Abstract
At a Nigerian university hospital, none of the motorcyclists who presented over a 12 month period had been wearing a helmet, and of the eight patients who died, seven had head injuries. Of the five collision types described, the rate of motorcycle‐other vehicle collisions was highest at 40.6%, while the motorcycle‐pedestrian rate was 23.4%. Measures to prevent these collisions might reduce overall crashes by 64%; in addition, helmet law should be enforced.
Keywords: motorcycle, Nigeria
Motorcycles injuries (MCIs) are underreported from developing countries. Globally, road traffic injuries (RTIs) are responsible for a significant proportion of overall injury morbidity and mortality; 90% of mortalities are seen in developing countries.1 Motorcycle users are vulnerable on the road and represent an important group to target for reducing RTIs. Even in developed countries with low morbidity and mortality rates from MCIs, the risk of dying for every kilometer travelled from a motorcycle crash is 20 times higher than from a motor vehicle crash.2 Despite a doubling of the numbers of automobiles in Nigeria—144 480 units to 284 124 units,3 there has been little change in the proportion of MCIs among RTIs.4,5,6,7 The motorcycle, commonly called “okada” in Nigeria, has become increasingly popular as a means of commercial transport as it is often the only means of transport available and is useful for navigating poor road networks or traffic hold‐ups. The riders often ignore safety measures, making them more vulnerable to accidents with other motorized vehicles.8 In addition, the absence of pedestrian walkways has increased the vulnerability of pedestrians to all motorized vehicles.
Previous studies have shown that limb and head injuries are the commonest causes of morbidity and mortality in MCIs,2,5,8 attributing the latter to the low use of crash helmets in Nigeria; a situation seen in other developing countries. An apparent increase in MCIs has been noted; it is therefore the aim of this study to determine the scope and type of collisions from motorcycle injuries and the rate of helmet use among riders and passengers visiting a hospital, to identify potential areas of intervention in order to reduce morbidity and mortality from MCIs.
Patients and methods
This was a prospective study of patients with MCIs excluding ocular injuries presenting at the surgical emergency room of the University of Ilorin Teaching Hospital (UITH), Nigeria from 1 August 2004 to 31 July 2005. The UITH is the only functional major hospital with capacity to promptly treat injured patients from Kwara, northern parts of Oyo, Osun, the southern part of Niger, and western parts of Kogi and Ekiti States of Nigeria. Nigeria has 36 states, a population of 120 million; the catchment area of the UITH is about 10 million.
Data collected on a proforma included age, gender, occupation, injury host status (whether rider, passenger, or pedestrian), type of collision (motorcycle‐other vehicles, motorcycle‐motorcycle, motorcycle‐pedestrian, lone motorcyclist, and other collisions). The prehospital transport by relatives, police/federal road safety corps, and bystanders was studied, in addition to injury arrival interval (0–1 hour, >1–6 hours, >6–24 hours, >24–48 hours, >48 hours), helmet use, and body regions injured. Other outcome variables using trauma scores were injury severity score (ISS), revised trauma score (RTS), probability of survival (TRISS), and whether alive or dead. Two of the authors (AAN and OKO) collected the data within hours of the arrival of the patients.
Results
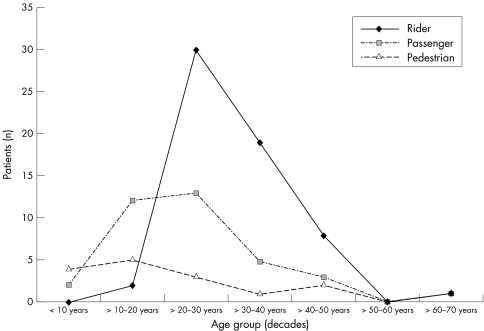
Within the period, 412 RTI patients presented; 112 (27.2%) were MCI victims—99 males and 13 females, age range 5–70 years, mean (SD) 28.7 (11.5) years, peak incidence 21–30 years (46 patients, 41.1%; fig 1).
Figure 1 Distribution of riders, passengers, and pedestrians among the age groups.
The majority of patients arrived under 1 hour (76, 67.9%); 16 patients (14.3%) arrived after 1 hour but less than 6 hours; seven patients (6.3%) arrived after 6 hours but less than 24 hours; two patients arrived between 24 and 48 hours, and six patients arrived after 48 hours.
The majority of the MCI patients were students (people attending school as well as those in higher education: 23, 20.5%) either as passengers or pedestrians while on journeys to and from school; while others—traders (17.9%), artisans (17.0%), and commercial cyclists (11.6%)—were mainly riders. However, riders were in the majority (60, 53.6%) while passengers numbered 36 (32.1%) and pedestrians 16 (14.3%). None was wearing a helmet at the time of injury.
Five types of collisions occurred: motorcycle‐other vehicle collisions (morbidity 46 and mortality 2), motorcycle‐pedestrian (27 and 1), lone motorcyclist crash (25 and 2), motorcycle‐motorcycle (12 and 3), and other collisions (2 and 0). The lone motorcyclist crashes were collisions with stationary objects and unexpected loss of control. Many patients, 79 (70.5%), sustained injuries to the extremities while 71 (63.4%) had head injuries, suggesting existence of multiple injuries (table 1).
Table 1 Site of injuries among the victims.
| Site | Riders | Passengers | Pedestrian | Patients (%) |
|---|---|---|---|---|
| Extremities | 35 | 32 | 12 | 79 (70.5) |
| Head and neck | 57 | 23 | 1 | 71 (63.4) |
| Chest | 4 | 2 | 1 | 7 (6.2) |
| Abdomen | 1 | 0 | 2 | 3 (2.7) |
| Pelvis | 0 | 1 | 0 | 1 (0.9) |
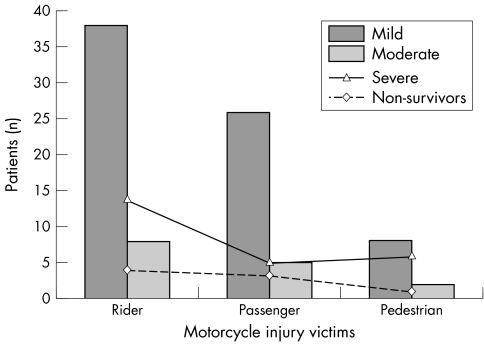
In figure 2, 76.8%, sustained mild to moderate trauma with ISS <15, although 91.1% had TRISS ⩾95% probability of survival. Eight patients died, seven of whom had HI with ISS >15 although only six had probability of survival (TRISS) ⩾50%. The eighth patient died of excessive blood loss from open fractures which had occurred 80 km away. Four of the dead were riders, three were passengers, and one was a pedestrian. Five patients needed intensive care; all had head injury and three of them died. Of the 104 survivors (92.9%), 65.4% were discharged, 29.8% discharged against medical advice (DAMA), and 4.8% transferred. No postmortem was done for any of the mortalities.
Figure 2 Severity of injury among the victims of motorcycle injury.
Discussion
This study did not capture some fatal and non‐fatal MCIs (which include people who have been saved from injury through helmet use as they did not present in the hospital). This paper has shown that the incidence of MCIs from Nigeria has doubled (27%), compared to 10.3–14.1% in previous studies.5,6,7 It is similar to 22.8% in China,9 but much lower than the 62% in Vietnam.10 In Nigeria, four reasons sustain increasing use of motorcycles: cheaper cost when brand new (about US$500) compared to second hand cars (about US$3000); only means of transport to many streets, connecting roads, or villages; fast and can beat traffic jams in urban roads; and because commercial operators make quick money (in fact, many are quitting menial jobs and becoming commercial riders overnight and without undergoing the necessary pre‐license tests).11 The 53.6% riders found in this study agrees with others with 41.7% to 62.6% riders.5,6,7,8 This suggests that riders constitute the majority among MCI victims reporting to hospital. As students were the largest group of MCI victims while journeying to and from school, an improved school transportation system that obviates students' need for the motorcycle may reduce MCI incidence.
Five types of crashes were reported showing how motorcyclists are vulnerable to other motor vehicles and how pedestrians remain vulnerable to motorcyclists. Is vulnerability a question of size, speed, or both? This is a viable direction of future study. Improved visibility (use of daytime running lights and reflective clothing), better driver training, education, and speed reduction are effective measures that can reduce collisions.
None of the patients wore a helmet at the time of injury. Head injuries from MCIs are associated with a five‐ to sixfold chance of death than those from other vehicles.12 It is common knowledge that helmet use in developing countries is low.5,8 However, Asogwa in Nigeria in 1980 reported that 34.5% of riders used helmets.11 Studies have shown that helmets reduce mortality from head injuries.13,14 In Nigeria, a mandatory helmet law was repealed in 1979 and was recently re‐enacted in the last six months of this study, yet no‐one used a helmet in this study—the result of non‐compliance by motorcyclists and reluctant enforcement by the authority. We gathered that the government itself discouraged enforcement for political reasons because many riders (political party supporters) gave excuses regarding cost of helmets and the tropical heat (personal communication with the Kwara State Sector Commander of the Federal Road Safety Commission, the agency charged with enforcing safety on Nigerian roads). As seven of the eight dead patients and all five patients who needed intensive care were head injured, three of whom later died, and because head injury was also seen in 63.4% patients, the necessity for helmet use is more than justified in this study. Making low cost helmets that are appropriate in hot weather available and enforcement of helmet use might be helpful. Enactment and enforcement of helmet laws in other climes have been found to increase rates of helmet use15,16 while repeal of such laws has led to an increase in the non‐helmeted crash scene fatality rate.17 Seventy five percent (six) of the dead patients had more than 50% probability of survival accounting for a preventable death rate of 75%. Although it was shown in figure 2 that these were patients with severe injuries (ISS>15), the high probability of survival despite this suggests the poor state of healthcare services, especially in‐hospital care, which previous studies have documented.18,19 The high proportion of patients who discharged against medical advice was 29.8%, higher than the 4.1% reported by Odelowo in the same centre 20 years earlier.5 Many of these were due to patronage of traditional bone setters (indigenous people (non‐doctors) who are self‐taught and popular because of their accessibility and low charges) for extremity injuries, which were the most common.20
A broader study involving other regions and one comparing injuries from four‐wheel vehicles may disclose other special features of MCIs.
Key points
Of all road traffic injury, the incidence of motorcycle injury (MCI) reported from Nigeria since 1966 has been about 13%.
Limb and head injuries are the most common types of injury.
The incidence of MCI from Nigeria has since doubled to 27%.
Five types of collisions in MCIs have been described, with the highest mortality from motorcycle‐motorcycle collisions.
Students are the largest group of motorcycle injury victims, both as passengers or pedestrians.
Low cost helmets that are appropriate in hot weather should be made available and helmet use enforced.
Abbreviations
ISS - injury severity score
MCI - motorcycle injury
RTI - road traffic injury
RTS - revised trauma score
TRISS - probability of survival
UITH - University of Ilorin Teaching Hospital
References
- 1.Peden M, McGee K, Sharma G.The Injury Chart Book: A graphical overview of the global burden of injuries. Geneva: World Health Organization, 20025
- 2.Peden M.World report on road traffic injury prevention‐summary. Geneva: World Health Organization, 200412
- 3.Owosina F A O. The traffic scene in Nigeria—an African example. The WHO/OBCD/World Bank's Conference on road traffic accidents in developing countries, Mexico City 198136–38.
- 4.Oyemade A. Epidemiology of road traffic accidents in Ibadan and its environs. Nig Med J 19733174–177. [Google Scholar]
- 5.Odelowo E O O. Pattern of trauma resulting from motorcycle accidents in Nigerians: a two‐year prospective study. Afr J Med Med Sci 199423109–112. [PubMed] [Google Scholar]
- 6.Adegbehingbe B O, Oluwadiya K S, Adegbehingbe O O. Motorcycle associated ocular injuries in Ile‐Ife, Nigeria. African Journal of Trauma 2004235–39. [Google Scholar]
- 7.Umebese P F A, Okukpo S U. Motorcycle accidents in a Nigerian university campus: a one year study of the pattern of trauma sustained in University of Benin Campus. Nig J Clin Pract 2001433–36. [Google Scholar]
- 8.Oluwadiya K S, Oginni I M, Olasinde A A.et al Motorcycle limb injuries in a developing country. West Afr J Med 20042342–46. [DOI] [PubMed] [Google Scholar]
- 9.Zhang J, Norton R, Tang K C.et al Motorcycle ownership and injury in China. Inj Control Saf Promot 200411159–163. [DOI] [PubMed] [Google Scholar]
- 10.Nantulya V M, Reich M R. The neglected epidemic: road traffic injuries in developing countries. BMJ 20023241139–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asogwa S E. Some characteristics of drivers and riders involved in road traffic accidents in Nigeria. East Afr Med J 198057399–404. [PubMed] [Google Scholar]
- 12.Sosin D M, Sacks J J. Motorcycle helmet‐use laws and head injury prevention. JAMA 19922671649–1651. [DOI] [PubMed] [Google Scholar]
- 13.Keng S H. Helmet use and motorcycle fatalities in Taiwan. Accid Anal Prev 200531349–355. [DOI] [PubMed] [Google Scholar]
- 14.Brandt M M, Ahrns K S, Corpron C A.et al Hospital cost is reduced by motorcycle helmet use. J Trauma 200253469–471. [DOI] [PubMed] [Google Scholar]
- 15.Ichikawa M, Chadbunchachai W, Marui E. Effect of the helmet act for motorcyclists in Thailand. Accid Anal Prev 200335183–189. [DOI] [PubMed] [Google Scholar]
- 16.Muelleman R L, Mlinek E J, Collicot P E. Motorcycle crash injuries and costs: effect of a re‐enacted comprehensive helmet use law. Ann Emerg Med 199221266–272. [DOI] [PubMed] [Google Scholar]
- 17.Bledsoe G H, Schexnayder S M, Carey M J.et al The negative impact of the repeal of the Arkansas motorcycle helmet law. J Trauma 2002531078–86 discussion 1086–7. [DOI] [PubMed] [Google Scholar]
- 18.Solagberu B A, Adekanye A O, Ofoegbu C P K.et al Clinical spectrum of trauma at a university hospital in Nigeria. Eur J Trauma 200228365–369. [Google Scholar]
- 19.Solagberu B A, Kuranga S A, Adekanye A O.et al Preventable trauma deaths in a country without emergency medical services. African Journal of Trauma 2003139–44. [Google Scholar]
- 20.Solagberu B A. Long bone fractures treated by traditional bonesetters: a study of patients' behaviour. Trop Doc 200535106–107. [DOI] [PubMed] [Google Scholar]