Abstract
Purpose
How medical students learn and develop the characteristics associated with good teaching in medicine is not well known. Information about this process can improve the academic preparation of medical students for teaching responsibilities. The purpose of this study was to determine how different experiences contributed to the knowledge, skills, and attitudes of medical school graduates and students regarding medical teaching.
Methods
A questionnaire was developed, addressing reliability and validity considerations, and given to first year residents and third year medical students (taught by those residents). Completed questionnaires were collected from 76 residents and 110 students (81% of the sample group). Item responses were analysed using descriptive and inferential statistics.
Results
Most residents (n = 54; 71%) positively viewed opportunities they had to practice teaching when they were seniors. Residents rated three activities for learning to teach highest: (1) observing teachers as they teach; (2) reviewing the material to be taught; and (3) directly teaching students; representing both individual and participatory ways of learning. Residents' self ratings of teaching behaviours improved over time and this self assessment by the residents was validated by the students' responses. Comparison between residents' self ratings and students' views of typical resident teaching behaviours showed agreement on levels of competence, confidence, and motivation. The students rated characteristics of enthusiasm, organisation, and fulfilment lower (p<0.002) than residents rated themselves.
Conclusions
The residents and students in this study viewed academic preparation for teaching responsibilities positively and showed agreement on characteristics of good teaching that may be helpful indicators in the process of developing medical teachers.
Keywords: medical education, undergraduate; medical education, internship and residency; teaching methods; experiential learning; educational techniques
The field of medical education encompasses the development, support, and administration of physician training within the broader context of health care systems.1,2 Medical educators and clinicians alike recognise the growing importance of preparing future physicians as teachers.3,4 Physicians are expected to engage in lifelong learning; to teach themselves and others, to disseminate health care information to students, patients, and staff.5,6,7 These concomitant responsibilities underscore the need to develop physicians as knowledgeable, skilled teachers as well as competent clinicians.
The formal objectives of teaching preparation programmes/curriculum in medical schools include (1) advancing knowledge of education principles, (2) increasing skills in teaching behaviours and (3) expanding attitudes about teaching and learning in medicine.8,9 Although researchers have studied the results of such programmes, how medical students actually learn about and develop the characteristics associated with good teaching in medicine is not well known.10,11,12 Information about this process can improve the academic preparation of medical students and prepare them to face their future teaching responsibilities.
To focus early in the process of developing as a medical teacher, this study explored how a group of first year residents (as recent medical school graduates) viewed the preparation for teaching that they received in medical school. What do those who are in the early stages of teaching clinical medicine think about different learning to teach experiences that they have had. As a cross‐check of the residents' views, third year medical students were also surveyed about their experiences to determine if there was agreement between the two groups about teaching skills, preparation for teaching, and characteristics of teachers that support a good medical education experience. The purpose of this study was to investigate views of medical school graduates and students about processes that influence the development of medical teachers.
Methods
This study used survey methodology to examine the perceptions of first year residents (PGY‐1) and third year medical students (MS3) taught by the PGY‐1 residents. The study sample was drawn from a large midwestern medical school and its affiliated medical centre. All PGY‐1s (n = 100) from the 11 departments with intern posts and the MS3 students attending one class session (n = 127; 96% of the whole class) enrolled at the study site were recruited to participate. Study participants were surveyed using a questionnaire to identify characteristics of effective teaching and demographic data (sex and age).13,14 Follow up interviews with PGY‐1 volunteers were held to expand on the questionnaire responses and interpretation.15
Subjects
A good response rate was obtained for both groups. One hundred and eighty six participants completed the study with 76 (76%) of the PGY‐1 group and 110 (87%) of the MS3 group. Seven PGY‐1 subjects completed an interview session (50% of those that volunteered to be interviewed). Missing data were identified as missing values in statistical analysis and other than eight MS3 forms with incomplete sections on the back of the form, missing data were sporadic. Twenty one PGY‐1 (28%) indicated that they had completed a formal programme on learning to teach during medical school. While a review of the demographic information cannot completely rule out differences between those who responded and those who did not, as best as can be determined the participants were representative of the study sample.
Questionnaire development
The quantitative questionnaire developed for this study was used to ascertain the perceptions of recent medical school graduates' and medical students' regarding their educational experiences as they relate to preparation for their role as teachers. As such, it was titled the medical education teaching readiness questionnaire or METRQ. Information sources used in establishing the validity of the questionnaire were (1) research in the fields of teaching theory, learning methods, and medical education, (2) medical student teaching activities at the study site, and (3) content review by several groups of experts in medical education and higher education survey research.9,16,17,18,19,20,21,22,23 Table 1 shows the primary study variables along with corresponding question topics. The final draft of the METRQ was critiqued by several experienced medical educators to assess the validity of the tool and the degree to which the questionnaire operationalised the stated research goals. The authors will provide a copy of the METRQ PGY‐1and MS3 versions for interested readers.
Table 1 Primary study variables for preparation to teach with corresponding METRQ question topics.
| Study variable | Question topic |
|---|---|
| Teaching instruction | Did you participate in the following experiences during medical school? |
| practised teaching senior year | |
| received feedback on teaching skills | |
| had a formal learning to teach programme | |
| Ways of learning | How helpful were the following activities during your senior year to prepare you for teaching as a resident? |
| received instruction about how to teach | |
| read printed materials about how to teach | |
| reviewed the material to be taught | |
| observed my teachers teach | |
| taught other students | |
| reflected on teaching experiences | |
| received feedback on teaching skills | |
| was encouraged to assume a teaching role | |
| had teaching responsibilities | |
| Teaching preparedness | Rate your preparedness in these four teaching skills. |
| planning what to teach | |
| presenting material | |
| providing feedback | |
| evaluating the student | |
| Teacher characteristics | When did you learn the most about how to teach? |
| How do you view yourself as a teacher at each of three time points? | |
| at the beginning of medical school | |
| at graduation | |
| ending PGY‐1 year | |
| Teaching functions | What teaching activities have you done with students? |
| What is your residency programme type? | |
| Attitudes about teaching | Would you have liked a different level of practice teaching in medical school? |
| Rate the importance of medical schools to include preparation in these teaching skills? | |
| planning what to teach | |
| presenting material | |
| providing feedback | |
| evaluating the student | |
| Do you agree or disagree with medical teaching proverbs? |
To determine reliability of question items, the METRQ was pilot tested with two related sample groups on‐site: second and third year residents (n = 16) and senior medical students (n = 6). After completing the questionnaire, participants were asked to comment on the relevance of question items and task difficulty (that is, appropriateness of items and options, clarity, accuracy, and estimated completion time). A systematic review of the subjects' responses confirmed that METRQ items reflected learning to teach experiences and readiness and established that item responses were complete and varied. Conceptually related items were analysed using Cronbach's α to determine the intercorrelations of the items for possible use as index measures. Analysis of the list of teaching skills yielded a Cronbach α of 0.86 with six of eight items contributing. The outcome with the complete list of six teaching characteristics was a Cronbach α of 0.73. These results showed the questions concerning learning about teaching and teaching characteristics showed internal consistency comprising index measures of teaching development. Lastly, minor adjustments in wording and format to improve clarity of the items were made that had little probability of affecting the questionnaire in a significant way.
Data collection
Data collection occurred during mid to late spring of the academic year. With the support of individual programme directors, the METRQ was given at PGY‐1 resident meetings or, when group sessions were not feasible, a resident was designated to distribute and collect the questionnaire. The researcher presented the METRQ to all MS3 students in attendance at the final session of a class. For both groups, the purpose of this study was explained without any particular incentives for completing the questionnaire or penalty for declining to complete the questionnaire. Participants completed the questionnaires without any self identification. As responses were completely voluntary and confidential, the reasons why some residents and students chose not to complete the questionnaire are not known.
The researcher conducted interviews with a subset of the PGY‐1 participants (n = 7) privately in her office at times convenient for each interviewee. Care was taken in the procedures for collecting and analysing interview data to ensure that participants' perspectives were represented. Efforts to control for potential investigator bias with each interviewing phase included: (1) a semi‐structured format and encouragement of participants' freeform comments; (2) audio‐recording of the graduate's views on how academic experiences influenced development of teaching knowledge, skills, and attitudes; and (3) solicitation of the graduates' interpretations of general results from the METRQ.
The institutional review board at the site of the investigation approved the study design, both resident and student versions of the METRQ questionnaire, data analysis, and presentation of results. No external or internal funding sources provided financial support for this research.
Data analysis
Questionnaire data were analysed using descriptive and inferential statistics with the Statistical Package for the Social Sciences (SPSS version 10.1). An α level of 0.05 was used and all tests of significance were two tailed. The confidence interval used to estimate the range for population means was 95%. The statistical analyses included tests of significance to detect a difference on METRQ responses (χ2, Fisher's exact test, analysis of variance), to examine a relation (Pearson's product moment correlation), to compare groups (t tests, independent samples test), and to make predictions based on response patterns (regression analysis). The reliability of identified question sets was evaluated with Cronbach's α to develop a composite index for groups of variables (for example, teaching skill preparedness, teacher characteristics). The general linear model for repeated measures was used to analyse the PGY‐1 measures of teaching characteristics over three time points.
The procedures for analysing qualitative data, as outlined by Marshall and Rossman, guided interpretation of the interview transcripts.24 The qualitative portion of this research offered PGY‐1 perspectives of greater depth, than can be found from a questionnaire process and, to some extent, informed interpretation of the METRQ results. The analysis and validity of the results were improved through the use of data triangulation methodology described by Creswell et al.25 With data triangulation, it was possible to use the information collected from participants at different levels in the teaching‐learning exchange combined with the two different survey methods that were used in the study. For the purposes of this paper, largely, the quantitative results are reported.
Results
The findings presented here comprise baseline characteristics and perceptions of teaching preparation from this group of residents and students. Demographic information is reported first, then results from the residents' responses to METRQ items, followed by comparisons between the two groups.
The average age of the PGY‐1 residents was 28.0 (SD 3.5) years and of the MS3s, average age was 25.5 (SD 1.9) years. Forty four of the subjects in the PGY‐1 group were male and 32 were female. Of the MS3 participants 54 were male, 48 female; and eight not specified. As a class, the medical students were slightly higher in distribution of men than women (53% v 47%) and predominately white (88%).
Preparation for medical teaching
Most PGY‐1s (n = 54; 71%) positively viewed practice teaching they performed as students. Logically, those who participated in a formal teaching programme had a higher frequency of practice teaching (χ2 = 30.134, df = 4, p = 0.0001). As assessed using Fisher's exact test, formal teaching programme participants (n = 20) were also more likely to have received feedback on their teaching skills (p = 0.02). Every respondent who taught as a senior indicated a preference for the same or greater teaching practice, especially if accompanied by feedback on teaching skills. Most of those who responded that more teaching practice would have been helpful (20 of 29) had teaching experience at the lower levels (from 1 to 6 opportunities compared with from 7 to 10 and beyond). Of the PGY‐1s with practice teaching experience, 23 (43%) indicated that the feedback they received could have been more helpful.
The PGY‐1s viewed both individual and participatory ways of learning to teach to be beneficial, as shown in table 2. They rated the helpfulness of nine different activities on their development as teachers and each activity received at least one response rating of 7 (extremely helpful). The three activities with the highest ratings were (1) observed my teachers teach, (2) reviewed the material to be taught, and (3) taught other students. For three of the four activities with mean ratings in the midpoint range, a large proportion of residents indicated this activity was not available (ANA) to them: (1) received feedback on teaching skills (26% ANA); (2) received instructions about how to teach (32% ANA); and (3) read printed materials about how to teach (34% ANA). Although the activity, reflected on teaching experiences, was widely observed (91%), it also had just a midpoint rating for helpfulness. Reliability analysis, with seven of the nine learning activities contributing yielded a standardised α of 0.75 suggesting that this item provides an index measurement of ways of learning to teach.
Table 2 Summary of the PGY‐1 subjects' ratings (mean (SD)) on the “Helpfulness of different ways of learning to teach” question item.
| Learning activities | Rating* | Range* | Number | n for ANA† |
|---|---|---|---|---|
| Observed my teachers teach (P) | 6.2 (0.87) | 3–7 | 76 | 0 |
| Reviewed the material to be taught (I) | 5.8 (0.97) | 3–7 | 70 | 6 |
| Taught other students (P) | 5.6 (1.18) | 3–7 | 66 | 7 |
| Had teaching responsibilities (P) | 5.4 (1.45) | 1–7 | 68 | 8 |
| Was encouraged to assume teaching (P) | 5.3 (1.30) | 1–7 | 64 | 11 |
| Received feedback on teaching skills (P) | 4.9 (1.47) | 1–7 | 56 | 20 |
| Reflected on teaching experiences (I) | 4.8 (1.48) | 1–7 | 69 | 6 |
| Received instruction about how to teach (I) | 4.3 (1.56) | 1–7 | 52 | 24 |
| Read printed materials about how to teach (I) | 3.5 (1.54) | 1–7 | 50 | 26 |
(P), participatory activity; (I), individual activity. *Numeric rating scale where 1 = not at all helpful and 7 = extremely helpful; †ANA, activity not available; n = number.
Teaching characteristics
The PGY‐1s indicated their self rating on teaching characteristics over three time points (first year medical student, graduation from medical school, and ending the PGY‐1 year). Six pairs of contrasting adjectives represented the characteristics of interest: bored v enthusiastic; ineffective v competent; fearful v confident; disorganised v organised; frustrated v fulfilled; and unmotivated v motivated. The location of positive and negative descriptors was alternated to limit bias and encourage individual consideration of each response. Participants indicated their self rating for each teaching characteristic by placing a mark on a line drawn between each adjective pair. See table 3 for the results of self ratings of teaching and statistical testing of repeated measures. Most self ratings increased during the medical school period (n = 72, df 2, p<0.05). Except for the adjective motivated, where as a group, PGY‐1s had high levels at the start of medical school, showed comparatively small increases over medical school and almost no increase over the PGY‐1 year. Reliability analysis completed on self ratings for the PGY‐1 year yielded a standardised α of 0.76 showing a relation between these teaching adjectives. Thus, the resident's rating for each descriptive adjective was combined to yield a total self rating score.
Table 3 Multivariate and pairwise comparisons of 72 PGY‐1 subjects' responses on the “Self ratings on teaching adjectives over time” question item.
| Adjective pair | Rating* at time points | Pairwise comparisons (p value) | |||
|---|---|---|---|---|---|
| First year | Graduate | Intern | 1st year v graduate | Graduate v PGY‐1 | |
| Bored v enthusiastic | 4.64 (1.88) | 5.59 (1.39) | 5.71 (1.14) | 0.000 | 0.605 |
| Ineffective v competent | 4.18 (1.93) | 5.12 (1.59) | 5.23 (1.57) | 0.002 | 0.695 |
| Fearful v confident | 3.97 (1.79) | 4.85 (1.52) | 5.21 (1.61) | 0.002 | 0.075 |
| Disorganised v organised | 4.07 (1.71) | 5.19 (1.37) | 5.30 (1.44) | 0.000 | 0.596 |
| Frustrated v fulfilled | 3.95 (1.40) | 4.77 (1.34) | 4.78 (1.62) | 0.000 | 0.884 |
| Unmotivated v motivated | 4.69 (1.80) | 4.99 (1.74) | 5.05 (1.81) | 0.074 | 1.00 |
*Numeric rating scale where least positive = 1 and most positive = 7.
Graduates' ratings of teaching variables
The PGY‐1s completed several items that covered different aspects of their teaching: (1) their preparedness with teaching skills; (2) their self rating of teaching characteristics (noted above); and (3) their attitudes about learning to teach. Firstly, the PGY‐1s' ratings of their teaching skills (see study variable 3 in table 1) performed as a variable of teaching preparedness. The ratings on four main skills were combined to obtain a total preparedness score for each resident. With these five items (four skill ratings and the combined score) considered, the standardised α was 0.80; confirming that the graduates' self perceived preparedness with teaching skills acted as an index measure.
Next, the PGY‐1s' response patterns for the main findings of this study supported the proposed teaching variables. For example, the total self rating score and the total preparedness score were positively correlated (n = 73) with an r value of 0.300 and p value = 0.01 (Pearson's product moment correlation coefficient). One way analysis of variance of the level of practice teaching showed increased practice was positively associated with preparedness in the teaching skill planning (F(4,69) = 3.906; p = 0.006). As a group, the graduates who experienced formal learning to teach disagreed more with the attitude statement “good teachers are born not made” (t 2.1;df 67;p = 0.039).
Comparison of teaching experiences
The METRQ items prompted respondents to answer in general terms regarding multiple teaching encounters between interns and third year students. Firstly, medical students and the residents who taught them showed the highest agreement on an item that asked for types of teaching activities that they engaged in together. Both groups listed teaching activities that they shared similarly, such as writing orders (PGY‐1 = 63%; MS3 = 58%) and charting notes (PGY‐1 = 47%; MS3 = 46%). Both groups indicated the least frequent teaching activities were case presentations and patient education (20%–33%). Teaching with new patient evaluation had an occurrence rate of 59% for PGY‐1 compared with 40% for MS3 and this difference was significant (Fisher's exact test; p = 0.019).
Next, both groups rated the importance of including four key teaching skills in the medical school curriculum and the residents' preparedness in these areas (item three in table 1) using a numeric scale (where 1 = not at all to 7 = extremely). The mean ratings of learning teaching skills in medical school were similar both groups (ranging from 5.9 for giving feedback to 4.64 for planning). However, the importance of these four teaching skills was typically rated 1.5 points higher than the PGY‐1s' preparedness level with each skill. Also, the independent samples test showed a significant difference between groups regarding the PGY‐1s' preparedness with these teaching skills at p<0.01 (df 183, 181, 181, 178). For example, the PGY‐1 mean rating (SD) for skill with giving feedback was 4.38 (1.40) compared with a mean (SD) of only 3.48 (1.52) from the MS3 group on this resident skill.
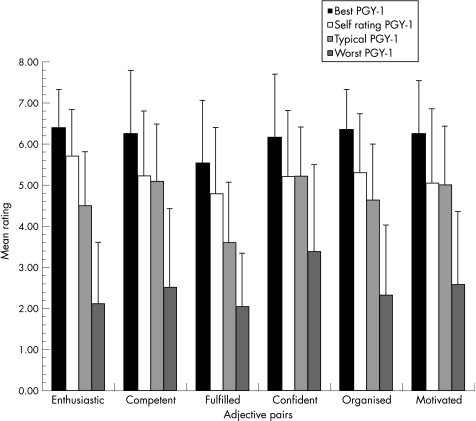
Thirdly, MS3s rated their resident teachers on the six sets of contrasting adjectives for teaching characteristics of the typical PGY‐1 teacher, and to offer ratings for the best and the worst teachers. Students showed a clear variance between best and worst PGY‐1 teacher on the six teaching characteristics (fig 1). Reliability testing for the scale of teaching adjectives was strongest for the best PGY‐1 teacher with a standardised α of 0.82 (typical: standardised α of 0.66; worst: standardised α of 0.73).
Figure 1 Ratings on teaching adjectives by PGY‐1 residents and MS3 students. Responses were provided on a seven point scale with least positive = 1 and most positive = 7.
The MS3s' rating of the typical PGY‐1 teacher was quite similar to the PGY‐1 self ratings on three adjectives, competence, confidence, and motivation. However, MS3s' ratings for enthusiasm, organisation, and fulfilled were lower (mean differences of 0.66–1.2 lower), showing the students viewed these characteristics less positively than the PGY‐1 self ratings. Results of one way analysis of variance testing between the two groups identified a significant difference for those three adjective pairs (p<0.002). The students' views of teaching actions that did not match the graduates' perceptions were also interesting.
Limitations of the study
The focus of this research was confined to participants' perceptions of medical teaching preparation in the early stages of their education at one site and thus how these results apply generally is not known. Graduates and students may be limited in their abilities to distinguish the effects of experiences that contributed to their sense about and skills with teaching. Without formal training in teaching (72% of this sample), it may be hard for these graduates to interpret learning to teach activities. Also, although the study participants may be considered representative of this sample group of PGY‐1 and MS3, the questionnaire and interviews were restricted to one site. The findings from this pilot study, through multiple data collection methods and data sources provide the basis to pursue this exploration of medical teacher preparation in a more general way.
Discussion
The perceptions of these medical school students and graduates uniquely contribute to the literature on preparing medical educators concerning what promoted their preparation to teach and what was lacking that could be improved. Participants from this study considered medical school an important time for preparation to teach and identified activities that support teaching development. Medical school may provide a safe environment for experimenting with instructional principles and medical curriculum while practising teaching and receiving feedback as found in teacher education.16,26,27 Responses from both groups showed their awareness that teaching activities occur in residency and the teacher‐learner relationship that existed between PGY‐1s and MS3s. This is consistent with the findings by Bing‐You and Sproul in a study of medical students and residents as teachers.28 The responses on the METRQ support the start of learning about teaching in medical school for immediate benefit to the students, as well. Also, potential gaps merit attention; the reliance on teaching role models while instruction and feedback on teaching were sometimes not available and the limited emphasis on patient education activities.
The graduates reported that both individual and participatory ways of learning to teach were helpful activities. For learning as an individual or cognitive activity, experiences such as reviewing the material to be taught and being instructed on teaching were helpful. This sentiment was echoed during the interviews, as the PGY‐1s emphasised that as students, first they needed to understand what they were teaching, before they could think about how to teach it. Alternatively, PGY‐1s also considered learning as part of a participatory or social realm, such as being encouraged to teach and receiving feedback on teaching. These study results were consistent with the circumstances for good teaching described by Salomon and Perkins.18 Both the cognitive processes and social realm of learning may improve medical teaching skill development.
As suggested by medical educators, preparation for medical teaching may increase overall competence in the profession.3,7,17 However, there is discrepancy in how educators describe the process—especially as to when learning to teach is beneficial. The variability in types of learning activities that contribute to becoming a medical teacher reported by these PGY‐1s and MS3s may explain some of the difference in outlooks. Some consider teaching a natural outcome of participating in the medical education environment and others deem individual study of teaching to be important. Both types of learning were reflected in the activities rated by these residents as helpful; with observing their teachers teach, studying the material to be taught, and practise teaching with feedback at the top of the list.
Conclusions
This study provides information about the process and perception of teaching knowledge, skills, and attitudes in this group of medical trainees. Many experiences were reported to support learning to teach. Although students are discerning consumers of medical teaching, at the novice stage of teaching, self reflection was only somewhat helpful, showing that self learning to teach may not be sufficient. Attention to the activities that promote learning to teach may improve the process during medical school and residency.
Medical school curriculums and other programmes that rely on learning through clinical teaching or the apprenticeship model can build on this information to prepare students for their teaching roles. Future studies suggested by this research are administration of METRQ at other sites and verification of teaching development variables. Along with practise teaching and feedback, the list of positive teaching characteristics has implications for teaching programme development. Graduates' and medical students' input about teaching and learning about teaching may help define outcome measures of instructional interventions. Further study may increase educators' understandings of how a combination of learning experiences can be optimised to positively influence students' development as teachers.
Footnotes
Funding: none.
Competing interests: none.
References
- 1.Ludmerer K M.A time to heal: American medical education from the turn of the century to the era of managed care. Oxford: Oxford University Press, 1999
- 2.Watson R T. Rediscovering the medical school. Acad Med 200378659–665. [DOI] [PubMed] [Google Scholar]
- 3.Association of American Medical Colleges ( A A M C ) Physicians for the twenty‐first century: report of the project panel on the general professional education of the physician and college preparation for medicine. J Med Educ 1984111–33. [PubMed] [Google Scholar]
- 4.Armstrong E G, Doyle J, Bennett N L. Transformative professional development of physicians as educators: assessment of a model. Acad Med 200378702–708. [DOI] [PubMed] [Google Scholar]
- 5.PEW Health Professions Commission Recreating health professional practice for a new century. San Francisco: Pew Health Professions Commission, 1998
- 6.Accreditation Council for Graduate Medical Education ( A C G M E. Institutional requirements. http://www.acgme.org (accessed 30 Jul 2005)
- 7.Liaison Committee on Medical Education ( L C M E ) Learning objectives for medical student education: guidelines for medical schools. http://www.aamc.org/meded/msop/start.htm (accessed 30 Jul 2005)
- 8.Westberg J, Jason H.Collaborative clinical education: the foundation of effective health care. Vol 16. New York: Springer Medical Education, 1993
- 9.Wilkerson L A, Irby D M. Strategies for improving teaching practices: a comprehensive approach to faculty development. Acad Med 199873387–396. [DOI] [PubMed] [Google Scholar]
- 10.Greenberg L W, Jewett L S. Preparing medical students to teach: an educational program using three approaches. Med Teach 19879409–414. [DOI] [PubMed] [Google Scholar]
- 11.Sasson V A, Blatt B, Kallenberg G.et al Teach 1, do 1 … better: superior communication skills in senior medical students serving as standardized patient‐examiners for junior peers. Acad Med 199974932–937. [DOI] [PubMed] [Google Scholar]
- 12.Field M, Burke J, Lloyd D.et al Peer‐assisted learning in clinical examination. Lancet 2004363490–491. [DOI] [PubMed] [Google Scholar]
- 13.Clifford C. How we use questionnaires for learner evaluation of clinical experiences. Med Teach 199214139–148. [DOI] [PubMed] [Google Scholar]
- 14.Marriott D J, Litzelman D K. Teaching the teachers: Is it effective? Acad Med 199873S72–S74. [DOI] [PubMed] [Google Scholar]
- 15.Creswell J W, Goodchild L F, Turner P P, Smart J C. Integrated qualitative and quantitative research: Epistemology, history, and designs. In: ed. Higher education: handbook of theory and research. Vol 11. New York: Agathon Press, 199790–136.
- 16.Bruffee K A.Collaborative learning: higher education, interdependence, and the authority of knowledge. Baltimore, MD: Johns Hopkins University Press, 1993
- 17.Fagan M J, Curry R H, Gallagher S J. The evolving role of the acting internship in the medical school curriculum. Am J Med 1998104409–412. [DOI] [PubMed] [Google Scholar]
- 18.Salomon G, Perkins D N, In Pearson P D, Iran‐Nejad A. Individual and social aspects of learning. eds. Review of Research in education. Washington, DC: American Educational Research Association, 1998
- 19.Shulman L S. Knowledge and teaching: foundations of the new reform. Harvard Educ Rev 1987571–22. [Google Scholar]
- 20.McKeachie W H.Teaching tips: strategies for research and theory for college and university teachers. Lexington, MA: DC Heath, 1994
- 21.Griffith C H, Wilson J F, Haist S A.et al Medical students and housestaff: partners in learning. Acad Med 199873S57–S59. [DOI] [PubMed] [Google Scholar]
- 22.Shulman L S, Hutchings P. Inventing the future. In: ed. Opening lines: approaches to the scholarship of teaching and learning. Menlo Park, CA: Carnegie, 200095–105.
- 23.Whitman N E, Schenk T L.The physician as teacher. Salt Lake City, UT: Whitman, 1997
- 24.Marshall C, Rossman G B.Designing qualitative research. 3rd ed. Thousand Oaks, CA: Sage, 1999
- 25.Creswell J W, Goodchild L F, Turner P P. Integrated qualitative and quantitative research: epistemology, history, and designs. In: Smart JC, ed. Higher education: handbook of theory and research. Vol 11. New York: Agathon Press, 1996
- 26.Feldman K A. The superior college teacher from the student's view. Research in Higher Education 1976543–88. [Google Scholar]
- 27.Major C, Pines R.Teaching to teach: new partnerships in teacher education. Washington, DC: National Education Association, 1999
- 28.Bing‐You R G, Sproul M S. Medical students' perceptions of themselves and residents as teachers. Medical Teacher 199214133–138. [DOI] [PubMed] [Google Scholar]