Abstract
This study examines how lower extremity fatigue of the quadriceps alters gait variables related to slip propensity. Sixteen healthy young adults were recruited to walk across vinyl floor surfaces in states of fatigue and no fatigue. Kinematic and kinetic data were collected using a three-dimensional motion analysis system and force plates. The results indicated a significant increase in both the heel contact velocity and required coefficient of friction and a decrease in the transitional acceleration of the whole body center of mass and peak knee joint moment in the fatigue trials. Thus, suggesting that slip propensity could increase with fatigue. Additionally, there was increased knee flexion and reduced ankle dorsiflexion at the heel contact phase of the gait cycle during fatigue trials. These findings provide new insights into the biomechanical relationship between localized muscle fatigue and gait parameters associated with slip propensity. The present study concluded that localized muscle fatigue affects gait parameters and hence can be considered as a potential risk factor for slip-induced falls.
1. Introduction
Slips and falls related injuries and fatalities continue to pose a significant burden to industry as well as the health sector. Floors, walkways or ground surfaces are a major extrinsic factor for fall accidents, causing over 86% of all fall-related injuries [2]. Occupationally induced localized muscle fatigue (LMF) has been identified as one of the intrinsic factors contributing to slip and fall accidents [3, 4, 5]. A third of the U.S. workforce exerts considerable strength as part of the demands of their employment and experience consequent fatigue at work [6]. LMF of the lower extremity can disrupt the quality of the signal from the sensory inputs and increase the risk of slip-induced falls due to delayed response selection [5, 7, 30]. An increase in postural sway was observed after fatigue from increased workload, which appears to be associated with a greater risk of falling [5, 16].
Changes in the gait characteristics such as increase in friction demand characteristics, heel contact velocity and reduction in transitional acceleration of the whole body center of mass during a gait cycle have been noted as risk factors for slip-induced fall accidents [8, 9, 10, 25]. The knee joint musculature is considered important in producing large flexion and extension moments while recovering from a slip [11]. Fatigue of the knee extensors and hip flexor muscles is associated with decreases in stabilization time [12]. Additionally, LMF of the quadriceps adversely affects knee proprioception [13]. The quadriceps and the hamstring musculature aid control of knee flexion and extension, and fatiguing these muscle groups may affect the knee joint moment production during gait. In addition, fatiguing the lower extremity musculature may alter gait variables pertinent to slip initiation and recovery phases. Although epidemiological studies link risk of slip-induced falls with LMF, the gait changes associated with fatigue and its relationship to slip-induced fall accidents still remain unclear.
The primary objective of the current study was to investigate the effects of localized muscle fatigue of the quadriceps muscle group on gait characteristics. The relationship between changes in gait variables and higher risk of slip-initiated falls was investigated. It was hypothesized that localized muscle fatigue of the quadriceps would affect the kinematic and kinetic variables related to slip propensity leading to higher risks of slip-induced falls
2. Methods
2.1 Subjects
Sixteen healthy young adults (10 males and 6 females) participated in the study. The sample size was estimated from the results of the pilot study. The inter subject variability in the horizontal heel contact velocity during fatigue and no fatigue states was used to calculate the power [31]. Informed consent was approved by the Institutional Review Board (IRB) of Virginia Polytechnic Institute and State University (IRB #03-069-AD). The participants (mean age 24.7 ± 3.9 years, height 1.7 ± 0.1 m, Mass 65.9 ± 10.9 kg, BMI 22.1 ± 2.5 kg/m2) did not have any musculoskeletal injuries that affected their ability to perform the fatiguing exertions.
2.2 Equipment
Walking trials were conducted on a linear walkway (1.5 × 15.5m) embedded with two force plates (BERTEC # K80102, Type 45550-08, Bertec Corporation, OH 43212, USA). Kinetic data from the forces plate were collected at a sampling rate of 1200 Hz. Experimental shoes were provided to participants to minimize shoe sole differences. Twenty-three reflective markers were placed over various bony landmarks of the body [8]. A six-camera ProReflex system (Qualysis) was used to collect three-dimensional position data of the participant while walking. Kinematic data from the camera were sampled and recorded at 120 Hz. A fall arresting harness was used for safety [11]. A Biodex Dynamometer (Biodex Medical Systems, Inc., Shirley, NY) was used to induce fatigue. A special bilateral knee attachment was constructed for the Biodex. The attachment allowed participants to extend and flex both of their knees together. Maximum voluntary exertion (MVE) of both the knees was performed while applying minimal resistance when the joints returned to the original position.
2.3 Fatigue inducement and experiment protocol
Bilateral fatigue was induced by performing repetitive isokinetic knee extension movements of the quadriceps. The fatigue inducement procedures were similar to those described by Yaggie and McGregor [14], with the exception that bilateral fatigue of the quadriceps was used. All exertions were performed at 60°/s (eccentric-concentric mode), a value consistent with earlier fatigue protocols [15]. After a 5-minute warm-up on the Biodex, a MVE baseline measure was recorded. Participants performed the exertions repeatedly against a resistance set at 70% of their baseline MVE. Visual feedback was provided to the participants for their current and target moment levels. An MVE was performed at regular intervals (5 minutes) until the participants reached 60% of their baseline MVE, and this was considered to be the fatigue state.
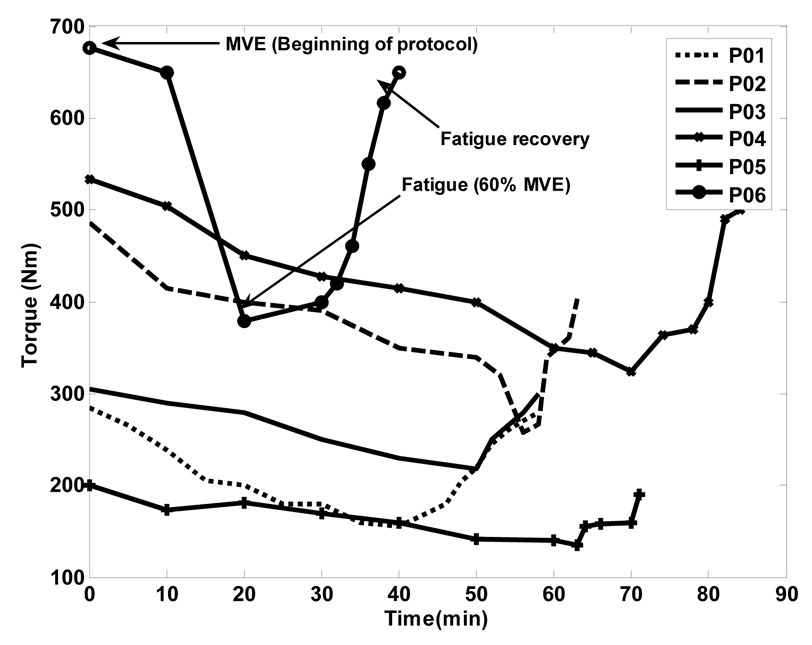
The participants were tested for two different sessions, fatigue (F) and no fatigue (NF), within a period of one week. The experiment was randomized for the two different sessions. In the NF session, participants were instructed to walk at a self-selected pace across the linear walkway for 15–20 minutes. The force plate and kinematic data were collected once the participants felt comfortable walking with the harness and produced consistent repetitive gait, i.e., the participant’s feet landed on the center of the force plate and in the desired sequence (right-left). Three gait cycles were recorded for each participant to represent the mean. In the F session, the participants performed the walking trials similar to the NF session and this was followed by the fatigue inducement procedure. Immediately after the fatiguing protocol (< 5 minutes), the participants walked across the walkway and data were collected to represent their fatigue walking. Based on the existing evidence, full recovery of the stabilometric measures is expected within about 20 minutes, but this holds true for postural sway studies after fatigue [14, 16]. To avoid confounding effects due to recovery from imposed muscle fatigue while walking, it is important to minimize the time between fatiguing exercise and data collection. The recovery time after fatigue was assessed from a pilot test conducted prior to the experiment. Six healthy young adults (3 males and 3 females) performed the fatigue exertions as described above and walked on the walkway post fatigue. Immediately after walking, they were brought back to the Biodex and their MVE was measured again. This was repeated until the participants recovered their baseline MVE. The study indicated different recovery patterns for each individual with no one returning to their baseline MVE before 10 minutes (Fig. 1). Therefore, results from the pilot study were utilized as a reference time window for data collection after fatigue inducement.
Figure 1.
Bilateral isokinetic fatigue development and recovery pattern of six young healthy adults. (demonstrates, baseline MVE- 0 minute, end of fatigue protocol at 60% MVE, and recovery period after fatigue inducement).
2.4 Data Analysis
The independent variable in this experiment was the fatigue status (F and NF). The dependent variables consisted of various kinematic and kinetic gait variables. Heel contact velocity (HCV) was calculated by numerically differentiating the position data of the heel before and after the heel contact phase of the gait cycle [8, 17]. Transitional acceleration of the whole body center of mass (TA) was defined as the change in the horizontal center of mass (COM) velocity between the heel contact phase and shortly after the heel contact phase of the gait cycle [8]. Walking velocity (WV) was obtained from the whole body COM velocity during forward progression [8]. The joint angles and angular velocities were determined using the position data as described by Liu and Lockhart [11]. The required coefficient of friction (RCOF) is defined as the ratio of horizontal ground reaction force to vertical ground reaction force. It represents the minimum required coefficient of friction between the shoe and floor interface to prevent slipping [18]. Two-dimensional sagittal knee joint moment was calculated using the inverse dynamics approach [11]. A one-way repeated measures ANOVA was used to test for significant differences between various gait parameters for two levels of fatigue (NF and F). The level of significance was set at α < 0.05. Bivariate analysis was performed to examine the correlation between the different dependent measures.
3. Results
The one-way ANOVA indicated that the participants walked with a higher HCV in the F session (F(1,31) = 33.86, p = 0.01). The TA in the forward direction was reduced after the fatiguing protocol (F(1,31) = 3.85, p = 0.04). Participants walked with a reduced speed after fatigue exertions but the differences were not statistically significant (F(1,31) = 1.52, p = 0.08). The mean and standard deviation with the statistical results is provided in Table 1.
Table 1.
Summary of kinematic and kinetic gait parameters (HCV-heel contact velocity, WV- walking velocity, RCOF-required coefficient of friction, TA- whole body COM transitional acceleration, Kneemompeak- knee moment peak P1 and P3) during the no fatigue (NF) and fatigue (F) walking trials
| Variables | Session | ANOVA | |
|---|---|---|---|
| NF mean(S.D) | F mean(S.D) | ||
| HCV (cm/s) | 81.94 (51.22) | 97.83(66.67) | * |
| WV (cm/s) | 127.02(14.42) | 119.29(20.32) | N.S |
| RCOF | 0.15(0.007) | 0.18(0.005) | * |
| TA(cm/s2) | 199.21(41.27) | 159.27(57.16) | * |
| Knee angle at heel contact (deg) | 8.47 (1.34) | 2.59(1.50) | ** |
| Ankle angle at heel contact (deg) | 93.77 (4.74) | 86.66(3.95) | ** |
| Knee angular velocity at heel contact (deg/s) | 235.09 (15.31) | 134.07 (8.58) | * |
| Ankle angular velocity at heel contact (deg/s) | 56.18 (2.41) | 69.60 (2.51) | * |
| Kneemompeak (Nm/kg) P1 | 0.47(0.19) | 0.37(0.22) | N.S |
| Kneemompeak (Nm/kg) P3 | 0.65(0.36) | 0.43(0.15) | ** |
p < 0.05
p < 0.01
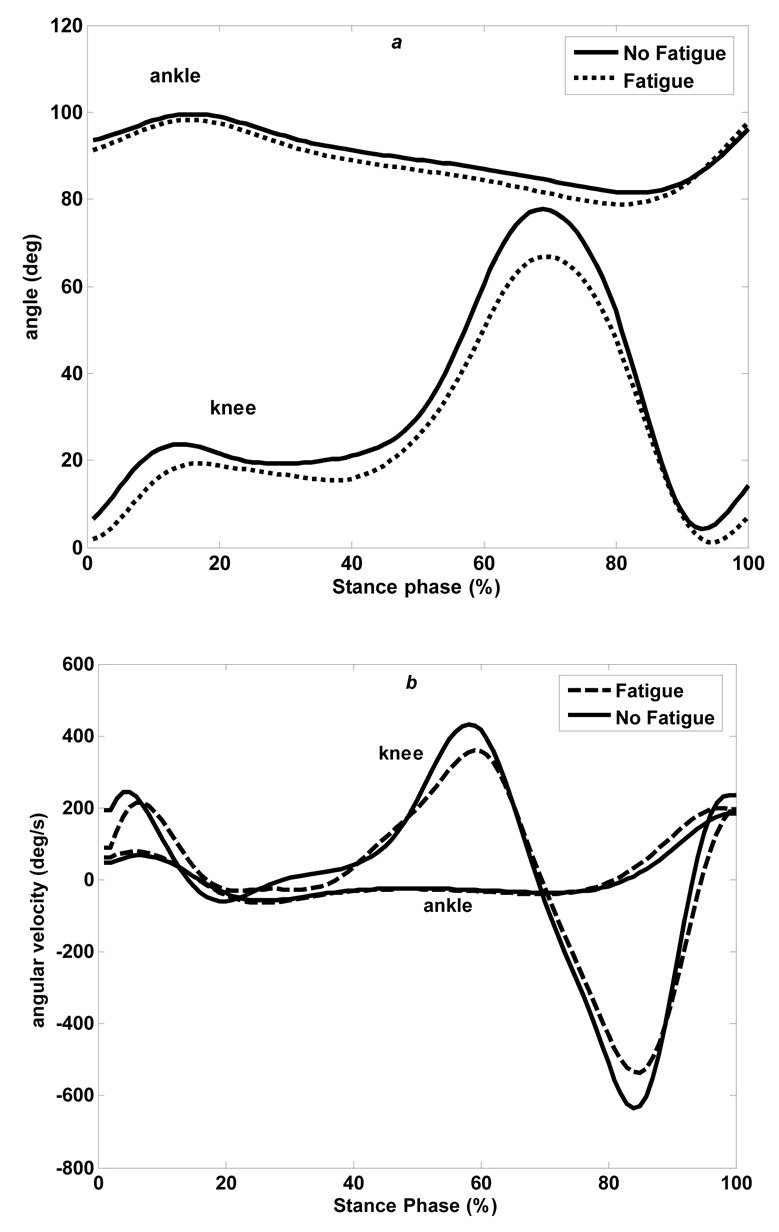
At heel contact, the ankle and knee kinematics were significantly different for NF and F sessions (ankle-F(1,31) = 18.01, p = 0.009, knee-F(1,31) = 130.02, p = 0.0001) (Table 1). The knee was flexed to a greater extent at the heel contact phase of the gait cycle during F session as compared to the NF session (Fig. 2a). The gait profile however was similar in both of the sessions, with the knee flexed for around 30 % of the stance and then flexed again during terminal stance. The ankle was in dorsiflexion at the heel contact but rapidly reached its peak plantar flexion around 15% of the stance phase for the NF session (Fig. 2a). During the F session, the ankle followed a similar gait profile but with reduced dorsiflexion and plantarflexion. The knee and ankle angular velocities were significantly different at the heel contact phase of the gait cycle in the F session (Fig. 2b, Table 1).
Figure 2.
(a) Mean profile of ankle and knee angles during the no fatigue and fatigue walking trials (b). Mean profile of ankle and knee angular velocities during the no fatigue and fatigue walking trials (+ dorsiflexion (ankle), + extension (knee)), (0- heel contact, 100- toe off).
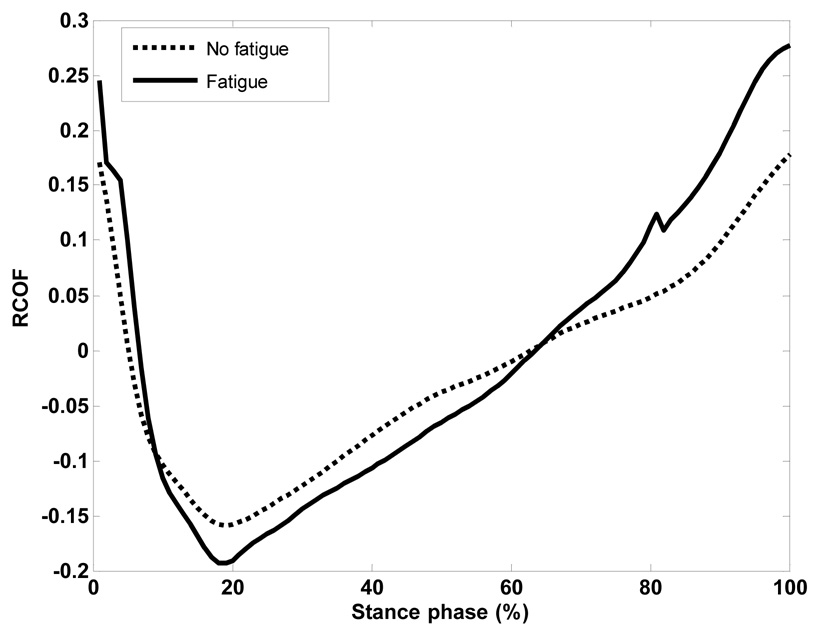
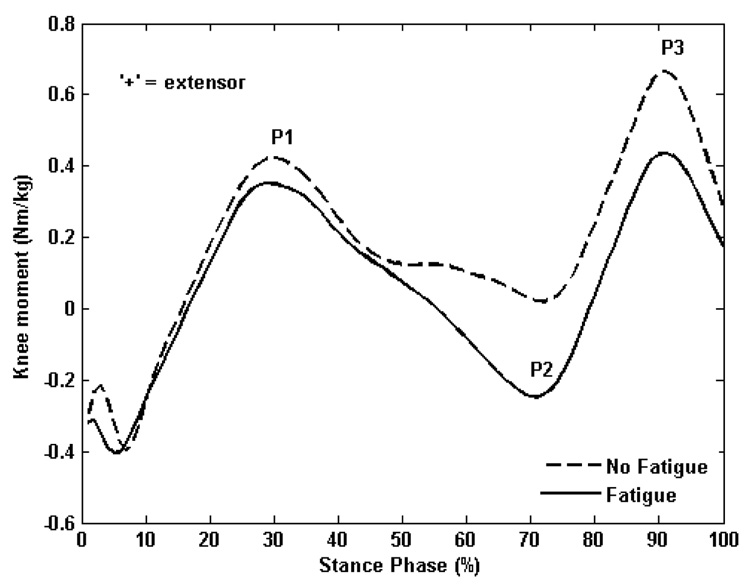
Consistent patterns of RCOF were observed during both of the sessions in all of the participants (Fig. 3). It was also observed that RCOF was higher during the F session (F(1,31) = 9.73 p = 0.04) as compared to the NF session. The sagittal knee joint moment showed flexor and extensor moment alternatively, in both NF and F sessions (Fig. 4). Two distinctive extensor moment peaks (P1 and P3) were analyzed for significant differences between the NF and F sessions. Although not statistically significant (p>0.05), there was a decrease in the peak extensor knee joint moment P1 in the F session as compared to the NF session (Table1). The Peak 3, which is also extensor dominant, was decreased in the F session and was significantly different from the NF session (F(1,23) = 16.89, p = 0.002). A second peak (P2) was observed in the F session which was flexor dominant and occurred during 60–70% of the stance phase. However, in the NF session, the joint moment profile was different with the knee less extended but not fully flexed at 60–70% of the stance phase. The bivariate correlation between the different dependent variables indicated that RCOF was positively correlated to HCV(r = 0.39, p = 0.026) and TA was positively correlated to the peak knee joint moment (P1 (r = 0.31, p=0.03), P3 (r = 0.45, p= 0.02)). Additionally, there was a negative correlation between HCV and TA (r = −0.37, p = 0.03). Although the correlations between the variables were significant, they were weak overall.
Figure 3.
Ensemble average of the required coefficient of friction (RCOF) during the no fatigue and fatigue walking trials. (0- heel contact, 100- toe off).
Figure 4.
Average knee joint moment profile at the stance phase of gait cycle during the no fatigue and fatigue walking trials. (0- heel contact, 100- toe off).
4. Discussion
The study examined the relationship between LMF and gait characteristics that may increase the risk of slip-induced falls. The results indicated that participants walked with a higher HCV after fatiguing the quadriceps. HCV affects the friction demand characteristics by altering the ratio of horizontal to vertical foot forces during walking [8]. An increase in HCV during the critical period of weight transfer may lead to a greater possibility of a slip-induced fall if the friction between the heel and the floor is reduced due to contamination of the floor surface (i.e., water, oil). The results are consistent with the study by Saggini et al. [21] who examined the effects of lower extremity fatigue and concluded that fatigue increased the gait cycle time and also increased the horizontal heel velocity. Lockhart et al. [8] studied frail older adults’ gait and found that risk of slip-induced falls were higher due to an increase in HCV [19, 20]. In this study, a positive correlation between HCV and RCOF was found. A likely factor influencing the higher HCV may be a change in the quadriceps-hamstrings co-activation rate [8]. Co-activation of hamstring and quadriceps muscles is important in heel contact dynamics. Fatigue of the quadriceps may influence this process and thereby increase the HCV. Although implicated, further EMG study is required to understand the relationship between quadriceps fatigue and the co-activation dynamics. Reduction in WV has been identified as a risk factor for slip-induced falls in the elderly [10]. Although implicated, no significant difference in WV was observed in this study. This may be attributed to the differences in individual strategy to adapt to gait speed after fatigue.
Transitional acceleration of the whole body COM is important in assessing the forward momentum of the body during recovery from a backward loss of balance. The results indicated a reduction in TA after fatiguing the quadriceps. This is in agreement with a study by Yoshino et al. [22] who found that fatigue reduces back acceleration and increases the loading rate during a gait cycle. Lockhart et al. [8] indicated that reduced push-off force of the stance leg further reduced TA and increased RCOF and risk of slip initiation.
The joint kinematics indicated that after the fatiguing of quadriceps, participants had greater knee flexion at heel contact and less knee extension during terminal stance. This was expected, as fatigue of the quadriceps may affect the knee extensors. In addition, fatigue of the quadriceps affected the ankle kinematics with less dorsiflexion at heel contact in the F session.
In terms of kinetic gait parameters, the results indicated a higher friction demand after the fatiguing protocol. The friction demand characteristics have been implicated as an important predictor variable related to severity of falls [8, 24]. The onset of lower extremity fatigue during walking changes the loading rate and increases the ground reaction forces [25]. As RCOF is dependent on the ground reaction forces (horizontal and vertical), increased ground reaction forces due to fatigue may alter friction demand characteristics. Furthermore, Lockhart et al. [8] indicated that a reduction in TA is likely to increase the friction demand at the shoe floor interface of the contacting foot. Kim et al. [10] found TA and HCV to be predictor variables for RCOF in younger adults. This is in accordance with the current study.
The average knee joint moment profiles during the NF session were in accordance with previous literature [11, 23]. The knee joint moment profile during the F session had reduced extensor and increased flexor peak moment. The peak extensor joint moment (P1) was less after fatigue, though the difference was not statistically significant for 30% of the stance phase. After midstance, there was a flexion moment peak (P2) in the F session, and the knee extension moment was significantly reduced during the push off phase of the gait cycle. Reduced push-off force of the stance leg reduces the transitional acceleration of the whole body COM and increases RCOF and risk of slip initiation [8]. The knee joint moment in the F session are contradictory to some studies in the past [26, 27]. The discrepancies may be attributed to variation in fatigue patterns (i.e., general lower extremity fatigue, dorsiflexor fatigue) in the previous studies.
One of the limitations of the present study could be that each participant reached their fatigue level at different times. These limitations could affect the results due to the difference in the fatigue level in each individual. Although implicated, the assumption of 60% of baseline MVE as fatigue state prior to testing ensured that all participants were fatigued at similar levels. Previous studies on the difference between the strength in unilateral and bilateral exertions have produced equivocal results [28]. However, a study by Jacobi et al. [29] concluded that the force production is not altered during bilateral contractions. Bilateral fatigue was induced in the current study to simulate a more realistic scenario where both limbs are fatigued (i.e., walking).
Conclusion
The present study provides evidence that there is a relationship between LMF of the quadriceps and the gait parameters that are linked with higher risks of slip-induced falls. Future research will investigate the effects of LMF of other musculatures in the lower extremities (i.e., hamstrings, ankle plantar flexors) on normal gait and slip events in a real world situation. However, results from the present study can be used as preliminary information on the specific gait parameters that are affected by LMF.
Table 2.
Nomenclature of the various variables utilized in the study
| RCOF | Required coefficient of friction |
| HCV | Heel contact velocity (cm/s) |
| TA | Transitional acceleration of the whole body center of mass (cm/s2) |
| WV | Walking velocity (cm/s) |
| Kneemompeak | Peak sagittal knee moment (Nm/kg) |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference
- 1.Courtney TK, Webster BS. Antecedent factors and disabling occupational morbidity - insights from the new BLS data. AIHAJ. 2001;62:622–632. doi: 10.1080/15298660108984662. [DOI] [PubMed] [Google Scholar]
- 2.Yoon HY, Lockhart TE. Nonfatal occupational injuries associated with slips and falls in united states. Int. J. Ind. Ergonomics. 2001;36:83–92. doi: 10.1016/j.ergon.2005.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bentley TA, Haslam RA. Identification of risk factors and countermeasures for slip, trip and fall accidents during delivery of mail. Appl. Ergonomics. 2001;32:127–134. doi: 10.1016/s0003-6870(00)00048-x. [DOI] [PubMed] [Google Scholar]
- 4.Cohen HH, Lin L. A retrospective case-control study of ladder fall accidents. J. Saf. Res. 1991;22:21–30. [Google Scholar]
- 5.Hsiao H, Simeonov P. Preventing falls from roofs: a critical review. Ergonomics. 2001;44:537–561. doi: 10.1080/00140130110034480. [DOI] [PubMed] [Google Scholar]
- 6.Swaen GMH, van Amelsvoort LGPM, Bültmann U, Kant IJ. Fatigue as a risk factor for being injured in an occupational accident: results from the Maastricht Cohort Study. Occup Environ Med. 2003;60:i88–i92. doi: 10.1136/oem.60.suppl_1.i88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lipscomb HJ, Glazner JE, Bondy J, Guarini K, Lezotte D. Injuries from slips and trips in construction. Appl. Ergonomics. 2006;37:267–274. doi: 10.1016/j.apergo.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Lockhart TE, Woldstad J, Smith JL. Effects of age-related gait changes on biomechanics of slips and falls. Ergonomics. 2003;46:1136–1140. doi: 10.1080/0014013031000139491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferber R, Osternig RL, Woolacott HM, Wasielewiski JM, Lee HJ. Relative balance adjustments to unexpected perturbations during human walking. Gait Posture. 2002;16:238–248. doi: 10.1016/s0966-6362(02)00010-3. [DOI] [PubMed] [Google Scholar]
- 10.Kim S, Lockhart TE, Yoon HY. Relationship between age related gait adaptations and required coefficient of friction. Saf. Sci. 2005;43:425–436. doi: 10.1016/j.ssci.2005.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu J, Lockhart TE. Comparison of 3D joint moments using local and global inverse dynamics approaches among three different age groups. Gait Posture. 2006;23:480–485. doi: 10.1016/j.gaitpost.2005.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller PK, Bird AM. Localized muscle fatigue and dynamic balance. Percept Mot Skills. 1976;42:135–138. doi: 10.2466/pms.1976.42.1.135. [DOI] [PubMed] [Google Scholar]
- 13.Lattanzio PJ, Petrella RJ, Sproule JR, Fowler PJ. Effect of fatigue on knee proprioception. Clin J Sport Med. 1997;7:22–27. doi: 10.1097/00042752-199701000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Yaggie JA, McGregor SJ. Effects of isokinetic ankle fatigue on the maintenance of balance and postural limits. Arch Phys Med Rehabil. 2002;83:224–228. doi: 10.1053/apmr.2002.28032. [DOI] [PubMed] [Google Scholar]
- 15.Kay D, St Clair Gibson A, Mitchell MJ, Lambert MI, Noakes TD. Different neuromuscular recruitment patterns during eccentric, concentric and isokinetic contractions. J Electromyogr Kinesiol. 2000;10:425–431. doi: 10.1016/s1050-6411(00)00031-6. [DOI] [PubMed] [Google Scholar]
- 16.Nardone A, Tarantola J, Giordano A, Schieppati M. Fatigue effects on body balance. Electroencephalogr Clin Neurophysiol. 1997;105:309–320. doi: 10.1016/s0924-980x(97)00040-4. [DOI] [PubMed] [Google Scholar]
- 17.Cham R, Redfern MS. Lower extremity corrective reactions to slip events. J Biomech. 2001;34:1439–1445. doi: 10.1016/s0021-9290(01)00116-6. [DOI] [PubMed] [Google Scholar]
- 18.Perkins PJ. Measurement of slip between the shoe and ground during walking American Society of Testing and Materials, Special Technical Publication. Vol. 649. 1978. pp. 71–87. [Google Scholar]
- 19.Winter DA. The Biomechanics and motor control of Human Gait: Normal, Elderly and Pathological. Vol. 2nd Ed. Waterloo Biomechanics, Graphic Services; 1991. [Google Scholar]
- 20.Lockhart TE, Wolstad J, Hsiang SM. Effects of Aging on the Biomechanics of Slips and Falls; Proceedings of Human Factors and Ergonomics Society Conference; 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saggini R, Pizzigallo E, Vecchiet J. Alteration of spatial-temporal parameters of gait in chronic fatigue syndrome patients. J Neurol Sci. 1998;154:18–25. doi: 10.1016/s0022-510x(97)00200-1. [DOI] [PubMed] [Google Scholar]
- 22.Yoshino K, Motoshige T, Araki T, Matsuoka K. Effect of prolonged free-walking fatigue on gait and physiological rhythm. J Biomech. 2004;37:1271–1280. doi: 10.1016/j.jbiomech.2003.11.031. [DOI] [PubMed] [Google Scholar]
- 23.Redfern MS, DiPasquale J. Biomechanics of descending ramps. Gait Posture. 1997;6:119–125. [Google Scholar]
- 24.Redfern MS, Bidanda B. Slip resistance of the shoe floor interface under biomechanically-relevant conditions. Ergonomics. 1994;37:511–524. [Google Scholar]
- 25.Syed IY, Davis BL. Obesity and osteoarthiritis of the knee: hypotheses concerning the relationship between ground reaction forces and quadriceps fatigue in long-duration walking. Med Hypotheses. 2000;54:182–185. doi: 10.1054/mehy.1999.0013. [DOI] [PubMed] [Google Scholar]
- 26.Bruggermann GP, Arndt A. Proceedings from the Eight Biennial Conference. Canadian Society of Biomechanics; 1994. Fatigue and lower extremity function. [Google Scholar]
- 27.Christina KA, White SC, Gilchrist LA. Effect of localized muscular fatigue on vertical ground reaction forces and ankle joint motion during running. Hum. Move. Sci. 2001;20:257–276. doi: 10.1016/s0167-9457(01)00048-3. [DOI] [PubMed] [Google Scholar]
- 28.Khodiguian N, Cornwell A, Lares E, DiCaprio PA, Hawkins SA. Expression of the bilateral deficit during reflexively evoked contractions. J Appl Physiol. 2003;94:171–178. doi: 10.1152/japplphysiol.00703.2002. [DOI] [PubMed] [Google Scholar]
- 29.Jakobi JM, Cafarelli E. Neuromuscular drive and force production are not altered during bilateral contractions. J Appl Physiol. 1998;84:200–206. doi: 10.1152/jappl.1998.84.1.200. [DOI] [PubMed] [Google Scholar]
- 30.Sparto PJ, Parnianpour M, Reinsel TE, Simon S. The effect of fatigue on multijoint kinematics, coordination, and postural sway stability during a repetitive lifting task. J Orthop Sports Phys Ther. 1997;25:3–12. doi: 10.2519/jospt.1997.25.1.3. [DOI] [PubMed] [Google Scholar]
- 31.Neter J, Kutner MH, Nachtssheim CJ, Wasserman W. Applied linear statistical model. Irwin: McGraw-Hill; 1996. [Google Scholar]