Abstract
Context: Obesity results from a prolonged small positive energy balance, and its treatment needs to reverse this imbalance.
Evidence Acquisition: Citations retrieved from PubMed and The Handbook of Obesity 2008 were selected to illustrate the points.
Evidence Synthesis: Many different diets have been tried to treat obesity, and weight loss occurs with all of them. There is currently no evidence that clearly supports a superiority of one macronutrient composition for diets used for weight loss. The principal effect seems to be the degree of adherence to the prescribed calorie reduction. Lifestyle strategies to modify eating behavior can be used in individual counseling sessions or in groups, both of which are important in helping patients modify their patterns of eating. Physical activity is particularly important in helping patients maintain a weight loss once achieved and is less valuable for weight loss itself. Food intake is controlled through many different mechanisms, but only a few drugs have been developed that tap these mechanisms. Orlistat, which blocks intestinal lipase, is one; sibutramine, a serotonin-norepinephrine reuptake inhibitor, is a second. Surgical approaches provide the most dramatic weight loss and have been demonstrated to reduce long-term mortality and reduce the incidence of diabetes.
Conclusions: Weight loss can be achieved by many methods, but the surgical procedures appear to be the most durable.
Although diet, lifestyle modification, and physical activity can treat obesity, surgery provides the most dramatic and long-lasting results.
Obesity is often described as an epidemic (1,2) with a prevalence exceeding 30% in US adults (3). The fundamental problem is the result of a small, but prolonged, positive energy balance, where energy from food exceeds energy needed for everyday living (4).
Realities in Treating an Obese Patient
One of the key messages for obese patients is that when caloric intake is reduced below that needed for daily energy expenditure, there is a predictable rate of weight loss (5,6,7). Men generally lose weight faster than women of similar height and weight on any given diet, because men have more lean body mass and therefore higher energy expenditure. Similarly, older patients have a lower metabolic expenditure and as a rule lose weight more slowly than do younger subjects with similar adherence to weight-loss programs. Thus, adherence to any program is an essential component of success.
Model for Addressing the Problem
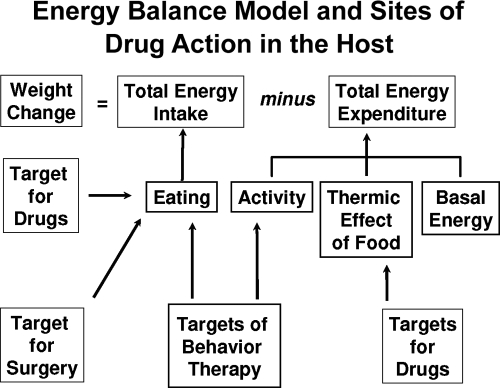
If obesity is the result of a prolonged small difference between energy intake and energy expenditure, then losing body fat requires reversing this imbalance. The relationship between energy intake and expenditure is shown at the top of Fig. 1. Below this are various strategies that can be used to treat this imbalance.
Figure 1.
A model for energy balance and treatment of obesity. A model relating energy balance to treatments for obesity. The top shows that changes in energy stores are the result of changes in intake and/or energy expenditure. The other boxes show ways in which these two components of the system can be altered therapeutically.
Diet and the Treatment of Obesity
Types of diet
Reducing energy intake from food is one strategy for weight loss (4). This can be done by reducing calories or by changing the intake of carbohydrate, fat, or protein that will in turn reduce total intake (8). We will discuss each of these in turn.
Very-low-calorie diets (VLCD)
VLCD or very-low-energy diets have energy levels between 200 and 800 kcal/d. The theory behind them is that the lower the energy intake, the more it would accelerate weight and fat loss. Contrary to this theory are data showing that weight loss from a 400-kcal/d VLCD compared with an 800-kcal/d diet was not different (9). Most weight-loss diets can produce a decline in energy expenditure with a drop in triiodothyronine and leptin. Treatment with leptin partially corrects these changes (10).
Balanced-deficit diets
Diets that reduce carbohydrate, protein, and fat, the so-called balanced-deficit diets or prudent diets, have been widely used in treating obesity. In a metaanalysis of low-calorie diets, Avenell and colleagues (11) found that in 12 studies, the difference after 12 months between control and treated groups was −5.31 kg [95% confidence interval (CI) = −5.86 to −4.77 kg). In another systematic review of 16 studies that used diet but without pharmacological intervention and that had more than 100 subjects in each group and a duration of more than 1 yr, weight loss after 2–3 yr was usually less than 5 kg below baseline (−3.5 ± 2.4 kg; range, 0.9–10.0 kg), and after 4–7 yr where there were data, it was −3.6 ± 2.6 kg (12).
Portion-controlled diets are one way of achieving a balanced caloric deficit. This can be done most simply by using individually packaged foods. Frozen low-calorie meals containing 250–350 kcal/package can be a convenient way to do this, except for the high salt content of many of these foods. In one 4-yr study, this approach resulted in early initial weight loss, which then was maintained (13).
Low-fat diets
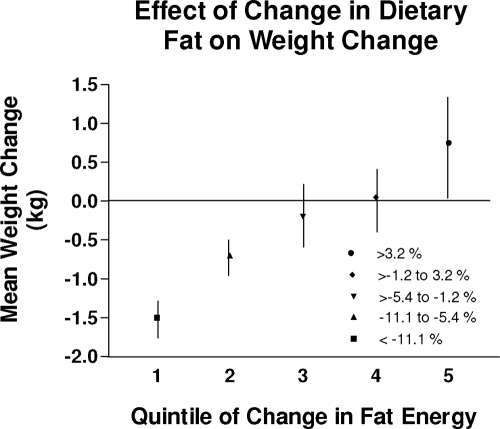
Low-fat diets are a standard strategy to help patients lose weight. A metaanalysis of five randomized controlled trials of low-fat diets showed that these diets produced significant weight loss but not more so than did the control diets (14). Subsequently, a large clinical trial of low-fat vs. control diets (15) randomly assigned 48,835 women to either low-fat or control diets. Weight loss was 2.2 kg below baseline at yr 1 and 0.6 kg after an average of 7.5 yr of follow-up. At both times, the low-fat diet group was significantly lighter than the normal-fat diet group. There was a clear relationship between the decrease in percent fat and weight loss (P < 0.001 for trend). This relationship is shown in Fig. 2. In another metaanalysis of weight-loss studies, Astrup and colleagues (16) found that over the first 6 months, low-fat diets produced weight loss and that heavier individuals lost more weight.
Figure 2.
Reducing dietary fat intake is associated with a reduction in weight gain. Relation of changes in fat intake to changes in body weight is shown. Subgroups of the Women’s Health Initiative who had different degrees of reduction in dietary fat intake are shown in relation to the changes in body weight during follow-up. The greater the reduction in fat intake, the less weight was regained.
Low-carbohydrate diets
Two strategies have been used to lower carbohydrate intake. One is to use foods with a lower glycemic index or lower glycemic load, and the other is to reduce the total amount of carbohydrate. The glycemic index is based on the rise in blood glucose in response to the test food compared with the rise after a 50-g portion of white bread (17); glycemic load is the product of glycemic index and amount of carbohydrate in the food.
Two randomized clinical trials of low-glycemic-load (higher-fiber) diets vs. a conventional diet failed to show any differences in weight loss between the two diets, but those on the lower-glycemic-load diet had a higher resting energy expenditure, lower triglycerides, and less insulin resistance (18,19). Thus, eating foods with more fiber can have benefits over and above any effect on body weight and make good nutritional sense.
The second low-carbohydrate strategy is the very-low-carbohydrate diet. Several recent studies have shown a small but significantly greater weight loss over the first 6 months, but not 12 months, in people eating a very-low-carbohydrate diet based on the Atkins plan compared with the control diet (20,21,22). Diets with similarly low carbohydrate levels but without a named diet plan did not show this effect, raising concern about whether it is the carbohydrate level itself or a placebo effect (7).
High-protein diets
High-protein diets have also been touted as weight-loss diets. One study compared 15 and 25% protein diets as part of a low fat intake. Weight loss over 6 months was greater with the higher-protein diet (23,24), and this difference was maintained at 12 and 24 months. Higher-protein diets may also enhance weight maintenance (24,25,26). After weight loss with a VLCD for 4 wk, 148 male and female subjects were stratified by age, BMI, body weight, restrained eating, and resting energy expenditure and randomized to a control condition or a supplement of 48.2 g/d additional protein. At the end of 3 months, the group receiving the protein supplement to bring protein to 18% had a 50% reduction in body weight regain.
Diets popularized through trade books
A recent analysis of several popular diets by Consumers Union (27) has been adapted in Table 1. Included in this analysis are a low-carbohydrate diet (Atkins) (28), a low-fat diet (Ornish) (29), a low-glycemic-index diet (South Beach) (30), computer diets (e-Diets), an energy-density diet (Volumetrics) (31), portion-controlled (13), and commercial groups.
Table 1.
Nutritional content of several popular diets
| Diet | Protein (%) | Fat (%) | Saturated fat (%) | Carbohydrate (%) | Fiber (g/1000 kcal) | Fruits and vegetables (daily servings) |
|---|---|---|---|---|---|---|
| Atkins | 29 | 60 | 20 | 11 | 12 | 6 |
| e-Diets | 24 | 23 | 5 | 53 | 19 | 12 |
| Jenny Craig | 20 | 18 | 7 | 62 | 16 | 6 |
| Ornish | 16 | 6 | 1 | 77 | 31 | 17 |
| Slim-Fast | 21 | 22 | 6 | 57 | 21 | 12 |
| South Beach | 22 | 39 | 9 | 38 | 19 | 3 |
| Volumetrics | 22 | 23 | 7 | 55 | 20 | 14 |
| Weight Waters | 20 | 24 | 7 | 56 | 20 | 11 |
Adapted from Ref. 27.
Comparison of diets with different macronutrient composition
Two randomized clinical trials have compared several trade-book diets head to head. In the first, 169 obese individuals were randomized to one of four popular diets, including the Atkins Diet, The Ornish Diet, the Weight Watchers Diet, and the Zone Diet (32). At the end of 12 months, each diet produced weight loss of about 5 kg, but there was no difference between diets. Adherence to the diet was the single most important criterion of success in this trial, and the Atkins and Ornish diets were apparently more difficult to adhere to. In a second 1-yr trial, the Atkins, Zone, Ornish, and LEARN diets were compared (33). This trial found that the Atkins diet produced more weight loss at 6 and 12 months compared with the other three diets, which had similar results. In this study, too, a post hoc analysis showed that adherence was the best predictor for weight loss and that the level of adherence was not very good to any diet (34). Two reasons are proposed for the differences. First, the study by Gardner and colleagues (33) had a more homogeneous population, including only premenopausal women. Second, the Gardner study was larger and thus had more statistical power to detect differences.
Lifestyle Changes and the Treatment of Obesity
Elements of a lifestyle program
Current behavioral packages usually include keeping food diaries and activity records, controlling the stimuli that activate eating, slowing down the rate of eating, setting goals, behavioral contracting and reinforcement, nutrition education, meal planning, modification of physical activity, social support, cognitive restructuring, and problem solving (35).
Behavioral programs can be successful when administered individually, as was done with the Diabetes Prevention Program, where weight loss averaged 7% below baseline by 6 months with only a slow gradual regain over the ensuing 3 yr (36,37). It can also be done using groups, which provide a more economical setting, because a single therapist can treat up to 15 or more participants (38). A recent review of long-term effectiveness of lifestyle and behavioral weight-loss interventions by Norris and colleagues (39) found 22 studies that examined weight loss in this group of patients with some studies lasting up to 5 yr. Compared with weight loss among more than 500 diabetics receiving usual care, behavioral strategies produced an added −1.7 kg of weight loss (95% CI = 0.3–3.2 kg). If physical activity and behavioral strategies were combined with a VLCD (n = 117 diabetics), weight loss was −3.0 kg more than in the VLCD comparison groups. With more intense physical activity added on top of behavioral and dietary advice, added weight loss was −3.9 kg. The authors conclude that weight-loss strategies involving behavior change, diet, and physical activity were associated with small between-group improvements in weight loss for diabetics. In a metaanalysis, Avenell and colleagues (11) found that in four trials, adding behavioral therapy to diet increased the weight loss after 12 months by −7.67 kg (95% CI = −11.97 to −3.36 kg).
Increasing physical activity was a key element in success for members of the National Weight Control Registry (35). In this group of more than 4000 individuals who had lost at least 13.6 kg (30 pounds) and kept it off for at least 1 yr, increasing physical activity was an important element in success. These individuals had lost an average of 33 kg and maintained it for an average of 5.7 yr. Women in the Registry reported expending 2545 kcal/wk and men 3293 kcal/wk. This would be equivalent to about 1 h/d moderate-intensity activity, such as brisk walking.
The efficacy of dietary counseling vs. control therapy has been examined in a metaanalysis (40). A random-effects model of 46 studies of dietary counseling showed a maximum net treatment effect of −1.9 BMI units (95% CI = −2.3 to −1.5 BMI units) (approximately 6% weight loss) over 12 months. There was a loss of about −0.1 BMI unit per month for the 12 months of active treatment and a regain of about 0.02–0.03 BMI units per month during subsequent phases. In a metaanalysis of four behavioral programs that included family members, Avenell and colleagues (11) found that after 12 months, a family-based intervention had a weight loss of −2.96 kg (95% CI = −5.31 to −0.60 kg) more than the control behavioral programs.
Exercise and the Treatment of Obesity
Elements: strength vs. endurance
Two kinds of exercise, endurance and strength training, have been used to treat obesity. Endurance exercises, such as walking briskly, jogging, running, or riding a bicycle, are useful for increasing cardiovascular fitness, whereas weight lifting strengthens individual muscle groups. Step counters that can be attached to the belt are a useful way to monitor walking. Current recommendations are to walk 30–90 min/d for 5 d/wk (41,42). In a trial of three dose levels of exercise, including the current level of 8 kcal/kg, Church et al. (41) showed a dose-dependent increase in cardiorespiratory performance across a range of exercise levels averaging 72, 136, and 192 min/wk but with no differences in body weight.
One of the best trials of exercise and diet is shown in a year-long study by Wood and colleagues (43), who reported a decrease of −7.2 kg in body weight in the group receiving the dietary prescription and a decrease of −4.0 kg in body weight in the group participating in the exercise intervention. There was a decrease in low-density lipoprotein-cholesterol and triglycerides and an increase in high-density lipoprotein (HDL)-cholesterol. These effects occurred in both men and women. In a metaanalysis of changes in lipids with diet and exercise, Dattilo and colleagues (44) found that for each decrease of 1 kg in body weight there was a decrease of −0.75 mg/dl in total cholesterol, a decrease of 0.6 mg/dl in triglycerides, and a change in HDL-cholesterol that depended on whether body weight was stable or body weight was still declining. If weight was stable, HDL-cholesterol increased +0.35 mg/dl, but if weight loss was still occurring, HDL-cholesterol was −0.25 mg/dl lower.
Exercise may also be beneficial in maintaining weight loss. Activity that expends about 2500 kcal/wk has shown benefit in helping patients maintain weight losses (41,45,46,47).
Medications and the Treatment of Obesity
Mechanisms underlying drug therapy of obesity
Currently available medications to treat obesity work in the brain and on the gut (4,48). A number of neurotransmitter systems, including monoamines, amino acids, and neuropeptides, are involved in modulating food intake (49). Serotonin 5-HT2C receptors modulate fat and caloric intake. Mice that cannot express the 5-HT2C receptor are obese and have increased food intake. Sibutramine blocks serotonin and norepinephrine reuptake. Lorcaserin, a drug in clinical trial, works directly on serotonin-2C receptors in the brain. These receptors may work through modulation of downstream melanocortin-4 receptors (50).
α1-Receptors also modulate feeding. Some α1-receptor drugs that are used to treat hypertension produce weight gain, indicating that this receptor is clinically important. In contrast, stimulation of α2-receptors increases food intake, and a polymorphism in the α2a adrenoceptor is associated with reduced metabolic rate in humans. Activation of β2-receptors in the brain reduces food intake, and β-blocker drugs can increase body weight.
The two endogenous endocannabinoids, anandamide and 2-arachidonoylglycerol, increase food intake by acting on the cannabinoid-1 (CB-1) receptor (51). This is a preganglionic receptor, where antagonists (rimonabant and taranabant) have been shown to reduce food intake and lead to weight loss.
Other drugs act in the periphery. Blockade of intestinal lipase with orlistat will produce weight loss. Glucagon-like peptide-1 released from intestinal L-cells acts on the pancreas and brain to reduce food intake. Amylin is secreted from the pancreas and can reduce food intake.
Drugs approved by the U.S. Food and Drug Administration (FDA) for the treatment of obesity
Several drugs are currently approved in the United States to treat obesity (Table 2).
Table 2.
Drugs approved by the FDA that produce weight loss
| Generic name | Trade names | Usual dose | Comments |
|---|---|---|---|
| Drugs approved by the FDA for the long-term treatment of obesity (12 months) | |||
| Orlistat | Xenical | 120 mg 3 times/d | May have gastrointestinal side effects |
| Sibutramine | Meridia (U.S.) Reductil (rest of world) | 5–15 mg once daily | Norepinephrine-serotonin reuptake inhibitor; may raise blood pressure |
| Drugs approved by the FDA for short-term treatment of obesity (12 wk) | Sympathomimetic drugs; approved for only a | ||
| Diethylpropion | short time | ||
| Tablets | Tenuate | 25 mg 3 times/d | |
| Extended release | Tenuate | 75 mg in morning | |
| Phentermine HCl | |||
| Capsules | Phentridol, Teramine, Adipex-P | 15–37.5 mg in the morning | |
| Tablets | Tetramine, Adipex-P | 15–37.5 mg in the morning | |
| Extended release | Ionamin | 15 or 30 mg/d in the morning | |
| Benzphetamine | Didrex | 25–150 mg/d in single or divided doses | |
| Phendimetrazine | |||
| Capsules, extended release | Adipost, Bontril, Melfial | 105 mg once daily | |
| Tablets | Prelu-2, X-trozine, Bontril, Obezine | 35 mg 2–3 times/d |
Adapted from Ref. 48.
Sibutramine
Sibutramine is a serotonin-norepinephrine reuptake inhibitor. In a 6-month trial where 1047 patients were randomized to placebo or doses of sibutramine ranging from 1–30 mg/d, there was a clear dose-response effect (52). Longer trials with sibutramine have been conducted in uncomplicated obese patients, in patients with hypertension, in diabetics, and in children (4,48). In a metaanalysis of long-term studies of sibutramine, the placebo group had a weighted mean weight loss of −2.18 ± 5.23 kg. The drug-treated group had a weighted mean weight loss of −6.35 ± 6.47 kg for a net, or placebo-subtracted weight loss, of −4.16 kg (95% CI = −4.73 to −3.59) (53). Sibutramine can be used as intermittent therapy (54). During this 12-month trial, the continuous-therapy and intermittent-therapy groups lost the same amount of weight. Sibutramine has been used in children (52). In a large 12-month-long multicenter trial with 498 adolescents ages 12–16 yr, the mean absolute change in BMI was −2.9 kg/m2 (−8.2%) in the sibutramine group compared with −0.3 kg/m2 (−0.8%) in the placebo group (P < 0.001) (55). Sibutramine has also been studied as part of a behavioral weight-loss program. With sibutramine alone and minimal behavioral intervention, the weight loss over 12 months was approximately −5.0 ± 7.4 kg over 12 months. Behavior modification alone produced a weight loss of −6.7 ± 7.9 kg. Adding a brief behavioral therapy session to a group that also received sibutramine produced a slightly larger weight loss of −7.5 ± 8.0 kg. When the intensive lifestyle intervention was combined with sibutramine, the weight loss increased to −12.1 ± 9.8 kg (56).
Safety.
Sibutramine increases blood pressure levels in normotensive patients or blunts the decrease that might have occurred with weight loss. Systolic and diastolic blood pressure levels increased an average of +0.8 mm Hg and +0.6 mm Hg, and pulse increased approximately 4–5 beats/min (48,57). Caution should be used when combining sibutramine with other drugs that may increase blood pressure levels. Sibutramine is contraindicated in patients with a history of coronary artery disease, congestive heart failure, cardiac arrhythmias, or stroke. Sibutramine should not be used with selective serotonin reuptake inhibitors or monoamine oxidase inhibitors, and there should be a 2-wk interval between terminating monoamine oxidase inhibitors and beginning sibutramine. Because sibutramine is metabolized by the cytochrome P-450 enzyme system (isozyme CYP3A4), it may interfere with the metabolism of erythromycin and ketoconazole, and it has a small effect (7% increase in area under the curve) on the metabolism of simvastatin, but not other statins.
Sympathomimetic drugs
The sympathomimetic drugs, benzphetamine, diethylpropion, phendimetrazine, and phentermine, are grouped together because they act like norepinephrine and were tested before 1975. One of the longest of the clinical trials of drugs in this group lasted 36 wk and compared placebo treatment with continuous phentermine or intermittent phentermine (48). Both continuous and intermittent phentermine therapy produced more weight loss than did placebo.
Safety of sympathomimetic drugs.
Sympathomimetic drugs produce insomnia, dry mouth, asthenia, and constipation. They are scheduled by the Drug Enforcement Agency, suggesting the U.S. government’s view that they may be abused. Sympathomimetic drugs can also increase blood pressure.
Orlistat
Orlistat is a potent and selective inhibitor of pancreatic lipase that reduces intestinal digestion of fat. A number of long-term clinical trials with orlistat have been published using uncomplicated obese patients and obese patients with diabetes. A 4-yr double-blind, randomized, placebo-controlled trial with orlistat in 3304 overweight patients, 21% of whom had impaired glucose tolerance (58), achieved a weight loss during the first year of more than −11% below baseline in the orlistat-treated group compared with 6% below baseline in the placebo-treated group. Over the remaining 3 yr of the trial, there was a small regain in weight, such that by the end of 4 yr, the orlistat-treated patients were −6.9% below baseline, compared with −4.1% for those receiving placebo. There was a reduction of 37% in the conversion of patients from impaired glucose tolerance to diabetes. Orlistat has also been studied in adolescents. In 539 adolescents, orlistat 120 mg three times per day decreased BMI by −0.55 kg/m2 in the drug-treated group compared with an increase of +0.31 kg/m2 in the placebo group (59). In a metaanalysis of trials with orlistat, the weighted mean weight loss in the placebo group was −2.40 ± 6.99 kg, and the weight loss in those treated with orlistat was −5.70 ± 7.28 kg for a net effect of −2.87 (95% CI = −3.21 to −2.53) (53).
Safety of orlistat.
Orlistat is not absorbed to any significant degree, and its side effects are thus related to the blockade of triglyceride digestion in the intestine (48). Fecal fat loss and related GI symptoms are common initially, but they subside as patients learn to use the drug. Orlistat can cause small but significant decreases in fat-soluble vitamins. Levels usually remain within the normal range, but a few patients may need vitamin supplementation. Because it is impossible to tell which patients need vitamins, it is wise to provide a multivitamin routinely with instructions to take it before bedtime. Orlistat does not seem to affect the absorption of other drugs, except acyclovir.
Combining orlistat and sibutramine
When orlistat was combined with sibutramine in a 4-month trial initiated at the end of a 12-month treatment period with sibutramine, there was no further weight loss (60). Thus, we have no data that combining orlistat and sibutramine is beneficial.
Drugs approved by European Regulatory Authorities but not by the FDA
Rimonabant
Rimonabant is approved and marketed in Europe, but at an Advisory Committee meeting to the FDA in June 2007, the vote was not to approve rimonabant in the United States. Rimonabant is a specific antagonist of the CB-1 receptor. Genetically engineered mice that lack the CB-1 receptor are lean and resistant to diet-induced obesity.
The results of four phase III trials of rimonabant for the treatment of obesity have been published (61,62,63,64): two in uncomplicated obesity, and one each in patients with dyslipidemia and diabetes. A fifth study, called STRADIVARIUS, examined the effect of treatment for rimonabant on coronary artery plaque thickness in patients needing coronary angiography (65). At the end of 18 months, there was no significant difference in the primary endpoint (percent atheroma volume) between groups (placebo vs. 20 mg/d rimonabant), but the secondary endpoint (total atheroma volume) showed significant improvement in the rimonabant group, raising the possibility that this drug may have benefits on the progression of coronary vascular disease.
Safety.
There were significantly more psychiatric side effects with the higher dose of rimonabant in the first year of treatment, and three suicides were reported to the FDA during clinical trials. Because patients with depression were excluded from the initial phase III studies, there is no information on how this drug works in depressed patients or those taking antidepressants (66).
Drugs that have been used to treat obesity but are not approved by the FDA for this purpose
Several drugs approved for purposes other than weight loss have been used for the treatment of obesity including metformin, fluoxetine, bupropion, topiramate, and zonisamide (4). Physicians who decide to try these agents are using them off-label and would be well advised to do so only with signed informed consent from the patient.
Combinations of drugs that produce weight loss
The first important clinical trial combining drugs that acted by separate mechanisms used phentermine and fenfluramine (67). This trial showed a highly significant weight loss of nearly 15% below baseline with fewer side effects by using combination therapy. This combination became very popular, but due to reports of aortic valvular regurgitation associated with its use (68), fenfluramine was withdrawn from the market worldwide on September 15, 1997. Several other combinations of existing drugs are now under development, and the results are awaited with interest (4).
Drugs that increase energy expenditure
There are no effective drugs in this class.
Conclusions
A number of treatments have been used in the obese patient, but all produce weight loss of about 10% below baseline. There are presently only two drugs approved for long-term treatment of overweight patients, and their effectiveness is limited to palliation of the chronic disease of obesity.
Footnotes
Disclosure Statement: G.B. has received research grant support from the National Institutes of Health; G.B. consults for Sanofi-Aventis and Merck and Co.; G.B. has served on advisory boards and councils for Sanofi-Aventis and Merck and Co.; G.B. has received consulting fees, honoraria, and lecture fees from Sanofi-Aventis and Merck and Co.
Abbreviations: CB-1, Cannabinoid; CI, confidence interval; HDL, high-density lipoprotein; VLCD, very-low-calorie diet.
References
- World Health Organization 2000 Obesity: preventing and managing the global epidemic. Report of a WHO consultation. Tech Rep Ser 894. Geneva: World Health Organization; i–xii, 1–253 [PubMed] [Google Scholar]
- NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults 1998 Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Obes Res 6:51S–63S [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM 2006 Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 295:1549–1555 [DOI] [PubMed] [Google Scholar]
- Bray GA 2007 The metabolic syndrome and obesity. Totowa, NJ: Humana Press [Google Scholar]
- Keys A, Brozek J, Henschel A, Mickelsen O, Taylor HL 1950 The biology of human starvation. Vols. 1 and 2. Minneapolis, MN: University of Minnesota Press [Google Scholar]
- Kinsell LW, Gunning B, Michaels GD, Richardson J, Cox SE, Lemon C 1964 Calories do count. Metabolism 13:195–204 [DOI] [PubMed] [Google Scholar]
- Bray GA 2008 Good calories, bad calories by Gary Taubes; New York: AA Knopf. Obes Rev 9:251–263 [Google Scholar]
- Freedman MR, King J, Kennedy E 2001 Popular diets: a scientific review. Obes Res 9(Suppl 1):1S–40S [DOI] [PubMed] [Google Scholar]
- Foster GD, Wadden TA, Peterson FJ, Letizia KA, Bartlett SJ, Connill MJ 1992 A controlled comparison of three very-low calorie diets: effects on body weight, body composition and symptoms. Am J Clin Nutr 55:811–817 [DOI] [PubMed] [Google Scholar]
- Rosenbaum M, Murphy EM, Heymsfield SB, Matthews DE, Leibel RL 2002 Low dose leptin administration reverses effects of sustained weight-reduction on energy expenditure and circulating concentrations of thyroid hormones. J Clin Endocrinol Metab 87:2391–2394 [DOI] [PubMed] [Google Scholar]
- Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, Smith WC, Jung RT, Campbell MK, Grant AM 2004 Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement. Health Technol Assess 8:iii–iv, 1–182 [DOI] [PubMed] [Google Scholar]
- Douketis JD, Macie C, Thabane L, Williamson DF 2005 Systematic review of long-term weight loss studies in obese adults: clinical significance and applicability to clinical practice. Int J Obes (Lond) 29:1153–1167 [DOI] [PubMed] [Google Scholar]
- Flechtner-Mors M, Ditschuneit HH, Johnson TD, Suchard MA, Adler G 2000 Metabolic and weight loss effects of long-term dietary intervention in obese patients: four-year results. Obes Res 8:399–402 [DOI] [PubMed] [Google Scholar]
- Pirozzo S, Summerbell C, Cameron C, Glasziou P 2003 Should we recommend low-fat diets for obesity? Obes Rev [Erratum (2003) 4:185] 4:83–90 [DOI] [PubMed] [Google Scholar]
- Howard BV, Manson JE, Stefanick ML, Beresford SA, Frank G, Jones B, Rodabough RJ, Snetselaar L, Thomson C, Tinker L, Vitolins M, Prentice R 2006 Low-fat dietary pattern and weight change over 7 years: the Women’s Health Initiative Dietary Modification Trial. JAMA 295:39–49 [DOI] [PubMed] [Google Scholar]
- Astrup A, Grunwald GK, Melanson EL, Saris WH, Hill JO 2000 The role of low-fat diets in body weight control: a meta-analysis of ad libitum dietary intervention studies. Int J Obes Relat Metab Disord 24:1545–1552 [DOI] [PubMed] [Google Scholar]
- Ludwig DS 2002 The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA 287:2414–2423 [DOI] [PubMed] [Google Scholar]
- Pereira MA, Swain J, Goldfine AB, Rifai N, Ludwig DS 2004 Effects of a low-glycemic load diet on resting energy expenditure and heart disease risk factors during weight loss. JAMA 292:2482–2490 [DOI] [PubMed] [Google Scholar]
- Ebbeling CB, Leidig MM, Feldman HA, Lovesky MM, Ludwig DS 2007 Effects of a low-glycemic load vs low-fat diet in obese young adults: a randomized trial. JAMA [Erratum (2007) 298:627] 297:2092–2102 [DOI] [PubMed] [Google Scholar]
- Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, Mohammed BS, Szapary PO, Rader DJ, Edman JS, Klein S 2003 A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med 348:2082–2090 [DOI] [PubMed] [Google Scholar]
- Stern L, Iqbal N, Seshadri P, Chicano KL, Daily DA, McGrory J, Williams M, Gracely EJ, Samaha FF 2004 The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Ann Intern Med 140:778–785 [DOI] [PubMed] [Google Scholar]
- Brehm BJ, Seeley RJ, Daniels SR, D'Alessio DA 2003 A randomized trial comparing a very low carbohydrate diet and a calorie-restricted low fat diet on body weight and cardiovascular risk factors in healthy women. J Clin Endocrinol Metab 88:1617–1623 [DOI] [PubMed] [Google Scholar]
- Skov AR, Toubro S, Rønn B, Holm L, Astrup A 1999 Randomized trial on protein vs carbohydrate in ad libitum fat reduced diet for the treatment of obesity. Int J Obes Relat Metab Disord 23:528–536 [DOI] [PubMed] [Google Scholar]
- Due A, Toubro S, Skov AR, Astrup A 2004 Effect of normal-fat diets, either medium or high in protein, on body weight in overweight subjects: a randomised 1-year trial. Int J Obes Relat Metab Disord 28:1283–1290 [DOI] [PubMed] [Google Scholar]
- Westerterp-Plantenga MS, Lejeune MP, Nijs I, van Ooijen M, Kovacs EM 2004 High protein intake sustains weight maintenance after body weight loss in humans. Int J Obes Relat Metab Disord 28:57–64 [DOI] [PubMed] [Google Scholar]
- Paddon-Jones D, Westman E, Mattes RD, Wolfe RR, Astrup A, Westerterp-Plantenga M 2008 Protein, weight management, and satiety. Am J Clin Nutr 87:1558S–1561S [DOI] [PubMed] [Google Scholar]
- 2005 Rating the diets from Atkins to Dr. Sears Zone. Consum Rep 70:18–22 [PubMed] [Google Scholar]
- Atkins RC 2002 Dr. Atkins’s new diet revolution. New York: Avon [Google Scholar]
- Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Ports TA, Kirkeeide RL, Hogeboom C, Brand RJ 1998 Intensive lifestyle changes for reversal of coronary heart disease. JAMA [Erratum (1999) 281:1380] 280:2001–2007 [DOI] [PubMed] [Google Scholar]
- Agatson A 2003 The South Beach Diet. London: Headline Book Publishing [Google Scholar]
- Rolls BJ, Barnett RA 2000 Volumetrics: feel full on fewer calories. New York: Harper Collins [Google Scholar]
- Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ 2005 Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA 293:43–53 [DOI] [PubMed] [Google Scholar]
- Gardner CD, Kiazand A, Alhassan S, Kim S, Stafford RS, Balise RR, Kraemer HC, King AC 2007 Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial. JAMA [Erratum (2007) 298:178] 297:969–977 [DOI] [PubMed] [Google Scholar]
- Alhassan S, Kim S, Bersamin A, King AC, Gardner CD 2008 Dietary adherence and weight loss success among overweight women: results from the A TO Z weight loss study. Int J Obes (Lond) 32:985–991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Phelan S 2005 Long-term weight loss maintenance. Am J Clin Nutr 82(Suppl 1):222S–225S [DOI] [PubMed] [Google Scholar]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM; Diabetes Prevention Program Research Group 2002 Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Hamman RF, Bray GA, Delahanty L, Edelstein SL, Hill JO, Horton ES, Hoskin MA, Kriska A, Lachin J, Mayer-Davis EJ, Pi-Sunyer X, Regensteiner JG, Venditti B, Wylie-Rosett J; Diabetes Prevention Program Research Group 2004 Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obes Res 12:1426–1434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Look AHEAD Research Group, Pi-Sunyer X, Blackburn G, Brancati FL, Bray GA, Bright R, Clark JM, Curtis JM, Espeland MA, Foreyt JP, Graves K, Haffner SM, Harrison B, Hill JO, Horton ES, Jakicic J, Jeffery RW, Johnson KC, Kahn S, Kelley DE, Kitabchi AE, Knowler WC, Lewis CE, Maschak-Carey BJ, Montgomery B, Nathan DM, Patricio J, Peters A, Redmon JB, Reeves RS, Ryan DH, Safford M, Van Dorsten B, Wadden TA, Wagenknecht L, Wesche-Thorbaben J, Wing RR, Yanovski SZ 2007 Reduction in weight and cardiovascular disease (CVD) risk factors in individuals with type 2 diabetes: one year results of Look AHEAD Trial. Diabetes Care 30:1374–1383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris SL, Zhang X, Avenell A, Gregg E, Bowman B, Serdula M, Brown TJ, Schmid CH, Lau J 2004 Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: a meta-analysis. Am J Med 117:762–774 [DOI] [PubMed] [Google Scholar]
- Dansinger ML, Tatsioni A, Wong JB, Chung M, Balk EM 2007 Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med 14741–14750 [DOI] [PubMed] [Google Scholar]
- Church TS Earnest CP, Skinner JS, Blair SN 2007 Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: a randomized controlled trial. JAMA 297:2081–2091 [DOI] [PubMed] [Google Scholar]
- Saris WH, Blair SN, van Baak MA, Eaton SB, Davies PS, Di Pietro L, Fogelholm M, Rissanen A, Schoeller D, Swinburn B, Tremblay A, Westerterp KR, Wyatt H 2003 How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev 4:101–114 [DOI] [PubMed] [Google Scholar]
- Wood PD, Stefanick ML, Dreon DM, Frey-Hewitt B, Garay SC, Williams PT, Superko HR, Fortmann SP, Albers JJ, Vranizan KM, Ellsworth NM, Terry RB, Haskell WL 1988 Changes in plasma lipids and lipoproteins in overweight men during weight loss through dieting as compared with exercise. N Engl J Med 319:1173–1179 [DOI] [PubMed] [Google Scholar]
- Dattilo AM, Kris-Etherton PM 1992 Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr 56:320–328 [DOI] [PubMed] [Google Scholar]
- Jakicic JM, Winters C, Lang W, Wing RR 1999 Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women: a randomized trial. JAMA 282:1554–1560 [DOI] [PubMed] [Google Scholar]
- Schoeller DA, Shay K, Kushner RF 1997 How much physical activity is needed to minimize weight gain in previously obese women? Am J Clin Nutr 66:551–556 [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Wing RR, Sherwood NE, Tate DF 2003 Physical activity and weight loss: does prescribing higher physical activity goals improve outcome? Am J Clin Nutr 78:684–689 [DOI] [PubMed] [Google Scholar]
- Bray GA, Greenway FL 2007 Pharmacological treatment of the overweight patient. Pharmacol Rev 59:151–184 [DOI] [PubMed] [Google Scholar]
- Berthoud HR 2002 Multiple neural systems controlling food intake and body weight. Neurosci Biobehav Rev 26:393–428 [DOI] [PubMed] [Google Scholar]
- Lam DD, Pryzdzial MJ, Ridley SH, Yeo GS, Rochford JJ, O'Rahilly S, Heisler LK 2008 Serotonin 5-HT2C receptor agonist promotes hypophagia via downstream activation of melanocortin 4 receptors. Endocrinology 40:1323–1328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagotto U, Marsicano G, Cota D, Lutz B, Pasquali R 2006 The emerging role of the endocannabinoid system in endocrine regulation and energy balance. Endocr Rev 27:73–100 [DOI] [PubMed] [Google Scholar]
- Bray GA, Blackburn GL, Ferguson JM, Greenway FL, Jain AK, Mendel CM, Mendels J, Ryan DH, Schwartz SL, Scheinbaum ML, Seaton TB 1999 Sibutramine produces dose-related weight loss. Obes Res 7:189–198 [DOI] [PubMed] [Google Scholar]
- Rucker D, Padwal R, Li SK, Curioni C, Lau DC 2007 Long term pharmacotherapy for obesity and overweight: updated meta-analysis. BMJ 335:1194–1199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirth A, Krause J 2001 Long-term weight loss with sibutramine: a randomized controlled trial. JAMA 286:1331–1339 [DOI] [PubMed] [Google Scholar]
- Berkowitz RI, Fujioka K, Daniels SR, Hoppin AG, Owen S, Perry AC, Sothern MS, Renz CL, Pirner MA, Walch JK, Jasinsky O, Hewkin AC, Blakesley VA; Sibutramine Adolescent Study Group 2006 Effects of sibutramine treatment in obese adolescents: a randomized trial. Ann Intern Med 145:81–90 [DOI] [PubMed] [Google Scholar]
- Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK, Hesson LA, Osei SY, Kaplan R, Stunkard AJ 2005 Randomized trial of lifestyle modification and pharmacotherapy for obesity. N Engl J Med 353:2111–2120 [DOI] [PubMed] [Google Scholar]
- Kim SH, Lee YM, Jee SH, Nam CM 2003 Effect of sibutramine on weight loss and blood pressure: a meta-analysis of controlled trials. Obes Res 11:1116–1123 [DOI] [PubMed] [Google Scholar]
- Torgerson JS, Hauptman J, Boldrin MN, Sjöström L 2004 XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care [Erratum (2004) 27:856] 27:155–161 [DOI] [PubMed] [Google Scholar]
- Chanoine JP, Hampl S, Jensen C, Boldrin M, Hauptman J 2005 Effect of orlistat on weight and body composition in obese adolescents: a randomized controlled trial. JAMA [Erratum (2005) 294:1491] 293:2873–2883 [DOI] [PubMed] [Google Scholar]
- Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Arnold ME, Steinberg CM 2000 Effects of sibutramine plus orlistat in obese women following 1 year of treatment by sibutramine alone: a placebo-controlled trial. Obes Res 8:431–437 [DOI] [PubMed] [Google Scholar]
- Van Gaal LF, Rissanen AM, Scheen AJ, Ziegler O, Rössner S; RIO-Europe Study Group 2005 Effects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe study. Lancet [Erratum (2005) 366:370] 365:1389–1397 [DOI] [PubMed] [Google Scholar]
- Després JP, Golay A, Sjöström L; Rimonabant in Obesity-Lipids Study Group 2005 Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia. N Engl J Med 353:2121–2134 [DOI] [PubMed] [Google Scholar]
- Pi-Sunyer FX, Aronne LJ, Heshmati HM, Devin J, Rosenstock J; RIO-North America Study Group 2006 Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: a randomized controlled trial. JAMA [Erratum (2006) 295:1252] 295:761–775 [DOI] [PubMed] [Google Scholar]
- Scheen AJ, Finer N, Hollander P, Jensen MD, Van Gaal LF; RIO-Diabetes Study Group 2006 Efficacy and tolerability of rimonabant in overweight or obese patients with type 2 diabetes: a randomised controlled study. Lancet [Erratum (2006) 368:1650] 368:1660–1672 [DOI] [PubMed] [Google Scholar]
- Nissen SE, Nicholls SJ, Wolski K, Rodés-Cabau J, Cannon CP, Deanfield JE, Després JP, Kastelein JJ, Steinhubl SR, Kapadia S, Yasin M, Ruzyllo W, Gaudin C, Job B, Hu B, Bhatt DL, Lincoff AM, Tuzcu EM; STRADIVARIUS Investigators 2008 Effect of rimonabant on progression of atherosclerosis in patients with abdominal obesity and coronary artery disease: the STRADIVARIUS randomized controlled trial. JAMA 299:1547–1560 [DOI] [PubMed] [Google Scholar]
- Christensen R, Kristensen PK, Bartels EM, Bliddal H, Astrup 2007 A Efficacy and safety of the weight-loss drug rimonabant: a meta-analysis of randomised trials. Lancet [Erratum (2008) 371:558] 370:1706–1713 [DOI] [PubMed] [Google Scholar]
- Weintraub M 1992 Long-term weight control: the National Heart, Lung, and Blood Institute funded multimodal intervention study. Clin Pharmacol Ther 51:581–585 [DOI] [PubMed] [Google Scholar]
- Connolly HM, Crary JL, McGoon MD, Hensrud DD, Edwards BS, Edwards WD, Schaff HV 1997 Valvular heart disease associated with fenfluramine-phentermine. N Engl J Med 337:581–588 [DOI] [PubMed] [Google Scholar]