991;98:108–109. doi: 10.1111/j.1471-0528.1991.tb10323.x. [DOI] [PubMed] [Google Scholar]