Abstract
Purpose
The aims of the present work were to investigate the in vitro and in vivo antiangiogenic effects of chronic temozolomide treatment on various glioma models and to demonstrate whether bevacizumab (Avastin) increased the therapeutic benefits contributed by temozolomide in glioma.
Experimental Design
The expression levels of various antiangiogenic factors in four glioma cell lines were evaluated after chronic in vitro treatment with temozolomide by Western blot. Proliferation and migration assays were performed on human endothelial cells incubated with supernatants of glioma cells treated with and without temozolomide. Orthotopic glioma models were used to evaluate the antiangiogenic effects of temozolomide in vivo and the therapeutic benefits of different temozolomide treatment schedules used alone or in combination with bevacizumab.
Results
Temozolomide, a proautophagic and proapoptotic drug, decreased the expression levels of HIF-1α, ID-1, ID-2, and cMyc in the glioma models investigated, all of which playing major roles in angiogenesis and the switch to hypoxic metabolism. These changes could be, at least partly, responsible for the impairment of angiogenesis observed in vitro and in vivo. Moreover, combining bevacizumab with temozolomide increased the survival of glioma-bearing mice in comparison to each compound administered alone.
Conclusions
In addition to the numerous mechanisms of action already identified for temozolomide, we report here that it also exerts antitumor effects by impairing angiogenic processes. We further emphasize that bevacizumab, which is an antiangiogenic drug with a different mechanism of action, could be useful in combination with temozolomide to increase the latter's therapeutic benefit in glioma patients.
Introduction
Glioblastoma (GBM) is the most frequent and most malignant human brain tumor [1,2]. Prognosis remains very poor because GBM cells dramatically invade brain parenchyma and they are naturally resistant to apoptosis and thus to most cytotoxic drugs and to radiotherapy [3,4]. The treatment of GBMs requires a multidisciplinary approach that takes the presently incurable nature of the disease into consideration and normally includes surgery, radiotherapy, and chemotherapy [5]. Although temozolomide (TMZ; Temodal) does not cure GBM patients, it significantly improves GBM patient survival and quality of life [6] even of patients harboring 9p or 10q chromosomal deletions which are associated with dismal prognosis [7]. Temozolomide exerts its antitumor effects through several distinct mechanisms of action. Temozolomide increases GBM sensitivity to radiotherapy [8] most effectively in O6-methylguanine-DNA methyltransferase (MGMT)-negative GBMs by increasing the degree of radiation-induced double-strand DNA damage [9]. Part of TMZ's cytotoxicity toward GBM cells is exerted through proautophagic [10] and/or apoptotic [11] processes. Hegi et al. [12] showed that patients who had GBMs that contained a methylated MGMT promoter benefited from TMZ, whereas those who did not were less responsive. In addition to MGMT [12,13], other determinants of sensitivity of gliomas to TMZ are p53 status, proliferation rate, and double-strand breaks (DSBs) repair [11,13]. The O6-methylguanine adducts formed by TMZ also lead to inhibition of the NF-κB signaling pathway [14], which is constitutively activated in GBMs and contributes to their resistance to cytotoxic drugs and to radiotherapy [3]. The Akt signaling pathway is also directly involved in GBM cell resistance to apoptosis [3,15], and Akt activation suppresses TMZ-induced Chk2 activation and G2 arrest, with the overriding effect being protection from TMZ-induced cytotoxicity [16]. It has also been suggested that TMZ-induced anti-GBM effects could relate to antiangiogenic effects [17–20].
Apart from all these detrimental effects of TMZ against GBM cells leading to beneficial therapeutic consequences for GBM patients, the compound can also be associated with positive effects on GBM cells. By impairing these TMZ-associated positive effects on GBM cells, at least partly, it would be possible to further increase the therapeutic benefits contributed by this drug to GBM patients. For example, TMZ can induce an autophagy-associated ATP surge that protects glioma cells and may contribute to drug resistance [21]. Fisher et al. [22] have shown that treatment of human GBM cells with TMZ activates stress mechanisms that include the angiogenesis-inducing proteins notably hypoxia-inducible factors such as HIF-1α and vascular endothelial growth factor (VEGF), leading therefore to proangiogenic signals [22]. This is in contrast to previous antiangiogenic effects reported for the drug [17–20]. We recently demonstrated that TMZ increases galectin-1 expression in GBM cells both in vitro and in vivo [23,24]. Galectin-1 is a hypoxia-regulated protein [25] that exerts potent proangiogenic effects [26] and controls GBM cell migration [27]. However, reducing galectin-1 expression in these cells by siRNA increases the antitumor effects of various chemotherapeutic agents, in particular, TMZ, both in vitro and in vivo [23,24]. We have shown that decreasing galectin-1 expression in GBM [24] models markedly impairs tumor neoangiogenesis through impairment of ORP150 expression, which leads to defects in VEGF maturation (and thus secretion) and ultimately increases the therapeutic benefits contributed by TMZ [24]. Taken together, these data strongly suggest that impairing VEGF expression in GBM would improve the therapeutic benefits of TMZ [24].
The aim of the present work was to investigate the in vitro and in vivo effects of chronic TMZ treatment on various GBM models and to identify those antiangiogenic pathways activated by the compound. Accordingly, the effects of TMZ on HIF-1α, inhibitor of differentiation factors ID-1 and ID-2 and the oncogene cMyc have been investigated. Additionally, the studies reported here aimed to demonstrate whether bevacizumab (Avastin; a humanized monoclonal antibody against VEGF, which may have activity in recurrent malignant gliomas [28]) increases the therapeutic benefits of TMZ in GBM models.
Materials and Methods
Cell Cultures and Compounds
The Hs683 (ATCC code HTB-138), U87 (ATCC code HTB-14), U373 (ATCC code HTB-17) and T98G (ATCC code CRL-1690) human GBM cell lines were obtained from the American Type Culture Collection (ATCC; Manassas, VA) and maintained in our laboratory as detailed previously [23,24,27].
Primary human umbilical vein endothelium cells (HUVECs) were obtained from umbilical cords sampled at the Erasmus University Hospital, Brussels, Belgium. The cells were isolated by collagenase treatment and were grown in endothelial cell growth medium EGM-2 MV BulletKit from Lonza (Verviers, Belgium). Human umbilical vein endothelium cell cultures were used between passages 5 and 10. Two distinct batches of HUVECs designated CH14 and HTG06 were prepared.
Temozolomide was obtained from Schering-Plough (Brussels, Belgium). Bevacizumab was obtained from Roche (Brussels, Belgium).
In Vitro Overall Growth Determination
Overall cell growth was assessed using the 3-[4,5-dimethylthiazol-2yl]-diphenyltetrazolium bromide (MTT) colorimetric assay (Sigma, Bornem, Belgium), as detailed elsewhere [23,29]. All determinations were carried out in sextuplicate. Control conditions consisted of endothelial cells cultured with endothelial cell growth medium EGM-2 MV BulletKit. Treatments were as follows: conditioned media from U373 GBM cells left untreated or treated with 100 °M TMZ for 72 hours were collected. The MTT test was performed on the two HUVEC primary cultures in the presence of these 100% conditioned media, a mixture of conditioned medium, and HUVEC EGM-2 MV BulletKit medium in various proportions ranging from 90% U373 conditioned medium + 10% endothelial cell medium to 10% U373 conditioned medium + 90% endothelial cell culture medium. As U373 cells are cultured in minimum essential medium supplemented with 5% FCS, minimum essential medium + 5% FCS-treated cells were included as an internal control.
The IC50 value, defined as the concentration that reduces the global cell growth of 50%, was calculated with the following formula: IC50 = (X2 - X1) x (50 - Y1) / (Y2 x Y1)) + X1, where X1 and X2 are the higher and lower used concentrations, respectively, that borders the concentration that reduces the global cell growth of 50% and Y1 and Y2 are the mean percentages of viable cells at the X1 and X2 concentrations, respectively.
In Vivo Orthotopic Xenografts
In vivo orthotopic xenografts of human Hs683 and U373 GBM cells in nude mice were obtained as described previously [23,24,30,31]. Briefly, 50 µl of serum-free culture medium containing 100,000 GBM cells were stereotactically injected into the brain of nude mice. All mice (6-week-old female nu/nu mice; 21 to 23 g; Iffa Credo, Charles Rivers, Arbresle, France) of a given experiment have Hs683 or U373 GBM cells stereotactically implanted into the brain on the same day. Each experimental group contained 11 mice. All the in vivo experiments described in the present study were performed based on Authorization #LA1230509 of the Animal Ethics Committee of the Federal Department of Health, Nutritional Safety, and the Environment (Belgium).
In Vivo Determination of Tumor Neoangiogenesis
Each mouse receiving a GBM orthotopic xenograft underwent euthanasia (in a CO2 atmosphere during 5 min) for ethical reasons when it had lost 20% of its body weight compared to the day of tumor grafting. The brain was removed from the skull, fixed in buffered formalin for 5 days, embedded in paraffin, and then cut into 5-µm-thick sections. Resulting histology slides were stained with hematoxylin and eosin for blood vessel counts. To quantify the level of angiogenesis, a grid was used to determine the surface area of blood vessels in brain sections as reported previously [31,32]. Antiangiogenic effects were analyzed in two distinct GBM models U373 (Figure 1C) and Hs683 (Figure 1D) with and without treatment with TMZ. The types of blood vessels taken into account are illustrated in Figure 2A. A minimum of five fields at a Gx400 magnification were analyzed per histologic slide and two slides were analyzed per tumor. Thus, a minimum total of 10 histologic fields per tumor were analyzed.
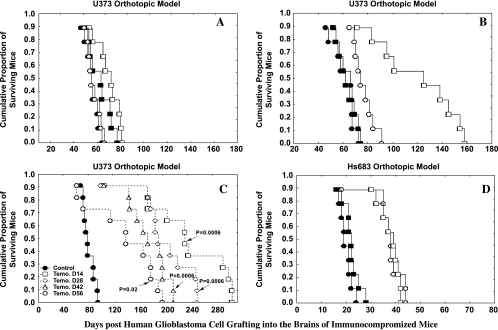
Figure 1.
TMZ in GBM models in vivo. (A) Intravenous TMZ treatment of immunocompromised mice bearing orthotopic xenografts of human U373 cells. The black symbols illustrate the survival of control (untreated) groups, whereas the open symbols show the groups treated i.v. with 40 mg/kg TMZ three times a week for three consecutive weeks, with the treatment starting on the 14th day after tumor graft. The two pairs of circles versus squares represent two independent experiments performed 6 months apart. (B) The legend is identical to that of (A), but the mice were treated for four (circles) or five (squares) consecutive weeks instead of three consecutive weeks. (C) Oral TMZ treatment of immunocompromised mice bearing orthotopic xenografts of human U373 cells. The black symbols illustrate the control (untreated) group, whereas the open symbols show the group treated with 80 mg/kg TMZ three times a week for five consecutive weeks, with treatment starting on the 14th, 28th, 42nd, or 56th day after tumor graft. (D) Intravenous TMZ treatment (40 mg/kg) of immunocompromised mice bearing orthotopic xenografts of human Hs683 cells. The black symbols illustrate the control (untreated) group, whereas the open symbols show the group treated with 40 mg/kg TMZ three times a week for three consecutive weeks, with the treatment starting on the 7th day after tumor graft. The two pairs of circles versus squares represent two independent experiments performed at 6 months apart.
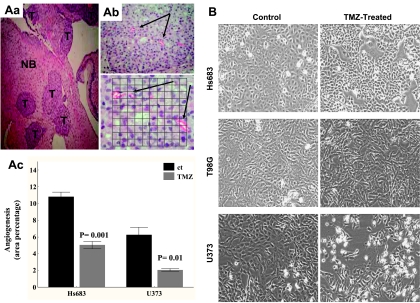
Figure 2.
Impact of TMZ administration on angiogenesis in GBMs. (A) Aa shows the typical morphologic and infiltrative characteristics of the Hs683 tumor (T) in the excised brains of mice (HE indicates Gx40; NB, normal brain tissue). Ab illustrates blood vessels in this tumor (black arrows, HE; upper panel, Gx100; lower panel, Gx400). The grid was used at Gx400 to determine the area covered by blood vessels in the tumor field. Ex vivo quantitative data on percent surface area attributable to blood vessels are presented in Ac for Hs683 and U373 control and TMZ-treated tumors excised from experiments defined in Figure 1, D and C, respectively. Results for excised U373 tumor relate to TMZ treatment starting on day 56 after tumor graft (Figure 1C, open circles). Results for excised Hs683 tumor relate to TMZ treatment starting on day 7 after tumor graft (Figure 1D, open symbols). (B) The effects of TMZ treatment on the overall growth of three different GBM cell cultures, namely, Hs683, T98G, and U373. Phase-contrast pictures of the three GBM cell lines left untreated or treated for 7 hours for five consecutive days with 100 µM TMZ (pictures taken 7 days after the last treatment).
In Vitro Determination of HUVEC Capillary Networking
When cultured on Matrigel, HUVECs form capillary-like networks [31]. An amount of 800 µl of cold Matrigel was allowed to set at 37°C for 10 minutes in a 3-cm Petri dish. The HUVECs growing as primocultures in 25-mm2 flasks (Nunc, VWR, Leuven, Belgium) were trypsinized, counted, and resuspended in the following culture media: control medium was composed of 90% untreated U373 conditioned medium mixed with 10% EGM medium; treated medium was composed of 90% conditioned medium of TMZ-treated U373 cells mixed with 10% EGM medium. U373 conditioned media were prepared as detailed above. A total of 250,000 HUVECs were seeded onto the matrix for each experiment conducted in duplicate. Formation of capillary networks was observed during 24 hours by means of a computer-assisted stereomicroscope (Olympus SZ-40; Omnilabo SA, Antwerp, Belgium).
Protein Expression Measurements
Western blot analyses were performed as detailed previously [29,33]. Briefly, 40 µg of denaturated protein extracts was loaded in a polyacrylamide gel. After electrophoresis, proteins were transferred onto a polyvinylidene fluoride membrane. To avoid aspecific binding of the antibodies, membranes were first blocked in a 5% milk or BSA buffer for 1 hour. The proteins were then detected by overnight incubation at 4°C with the following primary antibodies: anti-HIF-1α (dilution of 1:200; Abcam, Cambridge, UK), anti-ID-1 and -ID-2 (both at a dilution of 1:400; Santa Cruz, Heidelberg, Germany), anti-cMyc (dilution of 1:400; Santa Cruz), and antitubulin (dilution of 1:10,000; Abcam). Secondary antibodies were purchased from Pierce (PerbioScience, Erembodegem, Belgium). Control experiments included the omission of the incubation step with the primary antibodies (negative control). Tubulin immunoblot analysis was then performed on each membrane to assess the integrity and quantity of the extracts. Western blots were developed using the Pierce Supersignal Chemiluminescence system.
Statistical Analyses
Survival analyses were carried out by means of Kaplan-Meier curves and Gehan's generalized Wilcoxon test. Statistical comparisons between control and treated groups were established by carrying out the Kruskal-Wallis test (a nonparametric one-way analysis of variance) or the Mann-Whitney test (in the case of two groups). All statistical analyses were undertaken using Statistica (Statsoft, Tulsa, OK).
Results
Investigation of the Duration of TMZ Treatment on the Survival of U373 and Hs683 Human GBM Orthotopic Xenograft-Bearing Immunodeficient Mice
The U373 model is of astroglial origin and displays weak if any sensitivity to proapoptotic cytotoxic drugs [30], whereas the Hs683 model is of oligodendroglial origin [30] and is sensitive to proapoptotic drugs [30]. Both dramatically invade the brain parenchyma, and surgery has been demonstrated to be of limited therapeutic benefit in the U373 GBM model [34].
At a dosage of 40 mg/kg i.v. three times a week (Monday, Wednesday, and Friday) for three consecutive weeks which displayed no toxicity to mice (data not shown), TMZ (open symbols) did not significantly increase (P > .05) the survival of U373-bearing mice compared to controls (Figure 1A, black filled symbols). The two pairs of symbols: circles versus squares represent two independent experiments performed 6 months apart. Increasing the length of TMZ treatment (40 mg/kg i.v.) to three times a week for 4 weeks resulted in a weak but statistically significant increase in survival time (P < .05; Figure 1B, open circles). However, increasing further the length of TMZ treatment (40 mg/kg i.v.) to three times a week for 5 weeks markedly and significantly increased survival times in U373-bearing mice (P < .01; Figure 1B, open squares). Therapeutic benefits were also seen in the U373 GBM model when TMZ was administered orally at 80 mg/kg three times a week for five consecutive weeks, with marked improvements in survival time when the compound was administered for the first time on the 14th as opposed to the 56th day after tumor graft (Figure 1C).
The higher sensitivity of Hs683 to cytotoxic drugs compared to the U373 GBM model [30] was also observed here with respect to TMZ, as evidenced by a comparison of the data presented in Figure 1, D (Hs683) and A (U373). Mice bearing Hs683 xenografts were also treated with 40 mg/kg i.v. three times a week for 3 weeks.
Characterization of the In Vivo TMZ-Induced Effects on Angiogenesis in U373 and Hs683 Human GBM Orthotopic Xenografts
The levels of angiogenesis were evaluated by determining blood vessel surface area per field on histologic slides as detailed previously [31] and as illustrated in Figure 2Ab in the case of Hs683 GBM. For this analysis, brain samples were taken from animals implanted with U373 or Hs683 GBM and treated, respectively, as detailed in Figure 1, C (control versus TMZ 80 mg/kg p.o., 3i x 5w from 14 to 56 days after graft) and D (control versus TMZ 40 mg/kg i.v., 3i x 5w from 7 days after graft). A significant decrease in angiogenesis was found in U373 tumor samples when the TMZ treatment started on day 56 (Figure 2Ac) after tumor graft, whereas this was not the case if the treatment began earlier (data not shown). By contrast, clinical outcome (in survival) has been shown to be more improved when TMZ treatment started earlier (Figure 1C). This apparent discrepancy between the therapeutic benefits and the antiangiogenic effects of TMZ treatment could, however, be explained, at least partly, by the shorter time lapse between the end of TMZ treatment and the time of euthanasia for analysis when treatment started on day 56 (median time, ∼50 days) than the time lapse of the other groups (median time for the group beginning treatment on day 14, ∼170 days). For those later, angiogenesis could have reincreased after TMZ treatment. This hypothesis was further re-enforced with the significant decrease in angiogenesis obtained in the case of the more aggressive and shorter-lived Hs683 mouse model (Figure 2Ac) for which the delay between the last TMZ administration and euthanasia is quite short (median time, 12 days). Taken together, these data suggest that TMZ could act as an antiangiogenic compound in vivo.
Effects of TMZ on the Growth Characteristics of Human U87, T98G, U373, and Hs683 GBM Cell Lines In Vitro
In vitro IC50 inhibitory growth values for TMZ after 3 days of culture were 472 ± 14 µM for U87, 118 ± 3 µM for U373, 634 ± 23 µM for T98G, and 719 ± 12 µM for Hs683 GBM cells. These data are in accordance with those reported by Fisher et al. [22] who observed that a TMZ dose-related decrease in U251 and U87 GBM cell numbers was evident at a TMZ concentration of 200 µM, which became evident on day 6 and peaked after 8 days with a 3.5-fold reduction in cell viability.
U87, U373, T98G, and Hs683 GBM cells were treated in vitro in a chronic manner with 100 µM TMZ. The drug was added to the culture media each day for 7 hours (after that, the media were replaced with fresh medium without drug for 17 hours) for five consecutive days, and protein analyses were performed on the 3rd, 5th, and 7th days that followed the 5th TMZ administration to the GBM culture media (Figures 3 and 4). The morphologic illustrations in Figure 2B show that a treatment of 5 x 100 µM TMZ (with an observation 7 days after the 5th TMZ administration) did not impair T98G cell population growth, slightly impaired U87 (data not shown) and Hs683 cell population growth, and moderately impaired U373 cell population growth. These data are in accordance with those reported by Kanzawa et al. [10] who observed that 100 µM TMZ impaired cell growth and caused cell cycle arrest in the G2/M phase in U373 GBM cells but not in T98G cells. Thus, the in vitro 5 x 100 µM treatment adopted here for four distinct human GBM cel lines slightly, if any, impaired their growth characteristics. This protocol was then used to investigate whether TMZ was able to modify the expression levels of various key factors implicated in tumor angiogenesis as detailed below.
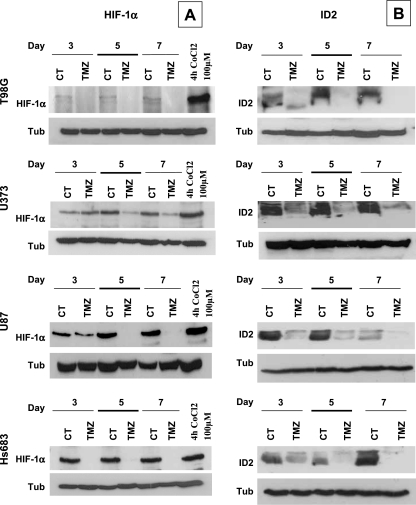
Figure 3.
Western blot analyses of the expression levels of HIF-1α and ID2 in Hs683, U373, T98G, and U87 GBM cell lines. Cells were treated for 7 hours for five consecutive days with 100 µM TMZ or left untreated. Protein extracts were collected on days 3, 5, and 7 after the last TMZ treatment. Tubulin blots were used to assess equal loading in each experiment.
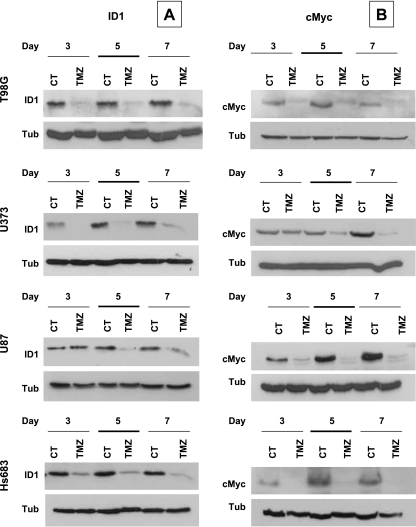
Figure 4.
Western blot analyses of the expression levels of ID-1 and c-Myc in Hs683, U373, T98G, and U87 GBM cell lines. Temozolomide treatment, sample processings, and legends are similar to those of Figure 3.
Characterization of TMZ-Induced Antiangiogenic Effects in Human U87, T98G, U373, and Hs683 GBM Cell Lines
When treating U87 and U251 GBM cells for 4 days with 100 µM TMZ, Fisher et al. [22] observed a common up-regulation of 61 genes in these two cell lines, with 14 of these genes being known to be up-regulated by the transcription factor HIF-1α. Analyzing the data provided by Fisher et al. [22] and our own previous results [23,24] of the potential relationship between endoplasmic reticulum stress, angiogenesis, and TMZ treatment in experimental GBMs and the data emphasizing the antiangiogenic effects of TMZ in various GBM models [18,19] or in GBM patients [17], we decided to investigate the effects of TMZ on hypoxia-related and proangiogenic factors, i.e., HIF-1α, ID-1, ID-2, and c-Myc. Cell lines were treated for 7 hours/day for 5 days with 100 µM TMZ or vehicle alone (controls) as indicated above, and samples were analyzed 3, 5, and 7 days after the last TMZ treatment.
Temozolomide produced a marked and sustained decrease in HIF-1α expression in the four GBM cell lines investigated (Figure 3A). Positive controls obtained by treating cells with 100 µM CoCl2 for 4 hours showed a marked increase in HIF-1α expression level.
ID factors, a family of four proteins interfering with transcription factors and preventing their activities, are implicated in the control of differentiation and cell cycle progression during embryogenesis and tumorigenesis but have also been shown to be major players in angiogenesis control [35]. ID-1 and ID-3 are required for endothelial cell proliferation, networking processes, and for endothelial precursor recruitment [35,36]. ID-2 is an HIF-1α-inducible protein [37] that exerts a major role in angiogenesis [35] as it functions as a master regulator of VEGF expression [38]. Temozolomide treatment of the four GBM cell lines led to a generally marked and sustained decrease in ID-1 and ID-2 expressions (Figures 3B and 4A).
The c-Myc oncogene has been shown to be involved in the angiogenic switch of tumors. This activity relates to modification in pro- versus antiangiogenic factor expression [39,40] and to a deep involvement in metabolic adaptation to hypoxia [41,42]. Although the proto-oncoprotein c-Myc seems to be the diametric opposite of HIF-1α in most processes, recent studies indicate that c-Myc is an integral part of the HIFs/c-Myc molecular pathway in the hypoxic response. It has been shown that HIFs engage with c-Myc by various mechanisms to achieve oxygen homeostasis for cell survival [42]. Temozolomide, which is a proautophagic agent, induced a significant and sustained decrease in the expression of c-Myc (up to 7 days after final drug treatment) in the four GBM cell lines (Figure 4B).
Characterization of TMZ-Induced Effects on Antiangiogenic Factors in HUVEC Endothelial Cell Lines
When TMZ is provided to GBM patients, it will target not only GBM cells but also a large set of cell types implicated in tumor angiogenesis, including endothelial cells. As shown above, TMZ modifies the expression levels of various angiogenic factors in GBM cells. These changes could lead to modifications to the microenvironment of tumor endothelial cells and thus to tumor angiogenesis. This hypothesis was evaluated in vitro by analyzing the effects of GBM cell culture supernatants on the global growth level of HUVEC cell lines. U373 GBM cells were treated for 72 hours with 100 µM TMZ or left untreated. The collected supernatants either neat or diluted with fresh HUVEC culture medium in different proportions were incubated with HUVEC endothelial cells and viability/proliferation assessed using the colorimetric MTT assay. Conditioned media from untreated U373 GBM cells induced a significant increase in the global growth of the two different primary HUVEC cell lines CH14 and HTG06 compared to endothelial growth medium (Figure 5A). By contrast, conditioned media from TMZ-treated U373 cells induced a significant decrease in the overall growth of these two primary HUVEC cell lines when compared to either endothelial cell culture medium (reported as 100% global growth in Figure 5A) or to conditioned media from untreated U373 cells. These results seem to indicate that TMZ exerts a marked indirect antiangiogenic effect in vitro, which may relate to the compound's effects on the expression of the proangiogenic factors studied above. Indeed, when TMZ is added alone into the endothelial culture medium, no effects are observed either on global growth or on capillary networking (data not shown).
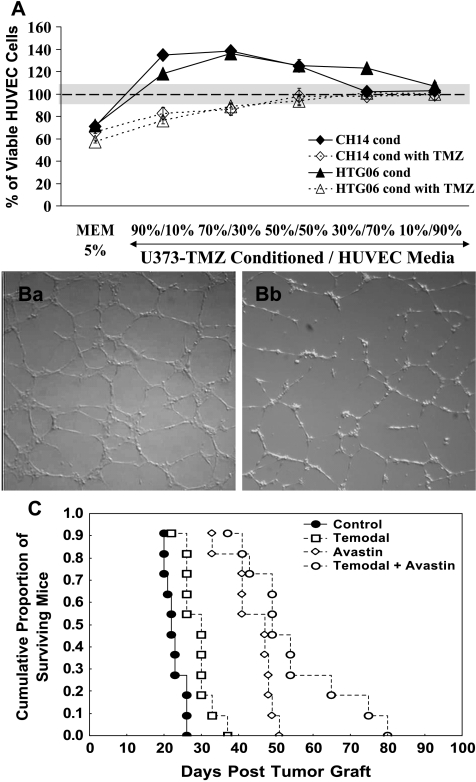
Figure 5.
Temozolomide effects on HUVECs in vitro and in combination with bevacizumab in vivo in GBM models. (A) Graphical representation of the effects of GBM conditioned media, either from U373 GBM cells treated with TMZ or left untreated, on the global growth of HUVECs. These results were obtained with the MTT assay. The percentage of viable HUVEC control cells was arbitrarily reported as 100%. The gray zone corresponds to the SEM of the control condition. The control condition was HUVECs cultured in endothelial cell growth medium EGM-2 MV BulletKit. Minimum essential medium, 5%, was the culture medium for U373 cells. CH14 and HTG06 were two independent batches of HUVECs. These were cultured in mixtures of conditioned medium from U373 cells (either untreated: CH14 and HTG06 “cond”; or treated with TMZ: CH14 and HTG06 “cond with TMZ”) and endothelial cell growth medium EGM (x axis). Results are presented as mean ± SEM. (B) Typical illustrations of the capillary networks formed by HUVECs when cultured for 24 hours on Matrigel. Ba relates to HUVECs cultured with 90% untreated U373 conditioned medium mixed with 10% EGM medium. Bb relates to HUVECs cultured with 90% conditioned medium of TMZ-treated U373 cells mixed with 10% EGM medium. (C) Survival analysis graphs for the in vivo Hs683 orthotopic GBM model treated with either TMZ (open squares) or bevacizumab (open diamonds) compounds alone or a combination of both drugs (open circles). Control groups are represented by black circles. Temozolomide and bevacizumab were administered separately or in combination at 40 mg/kg p.o. and 10 mg/kg i.v., respectively, three times per week for three consecutive weeks. Drug administration began 5 days after GBM cell grafting.
As a further evaluation, the effects of the GBM conditioned medium on the tubulogenesis of HUVECs were determined. Human umbilical vein endothelium cells were first treated for 24 hours with the GBM conditioned media detailed previously and then evaluated for capillary-like structure formation when seeded on a Matrigel matrix in the same conditioned culture medium. Figure 5Ba illustrates the tubular network formed by HUVECs cultured with a mixture of 90% untreated U373 conditioned medium and 10% endothelial culture medium. Using the U373 cells conditioned medium treated for 72 hours with 100 µM TMZ led to impairment of the tubular networking abilities of HUVECs as illustrated in Figure 5Bb. The antiangiogenic effects of TMZ observed in vivo could therefore be related to modifications in proangiogenic factor expression evidenced above in GBM cells in vitro.
Effects of Combining Bevacizumab and TMZ in Human GBM Orthotopic Xenograft Models
The Hs683 GBM orthotopic model was used to evaluate the potential of combining TMZ with bevacizumab, an antiangiogenic antibody targeting VEGF approved for the treatment of specified cancer indications [43].
Temozolomide and bevacizumab were administered individually or in combination at 40 mg/kg p.o. (suboptimal doses) and 10 mg/kg i.v., respectively, three times per week for three consecutive weeks. Drug administration began 5 days after GBM cell grafting. Temozolomide alone significantly improved animal survival times in Hs683 model (P = .002; Figure 5C). Hs683 was also responsive to bevacizumab, which had a more marked effect on animal survival times than TMZ (P < .0006 compared to the control group). However, the combination of bevacizumab with TMZ improved significantly the therapeutic benefits of TMZ or bevacizumab alone in this GBM model (P = .0008 and P = .02, respectively; Figure 5C). Similar experiment has been conducted in a human primary culture-derived orthotopic GBM model. Whereas this latter was highly responsive to temozolomide but did not respond to bevacizumab alone, combination of both treatment significantly (P < .001) improved the therapeutic benefits of temozolomide (data not shown).
Discussion
In addition to the large set of mechanisms of action already identified for TMZ's antitumor activities, the present study emphasizes that the compound also exerts its effects by impairing angiogenic processes. Indeed, it has been demonstrated in vitro in this study that the overall growth of HUVEC endothelial cell was decreased and capillary network formation impaired when these cells were treated with conditioned culture media from GBM cells treated with TMZ (Figure 5, A and B). Similar features have been recently observed with the cdk inhibitor SNS-032 [44]. The effects observed with TMZ could occur, at least partly, through a TMZ-induced decrease in the expression levels of several proangiogenic factors as indicated in Figures 3 and 4.
Hypoxia plays a major role in the induction and stimulation of angiogenesis through transcription factors like HIF family members or oncogenes like c-Myc. The present study shows that TMZ is able to inhibit HIF-1α expression in GBM cells. HIF-1α belongs to a heterodimeric transcription factor family composed of α and β subunits [45]. In general, angiogenesis is dependent on the accumulation of HIFs [45]. HIF-1 is among the primary genes involved in the homeostatic process, which can increase vascularization in hypoxic areas such as localized ischemia and tumors [45]. Moreover, the hypoxia-induced metabolic switch to the anaerobic regimen of cancer cells involves the activation and interplay of HIF and c-Myc transcription factors [41,42]. The proangiogenic activities of the latter relate to induced expression and release of interleukin 1β [39], which acts as proangiogenic factor, and decreasing thrombospondin-1 expression, which itself acts as an antiangiogenic factor [40]. Figure 4 reveals that TMZ induces a marked decrease in c-Myc expression in GBM cells. Given the important role of c-Myc in the hypoxic metabolism switch, it remains possible that the decrease in its expression induced by TMZ treatment could impair cell survival in an adverse hypoxic environment and induce autophagic processes which have been well documented by Kanzawa et al. [10] in the case of TMZ treatment of glioma.
It has been previously shown that TMZ increases the expression levels of galectin-1 in gliomas [23,24]. Galectin-1 is a potent proangiogenic factor [26] involved in the endoplasmic reticulum stress response [24]. In fact, regulation of angiogenesis results from the fine tuning of the balance between pro- and antiangiogenic factors [45]. Here, we have shown that TMZ induced a marked decrease in the expression of a number of proangiogenic factors leading to antiangiogenic effects, not only in vitro but also in vivo, as revealed in Figure 2, A and B. Our results therefore support previous publications demonstrating that conventional and metronomic TMZ treatments have antiangiogenic properties [17–20]. However, it still remains possible to increase the therapeutic benefit of TMZ with antiangiogenic approaches/compounds having different targets. This was previously evidenced by decreasing galectin-1 expression [24], which impaired VEGF maturation and secretion [23] and by knocking down HIF-1α (Table 1) [46].
Table 1.
Review of the Studies Combining Antiangiogenic Approaches With TMZ Treatment in GBM Models.
| Compound | Properties | Model | Graft | Effects | References |
| TNP-470 | Inactivates MetAP2 resulting in endothelial cell cycle arrest; antiangiogenic | Rat C6 | s.c. | ↓ TMZ concentrations in the tumor interstitial fluid | [47] |
| ↓ of microvessels | |||||
| Human SF188 [VEGF-] and transfected VEGF + | s.c. and i.c. | ↓ TMZ tumor concentrations | [48] | ||
| ↓ TMZ tumor/plasma ratio in both s.c. and i.c. models | |||||
| ↓ of microvessels [only in VEGF +] | |||||
| SU-5416 | VEGFR-2 inhibitor antiangiogenic | Human SF188 transfected VEGF + | s.c. and i.c. | ↑ TMZ tumor/plasma ratio only in i.c. models and not s.c. | [49] |
| ↓ of microvessels | |||||
| Thalidomide [THD] | Immunomodulator [↓ TNF-α] sedative, hypnotic antiangiogenic | Rat C6 | i.c. | THD +TMZ tumor growth <TMZ or THD with ↑ apoptosis, ↓ bFGF and VEGF by TMZ or THD | [18] |
| HIF-1α knockdown | Antiangiogenic | Human D54MG | s.c. | ↑ TMZ therapeutic benefit | [46] |
| ↑ cytotoxic effects of TMZ in vitro under hypoxia | |||||
| Vandetanib | Anti-Tyr kinases VEGFR-2 and EGFR; antiangiogenic | Human E98 and U87 | i.c. | ↓ TMZ therapeutic benefit, restore the BBB | [50] |
| ↓ TMZ-induced apoptosis | |||||
| Sunitinib | Anti-Tyr kinases [VEGFR1 VEGFR3, PDGFR, stem cell factor receptor…]; antiangiogenic | Human SF188 transfected VEGF + | s.c. | ↑ TMZ tumor/plasma ratio vascular normalization | [51] |
| Galectin-1 siRNA | Decreases the unfolded protein response, impairs VEGF maturation and secretion | Human Hs683 | i.c. | ↑ TMZ therapeutic benefit | [24] |
The principal property of each compound is underlined.
The present study shows that administering in combination TMZ and bevacizumab to Hs683 orthotopic GBM-bearing mice markedly delayed death in these animals compared to when each drug was administered alone (Figure 4). All in vivo studies conducted to date with TMZ in combination with antiangiogenic approaches for the experimental treatment of glioma models are summarized in Table 1. Therapeutic approaches combining antiangiogenic drugs such as bevacizumab with cytotoxics have recently entered routine practice for cancers in general [43,52]. For example, in the case of breast cancer, bevacizumab exerts potent antiangiogeneic activities [53] and potentiates paclitaxel antitumor effects [54]. The success of such combinations could result from at least three different mechanisms of action as emphasized by Kerbel [55]: 1) preventing nutrient supply for tumor cell repopulation, 2) normalization of tumor vasculature leading to improved cytotoxic drug delivery inside the tumor, and 3) increasing the antiangiogenic effects of the chemotherapeutic agents themselves.
Owing to well-known abnormalities, tumor blood vessel walls are leaky, leading to an increase in interstitial pressure, which in turn interferes with the diffusion of therapeutic agents into the tumor. Therefore, blood vessel normalization obtained with antiangiogenic compounds could be associated with higher drug tumor/plasma ratios as shown by Ma et al. [49] (Table 1) and recently by Zhou et al. [51] (Table 1) in the case of TMZ in glioma model treatment. However, in the case of brain tumors, blood vessel normalization could be linked to the restoration of the blood-brain barrier (BBB) which could hinder the transendothelial diffusion of anticancer agents like TMZ. This process has been evidenced in a human orthotopic glioma model (Table 1) [50]. A better understanding of the resulting effects of such combinations might be achieved when taking into account the tumor models (s.c. versus orthotopic implantation) and/or the antiangiogenic compounds used, which are characterized by different mechanisms of action leading to either synergistic or negative effects. Combination therapy of bevacizumab and a cytotoxic seems well tolerated and active against recurrent malignant gliomas [28,43]. Bevacizumab may alter the recurrence pattern of malignant gliomas by suppressing enhancing tumor recurrence more effectively than it suppresses nonenhancing infiltrative tumor growth [28]. However, Chamberlain [56] raises the point why the use of irinotecan in combination with bevacizumab in a phase 2 study [43] despite consideration of the extremely limited single-agent activity of irinotecan in recurrent GBM.
Antiangiogenic compounds also seem to be promising in increasing the therapeutic benefits of radiotherapy [57]. A phase 2 pilot study of bevacizumab in combination with TMZ and regional radiotherapy for the treatment of patients with newly diagnosed GBM recently reported that toxicities were acceptable to continue enrollment and a preliminary analysis of efficacy showed encouraging mean progression-free survival [58]. “Pure” antiangiogenic drugs, such as bevacizumab, should reenforce the antiangiogenic effects of certain cytotoxics. For TMZ in particular, we have demonstrated in the present study its antiangiogenic properties in vitro and in vivo when used alone. Using the Web site developed by the National Library of Medicine for the US National Institutes of Health, the authors obtained information on eight clinical trials being conducted with bevacizumab in combination with TMZ, which are recruiting patients with GBMs including those newly diagnosed. Our present study further validates these approaches.
Footnotes
This work has been supported partly by grants awarded by the Fonds Yvonne Boël (Brussels, Belgium) and by the FNRS (Brussels, Belgium).
References
- 1.Louis DN. Molecular pathology of malignant gliomas. Annu Rev Pathol Mech Dis. 2006;1:97–117. doi: 10.1146/annurev.pathol.1.110304.100043. [DOI] [PubMed] [Google Scholar]
- 2.Ohgaki H, Kleihues P. Genetic pathways to primary and secondary glioblastoma. Am J Pathol. 2007;170:1445–1453. doi: 10.2353/ajpath.2007.070011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lefranc F, Brotchi J, Kiss R. Possible future issues in the treatment of glioblastomas: special emphasis on cell migration and the resistance of migrating glioblastoma cells to apoptosis. J Clin Oncol. 2005;23:2411–2422. doi: 10.1200/JCO.2005.03.089. [DOI] [PubMed] [Google Scholar]
- 4.Lefranc F, Kiss R. The sodium pump alpha1 subunit as a potential target to combat apoptosis-resistant glioblastomas. Neoplasia. 2008;10:198–206. doi: 10.1593/neo.07928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lefranc F, Sadeghi N, Camby I, Metens T, Dewitte O, Kiss R. Present and potential future issues in glioblastoma treatment. Expert Rev Anticancer Ther. 2006;6:719–732. doi: 10.1586/14737140.6.5.719. [DOI] [PubMed] [Google Scholar]
- 6.Lefranc F, Facchini V, Kiss R. Proautophagic drugs: a novel means to combat apoptosis-resistant cancers, with a special emphasis on glioblastomas. Oncologist. 2007;12:1395–1403. doi: 10.1634/theoncologist.12-12-1395. [DOI] [PubMed] [Google Scholar]
- 7.Wemmert S, Ketter R, Rahnenführer J, Beerenwinkel N, Strowitzki M, Feiden W, Hartmann C, Lengauer T, Stockhammer F, Zang KD, et al. Patients with high-grade gliomas harboring deletions of chromosomes 9p and 10q benefit from temozolomide treatment. Neoplasia. 2005;7:883–893. doi: 10.1593/neo.05307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 9.Chakravarti A, Erkkinen MG, Nestler U, Stupp R, Mehta M, Aldape K, Gilbert MR, Black PM, Loeffler JS. Temozolomide-mediated radiation enhancement in glioblastoma: a report on underlying mechanisms. Clin Cancer Res. 2006;12:4738–4746. doi: 10.1158/1078-0432.CCR-06-0596. [DOI] [PubMed] [Google Scholar]
- 10.Kanzawa T, Germano IM, Komata T, Itoh H, Konco Y, Kondo S. Role of autophagy in temozolomide-induced cytotoxicity for malignant glioma cells. Cell Death Differ. 2004;11:448–457. doi: 10.1038/sj.cdd.4401359. [DOI] [PubMed] [Google Scholar]
- 11.Roos WP, Batista LF, Naumann SC, Wick W, Weller M, Menck CF, Kaina B. Apoptosis in malignant glioma cells triggered by the temozolomide-induced DNA lesion O6-methylguanine. Oncogene. 2007;26:186–197. doi: 10.1038/sj.onc.1209785. [DOI] [PubMed] [Google Scholar]
- 12.Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352:997–1003. doi: 10.1056/NEJMoa043331. [DOI] [PubMed] [Google Scholar]
- 13.Hermisson M, Klumpp A, Wick W, Wischhusen J, Nagel G, Roos W, Kaina B, Weller M. O6-methylguanine DNA methyltransferase and p53 status predict temozolomide sensitivity in human malignant glioma cells. J Neurochem. 2006;96:766–776. doi: 10.1111/j.1471-4159.2005.03583.x. [DOI] [PubMed] [Google Scholar]
- 14.Yamini B, Yu X, Dolan ME, Wu MH, Kufe DW, Weichselbaum RR. Inhibition of nuclear factor-kappaB activity by temozolomide involves O6-methylguanine induced inhibition of p65 DNA binding. Cancer Res. 2007;67:6889–6898. doi: 10.1158/0008-5472.CAN-06-4496. [DOI] [PubMed] [Google Scholar]
- 15.Hu X, Pandolfi PP, Li Y, Koutcher JA, Rosenblum M, Holland EC. mTOR promotes survival and astrocytic characteristics induced by Pten/AKT signaling in glioblastoma. Neoplasia. 2005;7:356–368. doi: 10.1593/neo.04595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hirose Y, Katayama M, Mirzoeva OK, Berger MS, Pieper RO. Akt activation suppresses Chk2-mediated, methylating agent-induced G2 arrest and protects from temozolomide-induced mitotic catastrophe and cellular senescence. Cancer Res. 2005;65:4861–4869. doi: 10.1158/0008-5472.CAN-04-2633. [DOI] [PubMed] [Google Scholar]
- 17.Kurzen H, Schmitt S, Näher H, Môhler T. Inhibition of angiogenesis by non-toxic doses of temozolomide. Anticancer Drugs. 2003;14:515–522. doi: 10.1097/00001813-200308000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Son MJ, Kim JS, Kim MH, Song HS, Kim JT, Kim H, Shin T, Jeon HJ, Lee DS, Park SY, et al. Combination treatment with temozolomide and thalidomide inhibits tumor growth and angiogenesis in an orthotopic glioma model. Int J Oncol. 2006;28:39–53. [PubMed] [Google Scholar]
- 19.Kim JT, Kim JS, Ko KW, Kong DS, Kang CM, Kim MH, Son MJ, Song HS, Shin HJ, Lee DS, et al. Metronomic treatment of temozolomide inhibits tumor cell growth through reduction of angiogenesis and augmentation of apoptosis in orthotopic models of gliomas. Oncol Rep. 2006;16:33–39. [PubMed] [Google Scholar]
- 20.Zhou Q, Guo P, Wang X, Nuthalapati S, Gallo JM. Preclinical pharmacokinetic and pharmacodynamic evaluation of metronomic and conventional temozolomide dosing regimens. J Pharmacol Exp Ther. 2007;321:265–275. doi: 10.1124/jpet.106.118265. [DOI] [PubMed] [Google Scholar]
- 21.Katayama M, Kawaguchi T, Berger MS, Pieper RO. DNA damaging agent-induced autophagy produces a cytoprotective adenosine triphosphate surge in malignant glioma cells. Cell Death Differ. 2007;14:548–558. doi: 10.1038/sj.cdd.4402030. [DOI] [PubMed] [Google Scholar]
- 22.Fisher T, Galanti G, Lavie G, Jacob-Hirsch J, Kventsel I, Zeligson S, Winkler R, Simon AJ, Amariglio N, Rechavi G, et al. Mechanisms operative in the antitumor activity of temozolomide in glioblastoma multiforme. Cancer J. 2007;13:335–349. doi: 10.1097/PPO.0b013e318157053f. [DOI] [PubMed] [Google Scholar]
- 23.Le Mercier M, Lefranc F, Mijatovic T, Debeir O, Haibe-Kains B, Bontempi G, Decaestecker C, Kiss R, Mathieu V. Evidence of galectin-1 involvement in glioma chemoresistance. Toxicol Appl Pharmacol. 2008;229:172–183. doi: 10.1016/j.taap.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 24.LeMercier M, Mathieu V, Haibe-Kains B, Bontempi G, Mijatovic T, Decaestecker C, Kiss R, Lefranc F. Knocking down galectin-1 in human Hs683 glioblastoma cells impairs both angiogenesis through ORP150 depletion and endoplasmic reticulum stress responses. J Neuropathol Exp Neurol. 2008;67:456–469. doi: 10.1097/NEN.0b013e318170f892. [DOI] [PubMed] [Google Scholar]
- 25.Le QT, Shi G, Cao H, Nelson DW, Wang Y, Chen EY, Zhao S, Kong C, Richardson D, O'Byrne KJ, et al. Galectin-1: a link between tumor hypoxia and tumor immune privilege. J Clin Oncol. 2005;23:8932–8941. doi: 10.1200/JCO.2005.02.0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thijssen VL, Postel R, Brandwijk RJ, Dings RP, Nesmelova I, Satijn S, Verhofstad N, Nakabeppu Y, Baum LG, Bakkers J, et al. Galectin-1 is essential in tumor angiogenesis and is a target for antiangiogenesis therapy. Proc Natl Acad Sci USA. 2006;103:15975–15980. doi: 10.1073/pnas.0603883103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Camby I, Belot N, Lefranc F, Sadeghi N, de Launoit Y, Kaltner H, Musette S, Darro F, Danguy A, Salmon I, et al. Galectin-1 modulates human glioblastoma cell migration into the brain through modifications to the actin cytoskeleton and levels of expression of small GTPases. J Neuropathol Exp Neurol. 2002;61:585–596. doi: 10.1093/jnen/61.7.585. [DOI] [PubMed] [Google Scholar]
- 28.Norden AD, Young GS, Setayesh K, Muzikansky A, Klufas R, Ross GL, Ciampa AS, Ebbeling LG, Levy B, Drappatz J, et al. Bevacizumab for recurrent malignant gliomas: efficacy, toxicity, and patterns of recurrence. Neurology. 2008;70:779–787. doi: 10.1212/01.wnl.0000304121.57857.38. [DOI] [PubMed] [Google Scholar]
- 29.Mégalizzi V, Mathieu V, Mijatovic T, Gailly P, Debeir O, De Neve N, Van Damme M, Bontempi G, Haibe-Kains B, Decaestecker C, et al. 4-IBP, a sigma1 receptor agonist, decreases the migration of human cancer cells, including glioblastoma cells, in vitro and sensitizes them in vitro and in vivo to cytotoxic insults of proapoptotic and proautophagic drugs. Neoplasia. 2007;9:358–369. doi: 10.1593/neo.07130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Branle F, Lefranc F, Camby I, Jeuken J, Geurts-Moespot A, Sprenger S, Sweep F, Kiss R, Salmon I. Evaluation of the efficiency of chemotherapy in in vivo orthotopic models of human glioma cells with and without 1p19q deletions and in C6 rat orthotopic allografts serving for the evaluation of surgery combined with chemotherapy. Cancer. 2002;95:641–655. doi: 10.1002/cncr.10710. [DOI] [PubMed] [Google Scholar]
- 31.Lefranc F, Mijatovic T, Mathieu V, Rorive S, Decaestecker C, Debeir O, Brotchi J, Van Ham P, Salmon I, Kiss R. Characterization of gastrin-induced proangiogenic effects in vivo in orthotopic U373 experimental human glioblastomas and in vitro in human umbilical vein endothelial cells. Clin Cancer Res. 2004;10:8250–8265. doi: 10.1158/1078-0432.CCR-04-0343. [DOI] [PubMed] [Google Scholar]
- 32.Mijatovic T, Mahieu T, Bruyère C, De Nève N, Dewelle J, Simon G, Dehoux MJ, van der Aar E, Haibe-Kains B, Bontempi G, et al. UNBS5162, a novel naphthalimide that decreases CXCL chemokine expression in experimental prostate cancers. Neoplasia. 2008;10:573–586. doi: 10.1593/neo.08290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mathieu V, Mijatovic T, van Damme M, Kiss R. Gastrin exerts pleiotropic effects on human melanoma cell biology. Neoplasia. 2005;7:930–943. doi: 10.1593/neo.05379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lefranc F, Sadeghi N, Metens T, Brotchi J, Salmon I, Kiss R. Characterization of gastrin-induced cytostatic effect on cell proliferation in experimental malignant gliomas. Neurosurgery. 2003;52:881–890. doi: 10.1227/01.neu.0000053366.00088.80. discussion 890–891. [DOI] [PubMed] [Google Scholar]
- 35.Benezra R, Rafii S, Lyden D. The Id proteins and angiogenesis. Oncogene. 2001;20:8334–8341. doi: 10.1038/sj.onc.1205160. [DOI] [PubMed] [Google Scholar]
- 36.Sakurai D, Tsuchiya N, Yamaguchi A, Okaji Y, Tsuno NH, Kobata T, Takahashi K, Tokunaga K. Crucial role of inhibitor of DNA binding/differentiation in the vascular endothelial growth factor-induced activation and angiogenic processes of human endothelial cells. J Immunol. 2004;173:5801–5809. doi: 10.4049/jimmunol.173.9.5801. Erratum (2005): J Immunol174, 3818. [DOI] [PubMed] [Google Scholar]
- 37.Lôfstedt T, Jôgi A, Sigvardsson M, Gradin K, Poellinger L, Påhlman S, Axelson H. Induction of ID2 expression by hypoxia-inducible factor-1. J Biol Chem. 2004;279:39223–39231. doi: 10.1074/jbc.M402904200. [DOI] [PubMed] [Google Scholar]
- 38.Lasorella A, Rothschild G, Yokota Y, Russell RG, Iavarone A. ID2 mediates tumor initiation, proliferation, and angiogenesis in Rb mutant mice. Mol Cell Biol. 2005;25:3563–3574. doi: 10.1128/MCB.25.9.3563-3574.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shchors K, Shchors E, Rostker F, Lawlor ER, Brown-Swigart L, Evan GI. The Myc-dependent angiogenic switch in tumors is mediated by interleukin 1beta. Genes Dev. 2006;20:2527–2538. doi: 10.1101/gad.1455706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Watnick RS, Cheng YN, Rangarajan A, Ince TA, Weinberg RA. Ras modulates Myc activity to repress thrombospondin-1 expression and increase tumor angiogenesis. Cancer Cell. 2003;3:219–231. doi: 10.1016/s1535-6108(03)00030-8. [DOI] [PubMed] [Google Scholar]
- 41.Kim JW, Gao P, Liu YC, Semenza GL, Dang CV. Hypoxia-inducible factor 1 and dysregulated c-Myc cooperatively induce vascular endothelial growth factor and metabolic switches hexokinase 2 and pyruvate dehydrogenase kinase 1. Mol Cell Biol. 2007;27:7381–7393. doi: 10.1128/MCB.00440-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang LE. Carrot and stick: HIF-alpha engages c-Myc in hypoxic adaptation. Cell Death Differ. 2008;15:672–677. doi: 10.1038/sj.cdd.4402302. [DOI] [PubMed] [Google Scholar]
- 43.Vredenburgh JJ, Desjardins A, Herndon JE, II, Marcello J, Reardon DA, Quinn JA, Rich JN, Sathornsumetee S, Gururangan S, Sampson J, et al. Bevacizumab plus irinotecan in recurrent glioblastoma multiforme. J Clin Oncol. 2007;25:4722–4729. doi: 10.1200/JCO.2007.12.2440. [DOI] [PubMed] [Google Scholar]
- 44.Ali MA, Choy H, Habib AA, Saha D. SNS-032 prevents tumor cell-induced angiogenesis by inhibiting vascular endothelial growth factor. Neoplasia. 2007;9:370–381. doi: 10.1593/neo.07136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bergers G, Benjamin LE. Tumorigenesis and the angiogenic switch. Nat Rev Cancer. 2003;3:401–410. doi: 10.1038/nrc1093. [DOI] [PubMed] [Google Scholar]
- 46.Li L, Lin X, Shoemaker AR, Albert DH, Fesik SW, Shen Y. Hypoxia-inducible factor-1 inhibition in combination with temozolomide treatment exhibits robust antitumor efficacy in vivo. Clin Cancer Res. 2006;12:4747–4754. doi: 10.1158/1078-0432.CCR-05-2842. [DOI] [PubMed] [Google Scholar]
- 47.Devineni D, Klein-Szanto A, Gallo JM. Uptake of temozolomide in a rat glioma model in the presence and absence of the angiogenesis inhibitor TNP-470. Cancer Res. 1996;56:1983–1987. [PubMed] [Google Scholar]
- 48.Ma J, Pulfer S, Li S, Chu J, Reed K, Gallo JM. Pharmacodynamic-mediated reduction of temozolomide tumor concentrations by the angiogenesis inhibitor TNP-470. Cancer Res. 2001;61:5491–5498. [PubMed] [Google Scholar]
- 49.Ma J, Li S, Reed K, Guo P, Gallo JM. Pharmacodynamic-mediated effects of the angiogenesis inhibitor SU5416 on the tumor disposition of temozolomide in subcutaneous and intracerebral glioma xenograft models. J Pharmacol Exp Ther. 2003;305:833–839. doi: 10.1124/jpet.102.048587. [DOI] [PubMed] [Google Scholar]
- 50.Claes A, Wesseling P, Jeuken J, Maass C, Heerschap A, Leenders WP. Antiangiogenic compounds interfere with chemotherapy of brain tumors due to vessel normalization. Mol Cancer Ther. 2008;7:71–78. doi: 10.1158/1535-7163.MCT-07-0552. [DOI] [PubMed] [Google Scholar]
- 51.Zhou Q, Guo P, Gallo JM. Impact of angiogenesis inhibition by sunitinib on tumor distribution of temozolomide. Clin Cancer Res. 2008;14:1540–1549. doi: 10.1158/1078-0432.CCR-07-4544. [DOI] [PubMed] [Google Scholar]
- 52.Gasparini G, Longo R, Fanelli M, Teicher BA. Combination of antiangiogenic therapy with other anticancer therapies: results, challenges, and open questions. J Clin Oncol. 2005;23:1295–1311. doi: 10.1200/JCO.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 53.Bäuerle T, Hilbig H, Bartling S, Kiessling F, Kersten A, Schmitt-Gräff A, Kauczor HU, Delorme S, Berger MR. Bevacizumab inhibits breast cancer-induced osteolysis, surrounding soft tissue metastasis, and angiogenesis in rats as visualized by VCT and MRI. Neoplasia. 2008;10:511–520. doi: 10.1593/neo.08220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Volk LD, Flister MJ, Bivens CM, Stutzman A, Desai N, Trieu V, Ran S. Nab-paclitaxel efficacy in the orthotopic model of human breast cancer is significantly enhanced by concurrent anti-vascular endothelial growth factor A therapy. Neoplasia. 2008;10:613–623. doi: 10.1593/neo.08302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kerbel RS. Antiangiogenic therapy: a universal chemosensitization strategy for cancer? Science. 2006;312:1171–1175. doi: 10.1126/science.1125950. [DOI] [PubMed] [Google Scholar]
- 56.Chamberlain MC. Bevacizumab plus irinotecan in recurrent glioblastoma. J Clin Oncol. 2008;26:1012–1013. doi: 10.1200/JCO.2007.15.1605. author reply 1013. [DOI] [PubMed] [Google Scholar]
- 57.Nieder C, Wiedenmann N, Andratschke N, Molls M. Current status of angiogenesis inhibitors combined with radiation therapy. Cancer Treat Rev. 2006;32:348–364. doi: 10.1016/j.ctrv.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 58.Lai A, Filka E, McGibbon B, Nghiemphu PL, Graham C, Yong WH, Mischel P, Liau LM, Bergsneider M, Pope W, et al. Phase II pilot study of bevacizumab in combination with temozolomide and regional radiation therapy for up-front treatment of patients with newly diagnosed glioblastoma multiforme: interim analysis of safety and tolerability. Int J Radiat Oncol Biol Phys. 2008;71:1372–1380. doi: 10.1016/j.ijrobp.2007.11.068. [DOI] [PubMed] [Google Scholar]