Abstract
The construction of cDNA clones encoding large-size RNA molecules of biological interest, like coronavirus genomes, which are among the largest mature RNA molecules known to biology, has been hampered by the instability of those cDNAs in bacteria. Herein, we show that the application of two strategies, cloning of the cDNAs into a bacterial artificial chromosome and nuclear expression of RNAs that are typically produced within the cytoplasm, is useful for the engineering of large RNA molecules. A cDNA encoding an infectious coronavirus RNA genome has been cloned as a bacterial artificial chromosome. The rescued coronavirus conserved all of the genetic markers introduced throughout the sequence and showed a standard mRNA pattern and the antigenic characteristics expected for the synthetic virus. The cDNA was transcribed within the nucleus, and the RNA translocated to the cytoplasm. Interestingly, the recovered virus had essentially the same sequence as the original one, and no splicing was observed. The cDNA was derived from an attenuated isolate that replicates exclusively in the respiratory tract of swine. During the engineering of the infectious cDNA, the spike gene of the virus was replaced by the spike gene of an enteric isolate. The synthetic virus replicated abundantly in the enteric tract and was fully virulent, demonstrating that the tropism and virulence of the recovered coronavirus can be modified. This demonstration opens up the possibility of employing this infectious cDNA as a vector for vaccine development in human, porcine, canine, and feline species susceptible to group 1 coronaviruses.
Coronaviruses are single-stranded, positive-sense RNA viruses and have the largest genomes known [around 30 kilobases (kb); refs. 1 and 2] among RNA viruses. Reverse genetics of coronaviruses has been done by targeted recombination following the procedure initially developed by Master's group (3–6). However, the construction of a full-length genomic cDNA clone will improve considerably the genetic manipulation of coronaviruses. To date, this objective has not been achieved, the viral cDNA instability being one of the main problems.
The instability problems observed with bacterial vectors containing viral cDNAs were first overcome by Rice et al. (7), who successfully generated infectious yellow fever virus RNA from a pair of cDNA clones ligated in vitro before RNA transcription. Infectious cDNA clones have now been constructed for members of many positive-stranded RNA virus families (7–12), including the Arteriviridae family closely related to coronaviruses (13). Negative-stranded RNA virus genomes have been generated for Mononegavirales by the simultaneous expression of the ribonucleoprotein containing the N protein, the polymerase cofactor phosphoprotein, and the viral RNA polymerase (14). Rescue of engineered RNAs in negative-strand RNA virus with eight genome segments was also possible for influenza virus (15).
Unfortunately, the enormous length of the coronavirus genome and the instability of plasmids carrying coronavirus replicase sequences have thus far hampered the construction of a full-length cDNA clone (6). To overcome these problems we have combined three strategies. (i) We started the construction of the full-length cDNA from a defective minigenome (DI) that was stably and efficiently replicated by the helper virus (16, 17). By using this DI, the full-length genome was completed, and the performance of the enlarged genome was checked after each step. This approach allowed for the identification of a cDNA fragment that was toxic to the bacterial host. This finding was used to advantage by reintroducing the toxic fragment into the viral cDNA in the last cloning step. (ii) We cloned the cDNA as a bacterial artificial chromosome (BAC), a low-copy number plasmid (one or two copies per cell). BACs have been useful to clone large DNAs stably from a variety of complex genomic sources into bacteria (18), including herpesvirus DNA (19). (iii) We used a two-step amplification system that couples transcription in the nucleus from the cytomegalovirus (CMV) immediate early promoter with a second amplification in the cytoplasm driven by the viral polymerase.
The work was done with the transmissible gastroenteritis coronavirus (TGEV) PUR46-MAD virus (abbreviated PUR-MAD), an attenuated strain of TGEV that infects newborn piglets (20, 21). To assemble a fully functional infectious cDNA clone, leading to a virulent virus able to infect both the enteric and respiratory tracts, the spike (S) gene of the PUR-MAD strain was replaced by the S gene of the TGEV virulent strain PUR46-C11 (abbreviated PUR-C11; ref. 22). These viruses belong to group 1 coronaviruses, which include human, porcine, canine, and feline isolates with high sequence identity.
In the present study, we report the recovery of infectious TGEV from cloned cDNA and show that this procedure can be used to generate a genetically modified TGEV.
Materials and Methods
Cells and Viruses.
Epithelial swine testis (ST) cells (23) were kindly provided by L. Saif (Ohio State University, Wooster, OH). The TGEV strains PUR-MAD and PUR-C11 (22) were grown and titered as described (24, 25).
Plasmids and Bacteria Strains.
Plasmid pBeloBAC11 (26) was kindly provided by H. Shizuya and M. Simon (California Institute of Technology, Pasadena, CA). Escherichia coli DH10B strain [F−mcr A Δ(mrr-hsdRMS-mcrBC) Ø80dlacZΔM15 ΔlacX74 deoR recA1 endA1 araD139 (ara,leu)7697 galU galK λ− rps L nupG] was obtained from GIBCO/BRL. DH10B cells were transformed by electroporation at 25 μF, 2.5 kV, and 200 Ω with a Gene Pulser unit (Bio-Rad) according to the manufacturer's instructions. After electroporation, cells were incubated at 37°C with gentle shaking for 45 min before being spread on LB plates containing 12.5 μg/ml chloramphenicol.
Plasmid DNA Preparation.
Recombinant clones were grown at 37°C in 5 ml of LB containing 12.5 μg/ml chloramphenicol, and plasmid DNA was isolated with the Qiagen (Chatsworth, CA) plasmid Mini Kit according to the manufacturer's specifications. Supercoiled plasmid DNA was purified further by digestion of linear and open circular DNA with Plasmid Safe ATP-dependent DNase (Epicentre Technologies, Madison, WI). For large-scale DNA preparation, the BAC vector and recombinant BACs were isolated by alkaline lysis with the Qiagen Plasmid Maxi Kit according to the manufacturer's specifications. The plasmid DNA was purified further by cesium chloride density gradient centrifugation.
Construction of the TGEV Full-Length cDNA.
As a backbone for the construction of the complete cDNA of the TGEV genome, the plasmid pDI-C (16, 17), containing a cDNA encoding a TGEV-derived DI was used. DI-C RNA has three deletions (Δ1, Δ2, and Δ3) of about 10, 1, and 8 kb within ORFs 1a, 1b, and between genes S and 7, respectively (Fig. 1a). To complete these deletions, a set of cDNAs encoding fragments of the missing regions was generated by standard RT-PCR techniques. All of the point mutations introduced by RT-PCR were corrected to the consensus TGEV sequence, except for a silent mutation at position 6,752, which was maintained as a rescue marker.
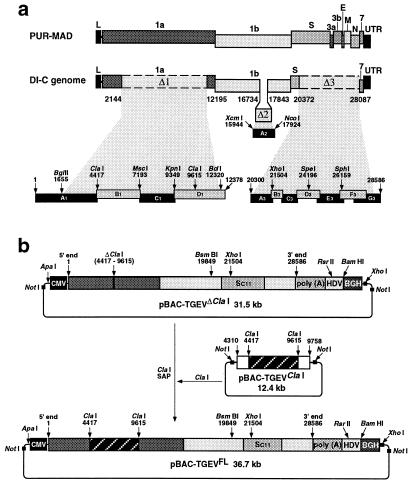
Figure 1.
Construction of a cDNA encoding an infectious TGEV RNA as a BAC. (a) Strategy for the construction of full-length cDNA clones of TGEV. Full-length TGEV cDNA was assembled from DI-C (16, 17), and subgenomic overlapping cDNA fragments were generated by reverse transcriptase–PCR (RT-PCR). The cDNA fragments were joined at shared restriction sites and assembled as described in Materials and Methods. The genetic map of TGEV (Top) and the defective minigenome DI-C (Middle) is shown. The cDNA clones and relevant restriction sites used to restore the three deletions (Δ1, Δ2, and Δ3) of DI-C are indicated. (Top) Letters indicate the viral genes. L, leader sequence; UTR, untranslated region. Numbers in the genetic map of DI-C indicate the position of the three deletions within the genome. (b) Cloning of the TGEV cDNA in pBeloBAC11. Plasmids pBAC-TGEVΔClaI, pBAC-TGEVClaI, and pBAC-TGEVFL were generated as described in Materials and Methods. Relevant restriction sites are indicated. CMV, CMV immediate-early promoter; poly(A) tail of 24 A residues; HDV, hepatitis delta virus ribozyme; BGH, bovine GH termination and polyadenylation sequences; Sc11, S gene of PUR-C11 strain; SAP, shrimp alkaline phosphatase.
The ORF 1a missing sequences (Δ1) were restored by adding cDNA fragments A1, B1, C1, and D1 (Fig. 1a). The resultant plasmid was unstable within the bacteria, and mutated forms were recovered that had incorporated deletions or insertions in fragments B1, C1, and D1. Then, the BglII–ClaI fragment from clone A1 and the ClaI–BclI fragment from clone D1 were inserted into pDI-C to fill in the Δ1 deletion partially. The 1-kb deletion (Δ2) in ORF 1b was restored by subcloning the XcmI–NcoI fragment from clone A2, generating a stable plasmid. The deleted Δ3 sequence was assembled from clones A3 to G3 to yield a plasmid encoding the full-length TGEV genome, lacking a 5.2-kb ClaI (4,417) to ClaI (9,615) fragment. The clones A3 to D3, encoding the S gene, were derived from the PUR-C11 strain, and the clones E3 to G3 were derived from the PUR-MAD strain. Details of this procedure will be published elsewhere. The cDNA encoding the full-length sequence of TGEV, except the 5.2-kb ClaI–ClaI fragment, was transferred to pBeloBAC11 to obtain the pBAC-TGEVΔClaI (Fig. 1b). To generate pBAC-TGEVClaI, a fragment spanning nucleotides 4,310 to 9,758, which includes the missing ClaI–ClaI sequence, was assembled and inserted in pBeloBAC11. The last step for the generation of a full-length cDNA (pBAC-TGEVFL) consisted of the insertion of the ClaI–ClaI fragment from pBAC-TGEVClaI into ClaI-linearized pBAC-TGEVΔClaI. For this purpose, a third genomic ClaI site at position 18,997 had been previously deleted by PCR-directed mutagenesis, creating a silent nucleotide change. This change was also used as a rescue marker.
The TGEV cDNA was flanked at its left end by the CMV immediate-early promoter and at its right end by a 24-bp synthetic poly(A) tail followed by the hepatitis delta virus ribozyme and the bovine GH termination and polyadenylation sequences (17).
Cloned cDNA Stability.
The stability of the viral sequences cloned into pBeloBAC11 was analyzed by studying the restriction endonuclease pattern (27). At least two clones for each construction were grown in 10 ml of LB containing 12.5 μg/ml chloramphenicol at either 37°C or 30°C. Cells from these primary cultures were propagated serially by diluting 106-fold daily. Each passage was considered to represent about 20 generations.
Sequence Analysis.
DNA was sequenced with an automatic 373 DNA Sequencer (Applied Biosystems). Sequence assembly and comparison with the consensus sequence of TGEV were performed with the seqman ii and align programs (DNAstar, Madison, WI), respectively. Potential splice sites were determined with the hspl program (28).
Transfection and Recovery of an Infectious TGEV from a cDNA Clone.
ST cells were grown to 60% confluence in 60-mm-diameter plates and were transfected with 10 μg of either pBAC-TGEVFL or pBAC-TGEVFL−(ClaI)RS (pBAC-TGEVFL plasmid carrying the ClaI–ClaI fragment in the reverse orientation) with 15 μg of Lipofectin (Life Technologies, GIBCO) according to the manufacturer's specifications. The cells were incubated at 37°C for 6 h, after which the transfection medium was replaced with fresh DMEM containing 8% (vol/vol) FBS. After an incubation period of 2 days, the cell supernatant (referred to as passage 0) was harvested and passaged six times on fresh ST cells. Virus present in the cell supernatant was analyzed by plaque titration and RT-PCR. After six passages, the virus was cloned by three plaque purification steps. The specific infectivity of the cDNA was determined by standard immunofluorescence techniques with TGEV-specific monoclonal antibodies (24).
RNA Isolation and RT-PCR Analysis.
Total or cytoplasmic RNA from infected or transfected ST cells was extracted as described (16). Northern blot and RT-PCR analyses were carried out following standard procedures (29). To analyze the extent of the splicing, the cytoplasmic RNA was amplified by semiquantitative RT-PCR by using a low number of cycles within the same tube and with the same primers. The relative proportion of the spliced and nonspliced molecules was deduced from the total RNA mass and was estimated with the Gel Documentation 2000 System (Bio-Rad).
TGEV Growth Kinetics in ST Cells.
ST cell monolayers were infected at multiplicities of infection of 0.05 and 5 with strains PUR-MAD, PUR-C11, or the recovered virus rPUR-MAD-Sc11. Aliquots of 200 μl were taken from the supernatant of each infected monolayer at different times after infection, and virus titer was determined as described (24).
Virulence Assay.
The in vivo growth and virulence of TGEV isolates and the recovered virus were determined as described (22). Briefly, groups of five 3-day-old National Institutes of Health miniswine (30) were oronasally and intragastrically inoculated with doses of 1 × 108 plaque-forming units (pfu) per route with PUR-MAD, PUR-C11, or the rPUR-MAD-Sc11 viruses, in a biosafety level 3 containment facility at 21°C. The virus titers in lung, jejunum, and ileum were determined 2 days after infection.
Results and Discussion
Strategy for the Construction of a cDNA Encoding an Infectious TGEV RNA.
To obtain a cDNA encoding a full-length TGEV RNA, a cDNA encoding a TGEV-derived DI-C of 9.7 kb was constructed (16, 17). This DI-C cDNA was stable in low and high copy number plasmids. The three deletions (Δ1, Δ2, and Δ3) of about 10, 1, and 8 kb, respectively, that DI-C has relative to the parental virus were restored (Fig. 1a). The 1-kb (Δ2) deletion in ORF 1b was filled in first, thus generating a stable plasmid. The ORF-1a-missing sequences (Δ1) were restored by adding cDNA fragments A1, B1, C1, and D1 (Fig. 1a). The new cDNA plasmid was not stable within the bacteria, and mutated forms were recovered that had incorporated deletions or insertions in fragments B1 to D1 (Z.P., J.M.G., F.A., and L.E., unpublished results). Interestingly, removal of a restriction endonuclease ClaI fragment of 5,198 bp from nucleotides 4,417 to 9,615 in the TGEV sequence generated a plasmid stable in E. coli DH10B cells. Subsequently, the deleted Δ3 sequences were restored by introducing the indicated cDNAs (Fig. 1a).
To increase the stability of the TGEV cDNA, a cDNA encoding the full-length sequence of TGEV, except for the deleted ClaI–ClaI fragment, was subcloned into the BAC plasmid pBeloBAC11 (18, 26) leading to plasmid pBAC-TGEVΔClaI (Fig. 1b). TGEV cDNA was cloned downstream of the CMV immediate-early promoter. At the 3′ end, this cDNA was flanked by a 24-bp poly(A) tail, followed by the hepatitis delta virus ribozyme and the bovine GH termination and polyadenylation sequences, as described (17). The missing ClaI–ClaI sequences, required to encode the complete full-length TGEV genome, were also cloned into a BAC plasmid, pBAC-TGEVClaI, containing a cDNA complementary to TGEV RNA nucleotides 4,310 to 9,758 (Fig. 1b). Both BAC plasmids were grown in DH10B cells and sequenced. Their sequences were identical to the consensus sequence of the PUR-MAD strain with the exception of two genetic markers previously introduced in the cDNA at positions A-6,752 → G (silent) and T-18,997 → C (silent). In addition, to generate a cDNA encoding a fully active TGEV that would replicate both within the enteric and respiratory tracts and preserve the virulence of the original in vivo isolates, the complete S gene of the PUR-MAD strain, which replicates abundantly within the respiratory tract (> 106 pfu/g of tissue) and scarcely (<103 pfu/g of tissue) in the enteric tract of swine, was replaced by the S gene of PUR-C11 strain, which replicates with high titers (>106 pfu/g of tissue) within both the respiratory and the enteric tracts (22). The S gene of the PUR-C11 strain has 14 nucleotide differences compared with the S gene of the PUR-MAD strain and an insertion of 6 nucleotides at the 5′ end of the gene (22).
A full-length TGEV cDNA (pBAC-TGEVFL) containing all of the genes from the PUR-MAD strain but with the S gene from the enteric PUR-C11 strain was constructed just before cell transformation by excising the ClaI–ClaI fragment from plasmid pBAC-TGEVClaI and cloning this fragment into pBAC-TGEVΔClaI (Fig. 1b). The resulting plasmid was stable for at least 80 generations during its propagation in DH10B cells, as determined by restriction endonuclease analysis (data not shown).
Rescue of an Infectious TGEV from the cDNA.
To recover an infectious TGEV from a full-length cDNA, ST cells were transfected with plasmid pBAC-TGEVFL, and the supernatant was passaged six additional times (Fig. 2a). Virus titers quickly increased with passage and were around 108 pfu/ml by passage 4. The number of infectious units was relatively low (36 infectious units/10 μg of DNA) as determined during one cycle of virus replication, by using immunofluorescence staining of plaques denoting cell to cell virus transfer. Nevertheless, the experiment was performed six times, and in all cases, infectious virus was recovered with similar titers; however, in the mock-transfected cultures or in cells transfected with the same plasmid but carrying the ClaI–ClaI fragment in the reverse-sense (pBAC-TGEVFL−(ClaI)RS), no virus was recovered (Fig. 2a). After six passages, the virus was cloned by three plaque isolation steps, and the selected virus was named rPUR-MAD-Sc11. All of the reported experiments were performed with both uncloned and cloned virus with identical results.
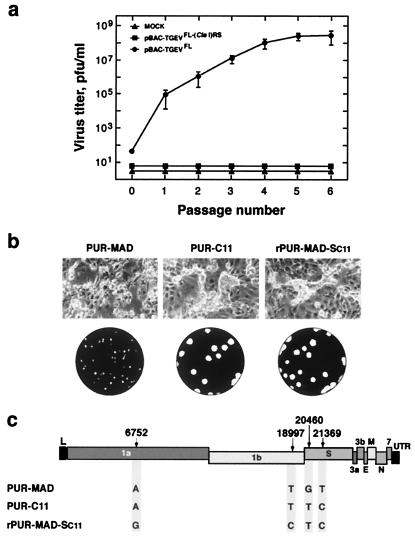
Figure 2.
Infectious TGEV recovered from cDNA. (a) Amplification of the rPUR-MAD-Sc11 virus. ST cells were transfected either with plasmid pBAC-TGEVFL encoding an infectious TGEV RNA or with plasmid pBAC-TGEVFL−(ClaI)RS encoding the coronavirus RNA carrying the ClaI fragment inserted in the reverse orientation, or they were mock transfected. The recovered virus was passaged, and the culture supernatants were titrated on ST cells. Error bars represent standard deviations of the mean from six experiments. (b) Cytopathic effect and plaque morphology produced by the indicated virus on ST cells. (c) Analysis of the genetic markers of the recovered rPUR-MAD-Sc11 virus. Nucleotide differences within the positions of the genetic markers between the rPUR-MAD-Sc11 and the parental virus providing the TGEV genome except the S gene (PUR-MAD) or the parental providing the S gene (PUR-C11) are indicated. Only 2 of the 14 nucleotide differences in the S gene between the PUR-MAD and the PUR-C11 strains are indicated. Letters on the top bar indicate the viral genes; L, leader sequence; UTR, untranslated region.
The cytopathic effects produced by the recombinant virus included induction of cell fusion and formation of large-size plaques (3-mm diameter). These characteristics are identical to those of the parental virus (strain PUR-C11), which provided the S gene, and not to the PUR-MAD strain, which provided the rest of the genome (Fig. 2b). These results suggest that the S gene is a determinant of cell fusion and plaque morphology.
ST cells infected with the rPUR-MAD-Sc11 clone were analyzed by immunofluorescence and Western blotting with monoclonal antibodies specific for the TGEV structural proteins (22, 24, 31). The recovered virus had the M and N proteins from the PUR-MAD strain and the S protein from the PUR-C11 strain, as engineered (data not shown). Furthermore, the rescued virus was neutralized by the expected TGEV-specific monoclonal antibodies (data not shown).
The cloned virus (rPUR-MAD-Sc11) was shown to originate from the cDNA construct by sequencing RT-PCR-amplified cDNA fragments, because the two nucleotide markers at positions 6,752 and 18,997 and two others at positions 20,460 and 21,369 within the S gene were those of the constructed cDNA (Fig. 2c).
The 5′ ends of the recovered virus at passages 0 and 6 were determined by 5′ rapid amplification of cDNA ends, carrying as a control the parental PUR-MAD RNA genome. In both cases, the 5′ termini were identical to the terminus of the parental virus genome (results not shown). These data strongly suggest that the initiation of the transcription was at the expected nucleotide as described by Dubensky et al. (32).
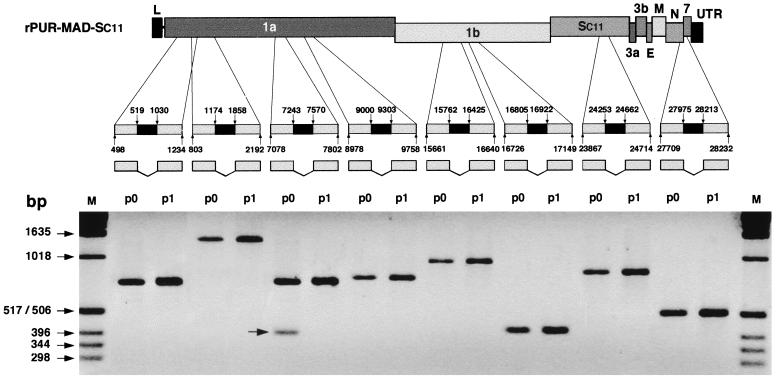
The Selected Infectious RNA Genome Underwent No Splicing.
Northern blot analysis of the genomic and mRNAs from the rescued virus showed a size apparently identical to that of the parental viruses, suggesting that there was no significant splicing of the genomic RNA during its translocation from the nucleus to the cytoplasm (data not shown). To investigate potential RNA splicing further, the sequences with the highest splicing potential along the TGEV sequence were identified (ref. 28; Fig. 3). ST cells were transfected with the infectious cDNA, and the RNA fragments with the potential splice sites were amplified by RT-PCR by using as template the cytoplasmic RNA at passages 0 and 1 (Fig. 3). Splicing was observed in only one amplified fragment that includes nucleotides 7,078 to 7,802. The splicing required this fragment to be in the virus-sense orientation, because no splicing was observed with a cDNA carrying the ClaI–ClaI fragment inserted in the reverse sense (results not shown). Furthermore, only 20% of the molecules of this fragment were spliced as estimated by semiquantitative RT-PCR. Interestingly, the genome with no splicing was favored by selection after one passage.
Figure 3.
Splicing at TGEV RNA sequence domains with high splicing potential. A databank search of the eight RNA sites with the highest probability to undergo splicing was performed as described (28). The location of the identified sites with highest splicing potential along the TGEV sequence is illustrated. ST cells were transfected with the infectious cDNA, and the potential splice sites were amplified by RT-PCR, by using as template the cytoplasmic RNA at passage zero (p0) or after the first passage (p1). The amplified DNA fragments were analyzed by agarose gel electrophoresis. Letters on the top bar indicate the viral genes; L, leader sequence; UTR, untranslated region; Sc11, S gene of PUR-C11 strain; M, molecular mass markers.
To assess definitively whether splicing had taken place in the viral RNA selected during virus replication, we determined the full-length sequence of the cloned virus. Only five nucleotide differences (C-5,903 → T, silent; T-7,587 → C, Y → H; C-20,717 → T, T → I; G-21,722 → T, G → V; and G-25,399 → A, M → I) were observed between the sequence of the rescued RNA genome and that of the cDNA clone. The first two mutations, one of which is silent, are located within the virus replicase in domains with a still undefined role (33). The following two mutations map within the 5′ one-third end of the S gene, a sequence domain known to accumulate a high number of mutations or even deletions ranging in size from 3 nucleotides to more than 670 (22, 25). The fifth mutation is located within the ORF 3b, which is not transcribed in the parental TGEV and is not essential for TGEV replication in vitro or in vivo (20, 25). These five mutations have been accumulated during a total of nine virus passages and represent an accumulation of changes that could be considered normal for an RNA virus genome (34). Thus, it is not surprising that a virus has been selected with four of five mutations that possibly will have no effect on the virus replication.
Infectious viruses have been isolated in six independent experiments. The sequences homologous to the ones showing changes in the full-length sequenced clone were determined in six clones from two independent transfections. The results showed that the six clones were different (data not shown). These data suggest that the mutations observed were not selected. Also, because these mutations are not present within the parental virus passaged in the same cell line used for the transfections, it seems reasonable to assume that the observed mutations most likely are random. Of course, the analysis of a large number of clones would be needed to rule out the selection of specific mutations during the isolation of infectious virus from the cDNA.
These results indicate that the selected molecules essentially retained the sequence of the original cDNA, and no splicing was observed within the rescued genome. In addition, these results imply that nuclear transcription of long and complex RNA molecules, followed by translocation to the cytoplasm and replication, may be a useful procedure to express RNAs, particularly when there is a selection procedure, as happens with viral genomes.
Engineering the Tropism and Virulence of the Infectious cDNA.
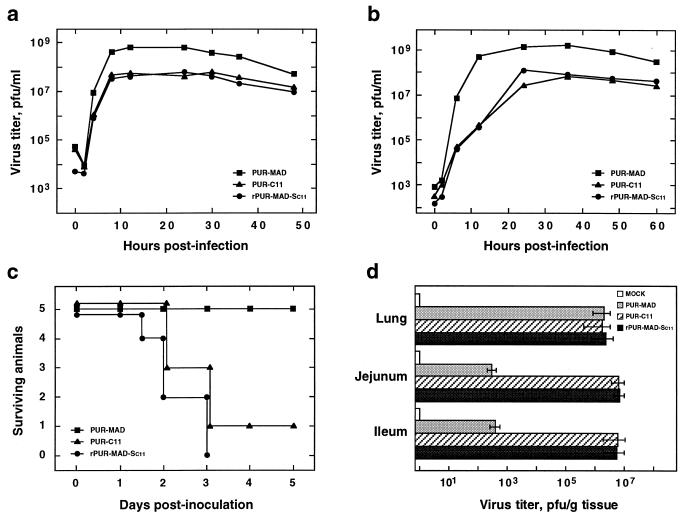
The cloned virus showed standard growth kinetics after infection at both high (5 pfu per cell) and low (0.05 pfu per cell) multiplicities of infection (Fig. 4 a and b), which were similar to those of the parental virus that provided the S gene (strain PUR-C11) and not to the PUR-MAD strain.
Figure 4.
Growth of the TGEV recovered from the cDNA in cell culture and in vivo. (a and b) Growth kinetics of rPUR-MAD-Sc11, PUR-MAD, and PUR-C11 virus on ST cells after infection at high (5 pfu per cell) and low (0.05 pfu per cell) multiplicities of infection, respectively. Mean values of three experiments are indicated. The standard deviation was lower than 30% in all cases (not shown). (c) Surviving newborn National Institutes of Health minipigs infected with rPUR-MAD-Sc11, PUR-MAD, or PUR-C11 virus at 48 h after birth with 2 × 108 pfu per animal. This experiment was performed twice with similar results. (d) Growth of rPUR-MAD-Sc11, PUR-MAD, and PUR-C11 virus in the indicated tissues. Values represent the means of representative tissue samples from three animals killed 3 days after inoculation. Error bars represent standard deviation.
The in vivo properties of clone rPUR-MAD-Sc11 also resembled those of the PUR-C11 strain (Fig. 4c), because its virulence (mortality of 100%; 10 of 10 piglets) was similar to that of the parental virus PUR-C11 (mortality of 80%; 8 of 10) when infecting breast-fed newborn animals. In contrast, the parental virus providing all of the genes except the S gene produced no clinical signs (Fig. 4c). The rPUR-MAD-Sc11 virus rescued from the infectious cDNA grew in the jejunum and ileum of infected miniswine to titers as high (>106 pfu/g of tissue) as those of the parental enteric virus providing the S gene (PUR-C11), whereas the parental virus providing all of the genome except the S gene produced low titers (<103 pfu/g of tissue; Fig. 4d). Both parental viruses and the rescued one grew very well in the lungs (106 pfu/g of tissue). It seems reasonable to conclude that the S gene is a determinant of TGEV tropism and virulence for the following reasons. (i) The sequence of the parental virus (PUR-MAD) has been compared with that of six clones of the rPUR-MAD-Sc11 (data not shown), and the only common difference is the S gene, all of the other mutations being specific to each clone. (ii) These results are complementary with our previous data (22, 35). In these reports, it is shown that, after replacing the S gene of two different TGEV respiratory strains by the S gene from the enteric isolate PUR-C11 by targeted recombination, a collection of 14 recombinants was obtained, all of which showed an enteric tropism. In this article, we have constructed similar types of recombinants but, by using a different approach, engineered the TGEV cDNA. The common feature in all of the recombinants is the replacement of the S gene.
The change in tropism based on the replacement of the S gene by one from a coronavirus targeting the required host opens up the possibility of employing the infectious cDNA as a tissue- or species-specific expression vector.
Conclusions
To our knowledge, this is the first time that an infectious cDNA has been constructed for a coronavirus. The assembled cDNA has allowed the rescue of a virulent virus that replicates both in the enteric and the respiratory tracts of swine, properties that now can be knocked out selectively to study the molecular basis of these activities. The engineered cDNA will have an important impact on the study of mechanisms of coronavirus replication and transcription and provides an invaluable tool for the experimental investigation of virus–host interactions. This cDNA may also be the basis for a tissue-specific expression system that may be used in four species—human, porcine, canine, and feline—by replacing the S gene included in the cDNA with that of the coronavirus infecting the target species. It is anticipated that by this procedure either fully infectious viruses or at least partially competent isolates able to express foreign genes will be generated, both being of practical interest.
Possibly of major interest will be the experimental evidence that two strategies used in the generation of the infectious cDNA, cloning into BACs and rescue of large RNA molecules transcribed in the nucleus, could be extended to the expression of other large-size RNAs of biological relevance.
Acknowledgments
This publication is dedicated to the memory of Prof. Eladio Viñuela, promoter of Molecular Biology in Spain. We thank I. Sola and C. G. Cámara for critically reading this manuscript. This research was supported by grants from the Comisión Interministerial de Ciencia y Tecnología (Spain), the Dirección General de Investigación (Community of Madrid), the European Community (Biotechnology, Fishery and Agro-Industrial Research and Control of Infectious Diseases Programs), and Fort Dodge Veterinaria Sociedad Aronima (Spain). F.A., Z.P., and E.C. received fellowships from the Biotechnology and Fishery and Agro-Industrial Research Programs of the European Community. J.M.G. received a fellowship from the Spanish Department of Education and Culture, and A.I. received a fellowship from the Department of Education, University and Research of the Gobierno Vasco, Spain.
Abbreviations
- kb
kilobase
- BAC
bacterial artificial chromosome
- DI
defective minigenome
- CMV
cytomegalovirus
- TGEV
transmissible gastroenteritis coronavirus
- PUR-MAD
PUR46-MAD strain
- PUR-C11
PUR46-C11 strain
- ST cells
swine testis cells
- RT-PCR
reverse transcriptase–PCR
- pfu
plaque-forming unit
Footnotes
References
- 1.Enjuanes L, Brian D, Cavanagh D, Holmes K, Lai M M C, Laude H, Masters P, Rottier P, Siddell S G, Spaan W J M, et al. In: Virus Taxonomy. van Regenmortel M H V, Fauquet C M, Bishop D H L, Carsten E B, Estes M K, Lemon S M, Mayo M A, McGeoch D J, Pringle C R, Wickner R B, editors. New York: Academic; 1999. pp. 835–849. [Google Scholar]
- 2.Lai M M C, Cavanagh D. Adv Virus Res. 1997;48:1–100. doi: 10.1016/S0065-3527(08)60286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koetzner C A, Parker M M, Ricard C S, Sturman L S, Masters P S. J Virol. 1992;66:1841–1848. doi: 10.1128/jvi.66.4.1841-1848.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van der Most R G, Heijnen L, Spaan W J M, Degroot R J. Nucleic Acids Res. 1992;20:3375–3381. doi: 10.1093/nar/20.13.3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Masters P S, Koetzner C A, Kerr C A, Heo Y. J Virol. 1994;68:328–337. doi: 10.1128/jvi.68.1.328-337.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masters P S. Adv Virus Res. 1999;53:245–264. doi: 10.1016/S0065-3527(08)60351-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rice C M, Grakoui A, Galler R, Chambers T J. New Biol. 1989;1:285–296. [PubMed] [Google Scholar]
- 8.Racaniello V R, Baltimore D. Science. 1981;214:916–919. doi: 10.1126/science.6272391. [DOI] [PubMed] [Google Scholar]
- 9.Ahlquist P, French R, Janda M, Loesch-Fries L S. Proc Natl Acad Sci USA. 1984;81:7066–7070. doi: 10.1073/pnas.81.22.7066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rice C M, Levis R, Strauss J H, Huang H V. J Virol. 1987;61:3809–3819. doi: 10.1128/jvi.61.12.3809-3819.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liljeström P, Garoff H. Biotechnology. 1991;9:1356–1361. doi: 10.1038/nbt1291-1356. [DOI] [PubMed] [Google Scholar]
- 12.Satyanarayana T, Gowda S, Boyko V P, Albiach-Marti M R, Mawassi M, Navas-Castillo J, Karasev A V, Dolja V, Hilf M E, Lewandowski D J, et al. Proc Natl Acad Sci USA. 1999;96:7433–7438. doi: 10.1073/pnas.96.13.7433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Dinten L C, den Boon J A, Wassenaar A L M, Spaan W J M, Snijder E J. Proc Natl Acad Sci USA. 1997;94:991–996. doi: 10.1073/pnas.94.3.991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schnell M J, Mebatsion T, Conzelmann K-K. EMBO J. 1994;13:4195–4203. doi: 10.1002/j.1460-2075.1994.tb06739.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fodor E, Devenish L, Engelhardt O G, Palese P, Brownlee G G, García-Sastre A. J Virol. 1999;73:9679–9682. doi: 10.1128/jvi.73.11.9679-9682.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Méndez A, Smerdou C, Izeta A, Gebauer F, Enjuanes L. Virology. 1996;217:495–507. doi: 10.1006/viro.1996.0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Izeta A, Smerdou C, Alonso S, Penzes Z, Méndez A, Plana-Durán J, Enjuanes L. J Virol. 1999;73:1535–1545. doi: 10.1128/jvi.73.2.1535-1545.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shizuya H, Birren B, Kim U J, Mancino V, Slepak T, Tachiiri Y, Simon M. Proc Natl Acad Sci USA. 1992;89:8794–8797. doi: 10.1073/pnas.89.18.8794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Messerle M, Crnkovic I, Hammerschmidt W, Ziegler H, Koszinowski U H. Proc Natl Acad Sci USA. 1997;94:14759–14763. doi: 10.1073/pnas.94.26.14759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Enjuanes L, Van der Zeijst B A M. In: The Coronaviridae. Siddell S G, editor. New York: Plenum; 1995. pp. 337–376. [Google Scholar]
- 21.Enjuanes L, Siddell S G, Spaan W J. Coronaviruses and Arteriviruses. New York: Plenum; 1998. [Google Scholar]
- 22.Sánchez C M, Izeta A, Sánchez-Morgado J M, Alonso S, Sola I, Balasch M, Plana-Durán J, Enjuanes L. J Virol. 1999;73:7607–7618. doi: 10.1128/jvi.73.9.7607-7618.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McClurkin A W, Norman J O. Can J Comp Med Vet Sci. 1966;30:190–198. [PMC free article] [PubMed] [Google Scholar]
- 24.Sánchez C M, Jiménez G, Laviada M D, Correa I, Suñé C, Bullido M J, Gebauer F, Smerdou C, Callebaut P, Escribano J M, et al. Virology. 1990;174:410–417. doi: 10.1016/0042-6822(90)90094-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sánchez C M, Gebauer F, Suñé C, Méndez A, Dopazo J, Enjuanes L. Virology. 1992;190:92–105. doi: 10.1016/0042-6822(92)91195-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang K, Boysen C, Shizuya H, Simon M I, Hood L. BioTechniques. 1997;23:992–994. doi: 10.2144/97236bm04. [DOI] [PubMed] [Google Scholar]
- 27.Kim U-J, Shizuya H, de Jong P, Birren B W, Simon M I. Nucleic Acids Res. 1992;20:1083–1085. doi: 10.1093/nar/20.5.1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Solovyev V V, Salamov A A, Lawrence C B. Nucleic Acids Res. 1994;22:5156–5163. doi: 10.1093/nar/22.24.5156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sambrook J, Fritsch E F, Maniatis T. Molecular Cloning: A Laboratory Manual. 2nd Ed. Plainview, NY: Cold Spring Harbor Lab. Press; 1989. [Google Scholar]
- 30.Sachs D, Leight G, Cone J, Schwarz S, Stuart L, Rosemberg S. Transplantation. 1976;22:559–567. doi: 10.1097/00007890-197612000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Gebauer F, Posthumus W A P, Correa I, Suñé C, Sánchez C M, Smerdou C, Lenstra J A, Meloen R, Enjuanes L. Virology. 1991;183:225–238. doi: 10.1016/0042-6822(91)90135-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dubensky T W, Driver D A, Polo J M, Belli B A, Latham E M, Ibanez C E, Chada S, Brumm D, Banks T A, Mento S J, et al. J Virol. 1996;70:508–519. doi: 10.1128/jvi.70.1.508-519.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eleouet J F, Rasschaert D, Lambert P, Levy L, Vende P, Laude H. Virology. 1995;206:817–822. doi: 10.1006/viro.1995.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Domingo E, Holland J J. Annu Rev Microbiol. 1997;51:151–178. doi: 10.1146/annurev.micro.51.1.151. [DOI] [PubMed] [Google Scholar]
- 35.Ballesteros M L, Sánchez C M, Enjuanes L. Virology. 1997;227:378–388. doi: 10.1006/viro.1996.8344. [DOI] [PMC free article] [PubMed] [Google Scholar]